Abstract
Social support has been shown to act as a buffer for cardiovascular responses to stress. However, little is known about how social support and networks are related to cardiovascular responses to immigration stress recall. The current study evaluated the impact of structural and functional support on cardiovascular reaction following immigrant stress recall provocation as well as the moderation effect of interdependent self-construal among first-generation Chinese immigrants. One hundred fifty Chinese immigrants were recruited in the New York Chinatown area. Participants completed questionnaires assessing their levels of social support and networks, and interdependent self-construal. Following adaptation, participants recalled a recent post-immigration stress-provoking situation. Cardiovascular measures were taken during adaptation, stressor task, and recovery period. Hierarchical multiple regression analysis was performed. Social network size and type, as well as perceived emotional support were positively predictive of systolic blood pressure (SBP) reactivity changes. Instrumental support seeking was a positive predictor of SBP and diastolic blood pressure (DBP) reactivity. The moderation effect between instrumental support seeking and interdependent self-construal were significantly predictive of DBP reactivity and recovery, suggesting that perceptions about themselves in relation to others is a crucial factor for determining whether support seeking is beneficial or not. Social support was not a direct buffer on cardiovascular responses to stress among Chinese immigrants. Chinese values of interdependence and collectivism may partly explain the disconfirming results. Still, when interdependent self-construal was taken into account, Chinese immigrants who had less interdependent self-construal, but solicited more instrumental support, had faster adaptation to stress over the long term.
Keywords: Social network, Social support, Cardiovascular health, Immigrants
Background
According to the United States Census Bureau [1], Chinese Americans made up approximately 3.35 million of the population, with 1.9 million (56.7 %) reporting being foreign-born—the second largest immigrant population in the country. The New York City metropolitan area has an estimated 695,000 Chinese Americans, constituting one of the largest Chinese populations in the United States and the second largest foreign-born group in New York City.
Immigrants commonly experience post-immigration adjustment and acculturative stress during their process of adapting to a new country and culture [2]. In the course of adapting to new environments and social norms, immigrants often experience intense stress and various kinds of stressors such as language barriers, stress relating to immigration logistics, and adjustment issues related to adapting to new values and customs as well as the identity of being an immigrant [3]. Strong evidence has shown the harmful impact of chronic stress on bodily functions such as the cardiovascular system [4]. Among Chinese immigrants, studies have found that mortality rates related to coronary heart disease and hemorrhagic stroke were significantly higher among Chinese immigrants in the United States than Chinese nationals [5–7]. It is possible that changes in lifestyle and exposure to chronic stress related to immigration adaptation and acculturation contribute to their vulnerability for developing cardiovascular disease (CVD) [8, 9].
Besides epidemiological studies, the impact of chronic stress on the cardiovascular system can be measured via two methods: cardiovascular reactivity (CVR) to stress and cardiovascular recovery from stress. CVR to stress examines elevation in heart rate (HR) and blood pressure (BP) to stress while cardiovascular recovery from stress focuses on the return rate of HR and BP back to pre-stress levels. Exaggeration in both measures has been found to be associated with an increased future risk for developing CVD [10, 11]. Specific to the Asian and Asian American populations, results from comparative studies have mainly suggested that either Chinese nationals had less CVR to stress than other Asian groups or Asian Americans had lower CVR to stress relative to European Americans [12–14]. Besides our recent study [15], there have been no other studies relating to CVR to stress among Chinese immigrants.
In relation to the impact of stress on the cardiovascular system, high level of social support has been shown to act as a buffer for the adverse impact of stress on cardiovascular functions [16, 17]. Social support, which is a complex and multidimensional construct [4], consists of structural and functional dimensions [18, 19]. Structural support, also known as social network, focuses on the quantitative and objective aspects of social relationships such as size and type [20, 21]. Functional support measures both cognitive (perceived availability of support) and behavioral (social support seeking) aspects of social relationships. Studies using experimental manipulation of social support to laboratory stressors or naturalistic assessment of social support have indicated the benefits of high levels of social support on CVR to stress [22, 23]. However, it is unclear whether similar findings may be replicated among Chinese immigrants.
Post-immigration and acculturation experiences have been shown to change the use of social support among Chinese immigrants [24]. For instance, older Chinese immigrants may seek less support from their westernized children in order to reduce conflicts which were very contrary to Chinese values of filial responsibilities, younger generation should look after their older parents [24]. One way to measure individuals’ acculturation level is to understand the extent in which they identify themselves as upholding more individualistic or collectivistic cultures [25]. Individuals who value Chinese cultures tend to have a strong interdependent self-construal, meaning they value collective goals and view the self as interdependent with others [26]. Conversely, those who uphold American cultures tend to have a low level of interdependent self-construal as they focus more on personal values and view the self as independent from others [27]. It is probable that those who uphold a greater interdependent self-construal are less willing to seek support due to the fear of burdening their in-groups (family and friends) and the importance of maintaining a harmonious relationship with them [28, 29]. Cross-cultural studies have shown that Asians and/or Asian Americans tend to seek less support than European Americans, and seeking support can be a more stressful experience for Asians and/or Asian Americans than European Americans, as indicated by their increased production of cortisol [30–32]. Thus, it is possible that Chinese immigrants who have strong interdependent self construal will be less likely to seek support to cope with stress than those who are more acculturated to western culture.
The present study assessed the cross-cultural applicability of the social support stress buffering model on cardiovascular responses to stress provocation, and investigated whether interdependent self-construal moderated the impact of Chinese immigrants’ social support seeking and their cardiovascular reactions to stress. We hypothesized that (1) larger social network, (2) stronger perceived availability of emotional or instrumental support, and (3) seeking more emotional or instrumental support would predict lower HR, systolic blood pressure (SBP), and diastolic blood pressure (DBP) to stress during baseline, during the course of the interview, and during recovery from provocation, compared to those who received less structural and functional support among Chinese immigrants. We also hypothesized that those who were less likely to uphold their Chinese interdependent cultures would be more likely to seek emotional or instrumental support, and had lower cardiovascular responses to stress during baseline, interview, and relaxation from provocation than others.
Methods
Participants
Participants in this study were recruited from a larger study focusing on medical and psychosocial factors, and cardiovascular health among Chinese immigrants at a hospital in the New York Chinatown area. They were originally recruited from senior citizen centers, community organizations, and the hospital community program. Once they completed the larger study, they were contacted through phone or in-person regarding their interest in participating in this study. They were eligible for this study if they are Chinese and were born in a foreign country. They were excluded if they had difficulty completing the questionnaire, verbally reported that they had a history of serious mental illness, or had a debilitating illness that impacted their ability to participate in the study.
One hundred fifty Chinese immigrants ages 21–87 years old (M = 53.3, SD = 17.40) enrolled and participated in the study. The average length of time of living in the United States was 20 years. Three subjects refused to participate in the stressor task and no cardiovascular measures were obtained for them. One participant was later found not to have participated in the larger study and, thus, no medical information (e.g., body mass index (BMI), waist circumference, medical history) was collected for that individual. Table 1 provides detailed demographic information about this sample.
Table 1.
Sample characteristics (N = 150)
| N | % | N | % | ||
|---|---|---|---|---|---|
| Gender | Annual household income | ||||
| Male | 64 | 42.7 | 0–9,999 | 44 | 29.3 |
| Female | 86 | 57.3 | 10,000–19,999 | 42 | 28 |
| Marital status | 20,000–29,999 | 31 | 20.7 | ||
| Currently married | 96 | 64 | 30,000–49,999 | 11 | 7.3 |
| Never married | 24 | 16 | 50,000 or above | 20 | 13.3 |
| Separated | 5 | 3.3 | Not stated | 2 | 1.4 |
| Divorce | 7 | 4.7 | BMI (kg/m2) | ||
| Widow | 18 | 12 | <18.5 | 7 | 4.6 |
| Preferences of language spoken | 18.5–24.9 | 94 | 62.7 | ||
| Chinese only | 120 | 80 | 25–29.9 | 40 | 26.7 |
| English only | 1 | .7 | >30 | 8 | 5.3 |
| Both | 29 | 19.3 | Missing | 1 | .7 |
| Level of education | Waist circumferences (inches) | ||||
| No school | 3 | 2 | Male >40 | 6 | 9.4 |
| Elementary school | 29 | 19.3 | <40 | 57 | 89 |
| High school | 69 | 46 | Missing | 1 | 1.6 |
| College or above | 48 | 32 | Female >35 | 2 | 33.7 |
| Missing | 1 | .7 | <35 | 57 | 66.3 |
| Employment status | Hypertension | ||||
| Employed | 67 | 44.7 | Yes | 45 | 30 |
| Unemployed | 13 | 8.7 | No | 104 | 69.3 |
| Retired | 49 | 32.6 | Missing | 1 | .7 |
| Housewife | 18 | 12 | Heart problem | ||
| Not stated | 3 | 2 | Yes | 14 | 9.3 |
| Status of smoking | No | 135 | 90 | ||
| Yes | 14 | 9.3 | Missing | 1 | .7 |
| No | 135 | 90 | |||
| Missing | 1 | .7 | |||
Data Collection
Bilingual trained study personnel provided participants with a written consent form and verbal information about the study. If they agreed to participate and fulfilled the eligibility for the study, they were then asked to complete a questionnaire that measured their levels of social support, social networks, and acculturation. Social support was measured by both instrumental and emotional support because they have been found to be the two most important types of functional support [33].
Demographic data were also obtained, except for the following items which were collected from the larger study: weight, waist circumference, BMI, medical history, educational level, employment status, and annual household income. Following the completion of the questionnaire, a blood pressure cuff was placed on participants’ non-dominant arm. Four HR, SBP, and DBP readings were obtained every 2 min during the baseline period. Participants were instructed to sit quietly during that time. Following an 8-min resting period, a trained bilingual Chinese interviewer used the 8-min Social Competence Interview to guide participants to recall a stressful situation that had occurred within the past 6 months and was associated with their post-immigration experience. During the interview, the participants’ cardiovascular measures were taken at 1-min intervals. Eight readings were obtained during that time. Once the interview was completed, the recovery period was monitored for 20 min at 2-min intervals and a total of ten cardiovascular measures were taken at that time.
Since a majority of the participants were Chinese-speaking, the questionnaire was translated into Chinese. The questionnaire was first translated to Chinese and then back-translated into English. The new version was compared with the original English version to ensure accuracy. If discrepancies were indicated, they were resolved through discussion. Participants decided on their own whether they preferred to use the Chinese or English version of the questionnaire. In total, there were only 7 subjects (4.67 %) who utilized English to complete the study. Both the study personnel and interviewer were trained and bilingual.
Measures
Social Network Index (SNI) [34]
The SNI measures 12 kinds of social relationships (e.g., spouse, parents, neighbors, friends, colleagues from work, etc.). Social Network Type measures the kinds of social networks that individuals contact either in person or by phone at least once every 2 weeks. Social Network Number assesses the total number of people that individuals have contact with at least once every 2 weeks. This index has never been used for a Chinese population and no study to date has assessed its reliability or validity, even in the general population.
Interpersonal Support Evaluation List—Emotional Support and Instrumental Support Subscales (ISEL) [35]
These ISEL subscales measure perceived availability of emotional and instrumental support. It is a 5-point Likert scale, with a higher score suggesting higher levels of perceived emotional and/or instrumental support. These subscales were found to have a coefficient alpha range from .70 to .90 [36]. The measure has been previously utilized on a Chinese population and a Cronbach’s alpha coefficient ranged from .93 to .97 [37].
Coping Orientations to Problems Experienced Scale—Seeking Social Support—Instrumental and Seeking Social Support—Emotional Subscales (COPE) [38]
These COPE subscales measure emotional and instrumental support seeking on a 4-point Likert scale. Alpha reliabilities of both subscales are above .6 [38]. While the abbreviated version of COPE has been utilized with Asian Americans [30], it has not been used on a Chinese population. Overall, COPE has good convergent and discriminant validity [39].
Self-Construal Scale—Interdependent Subscale (SCS) [40]
This SCS subscale was utilized to measure individuals’ perception of themselves in relation to others, specifically assessing the extent to which individuals identify the self as interdependent and collectivistic. This subscale has a Cronbach’s alpha reliability coefficient of .74. It is a 7-point Likert scale, with higher scores indicating greater interdependent values. Studies focusing on Chinese populations have utilized this measure and a Cronbach’s alpha of .73 was indicated [40, 41].
Heart Rate and Blood Pressure (SBP and DBP)
Cardiovascular measures were taken in participants’ non-dominant arm through the OMRON HEM-780 Automatic Blood Pressure Monitor (OMRON Healthcare, Inc., Bannockburn, IL). This device uses the oscillometric method to measure blood pressure. The accuracy of the readings is ±3 mm Hg or 2 % of reading.
Social Competence Interview (SCI) [42–44]
This semi-structured interview was designed to obtain participants’ cardiovascular measures while they discussed a stressful personal situation occurring within the past 6 months. For the purpose of this study, the original SCI was modified so that it would be more applicable for the Chinese immigrant population. Participants are given nine cards (original version only consists of six cards). Each card lists a specific problem that participants might experience (i.e., problems related to family, friends, work, school, money, health, society, neighborhood, and others). The interview then focuses only on the most stressful topic that the participants chose. This study will not focus on the content of the interviews.
Analysis
The study measures three cardiovascular parameters: HR, SBP, and DBP. Baseline data were calculated by averaging the four measures that were obtained during the adaptation period. Raw change score method (i.e., the difference between the mean raw value of the interview and the mean of baseline raw measures) was utilized to calculate HR, SBP, and DBP reactivity scores. This is a valid method to assess CVR to stress [45]. Excursion was used to measure the difference between area under the recovery curve and the average baseline value for each cardiovascular parameter. The following formula was utilized to calculate recovery with fixed time interval being 120 s: Excursion = .5 * fixed time interval [(cardiovascular measure at recovery time 1) + (2 * cardiovascular measure at recovery time 2) + (2 * cardiovascular measure at recovery time 3) + ⋯ + (cardiovascular measure at recovery time 10) − (baseline cardiovascular measure * fixed time interval)]. This formula was adapted from Neumann and her colleagues [46].
SPSS 14.0 graduate student statistical package was utilized to analyze the data. Descriptive statistics on results from self-report and medical measures were computed (see Table 2). Separated hierarchical multiple regression analyses were conducted to examine whether larger structural and/or functional support would be predictive of lower HR, SBP, and DBP, during baseline, reactivity, and recovery. Preliminary analysis was computed with results indicating a significant association between age, waist circumference, gender, and history of hypertension with cardiovascular measures. Thus, they were entered as the first step of the regression equation as covariates. Then, each social network and social support measure was added separately to explore their predictions on HR, SBP, and DBP at baseline, reactivity, and recovery.
Table 2.
Descriptive statistics of participants’ levels of social support and cardiovascular measures (N = 150)
| Participants characteristics | M ± SD | Range |
|---|---|---|
| Social network types | 5.13 ± 1.95 | 0–10 |
| Social network sizes | 14.36 ± 8.72 | 0–63 |
| Perceived emotional support | 24.05 ± 6.24 | 5–30 |
| Perceived instrumental support | 22.11 ± 6.83 | 0–30 |
| Emotional support seeking | 2.79 ± .86 | 1–4 |
| Instrumental support seeking | 3.06 ± .76 | 1–4 |
| Cardiovascular parameters | ||
| Baseline HR | 72.83 ± 10.60 | 52–123.50 |
| Baseline SBP | 116.99 ± 16.64 | 88.50–178.25 |
| Baseline DBP | 72.16 ± 10.04 | 50.75–104.13 |
| HR reactivity | 76.78 ± 11.75 | 53.88–127.00 |
| SBP reactivity | 128.99 ± 17.88 | 90.50–183.38 |
| DBP reactivity | 81.57 ± 11.49 | 54.50–117.00 |
| HR recovery | 71.22 ± 9.57 | 52.50–108.90 |
| SBP recovery | 116.78 ± 16.73 | 84.60–183.80 |
| DBP recovery | 72.41 ± 9.98 | 51.00–106.60 |
Finally, the moderation effect between emotional or instrumental support seeking and interdependent self-construal on HR, SBP, and DBP at baseline, reactivity, and recovery were conducted. In each analysis, covariates were entered into the model as a first step. The centered main effect terms (emotional or instrumental support seeking and interdependent self-construal) were entered next. The centered cross product terms (emotional or instrumental support seeking × interdependent self-construal) were entered last. Main effect terms were then divided into three groups based on the mean and ±1 standard deviation from the mean. The results were then graphed to examine the interaction effect [47].
This study obtained approval from the Albert Einstein College of Medicine Institutional Review Board.
Results
Social Network Type and Its Prediction of Cardiovascular Measures
Participants reported having contact with five types of social relationships at least once every 2 weeks. Larger social network type was associated with larger SBP reactivity changes (β = .85, R2 = .16, p < .05). No significant results were found between social network type and cardiovascular measures at baseline and recovery.
Social Network Size and Its Prediction of Cardiovascular Measures
Participants indicated that they contacted an average of 14 people at least once every 2 weeks. Having a larger social network size was predictive of larger SBP reactivity changes (β = .21, R2 = .17, p < .03). No significant result was indicated between social network size and cardiovascular measures during baseline and recovery.
Perceived Emotional Support and Its Association with Cardiovascular Measures
On average participants reported perceiving themselves having a moderate level of emotional support. A higher level of perceived emotional support was associated with an increase in SBP reactivity to stress (β = .34, R2 = .17, p < .02). There was no significant prediction between perceived emotional support and cardiovascular measures at other time points.
Perceived Instrumental Support and Its Association with Cardiovascular Measures
Participants reported perceiving themselves as having a moderate level of instrumental support. Perceived instrumental support was not a significant predictor of any cardiovascular parameters.
Emotional Support Seeking and Its Association with Cardiovascular Measures
Participants reported seeking a moderate amount of emotional support as needed. Seeking emotional support was not predictive of any cardiovascular measures.
Instrumental Support Seeking and Its Association with Cardiovascular Measures
Participants indicated seeking a medium level of instrumental support. Instrumental support seeking was significant in predicting SBP (β = 2.52, R2 = .17, p < .03) and DBP (β = 1.86, R2 = .14, p < .02) reactivity changes. There was no significant association between instrumental support seeking and any other cardiovascular measures.
Moderation Effects of Social Support Seeking and Interdependent Self-Construal on Cardiovascular Measures
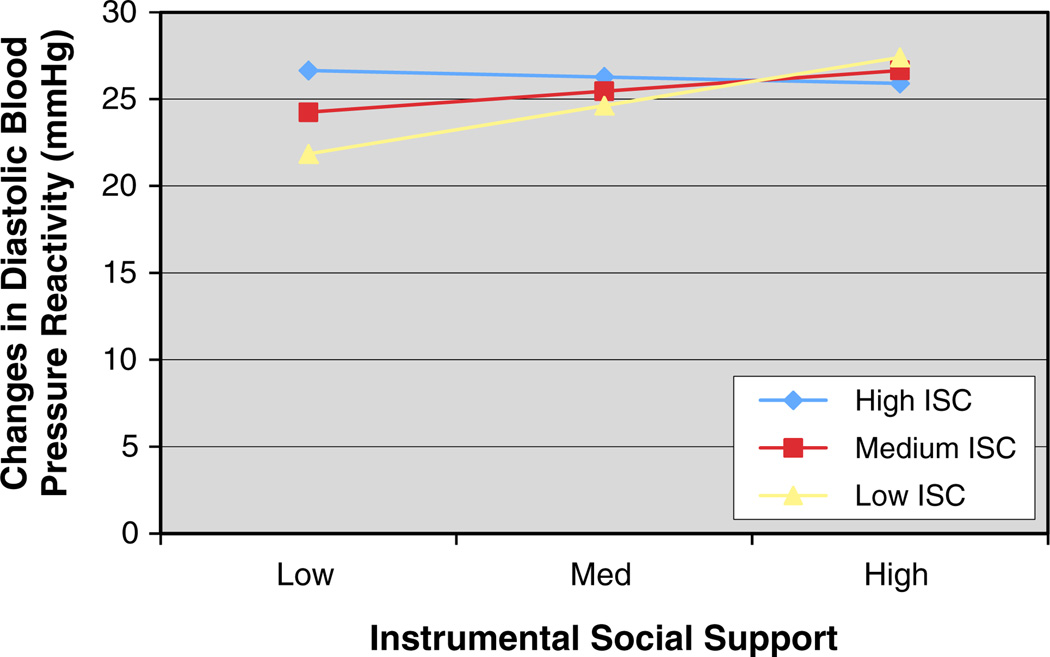
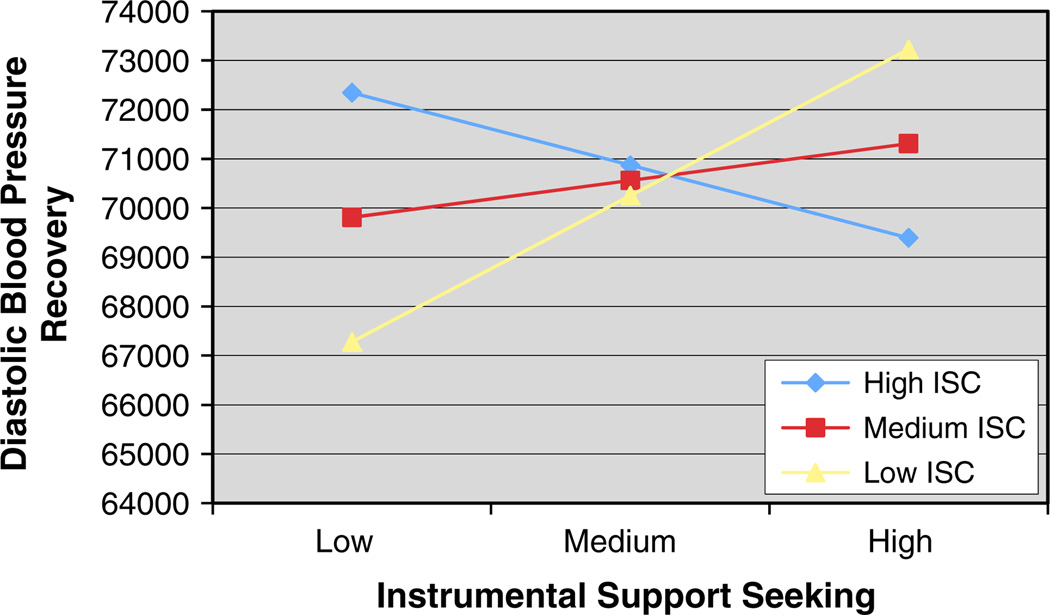
The interactions between instrumental support seeking and interdependent self-construal on DBP reactivity (β = −2.48, R2 = .18, p < .009) and recovery (β = −3,501.18, R2 = .09, p < .02) were significant as illustrated in Tables 3 and 4 as well as Figs. 1 and 2. Based on the results from the interaction of instrumental support seeking and interdependent self-construal on DBP reactivity and recovery, those who solicited a low level of instrumental support, but upheld less interdependent self-construal (i.e., less acculturated) were predicted to have less DBP reactivity and faster DBP recovery than other groups. Those who solicited less instrumental support and upheld a high level of interdependent self-construal were predictive of greater DBP reactivity and slower DBP recovery. Those who solicited more instrumental support and upheld less interdependent self-construal were associated with greater DBP reactivity and slower DBP recovery. Finally, those who solicited a high level of instrumental support, but reported upholding more interdependent self-construal was predicted to have slightly greater DBP reactivity, but faster recovery than other groups.
Table 3.
Summary of hierarchical regression analysis predicting diastolic blood pressure reactivity change from instrumental support seeking and interdependent self-construal (N = 150)
| Variable | B | SE | β | R2 | ΔR2 |
|---|---|---|---|---|---|
| Dependent variable: DBP reactivity change | |||||
| Step 1 | .10** | ||||
| Age | .01 | .04 | .02 | ||
| Waist circumferences | −.31 | .16 | −.18 | ||
| Gender | 3.05 | 1.21 | .22* | ||
| History or hypertension | 1.17 | 1.44 | .08 | ||
| Baseline DBP | −.03 | .06 | −.04 | ||
| Step 2 | .14** | ||||
| Age | −.01 | .04 | −.03 | ||
| Waist circumferences | −.36 | .16 | −.21* | ||
| Gender | 2.01 | 1.25 | .14 | ||
| History of hypertension | 1.88 | 1.44 | .13 | ||
| Baseline DBP | −.03 | .06 | −.05 | ||
| Centered ISC | .81 | .81 | .10 | ||
| Centered ISS | 1.59 | .79 | .18* | ||
| Step 3 | .18*** | .04** | |||
| Age | −.03 | .04 | −.07 | ||
| Waist circumferences | −.38 | .15 | −.21* | ||
| Gender | 2.17 | 1.23 | .16 | ||
| History of hypertension | 2.53 | 1.43 | .17 | ||
| Baseline DBP | −.06 | .06 | −.08 | ||
| Centered ISC | .98 | .79 | .12 | ||
| Centered ISS | −1.58 | .77 | −.18* | ||
| ISC × ISS | −2.48 | .92 | −.22** | ||
ISC interdependent self-construal, ISS instrumental support seeking
p < .05;
p < .01;
p < .001
Table 4.
Summary of hierarchical regression analysis predicting diastolic blood pressure recovery from instrumental support seeking and interdependent self-construal (N = 150)
| Variable | B | SE | β | R2 | ΔR2 |
|---|---|---|---|---|---|
| Dependent variable: DBP recovery | |||||
| Step 1 | .04 | ||||
| Age | −47.70 | 56.71 | −.08 | ||
| Waist circumferences | 154.81 | 225.69 | .06 | ||
| Gender | −2,090.43 | 1,747.37 | −.11 | ||
| History of hypertension | 2,383.13 | 2,095.20 | .11 | ||
| Step 2 | .05 | .01 | |||
| Age | −48.75 | 64.98 | −.08 | ||
| Waist circumferences | 134.54 | 230.31 | .05 | ||
| Gender | −2,582.74 | 1,850.79 | −.13 | ||
| History of hypertension | 2,705.57 | 2,144.16 | .13 | ||
| Centered ISC | 100.10 | 1,209.10 | .01 | ||
| Centered ISS | 1,022.79 | 1,178.98 | .08 | ||
| Step 3 | .09 | .04* | |||
| Age | −70.63 | 64.25 | −.12 | ||
| Waist circumferences | 108.39 | 225.96 | .04 | ||
| Gender | −2,256.65 | 1,818.39 | −.11 | ||
| History of hypertension | 3,557.03 | 2,127.29 | .17 | ||
| Centered ISC | 361.40 | 1,189.38 | .03 | ||
| Centered ISS | −988.11 | 1,155.62 | −.08 | ||
| ISC × ISS | −3,501.18 | 1,357.17 | −.22* | ||
ISC interdependent self-construal, ISS instrumental support seeking
p < .05;
p < .01;
p < .001
Fig. 1.
Mean changes in diastolic blood pressure reactivity as a function of instrumental support seeking and interdependent self-construal. Note: ISC interdependent self-construal
Fig. 2.
Mean changes in diastolic blood pressure recovery as a function of instrumental support seeking and interdependent self-construal. Note: ISC interdependent self-construal
No two-way interaction between emotional support seeking and interdependent self-construal on cardiovascular parameters was indicated.
Discussion
This psychophysiological study examined the impacts of the multidimensional nature of social support on cardiovascular responses to stress among Chinese immigrants. The present study did not support the direct buffering effect of social support on cardiovascular responses following provocation. A higher level of structural support, perceived emotional support, and instrumental support seeking were significant predictors of greater BP reactivity. Besides distinctions related to the background of study participants from previous studies, the inconsistent results may also be attributed to the cultural factors, measures, and the stressor specifically utilized for this study.
Chinese culture values reciprocity and indebtedness [48]. This implies that if individuals receive support and assistance from others, the supported recipient may feel obligated to repay the support that they have received. With this type of exchange being constant and lifelong, and with the expectation that favors must be repaid, having a large social network and perceiving themselves as having a large support system can be an added burden for individuals [48].
Chinese culture also emphasizes interdependence. Since individuals are more bound to the in-group and group consensus is more valued than individual attributes [32], seeking support may be culturally inappropriate for Chinese immigrants. This is because support seeking can draw attention from others and bring disgrace to the family, leading others to think that an individual’s family and friends do not provide enough support [49]. Thus, soliciting support can be a stressful experience and may negatively impact BP reactivity.
Regarding the measures that were utilized, given that Chinese cultures tend to draw a clear boundary between their in-group (e.g., spouse and children) and out-group members (e.g., neighbor and colleagues), certain relationships appear to be more important than others [50]. Though the SNI weighs all social roles equally, it may not measure Chinese immigrants’ social network accurately.
The nature of the stressor may also impact the findings. Chinese culture tends to discourage negative emotional sharing as individuals believe that this may worsen their problems [51, 52]. Since the interview required participants to discuss a stressful personal situation, the nature of the task itself may have been a confounder that exacerbated individuals’ cardiovascular responses.
The construct of social support that we utilized may also explain the disconfirming results. Recent investigators have distinguished between explicit and implicit support. Explicit support depicts the western concept of support which assesses individuals’ tendency to seek and receive support [31]. Implicit support refers to the comfort that individuals receive without disclosing their predicaments [32]. As indicated by lower neuroendocrine responses, Asian Americans were less stressed and benefited from implicit support more than explicit support [32]. It is possible that the present conflicting findings are related to measures assessing more explicit support rather than implicit support.
Additionally, the provision of various kinds of social support can be impacted by cultural factors. Chen and her colleagues showed that Japanese participants appeared to be more eager to provide support in order to achieve the goal of closeness and increased the support recipient’s self esteem more than European Americans [53]. It is likely that seeking instrumental support is not only a culturally acceptable type of support, but also a way for Asian/Chinese immigrants who were less acculturated to utilize this method to stay close with their support recipient.
Still, this study did support the moderation impact of interdependent self-construal between instrumental support seeking and DBP reactivity and recovery. The results indicated that those who solicited less instrumental support and upheld less interdependent self-construal were the healthiest group, as indicated by smaller DBP reactivity change and faster recovery. Among individuals who upheld more interdependent self-construal, although seeking instrumental support in response to acute stress can be stressful (as indicated by the DBP reactivity change), the support obtained appeared to help them recover faster following stress (i.e., faster DBP recovery).
Results from the interaction effect can be explained by individuals’ acculturation level. Those who are more acculturated tend to value independence, autonomy, and self-competence, uphold less interdependent self-construal, seek less material and tangential support, and, thus, tend to be less stressed than those who require support [32]. Among those who upheld more interdependent self-construal (possibly less acculturated), seeking instrumental support was found to be beneficial for their long-term cardiovascular health. With language and cultural barriers, Chinese immigrants may have difficulty fully adjusting to mainstream society. Instrumental support may be helpful for them to fulfill their basic needs such as finding jobs and receiving financial assistance. Thus, those who upheld more interdependent self-construal and did not seek support experienced the highest stress, as suggested by their exaggerated DBP reactivity and slow recovery.
Additionally, instrumental support is a more appropriate form of support for Asians/Chinese [33]. Chinese people tend to express love and care through material aid and assistance (e.g., financial support and doing household chores) rather than verbal expression (e.g., saying I love you). However, because Chinese culture emphasizes reciprocity and indebtedness, accepting and seeking tangential help from others can lead to stress, including feelings of shame or relating to feelings of obligation to repay the support and kindness that support providers have given [48].
Recently, Mojaverian and Kim [54] conducted two studies focusing on solicited and unsolicited instrumental support, finding that compared to European Americans, Asian Americans benefitted from unsolicited support and were found to be less stressed when unsolicited support was provided. It appears that unsolicited instrumental support is a stress buffer for Asian Americans. Future studies should explore its benefits on cardiovascular measures to stress among Chinese immigrants.
This study has several limitations. First, it mainly recruited first generation Chinese immigrants who were affiliated with Chinatown and spoke limited or no English. Thus, results from this study may not be generalizable for Chinese immigrants who are more acculturated. Second, research has highlighted the influence of genetics and medication (e.g. beta blockers) on cardiovascular measures [55, 56]. Since this study did not collect information relating to family medical history and prescribed medications, it is unclear whether these factors may have affected the findings. Third, the SCS—interdependent subscale only measures stable trait-like construct rather than the flexible nature of the interdependent self-construal [57]. It is unknown whether other aspects of acculturation such as behavioral adaptation could also affect Chinese immigrants’ cognitive and behavioral aspects of social support and network. A multidimensional acculturation measure such as the Asian American Multidimensional Acculturation Scale should be utilized in the future [58]. This study also did not monitor participants’ BP variability or utilize the impedance cardiography method to assess cardiovascular measures. Research has shown that BP variability has been positively associated with cardiovascular disease events and that the impedance cardiograph method is a comprehensive way to monitor cardiovascular responses [59]. Future studies should utilize the impedance cardiography method and BP variability to examine the buffering effect of social support on Chinese immigrants’ cardiovascular measures, which may help improve the association between the impact of social support and their process of cardiovascular reactivity and recovery from stress.
New Contribution to the Literature
This study has several important clinical implications for Asian immigrants’ social support and cardiovascular health. It adds support for the need to obtain a better understanding of what culturally appropriate social support will lower cardiovascular responses to stress among Asian Americans and immigrants. Although cross-cultural studies have indicated that Asians/Asian Americans tend to seek less support than other ethnicities [30], our study suggested that social support seeking is largely impacted by individuals’ perception of self in relation to others and whether social support is consistent with cultural values. Thus, more studies are needed to explore culturally relevant social support (e.g., invisible or unsolicited support) and ways to facilitate social support seeking behaviors for this population [29, 60].
Present findings indicated that our participants had an average of 12 mmHg increases from SBP baseline in reaction to stress, at least 30 % of individuals reported having hypertension with an additional ten participants who also met the criteria of clinical hypertension based on their average baseline measures, and several participants who had a high BMI and large waist circumference—which suggests a high CVD risk. Research in public health has demonstrated that a 5 mmHg decrease in SBP results in a 14 % decrease in stroke-related mortality, a 9 % reduction in death from CHD, and a 7 % decrease in all-cause mortality [61]. Thus, there is a great need to explore interventions and preventions as methods for improving cardiovascular health among Chinese immigrants.
In sum, our findings were inconsistent with those of previous studies. However, the purpose of this study was not to show that social support is not a cardioprotective factor for Chinese immigrants, but rather how cultural factors play a role in the buffering effects of social support on cardiovascular responses to stress among Chinese immigrants. Future studies should examine the impact of culturally relevant social support constructs, such as implicit or unsolicited support, on individuals’ cardiovascular responses to stress. Additionally, creating a language and information resource center in the immigrant community may be helpful as instrumental support appears to be beneficial for this population. Future investigations should explore whether this kind of intervention will be beneficial for Chinese immigrants’ cardiovascular health.
Acknowledgments
This research was supported in part by NIH grant funding from Grant # R01HL077809, the Diabetes Research and Training Center Grant P60 DK020541, and Clinical and Translational Science Award Grant UL1 RR025750. The Clinical Trials Identifier is NCT00362128.
Contributor Information
Yuen Shan Christine Lee, Email: yuenshan.lee@nyumc.org, New York University Langone Medical Center, New York, NY, USA.
Sonia Suchday, Ferkauf Graduate School of Psychology/Albert Einstein College of Medicine, Yeshiva University, New York, NY, USA.
Judith Wylie-Rosett, Albert Einstein College of Medicine, Yeshiva University, New York, NY, USA.
References
- 1.United States Census Bureau. The Asian population: 2010. [Retrieved March 20, 2013];2010 from http://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf.
- 2.Dillon FR, De La Rosa M, Ibanez GE. Acculturative stress and diminishing family cohesion among recent Latino immigrants. J Immigr Minor Health. 2013;15(3):484–491. doi: 10.1007/s10903-012-9678-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yakhnich L. Immigration as a multiple-stressor situation: stress and coping among immigrants from the former Soviet Union in Israel. Int J Stress Manag. 2008;15(3):252–268. [Google Scholar]
- 4.Uchino BN, Cacioppo JT, Kiecolt-Glaser JK. The relationship between social support and physiological processes: a review with emphasis on underlying mechanisms and implications for health. Psychol Bull. 1996;119(3):488–531. doi: 10.1037/0033-2909.119.3.488. [DOI] [PubMed] [Google Scholar]
- 5.Fang J, Foo SH, Fung C, Wylie-Rosett J, Alderman MH. Stroke risk among Chinese immigrants in New York City. J Immigr Minor Health. 2006;8(4):387–393. doi: 10.1007/s10903-006-9009-7. [DOI] [PubMed] [Google Scholar]
- 6.Fang J, Foo SH, Jeng JS, Yip PK, Alderman MH. Clinical characteristics of stroke among Chinese in New York City. Ethn Dis. 2004;14(3):378–383. [PubMed] [Google Scholar]
- 7.Fang J, Madhavan S, Alderman MH. Cardiovascular mortality of Chinese in New York City. J Urban Health. 1999;76:51–61. doi: 10.1007/BF02344461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anand SS, Yusuf S, Vuksan V, et al. The Study of Health Assessment and Risk in Ethnic groups (SHARE): rationale and design. The SHARE Investigators. Can J Cardiol. 1998;14(11):1349–1357. [PubMed] [Google Scholar]
- 9.Sheth T, Nair C, Nargundkar M, Anand S, Yusuf S. Cardiovascular and cancer mortality among Canadians of European, South Asian and Chinese origin from 1979 to 1993: an analysis of 1.2 million deaths. CMAJ. 1999;161(2):132–138. [PMC free article] [PubMed] [Google Scholar]
- 10.Glynn LM, Christenfeld N, Gerin W. The role of rumination in recovery from reactivity: cardiovascular consequences of emotional states. Psychosom Med. 2002;64(5):714–726. doi: 10.1097/01.psy.0000031574.42041.23. [DOI] [PubMed] [Google Scholar]
- 11.Phillips AC, Ginty AT, Hughes BM. The other side of the coin: blunted cardiovascular and cortisol reactivity are associated with negative health outcomes. Int J Psychophysiol. 2013;90(1):1–7. doi: 10.1016/j.ijpsycho.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Bishop GD, Robinson G. Anger, harassment, and cardiovascular reactivity among Chinese and Indian men in Singapore. Psychosom Med. 2000;62(5):684–692. doi: 10.1097/00006842-200009000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Shen BJ, Stroud LR, Niaura R. Ethnic differences in cardiovascular responses to laboratory stress: a comparison between Asian and white Americans. Int J Behav Med. 2004;11(3):181–186. doi: 10.1207/s15327558ijbm1103_7. [DOI] [PubMed] [Google Scholar]
- 14.Why YP, Bishop GD, Tong EM, et al. Cardiovascular reactivity of Singaporean male police officers as a function of task, ethnicity and hostility. Int J Psychophysiol. 2003;49(2):99–110. doi: 10.1016/s0167-8760(03)00082-5. [DOI] [PubMed] [Google Scholar]
- 15.Lee YS, Suchday S, Wylie-Rosett J. Perceived social support, coping styles, and Chinese immigrants’ cardiovascular responses to stress. Int J Behav Med. 2012;19(2):174–185. doi: 10.1007/s12529-011-9156-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Creaven AM, Hughes BM. Cardiovascular responses to mental activation of social support schemas. Intl J Psychophysiol. 2012;84(2):113–119. doi: 10.1016/j.ijpsycho.2012.01.018. [DOI] [PubMed] [Google Scholar]
- 17.Gramer M, Reitbauer C. The influence of social support on cardiovascular responses during stressor anticipation and active coping. Biol Psychol. 2012;85(2):268–274. doi: 10.1016/j.biopsycho.2010.07.013. [DOI] [PubMed] [Google Scholar]
- 18.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. [PubMed] [Google Scholar]
- 19.Fortmann AL, Gallo LC. Social support and nocturnal blood pressure dipping: a systematic review. Am J Hypertens. 2013;26(3):302–310. doi: 10.1093/ajh/hps041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lett HS, Blumenthal JA, Babyak MA, et al. Social support and coronary heart disease: epidemiologic evidence and implications for treatment. Psychosom Med. 2005;67(6):869–878. doi: 10.1097/01.psy.0000188393.73571.0a. [DOI] [PubMed] [Google Scholar]
- 21.Rutledge T, Reis SE, Olson M, et al. Social networks are associated with lower mortality rates among women with suspected coronary disease: the National Heart, Lung, and Blood Institute-Sponsored Women’s Ischemia Syndrome Evaluation study. Psychosom Med. 2004;66(6):882–888. doi: 10.1097/01.psy.0000145819.94041.52. [DOI] [PubMed] [Google Scholar]
- 22.Christenfeld N, Gerin W. Social support and cardiovascular reactivity. Biomed Pharmacother. 2000;54(5):251–257. doi: 10.1016/S0753-3322(00)80067-0. [DOI] [PubMed] [Google Scholar]
- 23.Phillips AC, Gallagher S, Carroll D. Social support, social intimacy, and cardiovascular reactions to acute psychological stress. Ann Behav Med. 2009;37(1):38–45. doi: 10.1007/s12160-008-9077-0. [DOI] [PubMed] [Google Scholar]
- 24.Wong ST, Yoo GJ, Stewart AL. The changing meaning of family support among older Chinese and Korean immigrants. J Gerontol B Psychol Sci Soc Sci. 2006;61(1):S4–S9. doi: 10.1093/geronb/61.1.s4. [DOI] [PubMed] [Google Scholar]
- 25.Rhee E, Uleman JS, Lee HK, Roman RJ. Spontaneous self-descriptions and ethnic identities in individualistic and collectivistic cultures. J Pers Soc Psychol. 1995;69(1):142–152. doi: 10.1037//0022-3514.69.1.142. [DOI] [PubMed] [Google Scholar]
- 26.Kitayama S, Markus HR, Matsumoto H, Norasakkunkit V. Individual and collective processes in the construction of the self: self-enhancement in the United States and self-criticism in Japan. J Pers Soc Psychol. 1997;72(6):1245–1267. doi: 10.1037//0022-3514.72.6.1245. [DOI] [PubMed] [Google Scholar]
- 27.Kashima Y, Yamaguchi S, Kim U, et al. Culture, gender, and self: a perspective from individualism-collectivism research. J Pers Soc Psychol. 1995;69(5):925–937. doi: 10.1037//0022-3514.69.5.925. [DOI] [PubMed] [Google Scholar]
- 28.Abe-Kim J, Takeuchi DR, Hwang W. Predictors of help seeking for emotional distress among Chinese Americans: family matters. J Consult Clin Psychol. 2002;70(5):1186–1190. [PubMed] [Google Scholar]
- 29.Taylor SE, Sherman DK, Kim HS, et al. Culture and social support: who seeks it and why? J Pers Soc Psychol. 2004;87(3):354–362. doi: 10.1037/0022-3514.87.3.354. [DOI] [PubMed] [Google Scholar]
- 30.Kim HS, Sherman DK, Ko D, et al. Pursuit of happiness and pursuit of harmony: culture, relationships, and social support seeking. Pers Soc Psychol Bull. 2006;32(12):1595–1607. doi: 10.1177/0146167206291991. [DOI] [PubMed] [Google Scholar]
- 31.Kim HS, Sherman DK, Taylor SE. Culture and social support. Am Psychol. 2008;63(6):518–526. doi: 10.1037/0003-066X. [DOI] [PubMed] [Google Scholar]
- 32.Taylor SE, Welch WT, Kim HS, et al. Cultural differences in the impact of social support on psychological and biological stress responses. Psychol Sci. 2007;18(9):831–837. doi: 10.1111/j.1467-9280.2007.01987.x. [DOI] [PubMed] [Google Scholar]
- 33.Glazer S. Social support across cultures. IJIR. 2006;30(5):605–622. [Google Scholar]
- 34.Cohen S, Doyle WJ, Skoner DP, et al. Social ties and susceptibility to the common cold. JAMA. 1997;277(24):1940–1944. [PubMed] [Google Scholar]
- 35.Cohen S, Mermelstein R, Kamarck T, et al. Social support: theory, research and applications. In: Sarason IG, Sarason BR, editors. Measuring the functional components of social support. Dordrecht: Martinus Nijhoff Publishers; 2004. pp. 73–94. [Google Scholar]
- 36.Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. J Appl Soc Psychol. 1983;13(1):99–125. [Google Scholar]
- 37.Fong KW. How parenting stress and social support affect the demand for respite care services for caregivers having children with mental handicaps in Hong Kong. Hong Kong: The University of Hong Kong; 2004. [Google Scholar]
- 38.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56(2):267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 39.Myers LB, Derakshan N. Monitoring and blunting and an assessment of different coping styles. Pers Indiv Differ. 2000;28(1):111–121. [Google Scholar]
- 40.Singelis TM. The measurement of independent and interdependent self-construals. Pers Soc Psychol Bull. 1994;20(5):580–591. [Google Scholar]
- 41.Lin H, Lin C, Liang S, Chung Y. Can independent and interdependent self coexist? Comparisons of Self-concept between the Hans and the aborigines in Taiwan. Poster presented at fourth SELF biennial international conference; Ann Arbor, MI. 2006. [Google Scholar]
- 42.Ewart CK, Ditmar MM, Suchday S, Sonnega JR. Instruction manual for the social competence interview. Syracuse University; 2006. [Google Scholar]
- 43.Ewart CK, Jorgensen RS, Schroder KE, et al. Vigilance to a persisting personal threat: unmasking cardiovascular consequences in adolescents with the Social Competence Interview. Psychophysiology. 2004;41(5):799–804. doi: 10.1111/j.1469-8986.2004.00199.x. [DOI] [PubMed] [Google Scholar]
- 44.Ewart CK, Kolodner KB. Social competence interview for assessing physiological reactivity in adolescents. Psychosom Med. 1991;53(3):289–304. doi: 10.1097/00006842-199105000-00003. [DOI] [PubMed] [Google Scholar]
- 45.Pickering TG. Challenge response predictors. General principles. Am J Hypertens. 1991;4(11):611–614. doi: 10.1093/ajh/4.11s.611s. [DOI] [PubMed] [Google Scholar]
- 46.Neumann SA, Sollers JJ, Thayer JF, et al. Alexithymia predicts attenuated autonomic reactivity, but prolonged recovery to anger recall in young women. Int J Psychophysiol. 2004;53(3):183–195. doi: 10.1016/j.ijpsycho.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 47.Aiken LS, West SG. Multiple regression: testing and interpreting interactions. Newbury Park, CA: Sage; 1990. [Google Scholar]
- 48.Lee LC, Zane NWS. Handbook of Asian American psychology. Thousand Oaks, CA: Sage Publications Inc.; 1998. [Google Scholar]
- 49.Uchida Y, Kitayama S, Mesquita B, et al. Is perceived emotional support beneficial? Well-being and health in independent and interdependent cultures. Pers Soc Psychol Bull. 2008;34(6):741–754. doi: 10.1177/0146167208315157. [DOI] [PubMed] [Google Scholar]
- 50.Iyengar SS, Lepper MR, Ross L. Cultural divides: understanding and overcoming group conflict. New York, NY: Russell Sage Foundation; 1999. Independence from whom? Interdependence with whom? Cultural perspectives on ingroups versus outgroups; pp. 273–301. [Google Scholar]
- 51.Kim HS, Markus HR. Freedom of speech and freedom of silence: an analysis of talking as a cultural practice. In: Shweder R, Minow M, Markus HR, editors. Engaging cultural differences: the multicultural challenge in liberal democracies. New York: Russell-Sage Foundation; 2002. pp. 432–452. [Google Scholar]
- 52.Sherman DK, Kim HS, Taylor SE. Culture and social support: neural bases and biological impact. Prog Brain Res. 2009;178:227–237. doi: 10.1016/S0079-6123(09)17816-0. [DOI] [PubMed] [Google Scholar]
- 53.Chen JM, Kim HS, Mojaverian T. Culture and social support provision: who gives what and why. Pers Soc Psychol Bull. 2012;38(1):3–13. doi: 10.1177/0146167211427309. [DOI] [PubMed] [Google Scholar]
- 54.Mojaverian T, Kim HS. Interpreting a helping hand: cultural variation in the effectiveness of solicited and unsolicited social support. Pers Soc Psychol Bull. 2013;39(1):88–99. doi: 10.1177/0146167212465319. [DOI] [PubMed] [Google Scholar]
- 55.Schmieder R, Friedrich G, Neus H, et al. The influence of beta blockers on cardiovascular reactivity and type A behavior pattern in hypertensives. Psychosom Med. 1983;45(5):417–423. doi: 10.1097/00006842-198310000-00005. [DOI] [PubMed] [Google Scholar]
- 56.Wu T, Sneider H, de Geus E. Genetic influences on cardiovascular stress reactivity. Neurosci Biobehav Rev. 2010;35(1):58–68. doi: 10.1016/j.neubiorev.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 57.Levine TR, Bresnahan MJ, Park HS, et al. Self-construal scales lack validity. Hum Commun Res. 2003;29(2):210–252. [Google Scholar]
- 58.Chung RH, Kim BS, Abreu JM. Asian American multidimensional acculturation scale: development, factor analysis, reliability, and validity. Cultur Divers Ethnic Minor Psychol. 2004;10(1):66–80. doi: 10.1037/1099-9809.10.1.66. [DOI] [PubMed] [Google Scholar]
- 59.Christian LM, Stoney CM. Social support versus social evaluation: unique effects on vascular and myocardial response patterns. Psychosom Med. 2006;68(6):914–921. doi: 10.1097/01.psy.0000244023.20755.cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chang EC. A look at the coping strategies and styles of Asian Americans: similar and different? In: Snyder CR, editor. Coping with stress: effective people and processes. New York: Oxford University Press; 2001. pp. 222–239. [Google Scholar]
- 61.Whelton PK, He J, Appel LJ, et al. Primary prevention of hypertension: clinical and public health advisory from the National High Blood Pressure Education Program. JAMA. 2002;288(2):1882–1888. doi: 10.1001/jama.288.15.1882. [DOI] [PubMed] [Google Scholar]