Introduction
Giant cell tumor (GCTTS) of the tendon sheath is the second most common benign tumor of the hand. Two morphological types have been described; localized and diffuse types [1]. While localized lesions are commonly seen in the hand, diffuse variety is similar to pigmented villonodular synovitis (PVNS) in morphology and often involves large joints, knee being the most common location. Local recurrence is the hallmark of the lesion with reported recurrence rates of more than 40 % [2]. We present our experience in surgical management of a rare case of recurrent, diffuse, multicentric giant cell tumor of the hand; discuss treatment options and review of the literature.
Case Report
A 24 years male presented with painful multiple swellings in a linear pattern over the right hand centered over the metacarpophalangeal (MCP) joints of the IV and V fingers. Past records revealed surgical excision done for a similar lesion 6 months ago with positive histopathology for GCTTS and flow cytometry report suggested high rates of mitotic activity and aneuploidy. Pre operative x rays showed minimal cortical indentation but no intra-osseous extension or adjacent joint degeneration. MR imaging showed multiple nodular lesions extending circumferentially over the common flexor tendon sheath of the IV and V digits from zone II to VII (Fig. 1).
Fig. 1.
Magnetic resonance image showing the extent of lesions
Per-operatively, the tumor mass was found invading into the FDS and FDP tendon (Fig. 2). The entire flexor apparatus of the IV and V digits including the carpal tunnel was excised till the musculotendinous junction. Reconstruction of the flexor apparatus (FDP tendon, carpal tunnel, A1 and A2 pulleys) was done using autologous fascia lata grafts (Fig. 3). Postoperative histopathology report confirmed the diagnosis of GCT with tumor free margins.
Fig. 2.
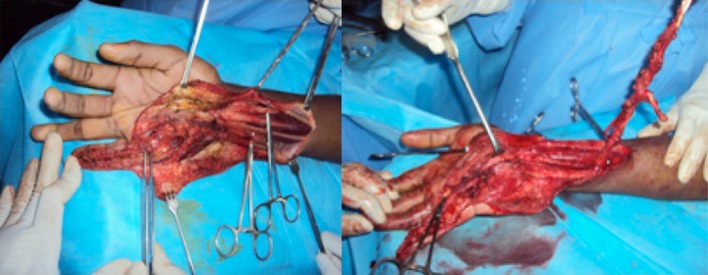
Intra-operative photographs showing the lesions and resected specimen
Fig. 3.

Flexor apparatus reconstruction using fascia lata grafts
Supervised mobilization exercises were started after 3 weeks. The patient underwent surgical release and scar excision for residual contractures after being lost in follow up for 2 months. Two years post surgery; the patient has been clinically free of disease, pain free with functional ROM (MCP joints: 0°–80°, PIP joints: 0°–80°, DIP joints: 0°–25°). Ultrasonogram at 1-year follow up showed a recurrence free hand.
Discussion
GCTTS commonly present as localized painless mass on the palmar aspect of the hand digits. The tumor is characteristically benign with a tendency for local recurrence though reports of malignant GCTTS have been documented [3]. Complete surgical excision can still result in recurrence rates ranging from 9 to 44 % [4]. Complete tumor clearance is the key to minimize local recurrence even if it involves amputation of the involved digit [5]. The use of radiotherapy has also been described to prevent recurrence [6].
Wide excision was planned for our patient due to the following reasons; i) the patient presented with an early recurrence, ii) the tumor was diffuse, multicentric with circumferential involvement of the common flexor sheath and flexor tendons iii) flow cytometry report after the initial surgery had showed high mitotic activity and varying degrees of aneuploidy. Following wide excision, reconstruction of minimum two pulleys with synovial lined grafts is recommended for near normal hand function [7, 8]. We used fascia lata grafts for both pulley and FDP reconstruction because of availability of large portions of grafts to reconstruct the entire flexor apparatus of two digits and the carpal tunnel. The functional results however were satisfactory.
Though being a common lesion, the high recurrence rates associated with GCTTS are of concern. The results should improve with more aggressive surgical clearance and reconstruction techniques being adopted. This will avoid multiple surgeries and provide good long-term function.
Acknowledgments
Conflict of interest
None
Footnotes
The work may be attributed to hand and microvascular surgery unit, Parvathy hospital, Chennai
References
- 1.Abdul-Karim FW, el-Naggar AK, Joyce MJ, Makley JT, Carter JR. Diffuse and localized tenosynovial giant cell tumor and pigmented villonodular synovitis: a clinicopathologic and flow cytometric DNA analysis. Hum Pathol. 1992;23:729–735. doi: 10.1016/0046-8177(92)90340-9. [DOI] [PubMed] [Google Scholar]
- 2.Granowitz SP, D’Antonio J, Mankin HL. The pathogenesis and long-term end-results of pigmented villonodular synovitis. Clin Orthop. 1976;114:335–351. [PubMed] [Google Scholar]
- 3.Ushijima M, Hashimoto H, Tsuneyoshi M, Enjoji M, Miyamoto Y, Okue A. Malignant giant cell tumor of tendon sheath. Report of a case. Acta Pathol Jpn. 1985;35:699–709. doi: 10.1111/j.1440-1827.1985.tb00611.x. [DOI] [PubMed] [Google Scholar]
- 4.Reilly KE, Stern PJ, Dale JA. Recurrent giant cell tumors of the tendon sheath. J Hand Surg [Am] 1999;24:1298–1302. doi: 10.1053/jhsu.1999.1298. [DOI] [PubMed] [Google Scholar]
- 5.Lu C-T, Chen H-C, Coskunfirat OK. Immediate toe transfer following index finger amputation for extensive giant cell tumor of the tendon sheath with intraosseous invasion. J Med. 2004;27:312–317. [PubMed] [Google Scholar]
- 6.Friedman M, Schwartz EE. Irradiation therapy of pigmented villo- nodular synovitis. Bull Hosp Joint Dis. 1957;18:19–32. [PubMed] [Google Scholar]
- 7.Mehta V, Phillips CS. Flexor tendon pulley reconstruction. Hand Clin. 2005;21:245–251. doi: 10.1016/j.hcl.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 8.Klinert HE, Bennett JB. Digital pulley reconstruction employing the always present rim of the previous pulley. J Hand Surg [Am] 1978;3:297–298. doi: 10.1016/S0363-5023(78)80098-7. [DOI] [PubMed] [Google Scholar]



