Abstract
Objective
Social network analysis was used to examine whether peer influence from one’s social networks moderates obesity prevention program effects on obesity related behaviors: healthful behaviors and unhealthful ones.
Design and Methods
Participants included 557 children residing in Southern California. Survey assessed health promoting behaviors (i.e., physical activity at school, physical activity outside of school, and fruit and vegetable intake), as well as unhealthful ones (high calorie low nutrient intake and sedentary activity), and peer exposure calculated from social network nominations as indicators of peer influence. Multilevel models were conducted separately on outcomes predicted by program participation, peer exposure, and program participation by peer exposure.
Results
Results indicated that peer exposure was positively associated with one’s own behavior for both healthful and unhealthful behaviors. Program participation effects were moderated by peer influence, but only when unhealthful peer influence was present. Results suggest that peer influence can diminish or amplify prevention programs
Conclusion
Future interventions should consider peer-led components to promote healthful influence of peers on healthful and unhealthful behaviors, and programs should be mindful that their effects are moderated by social networks.
Keywords: Social Network, Peer Influence, Obesity Prevention, Childhood Obesity, Program Effects
Introduction
Childhood obesity is a major public health problem in the United States. Recent data show that 16.9% of US children and adolescents are obese1 and the rate is increasing,2 although small decreases in the prevalence of extreme obesity among US preschool children from low income families have been recently shown.3 Public health concern is growing in this area as childhood obesity is likely to persist into adulthood with greater risk for developing health problems.4 This strongly suggests the need for early interventions to modify obesity-related risk behaviors at younger ages.5
Schools have been identified as an important context for the implementation of obesity prevention programs because attendance is almost universal.6 Several reviews have concluded that school-based programs can be effective in preventing childhood obesity in the short-term.7,8 However, the long-term effectiveness of these programs remains unclear, perhaps due to a lack of consideration of contextual influences that may compete with or undermine program effects, such as existing school food and physical activity policies.7 Thus, our understanding of the heterogeneity in school-based obesity prevention effectiveness may be improved by exploring contextual factors that moderate school-based prevention programs. One factor that has not been examined as a potential moderator of school-based obesity prevention effects is the influence of peer social networks, even though they have been identified as a primary social influence on children’s development.9, 10 In addition, studies show that body mass index (BMI) clustering can be demonstrated among school friends11 and adults.12
At least three theories may be useful in understanding how peer influence may have an impact on childhood obesity-related behaviors, especially with food intake and physical activity. First, social facilitation theory suggests that the mere presence of others can promote certain behaviors.13, 14 Change in eating and physical activity patterns as a result of presence of friends has been demonstrated in previous studies.9 Second, social learning theory posits that people adjust behaviors in response to modeled behavior.14, 15 Children have been shown to be influenced by the type (healthful/unhealthful) or amount of food intake and physical activity modeled by their peers.16, 17 Third, impression management has been identified as the individual’s motivation for changing eating or physical activity behavior.14 In order to maintain a certain image, the literature suggests children and adolescents will conform to peer’s behavior, such as in consuming fast food,18 selecting energy dense snacks,19 or being athletic.20 Although previous studies have explained the underlying mechanisms of peer influence, none of these studies have evaluated how it can interact with obesity prevention programs to diminish or amplify program effects.
One way to measure the effect of peer influence on health is through social network analysis. Conventionally measured by friendship nominations, analyzing social networks allow us to examine how much interaction exists between friends.21 We can also predict what type of peer influence (healthful/unhealthful) is prevalent, if we have information on the nominated friends. For example, if a student has more friends who eat fast food (unhealthful influence), the student will be exposed to greater negative peer behavior that may lead to less healthful eating. On the other hand, if a student is exposed to more friends who offer a positive influence, the student may be more likely to eat healthier food, such as fruits and vegetables (healthful influence). The current study is unique in that it used the friends’ report of their own behaviors to measure peer exposure, rather than relying on children’s perception of their friends’ behavior.
Although previous studies support the importance of school-based interventions and the role of peers, what has not been examined is whether peer influence can moderate an obesity prevention program. To fill this gap, this study has two objectives. The first is to explore the impact of peer influence on obesity-related health behaviors among children. As social facilitation occurs, we hypothesized that peer exposure would be associated with eating and physical activity patterns such that unhealthful peer influence would be associated with unhealthful individual behavior. The second objective is to examine whether peer social networks can moderate obesity prevention program effects on children. Because the prevention program focused on decision-making skills and social competence, we expected that it would translate to reject unhealthful peer influence. Based on previous theories, we expect program intervention may enhance children’s ability to judge peer modeling and the impression they wish to make on their peers. We hypothesized that the effect of school-based child obesity prevention will attenuate unhealthful peer influence and accentuate healthful peer influence for healthier behavioral outcomes.
Methods
Research and Measurement Designs
The present study is part of an ongoing longitudinal multicomponent childhood-obesity prevention study, Pathways to Health (Pathways), developed to promote healthful eating and physical activity in upper elementary school children.22 Pathways is a school-based randomized trial that follows a cohort of students from 4th grade through 6th grade in Southern California. Surveys assessed baseline and 6-month posttest at 4th grade followed by annual post-intervention assessments in 5th grade and 6th grade.23 Twenty-eight schools in Southern California were paired within each school district based on school-level demographic characteristics and randomly assigned to program or control condition.23 Translated from evidence-based substance use prevention programs, it is the first study known to incorporate personal, social, and environmental level mediators including emotional factors such as child impulse control, decision making and emotional regulation.22 A more detailed description of the study can be found elsewhere.22 All procedures of the study were approved by the University of Southern California Review Board.
Analytic Sample
Pathways included a panel of 1,005 fourth grade students with active parental consent. Of those, 709 (70.5%) from 24 schools were successfully tracked through 6th grade. The analysis sample for the present study consisted of students who provided complete social network data for both grades 5 and 6 (N=557). The mean age of participants was 10.74 years (SD =.52) in 5th grade and 11.58 years (SD=.55) in 6th grade. At baseline, 51% (n=283) were female, and 34.83% (n=194) were Hispanic. Twenty two percent (n=125) of the sample reported receiving free/reduced lunch, which was used as a proxy for lower Socio Economic Status (SES). To assess potential sample bias due to participants excluded for missing nomination data, a comparison was made between the participants included in the analyses (n=557) and those excluded from the analyses (n=488) from the 4th grade panel data (baseline) (n=1005) for all variables included in this analysis. Demographic variables were comparable between the two groups; however, excluded participants reported lower rates of receiving free/reduced lunch (χ2(1, N =1005) = 12.13, p <0.001)), higher rates of being Hispanic (χ2(1, N =1005) = 86.54, p <0.001), lower rates of physical activity at school (t(906)=−3.51, p<.001), higher High-Calorie, Low-Nutrient (HCLN) food intake (t (893)=3.05, p<.001) and higher levels of sedentary behaviors (t (902)=2.29, p<0.05).
Measures
Student Assessment
All data were collected by trained researchers with a second person who assisted with answering questions from students. Students completed a 143-item self-report survey that took one classroom period to complete. The items assessed food intake, physical activity, sedentary behavior, and peer networks. Due to time constraints, abbreviated scales were used.24
Physical Activity
Physical activity items were taken from the shorter version of a Physical Activity Questionnaire for Children (PAQ-C)25 that included six items dealing with level of activity in various settings.26 For example, items were phrased “In the last 7 days, during recess how often were you very active?” Response choices ranged from 1(=”None or I did not have PE, recess, etc.”) to 5 (= “6 or more times”). For the current study, constructs were further categorized into physical activity at school (3 items), and physical activity out of school (6 items).
Food Intake
Seven fruit and vegetable intake items were used from the Youth Risk Behavior Survey (YRBS).27 Validity of the scale has been tested for 4th grade students.26 Two items asked about past week fruit intake (e.g., “How often did you eat any fruit, fresh or canned?”) and five items assessed past week vegetable intake (7 items). To assess HCLN items such as candy, soda and French fries, five items were added from a previously validated food-frequency questionnaire.28 Response choice ranged from 1 (=“Less than once a week”) to 6 (=“2 or more of these a day”).
Sedentary Activity
Sedentary activity was adapted from the School Based Nutrition Monitoring Student Questionnaire.29 Three items asked about screen time on TV or video (e.g., On a regular school day, how many hours do you usually watch TV or video movies at home or away from school?), computer and video games. Answer options ranged from 1(e.g., “I don’t watch TV”) to 5 (e.g., “6 or more hours”).26
Team Sports
One item was included to assess whether children participated in one or more team sports. Question asked “During the past 12 months, on how many sports teams did you play?” Response choices ranged from 1= (“0 teams”) to 4 (= “3 or more teams”).
Body Mass Index (BMI) percentiles
Height and weight anthropometric data was converted to BMI (kg/m2) percentile and z-scores with 2000 The Center for Disease Control (CDC) reference charts, BMI percentile-for-age-and-sex.
Social Network Indicators
To obtain network data, students were asked to write the names of their five best friends in class(e.g., Please think of your five BEST FRIENDS in YOUR CLASSROOM.). Nominated friend names were later matched with a classroom roster provided by the school and linked with participant ID numbers for the consented students. Peer exposure was calculated by summing the nominated friends’ self-reported data for each obesity-related behavior outcome. The summation of the five best friends’ outcomes was chosen over the average, because the sum of these scores represented the contribution of each friend’s group behavior better than did the average. Higher peer exposure of fruit and vegetable intake would indicate healthful peer influence, while higher peer exposure to HCLN food intake would indicate unhealthful peer influence. Since the total number of nominated friends varied by student, out-degree (total number of nominations made) was used as a control variable in the final model. We tested models including both 5th and 6th grade peer exposure as predictors, but 5th grade peer exposure was not significant and it was dropped from the final model. Because both the nominator and nominated peers required matching IDs, information on nominated friends without valid IDs were removed from the analyses. Participants in this study nominated two friends in average (Mean=2.14, SD=1.23) after excluding friends that did not participate in this study. The rationale for limiting nominations to five stems from a study by Burt (1984), which showed that five was an optimal number to ask for nominations as the number drops off dramatically after five.30 Since that publication, most studies limit the number of nominations to five and research shows these measures to be valid and reliable.31
Statistical Analysis
Analyses were conducted using, R and SAS.32 Network calculations were performed in R33 then merged with the original dataset in SAS. Class-level intra-class correlations (ICCs) were calculated for the outcomes as the unit of social networks was bounded to classrooms, which ranged from 0 to 0.08. Thus, multilevel models were conducted to account for potential clustering effects, using PROC MIXED in SAS. All analyses were adjusted for demographics variables, network control variables (out-degree) and participation in team sports. We regressed the 6th grade obesity related behavior outcomes on program condition, peer exposure, and the interaction terms between the two. The model controlled for 5th grade obesity behavior instead of baseline values (4th grade) for the following reasons. First, the 4th grade baseline did not include the social network measures because it was added to the survey starting at 5th grade. Second, the 6th grade outcomes were assessed closer in time in 5th grade (12 months) than the baseline measurement (16 months). Theoretically, the effect of the program should remain the same controlling or not controlling for the baseline value of the outcome, since it is not correlated with the program condition due to randomization.
Results
Table 1 shows the group differences between program and control groups for all variables used in the analyses at 5th grade. A total of 343 (62%) students were in the program condition and 214 (38%) in the control. There were no significant group differences observed except that the control group had a higher proportion of students receiving free/reduced lunch (p<.05) and higher mean of physical activity at school (p<.05). The zero-order correlations between an individual’s obesity-related behaviors at 6th grade and that of their peers at 6th grade were all statistically significantly positive (p’s<.05), except for physical activity outside of school (results not shown).
Table 1.
Sample Characteristics at 5th Grade by Group
| Characteristic | Program (n=343) N(%, SE) or M (SE) |
Control (n=214) N(%, SE) or M (SE) |
|---|---|---|
| % Female | 166 (48.40%, 0.03) | 117 (54.67%, 0.03) |
| % Hispanic | 119 (34.69%, 0.03) | 76 (35.51%, 0.03) |
| % Free Lunch | 67 (19.53%, 0.02)* | 58 (27.10%, 0.03)* |
| Physical Activity at School | 3.14 (0.04)* | 3.26 (0.05)* |
| Physical Activity outside of School | 3.22 (0.06) | 3.21 (0.08) |
| Fruit/Vegetable Intake | 2.92 (0.05) | 2.90 (0.06) |
| HCLN Intake | 2.29 (0.05) | 2.22 (0.06) |
| Sedentary Activity | 2.63 (0.06) | 2.60 (0.08) |
n=557. HCLN – High Calorie Low Nutrient food and beverage intake.
p<0.05 based on two-tail test
Table 2 shows the results of the mixed linear regression models examining the relationship between self-reported behavior at 6th grade predicted by peer exposure at 6th grade, intervention program and the interaction between the two. Overall, the results show that, for students with a mean level of 6th grade peer exposure (the standardized 6th grade peer exposure=0), the intervention program had positive effects on physical activity at school (b=.21, p<0.05), physical activity outside of school (b=.14, p<.05), fruit and vegetable intake (b=.19, p<.05), and sedentary activity (b=−.24, p<.001). There were no program effects on HCLN food intake. Findings also show that, for the control group, peer exposure was positively associated with one’s own physical activity at school (b=.74, p<.001), fruit and vegetable intake (b=.39, p<.01), HCLN food intake (b=.35, p<.01) and sedentary behavior at 6th grade (b=.28, p<.01). All models controlled for self-reported behavior at 5th grade and continuous variables were standardized to a mean of 0 and variance of 1. All 5th grade behaviors were strongly associated with 6th grade behaviors.
Table 2.
Predicting 6th grade obesity related behaviors
| Dependent variables from 6th grade | |||||
|---|---|---|---|---|---|
| Healthful Behaviors | Un-healthful Behaviors | ||||
| Independent Variable | Physical Activity at school |
Physical Activity Outside of school |
Fruit & Vegetable Intake |
Sedentary Behavior |
HCLN Food Intake |
| 5th grade behavior | 0.33 (0.04)*** | 0.39 (0.04)*** | 0.51 (0.04)*** | 0.46 (0.04)*** | 0.49 (0.04)*** |
| Demographics | |||||
| Female | −0.09 (0.08) | −0.08 (0.07) | −0.06 (0.07) | −0.17 (0.07)* | −0.14 (0.07)+ |
| Hispanic | 0.01 (0.08)+ | 0.11 (0.08) | −0.08 (0.08) | 0.22 (0.08)** | 0.07 (0.08) |
| Free Lunch | −0.01 (0.10) | −0.02 (0.09) | 0.01 (0.09) | −0.03 (0.09) | −0.14 (0.09) |
| BMI percentile | 0.0001 (0.04) | −0.04 (0.03) | 0.0003 (0.03) | 0.0004 (0.03) | −0.10 (0.04)** |
| Team sports 6th grade | 0.13 (0.04)*** | 0.35 (0.04)*** | - | −0.09 (0.03)** | - |
| Network constructs | |||||
| Nominations made | −0.61 (0.13)*** | 0.09 (0.09) | −0.15 (0.09) | −0.05 (0.06) | −0.11 (0.08) |
| Peer exposure (sum) | 0.74 (0.16)*** | −0.14 (0.12) | 0.39 (0.13)** | 0.28 (0.07)*** | 0.35 (0.10)*** |
| Interventions conditions | |||||
| Pathways | 0.21(0.08)* | 0.14 (0.07)* | 0.19 (0.09)* | −0.24 (0.07)*** | −0.03 (0.08) |
| Pathways × Peer exposure | −0.14 (0.09)+ | 0.04 (0.09) | −0.28 (0.09)** | −0.16 (0.07)* | −0.19 (0.08)* |
All non-dichotomous variables were standardized.
Random effects adjusted for 6th grade classroom
Fixed effects controlled for gender, ethnicity, socioeconomic status, 5th grade value for the dependent variable, and total nominations made (out-degree).
p<0.05 based on two-tail test
No demographic variable was associated with 6th grade outcome behaviors except that females showed lower levels of sedentary behavior compared to males (p<.05) and Hispanics showed higher levels of sedentary behavior than non-Hispanics (p<.01). Being involved in team sports was positively associated with physical activity at school (p<.001), physical activity outside of school (p<0.001) and negatively associated with sedentary behavior (p<.01). Out-degree was negatively associated with physical activity at school (b=−.61, p<.001) and z-BMI was not significant for all models except for HCLN food intake (b=−.10, p<0.01).
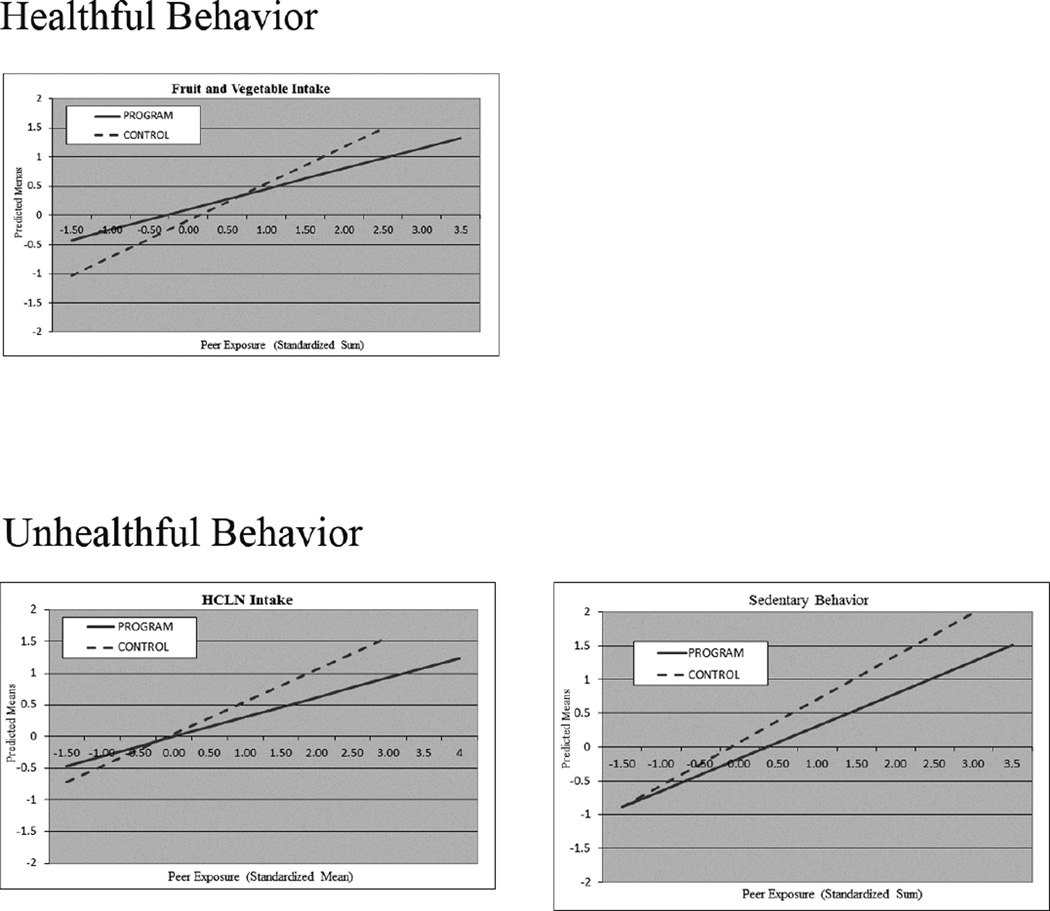
The results of the interaction between program and peer exposure showed that the effect of the intervention program was moderated by peer’s fruit and vegetable intake (b=−.28, p<.01), sedentary behavior (b=−.16, p<.05) and HCLN food intake (b=−.19, p<.05). Marginal results were observed for physical activity at school (b=−.14, p<.10). Graphs representing each significant interaction are provided. Figure 1 illustrates the differential association between the predicted means and peer exposure (standardized sum) by condition. In both control and program, peer exposure was positively associated with one’s own behavior. For healthful behavior (fruit and vegetable intake), children in the program group had higher means than the control group when healthful peers’ influence was reported less than the mean (less fruit and vegetable intake). In other words, the intervention program mitigated the detrimental influence of peer exposure when it was negative. However, for those whose peers reported high fruit and vegetable intake, being in the program condition was associated with less vegetable and fruit intake. In contrast, for those whose peers exhibited unhealthful behavior, such as high HCLN intake and sedentary behavior, being in the intervention program decreased these harmful peer influences.
Figure 1.
Predicted outcome means by average peer exposure by intervention conditions (program and control). The slope of the program condition was significantly different than the control condition for fruit and vegetable intake (p<0.01), HCLN food intake (p<0.05) and sedentary behavior (p<0.05).
Although the outcome behaviors are expected to be independently associated with risk of obesity, we additionally examined joint associations of related peer behaviors together: physical activity with sedentary behavior and fruit and vegetable intake with HCLN food intake. Table 3 shows the mixed regression models that include related peer behaviors as an additional main effect and the interaction with program for each outcome. We found that the program effects were not moderated by similar peer behaviors added. Only sedentary behavior of peers marginally moderated the program effects for physical activity at school (b=0.23, p<.10).
Table 3.
Predicting 6th grade obesity related behaviors: including related peer behaviors as an additional main effect
| Dependent variables from 6th grade | |||||
|---|---|---|---|---|---|
| Healthful Behaviors | Un-healthful Behaviors | ||||
| Independent Variable | Physical Activity at school |
Physical Activity Not at school |
Fruit & Vegetable Intake |
Sedentary Behavior |
HCLN Food Intake |
| 5th grade behavior | 0.33 (0.04)*** | 0.40 (0.04)*** | 0.51 (0.04)*** | 0.46 (0.04)*** | 0.48 (0.04)*** |
| Demographics | |||||
| Female | −0.11 (0.08) | −0.06 (0.07) | −0.06 (0.07) | −0.17 (0.07)* | −0.13 (0.07)+ |
| Hispanic | 0.02 (0.09) | 0.09 (0.08) | −0.07 (0.08) | 0.22 (0.08)** | 0.08 (0.08) |
| Free Lunch | −0.02 (0.10) | −0.03 (0.09) | 0.01 (0.09) | −0.04 (0.09) | −0.14 (0.09) |
| BMI percentile | −0.01 (0.04) | −0.04 (0.04) | −0.02 (0.04) | −0.00 (0.03) | −0.11 (0.04)** |
| Team sports 6th grade | 0.14 (0.04)*** | 0.35 (0.04)*** | - | −0.09 (0.03)** | - |
| Network constructs | |||||
| 6th Nominations made | −0.57 (0.16)*** | −0.04 (0.10) | −0.15 (0.11) | −0.00 (0.14) | −0.13 (0.12) |
| Peer 6th grade behavior (sum) | |||||
| Physical Activity at school | 0.83 (0.18)*** | −0.22 (0.18) | |||
| Physical Activity Not at School | −0.19 (0.14) | 0.19 (0.16) | |||
| Fruit and Vegetable Intake | 0.46 (0.17)** | −0.07 (0.17) | |||
| Sedentary Behavior | −0.16 (0.10) | 0.19 (0.09)* | 0.26 (0.09)** | ||
| HCLN Food Intake | −0.09 (0.14) | 0.41 (0.13)** | |||
| Interventions conditions | |||||
| Pathways | |||||
| Pathways × Peer behaviors | 0.19 (0.08)* | 0.16 (0.07)* | 0.18 (0.09)* | −0.25 (0.07)*** | −0.04 (0.08) |
| Pathways × Peer's Physical Activity at school | −0.33 (0.14)* | 0.14 (0.19) | |||
| Pathways × Peer's Physical Activity Not at School | 0.11 (0.13) | −0.16 (0.20) | |||
| Pathways × Peer's Fruit and Vegetable Intake | −0.38 (0.16)* | 0.14 (0.16) | |||
| Pathways × Peer's Sedentary Behavior | 0.23 (0.13)+ | −0.04 (0.12) | −0.16 (0.12) | ||
| Pathways × Peer's HCLN Food Intake | 0.11 (0.15) | −0.30 (0.15)* | |||
Added peer behavior was bolded in text. All non-dichotomous variables were standardized.
Random effects adjusted for 6th grade classroom.
Fixed effects controlled for gender, ethnicity, socioeconomic status, 5th grade value for the dependent variable, and total nominations made (out-degree).
p<0.05 based on two-tail test
Discussion
This article sought to fill an important gap in childhood obesity literature by identifying that the influence of children’s social networks can moderate the effectiveness of a childhood obesity program. Consistent with prior research, our findings suggested that healthful and unhealthful behaviors can be reinforced by peer influence.19, 34 All obesity related behaviors were positively associated with more exposure to negative/positive peer behavior, which supports social facilitation that occurs among peers. Peer influence was measured from friends’ self-reports providing a more objective than perceived peer behavior.35 While demonstrating positive intervention effects, it appeared that the prevention program can be moderated by peer influence even at younger ages.19 Results of this study emphasize policy implications for childhood obesity interventions to consider the influence of social networks.6
In terms of the interaction between the Pathways program and peer exposure, results indicated that Pathways provides a buffer for children from the effect of negative peer influence. Figure 1 shows that the program effect differs by behavior type. For fruit and vegetable intake, Pathways students with friends who engaged in unhealthful actions were less influenced by their peers to engage in unhealthful behaviors than control students. For example, Pathways students were eating more fruits and vegetables, even when their friends were eating much fewer fruits and vegetables. Thus, Pathways mitigated these potential negative peer influences. However, when peers were already engaging in healthful behavior, the program effect disappeared. This may indicate that adverse peer influences have to be present for the program to be effective. For unhealthful behaviors, Pathways students with friends who engage in negative actions (i.e., doing more of the unhealthful behavior) were less influenced by their peers than control students to engage in negative actions. Although previous research has shown that peers can influence behaviors both in a positive or negative direction,34 this is the first study to provide evidence that peers can also exert positive or negative influence on prevention efforts. In addition, we examined the interaction between the Pathways program with both unhealthy and healthy peer exposure as main effects in the model (i.e., physical activity and sedentary behavior). There were no significant program interaction with the added peer exposures in the models, but future studies can further investigate how the combinations of multiple behaviors may contribute to obesity risk.
Results may also imply that Pathways sets a healthy norm among students for social modeling and impression management. Since the slopes for the control group are steeper than the program group, it may be possible that the Pathways program is shifting the social norm among the students and homogenizing their health behaviors. As all program students receive the same amount of information delivered through the intervention, the differences in health behavior across “cliques” (i.e., peer groups) may have been reduced. Thus, the impact of peers in the program group may be weaker than the control group. It might be important for future studies to consider peer-led interventions to promote greater positive influence of peers on healthful and un-healthful behaviors.
One thing to note is that the interaction between program intervention and peer exposure was not significant for physical activity at school and outside of school. For physical activity at school, a possible explanation for the weaker program effect could be that students are not engaging much in physical activities with peers at school, including recess.36 For physical activity outside of school, there are few known explanations for these findings. First, peer influence may not be significant outside of school when peers are most likely not present.37 Second, as the majority of students included in this study were low SES, the environment to play outside of school with peers could be restrictive because of safety concerns.38 Future prevention studies may look into different friendships that exist out of school to explore peer influence more completely.
These results suggest that this obesity-prevention program may provide a buffer against unhealthful peer influence. One of the moderator Pathways targets is the executive cognitive function (ECF) which involves goal-directed behavior and emotional control.30 Previous literature has linked ECF with food intake and substance use,30 but its relation to peer influence is not yet known. Just as it operates in food or substance-use decisions, ECF may inhibit unhealthful peer influence by enhancing better decision-making power. Future studies can investigate how ECF operates with negative peer influence on making decisions related to risk factors for obesity, such as HCLN food intake and sedentary behavior and their relation to change in social network positions.
Several limitations of the present study should be noted. First, study data were generated from children’s self-report surveys. Thus, threats to validity related to self-report data cannot be discounted. Second, due to the large number of Hispanic students residing in a low SES urban setting, the current study may not be representative of the broader population. Future studies may consider conducting the study on a more heterogeneous sample. A third possible limitation is discrepancies of group characteristics between the analytic sample and the participants excluded because of missing nomination data. If a nominated friend did not participate in the study, there were no available measures for the student, thus that individual is not included in the peer exposure calculation. The analytic may include children with a greater propensity for being healthy (i.e., higher SES, non-Hispanic, higher physical activity, less HCLN intake and less sedentary) than the general adolescent population. Results are generalizable only to similar samples of youth. Lastly, change of peer influence was not measured. As classroom networks were only assessed once during an academic year, it was not possible to analyze change in social network. Thus, causal inferences (e.g., selection vs. homophily) regarding the peer network cannot be determined.39
Despite these limitations, the study contributes to the current literature by exploring the role of peer influence in childhood-obesity prevention. The increasing rate of childhood obesity demands an effective prevention program especially implemented at school where children spend most time away from home. While highlighting the importance of peer influence in young children for obesity-related behaviors, this study is among the first to examine the relationship between peer influence and program intervention in children. Given the strong role played by peers in health behavior, interventions should consider the opportunities to intervene simultaneously with children and their peers.
‘What is known about this subject?’.
Schools have been identified as an important context for the implementation of obesity prevention programs
Peers have been identified as a primary social influence on children’s development
However, influence of peer behavior has not been examined as a potential moderator of school-based obesity prevention program
‘What this study adds’
Using social network analysis, peer influence was measured from surveys of the nominated friends for more objectivity than perceived reports on friends.
Result of this study supported the hypothesis that the effect of school-based child obesity prevention will attenuate unhealthful peer influence and accentuate healthful peer influence for healthier behavioral outcome.
Also, this study supported the hypothesis that children are influenced by their peers even at younger ages, as most studies have been focused on adolescents.
Acknowledgments
This work was supported by the National Institute of Health grant R01HD052107-0182 (PI: M.P.) and T32CA09492 (PI: M.P.).
Footnotes
Conflicts of Interest Statement
This article contains no conflicts of interest to declare.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA: the journal of the American Medical Association. 2012;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spruijt-Metz D. Etiology, treatment, and prevention of obesity in childhood and adolescence: A decade in review. J Res Adolesc. 2011;21(1):129–152. doi: 10.1111/j.1532-7795.2010.00719.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pan L, Blanck HM, Sherry B, Dalenius K, Grummer-Strawn LM. Trends in the prevalence of extreme obesity among US preschool-aged children living in low-income families, 1998–2010. JAMA. 2012;308(24):2563–2565. doi: 10.1001/jama.2012.108099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Biro FM, Wien M. Childhood obesity and adult morbidities. Am J Clin Nutr. 2010;91(5):1499S–1505S. doi: 10.3945/ajcn.2010.28701B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hiltje OL, Louise B, Hanneke J, et al. Interventions for treating obesity in children. Cochrane database of systematic reviews. 2009 doi: 10.1002/14651858.CD001872.pub2. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD001872pub2/abstract. [DOI] [PubMed] [Google Scholar]
- 6.Dietz WH, Gortmaker SL. Preventing obesity in children and adolescents. Annu Rev Public Health. 2001;22:337–353. doi: 10.1146/annurev.publhealth.22.1.337. [DOI] [PubMed] [Google Scholar]
- 7.Dobbins M, De Corby K, Robeson P, Husson H, Tirilis D. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6–18. Cochrane Database Syst Rev. 2009;(1) doi: 10.1002/14651858.CD007651. CD007651. http://europepmc.org/abstract/MED/19160341. [DOI] [PubMed] [Google Scholar]
- 8.Story M, Kaphingst KM, French S. The role of schools in obesity prevention. The Future of Children. 2006;16(1):109–142. doi: 10.1353/foc.2006.0007. [DOI] [PubMed] [Google Scholar]
- 9.Duncan SC, Duncan TE, Strycker LA. Sources and types of social support in youth physical activity. Health Psychology. 2005;24(1):3–10. doi: 10.1037/0278-6133.24.1.3. [DOI] [PubMed] [Google Scholar]
- 10.Koehly LM, Loscalzo A. Peer reviewed: Adolescent obesity and social networks. Preventing chronic disease. 2009;6(3) [PMC free article] [PubMed] [Google Scholar]
- 11.Valente TW, Fujimoto K, Chou C, Spruijt-Metz D. Adolescent affiliations and adiposity: A social network analysis of friendships and obesity. Journal of Adolescent Health. 2009;45(2):202–204. doi: 10.1016/j.jadohealth.2009.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379. doi: 10.1056/NEJMsa066082. http://dx.doi.org/10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 13.Cottrell NB, Wack DL, Sekerak GJ, Rittle RH. Social facilitation of dominant responses by the presence of an audience and the mere presence of others. J Pers Soc Psychol. 1968;9(3):245–250. doi: 10.1037/h0025902. [DOI] [PubMed] [Google Scholar]
- 14.Salvy S, De La Haye K, Bowker JC, Hermans RC. Influence of peers and friends on children's and adolescents’ eating and activity behaviors. Physiol Behav. 2012 doi: 10.1016/j.physbeh.2012.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bandura A. Social learning theory. Vol. 247. Oxford, England: Prentice-Hall; 1977. [Google Scholar]
- 16.Efrat MW. The relationship between peer and/or friends’ influence and physical activity among elementary school children: A review. Californian Journal of Health Promotion. 2009;7:48–61. (Special Issue) [Google Scholar]
- 17.Romero ND, Epstein LH, Salvy S. Peer modeling influences girls' snack intake. J Am Diet Assoc. 2009;109(1):133–136. doi: 10.1016/j.jada.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Unger JB, Reynolds K, Shakib S, Spruijt-Metz D, Sun P, Johnson CA. Acculturation, physical activity, and fast-food consumption among asian-american and hispanic adolescents. J Community Health. 2004;29(6):467–481. doi: 10.1007/s10900-004-3395-3. [DOI] [PubMed] [Google Scholar]
- 19.de la Haye K, Robins G, Mohr P, Wilson C. Obesity-related behaviors in adolescent friendship networks. Social Networks. 2010;32(3):161–167. [Google Scholar]
- 20.Ommundsen Y, Gundersen KA, Mjaavatn PE. Fourth graders' social standing with peers: A prospective study on the role of first grade physical activity, weight status, and motor proficiency. Scandinavian Journal of Educational Research. 2010;54(4):377–394. [Google Scholar]
- 21.Valente TW. Social networks and health: Models, methods, and applications: Models, methods, and applications. USA: Oxford University Press; 2010. [Google Scholar]
- 22.Sakuma KK, Riggs NR, Pentz MA. Translating evidence based violence and drug use prevention to obesity prevention: Development and construction of the pathways program. Health Education Research. 2012;27(2):343–358. doi: 10.1093/her/cyr095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pentz M, Riggs N. Longitudinal relationships of executive cognitive function and parent influence to child substance use and physical activity. Prevention Science. 2013;14(3):229–237. doi: 10.1007/s11121-012-0312-3. http://dx.doi.org/10.1007/s11121-012-0312-3. [DOI] [PubMed] [Google Scholar]
- 24.Field AE, Peterson KE, Gortmaker SL, et al. Reproducibility and validity of a food frequency questionnaire among fourth to seventh grade inner-city school children: Implications of age and day-to-day variation in dietary intake. Public Health Nutr. 1999;2(03):293. doi: 10.1017/s1368980099000397. http://dx.doi.org/10.1017/S1368980099000397. [DOI] [PubMed] [Google Scholar]
- 25.Crocker P, Bailey DA, Faulkner RA, Kowalski KC, McGRATH R. Measuring general levels of physical activity: Preliminary evidence for the physical activity questionnaire for older children. Med Sci Sports Exerc. 1997;29(10):1344. doi: 10.1097/00005768-199710000-00011. [DOI] [PubMed] [Google Scholar]
- 26.Riggs NR, Spruijt-Metz D, Sakuma K, Chou C, Pentz MA. Executive cognitive function and food intake in children. Journal of Nutrition Education and Behavior. 2010;42(6):398–403. doi: 10.1016/j.jneb.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance?united states, 2005. J Sch Health. 2006;76(7):353–372. doi: 10.1111/j.1746-1561.2006.00127.x. [DOI] [PubMed] [Google Scholar]
- 28.Willett WC, Sampson L, Stampfer MJ, et al. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol. 1985;122(1):51–65. doi: 10.1093/oxfordjournals.aje.a114086. [DOI] [PubMed] [Google Scholar]
- 29.Hoelscher DM, Day RS, Kelder SH, Ward JL. Reproducibility and validity of the secondary level school-based nutrition monitoring student questionnaire. J Am Diet Assoc. 2003;103(2):186–194. doi: 10.1053/jada.2003.50031. [DOI] [PubMed] [Google Scholar]
- 30.Burt RS. Network items and the general social survey. Social networks. 1984;6(4):293–339. [Google Scholar]
- 31.Marsden PV. Recent developments in network measurement. Models and methods in social network analysis. 2005;8:30. [Google Scholar]
- 32.SAS Institute Inc. SAS OnlineDoc 9.1. 3. 2004 [Google Scholar]
- 33.Butts CT. The SNA package for R. [Accessed 11/1, 2012]; http://erzuli.ss.uci.edu/R.stuff/. Updated 2012. [Google Scholar]
- 34.Sirard JR, Bruening M, Wall MM, Eisenberg ME, Kim SK, Neumark-Sztainer D. Physical activity and screen time in adolescents and their friends. Am J Prev Med. 2013;44(1):48–55. doi: 10.1016/j.amepre.2012.09.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Valente TW, Fujimoto K, Soto D, Ritt-Olson A, Unger JB. A comparison of peer influence measures as predictors of smoking among predominately Hispanic/Latino high school adolescents. Journal of Adolescent Health. 2012 doi: 10.1016/j.jadohealth.2012.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McKenzie TL, Marshall SJ, Sallis JF, Conway TL. Leisure-time physical activity in school environments: An observational study using SOPLAY. Prev Med. 2000;30(1):70–77. doi: 10.1006/pmed.1999.0591. [DOI] [PubMed] [Google Scholar]
- 37.Jago R, MacDonal-Wallis K, Thompson JL, Page AS, Brockman R, Kenneth F. Better with a buddy: Influence of best friends on children's physical activity. Medicine & Science in Sports & Exercise. 2011;43(2):259–265. doi: 10.1249/MSS.0b013e3181edefaa. [DOI] [PubMed] [Google Scholar]
- 38.Sallis JF, McKenzie TL, Alcaraz JE, Kolody B, Faucette N, Hovell MF. The effects of a 2-year physical education program (SPARK) on physical activity and fitness in elementary school students. sports, play and active recreation for kids. Am J Public Health. 1997;87(8):1328–1334. doi: 10.2105/ajph.87.8.1328. http://dx.doi.org/10.2105/AJPH.87.8.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.de la Haye K, Robins G, Mohr P, Wilson C. Homophily and contagion as explanations for weight similarities among adolescent friends. Journal of Adolescent Health. 2011;49(4):421–427. doi: 10.1016/j.jadohealth.2011.02.008. [DOI] [PubMed] [Google Scholar]