Abstract
We offered rapid HIV testing at social events frequented by young men who have sex with men (MSM), a group disproportionately affected by the HIV epidemic. We tested 1,312 MSM; of those MSM, 1,072 (81.7%) reported HIV testing history. Of those reporting HIV testing history, 550 (51.3%) were non-Hispanic black and 404 (37.7%) were aged <25 years. One hundred twenty-eight (11.9%) had never tested for HIV; 77 (7.2%) were preliminarily positive, with 15 (19.5%) being first-time testers. Factors associated with no previous HIV test included young age (13–24 years) (adjusted odds ratio [AOR] = 3.5, 95% confidence interval [CI] 1.9, 6.5) and non-Hispanic black (AOR=3.2, 95% CI 1.6, 6.4) or Hispanic (AOR=2.8, 95% CI 1.2, 6.3) race/ethnicity. HIV testing at Gay Pride events reaches young, previously untested MSM. This venue-based HIV testing approach at nonclinical sociocultural events is an additional strategy for HIV prevention goals to increase the number of people aware of their HIV infection with subsequent linkage to HIV care.
An estimated 20% of 1.2 million people living with human immunodeficiency virus (HIV) infection in the United States are unaware of their HIV infection.1 Among people living with HIV, young non-Hispanic black men who have sex with men (MSM) are the only group with significant increases in incident HIV cases in recent years.2 Although young non-Hispanic black and Hispanic MSM are more likely to report being tested, they are also more likely to be unaware of an HIV infection than their white counterparts.3 A recent analysis reported that 44% of MSM in 21 cities were unaware of their infection; non-Hispanic black MSM comprised 59% of that group.4 People unaware of their HIV infection transmit approximately half of incident HIV infections.5
Although young non-Hispanic black MSM do not engage in risky behaviors more than young non-Hispanic white or Hispanic men,6 they are more vulnerable to becoming HIV-infected than MSM from other racial/ethnic groups. Reasons for this disproportionate impact on young MSM of color are unclear, but include high community prevalence of HIV, social and structural barriers to routine screening and treatment (e.g., less health insurance, higher unemployment, and higher rate of incarceration), and stigma and homophobia.7 MSM with increased risk of HIV exposure may benefit from increased access to HIV screening in nontraditional/clinical settings.
Early diagnosis and effective treatment with antiretroviral therapy are important components of reducing HIV transmission risk and incident HIV infections.3 Current recommendations support routine HIV screenings in health-care settings for people aged 13–64 years to provide opportunities for early diagnosis and linkage to care.8 Gaps in the implementation of these recommendations remain, however, and data suggest that opportunities to diagnose HIV infections in health-care settings, particularly among young MSM of color, may frequently be missed.9 Young MSM at increased risk of HIV exposure may benefit from more frequent testing intervals (i.e., every 3–6 months).6,10
HIV testing in nonclinical community settings is an additional prevention strategy to reach young minority MSM who disproportionately lack health-care access.10,11 Nonclinical social events where large numbers of at-risk people may gather at locations perceived to be culturally sensitive, such as Gay Pride festivals, offer expanded opportunities for HIV testing. In addition, from the provider perspective, analyses have shown that community-based efforts for HIV testing cost less than testing in clinical settings.12 These efforts are crucial as we work toward goals of the National HIV/AIDS Strategy.13
Previous reports of HIV testing outreach have supported the feasibility of this approach with racial/ethnic minority MSM.14,15 However, factors associated with having not been previously tested among MSM reached at these events are poorly understood.14 In this article, we summarize findings from the Behavioral Assessment and Rapid Testing (BART) project,16 a community-based HIV testing project that was implemented in multiple U.S. cities. Our objectives were to (1) describe characteristics of MSM who accepted HIV testing, (2) examine differences in time since previous HIV test for participants, and (3) describe factors associated with not having been previously tested for HIV.
METHODS
Recruitment and enrollment
From June 2009 to December 2010, the Centers for Disease Control and Prevention (CDC) conducted the BART project,16 which offered free rapid HIV testing at selected public sociocultural events serving at-risk populations. The BART project's goal was to increase the proportion of people (men and women) aware of their HIV status and linked to care. We recruited participants from 13 Gay Pride events held in 13 U.S. cities with high HIV prevalence and events scheduled within the window of BART data collection activities (Atlanta, Georgia; Chicago, Illinois; Houston, Texas; Little Rock, Arkansas; Los Angeles, California; Memphis, Tennessee; Miami, Florida; New Orleans, Louisiana; Palm Springs, California; Portland, Maine; San Diego, California; Toledo, Ohio; and Washington, D.C.) using convenience sampling methods. Recruitment at events was conducted collaboratively among local community-based organization (CBO), local health department (LHD), and CDC staff members by having a discreet HIV education display area at the events and by walking up to/directly engaging event attendees.
For this subanalysis of BART, eligible participants included men aged ≥13 years who reported having anal or oral sex with a man in the previous 12 months, who could describe their HIV testing history, and who were willing to undergo rapid HIV testing. Informed consent was obtained for all eligible individuals (including men aged <18 years and consistent with local laws for HIV testing of young people) by signing a consent form containing information about rapid HIV testing.
Demographic and behavioral assessments
We collected demographic and risk behavior data (previous 12 months) using a standardized CDC HIV testing intake form that included age, race/ethnicity, state of residence, HIV testing history and date of last test (if any), gender of partner(s), types of sex (i.e., oral, vaginal, or anal), history of sex with people known to be HIV infected, condom use, and history of sex with injection drug users.
HIV testing and referrals
We provided free, confidential rapid HIV testing in accordance with LHD policy and in collaboration with local HIV testing agencies; thus, testing procedures varied by jurisdiction, but all followed published CDC recommendations.8 The rapid HIV test offered was the OraQuick ADVANCE® Rapid HIV-1/2 antibody test (OraSure Technologies, Bethlehem, Pennsylvania) with an oral fluid specimen. Participants who tested preliminarily positive using the reactive rapid HIV test were confidentially counseled and referred for confirmatory testing by either Western blot or second rapid HIV test at the LHD facility and linked to care by LHD partners. People who resided in a city that was different from where they were tested were referred for local care based on their residence ZIP Code.
Data analysis
For this analysis, we included only male participants. We used Chi-square statistics to compare differences in the distributions of variables among three groups: participants who never tested before the event, those who tested ≤12 months before the event, and those who tested >12 months before the event. We considered p<0.05 to be statistically significant. All comparisons with statistically significant p-values were included in the final model. We used multivariate logistic regression to identify factors associated with having never previously been tested for HIV. Unadjusted odds ratios (ORs) and adjusted ORs (AORs) were reported with 95% confidence intervals (CIs). We performed analyses using SAS® version 9.1.3.17
RESULTS
A total of 2,517 men were approached for BART participation. Of those men, 1,312 (52.1%) self-identified as MSM, completed surveys, and agreed to an on-site rapid HIV test; 240 men (18.3%) did not report their HIV testing history and were excluded from analysis. Excluded participants did not differ significantly from those included in terms of risk factors and HIV test positivity. The final analysis sample contained 1,072 participants. The 1,205 (47.9%) of 2,517 men approached who did not self-identify as MSM reported heterosexual activity only (82.6%) or declined to participate in the study.
Table 1 summarizes selected characteristics of participants. Of the 1,072 participants, 550 (51.3%) were non-Hispanic black, 404 (37.7%) were <25 years of age, 574 (53.5%) reported having sex without a condom, 138 (12.9%) had sex with an HIV-positive person, 956 (89.2%) had sex exclusively with men, and 438 (40.9%) resided in the event community.
Table 1.
Reported history of HIV testing among MSM receiving rapid HIV test results at sociocultural events, by selected characteristics—BART project, 13 U.S. cities,a 2009–2010
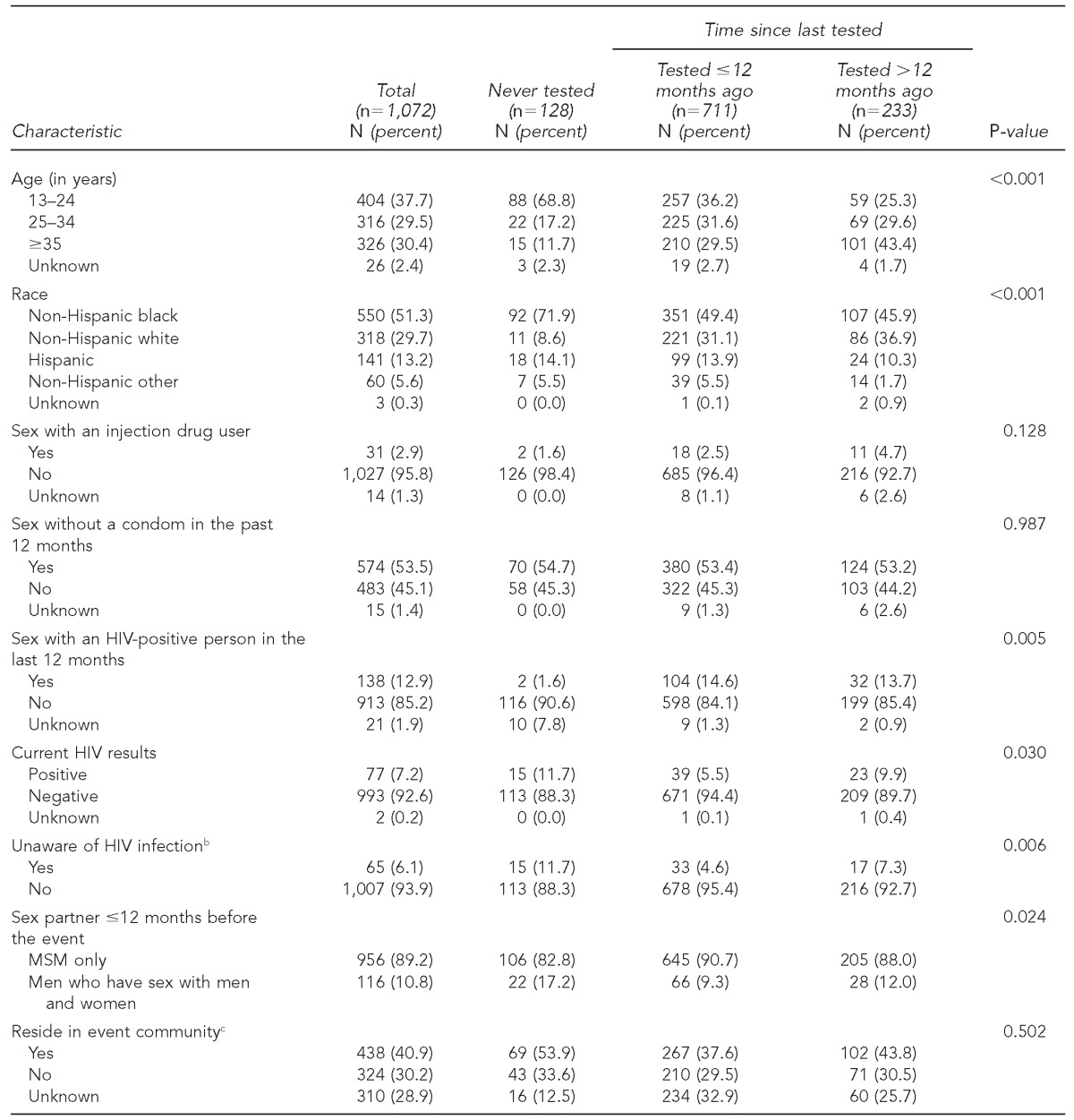
The 13 U.S. cities included those with high HIV prevalence and events scheduled within the window of BART data collection activities (Atlanta, Georgia; Chicago, Illinois; Houston, Texas; Little Rock, Arkansas; Los Angeles, California; Memphis, Tennessee; Miami, Florida; New Orleans, Louisiana; Palm Springs, California; Portland, Maine; San Diego, California; Toledo, Ohio; and Washington, D.C.).
bParticipants had not previously had a positive HIV test result.
cSan Diego, California, did not report ZIP Code data.
HIV = human immunodeficiency virus
MSM = men who have sex with men
BART = Behavioral Assessment and Rapid Testing
Among the 1,072 MSM, 128 (11.9%) had never been tested previously for HIV, 711 (66.3%) had tested ≤12 months before the event, and 233 (21.7%) had tested >12 months before the event. Of the participants who never previously tested for HIV, most were aged 13–24 years (n=88, 68.8%), were non-Hispanic black (n=92, 71.9%), reported sex without a condom in the last 12 months (n=70, 54.7%), and resided in the BART event community (n=69, 53.9%) (Table 1).
Seventy-seven (7.2%) participants tested preliminarily HIV positive (i.e., had a positive reactive rapid HIV test), of whom 15 (19.5%) had never tested previously for HIV, 39 (50.6%) had a negative test ≤12 months before the event, and 23 (29.9%) had a negative test >12 months before the event. Confirmed HIV-positive status from LHD partners was obtained for nine preliminarily HIV-positive participants. The proportion of preliminarily HIV-positive participants who had never been previously tested for HIV was significantly higher than the proportion of HIV-negative participants who had not previously been tested for HIV (15/77, 19.5% vs. 113/993, 11.4%, p=0.03) (Table 1).
Sixty-five of 77 participants (84.4%) who tested preliminarily HIV positive stated they were unaware of their possible infection (Table 1). Fifty-eight of the 65 (89.2%) preliminarily HIV-positive participants who were unaware of their HIV infection were non-Hispanic black, six (9.2%) were Hispanic, and one (1.5%) was non-Hispanic white. Of the 58 non-Hispanic black people who tested preliminarily positive, 29 (50.0%) had never tested previously for HIV, 16 (27.6%) had a negative test ≤12 months before the event, and 13 (22.4%) had a negative test >12 months before the event. Three of the Hispanic men and the one non-Hispanic white man, all of whom were unaware of possible infection, had a negative test ≤12 months before the event (data not shown).
After adjusting for age, race/ethnicity, sex without a condom, current HIV status, and sex with either a male partner only or with both male and female partners, younger age (aged 13–24 years, AOR=3.5, 95% CI 1.9, 6.5) compared with older age (aged ≥35 years) was significantly associated with never testing for HIV. Likewise, non-Hispanic black (AOR=3.2, 95% CI 1.6, 6.4) and Hispanic (AOR=2.8, 95% CI 1.2, 6.3) race/ethnicity compared with non-Hispanic white race/ethnicity were significantly associated with never testing for HIV (Table 2).
Table 2.
Multivariate logistic regression of factors associated with never previously testing for HIV among MSM: BART project, 13 U.S. cities,a 2009–2010
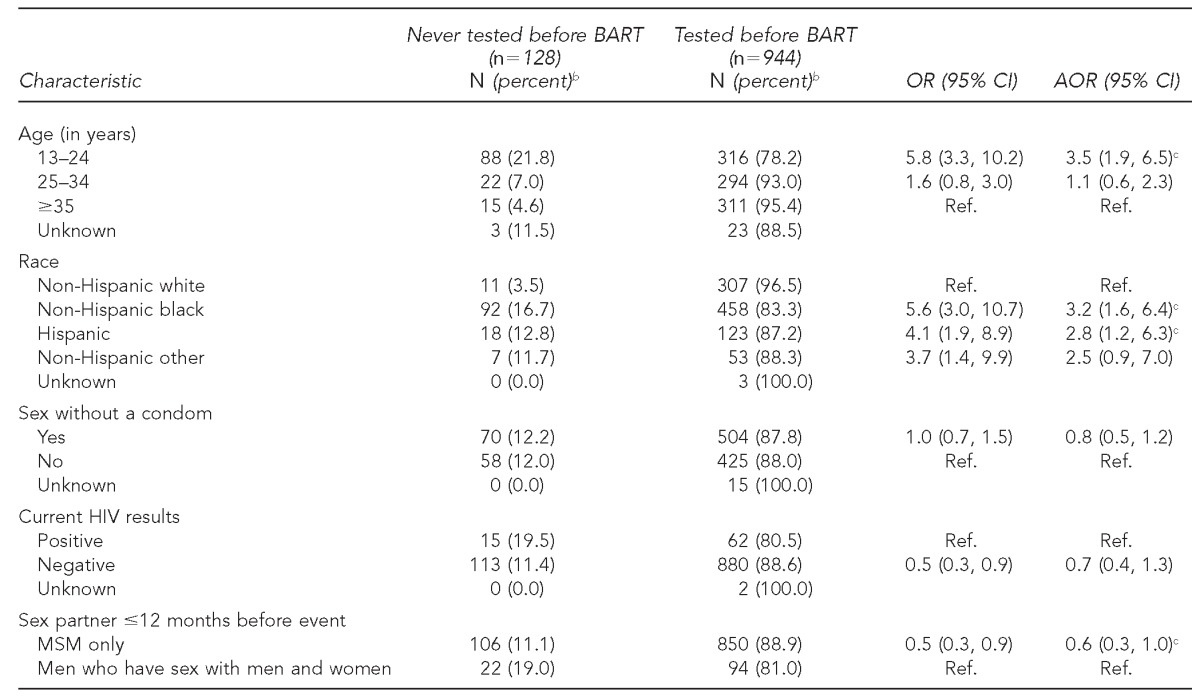
The 13 U.S. cities included those with high HIV prevalence and events scheduled within the window of BART data collection activities (Atlanta, Georgia; Chicago, Illinois; Houston, Texas; Little Rock, Arkansas; Los Angeles, California; Memphis, Tennessee; Miami, Florida; New Orleans, Louisiana; Palm Springs, California; Portland, Maine; San Diego, California; Toledo, Ohio; and Washington, D.C.).
bRow percentages are shown.
cSignificant at p<0.05 (model adjusted for age, race, sex without a condom, current HIV status, and sex partner in the last 12 months)
HIV = human immunodeficiency virus
MSM = men who have sex with men
BART = Behavioral Assessment and Rapid Testing
OR = odds ratio
CI = confidence interval
AOR = adjusted odds ratio
Ref. = reference group
DISCUSSION
This study demonstrates that on-site, rapid HIV testing at Gay Pride events can successfully reach at-risk young non-Hispanic black and Hispanic MSM, including people who have not previously tested for HIV. Young minority MSM face particular barriers to getting tested, including decreased health-care access,18 low insurance coverage,19,20 and concerns about homophobia and stigma.21 HIV testing provided outside of the health-care setting, such as at Gay Pride events, is an important strategy to reach MSM who might not regularly access health care.14 By partnering with trained, locally recognized CBOs and LHD staff using direct engagement strategies, we were able to enroll people attending sociocultural events for HIV surveys and on-site testing. Compared with clinical settings, the rate of newly diagnosed HIV infection in nonclinical settings such as BART was higher (1.1% vs. 0.6%), which suggests that testing at sociocultural events such as BART can be more effective at diagnosing new HIV infections than some clinical settings.11 BART expands on -previous sociocultural HIV testing reports14 by obtaining behavioral information to help inform future prevention strategies with MSM.
More than half of our participants reported having anal sex without a condom in the past year. Despite risk behaviors, 84% of participants who tested preliminarily positive were unaware of their possible HIV infection. Many of them were young non-Hispanic black MSM who tested for the first time at the BART event. As non-Hispanic black and Hispanic MSM are overrepresented among those with unrecognized HIV infection,22 testing efforts that are tailored to this population are especially important to decrease new infections and thwart unintended spread of HIV in disproportionately affected minority communities. In addition, people who are aware of their infection are more likely to curb risk behaviors to protect themselves and their loved ones.23
Factors associated independently with no history of HIV testing were young age (13–24 years of age) and non-Hispanic black and Hispanic race/ethnicity. Lack of testing in these groups has been associated with lack of access to care,24 lack of testing by providers,25 and lack of medical insurance.21,26 Free HIV testing at sociocultural events may be appealing to some minority and young MSM, as cost associated with testing is eliminated, access to testing is increased, and concern about stigma that could be associated with disclosing sexual behaviors to providers is reduced.27
Limitations
This study was subject to several limitations. First, the denominators of people attending these events were not available; as such, it is unknown what percentage of event attendees comprised our participants. Our participant rate was likely low at some BART events, mainly because some people approached were more focused on the sociocultural event and were unable to wait for the BART survey and HIV test component due to time constraints. Second, our analysis contained preliminarily positive results; we had no information regarding the proportion of false-positives among these participants. However, rates of false-positive results with the rapid HIV test used are low (specificity = 99.9%).28 Third, even though HIV linkage-to-care protocols were followed and all participants who tested preliminarily positive were referred, we were unable to systematically collect data confirming linkage to care from local partners; we documented confirmed HIV-positive status for nine participants. More recent CDC event-based testing efforts are working to strengthen local capacity and interagency communication to report confirmatory testing and linkage to care for ≥85% of newly diagnosed people.11 Fourth, self-selection bias was possible due to convenience sampling methods and likely stigma of HIV discussions in public venues; therefore, our findings may not be generalizeable to all people who attended these events.
CONCLUSION
This study demonstrates that offering HIV testing at nonclinical sociocultural events can be a useful strategy, especially for reaching untested young racial/ethnic minority MSM. Testing at these nonclinical venues can be an important additional tool to increase HIV awareness and reduce racial/ethnic HIV-related disparities.
Footnotes
The authors thank the Behavioral Assessment and Rapid Testing (BART) study participants, local health department staff, and testing agency collaborators and study staff members who helped make the BART project possible. The final protocol was approved by the Centers for Disease Control and Prevention (CDC) Institutional Review Board.
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of CDC.
REFERENCES
- 1.HIV surveillance—United States 1981–2008 [published erratum appears in MMWR Morb Mortal Wkly Rep 2011;60(25)852] MMWR Morb Mortal Wkly Rep. 2011;60(21):689–93. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (US) Estimated HIV incidence in the United States, 2007–2010. HIV Surveillance Supplemental Report. 2012. [cited 2013 Apr 19]. p. 17. Also available from: URL: http://www.cdc.gov/hiv/topics/surveillance/resources/reports/#supplemental.
- 3.Oster AM, Wiegand RE, Sionean C, Miles IJ, Thomas PE, Melendez-Morales L, et al. Understanding disparities in HIV infection between black and white MSM in the United States. AIDS. 2011;25:1103–12. doi: 10.1097/QAD.0b013e3283471efa. [DOI] [PubMed] [Google Scholar]
- 4.Prevalence and awareness of HIV infection among men who have sex with men—21 cities, United States, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(37):1201–7. [PubMed] [Google Scholar]
- 5.Hall HI, Holtgrave DR, Maulsby C. HIV transmission rates from persons living with HIV who are aware and unaware of their infection. AIDS. 2012;26:893–6. doi: 10.1097/QAD.0b013e328351f73f. [DOI] [PubMed] [Google Scholar]
- 6.Black AIDS Institute. Exit strategy: ending the AIDS epidemic in black America. 2012. [cited 2013 Feb 14]. Available from: URL: http://www.blackaids.org/images/media/12_exit.pdf.
- 7.Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL, 4th, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380:341–8. doi: 10.1016/S0140-6736(12)60899-X. [DOI] [PubMed] [Google Scholar]
- 8.Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14):1–17. [PubMed] [Google Scholar]
- 9.Millett GA, Ding H, Marks G, Jeffries WL, 4th, Bingham T, Lauby J, et al. Mistaken assumptions and missed opportunities: correlates of undiagnosed HIV infection among black and Latino men who have sex with men. J Acquir Immune Defic Syndr. 2011;58:64–71. doi: 10.1097/QAI.0b013e31822542ad. [DOI] [PubMed] [Google Scholar]
- 10.HIV testing among men who have sex with men—21 cities, United States, 2008. MMWR Morb Mortal Wkly Rep. 2008;60(21):694–9. [PubMed] [Google Scholar]
- 11.Results of the Expanded HIV Testing Initiative—25 jurisdictions, United States, 2007–2010. MMWR Morb Mortal Wkly Rep. 2011;60(24):805–10. [PubMed] [Google Scholar]
- 12.Pinkerton SD, Bogart LM, Howerton D, Snyder S, Becker K, Asch SM. Cost of OraQuick oral fluid rapid HIV testing at 35 community clinics and community-based organizations in the USA. AIDS Care. 2009;21:1157–62. doi: 10.1080/09540120902729940. [DOI] [PubMed] [Google Scholar]
- 13.White House, Office of National AIDS Policy (US) National HIV/AIDS strategy. 2010. [cited 2013 Apr 14]. Available from: URL: http://www.whitehouse.gov/administration/eop/onap/nhas.
- 14.Rapid HIV testing among racial/ethnic minority men at Gay Pride events—nine U.S. cities, 2004–2006. MMWR Morb Mortal Wkly Rep. 2007;56(24):602–4. [PubMed] [Google Scholar]
- 15.Bowles KE, Clark HA, Tai E, Sullivan PS, Song B, Tsang J, et al. Implementing rapid HIV testing in outreach and community settings: results from an Advancing HIV Prevention demonstration project conducted in seven U.S. cities. Public Health Rep. 2008;123(Suppl 3):78–85. doi: 10.1177/00333549081230S310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thomas PE, Walker A, Chavez PR. Using event-based HIV testing to increase awareness of HIV status and identify undiagnosed infection among black populations: the Behavioral Assessment and Rapid Testing (BART) project. Presented at the American Public Health Association 139th Annual Meeting and Exposition; 2011 Oct 29–Nov 2; Washington. [cited 2013 Nov 25]. Also available from: URL: https://apha.confex.com/apha/139am/webprogram/Paper239484.html. [Google Scholar]
- 17.SAS Institute, Inc. SAS®: Version 9.1.3. Cary (NC): SAS Institute, Inc.; 2010. [Google Scholar]
- 18.Disparities in diagnoses of HIV infection between blacks/African Americans and other racial/ethnic populations—37 states, 2005–2008. MMWR Morb Mortal Wkly Rep. 2011;60(4):93–8. [PubMed] [Google Scholar]
- 19.Kaiser Family Foundation. Menlo Park (CA): Kaiser Family Foundation; 2010. The uninsured: a primer—key facts about health insurance on the eve of coverage expansions. [Google Scholar]
- 20.Callahan ST, Cooper WO. Uninsurance and health care access among young adults in the United States. Pediatrics. 2005;116:88–95. doi: 10.1542/peds.2004-1449. [DOI] [PubMed] [Google Scholar]
- 21.Dowshen N, Binns HJ, Garofalo R. Experiences of HIV-related stigma among young men who have sex with men. AIDS Patient Care STDS. 2009;23:371–6. doi: 10.1089/apc.2008.0256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21:2083–91. doi: 10.1097/QAD.0b013e3282e9a64b. [DOI] [PubMed] [Google Scholar]
- 23.Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39:446–53. doi: 10.1097/01.qai.0000151079.33935.79. [DOI] [PubMed] [Google Scholar]
- 24.Black AIDS Institute. Passing the test: the challenges and opportunities of HIV testing in black America. [cited 2014 Jan 29]. Available from: URL: http://www.blackaids.org/news-2009/355-passing-the-test-the-challenges-and-opportunities-of-hiv-testing-in-black-america.
- 25.Lanier Y, Sutton MY. Reframing the context of preventive health care services and prevention of HIV and other sexually transmitted infections for young men: new opportunities to reduce racial/ethnic sexual health disparities. Am J Public Health. 2013;103:262–9. doi: 10.2105/AJPH.2012.300921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kates J, Levi J. Insurance coverage and access to HIV testing and treatment: considerations for individuals at risk for infection and for those with undiagnosed infection. Clin Infect Dis. 2007;45(Suppl 4):S255–60. doi: 10.1086/522547. [DOI] [PubMed] [Google Scholar]
- 27.Thomas PE, Henry KD, Voetsch AC, Oster AM, Callaway D, Smith M, et al. A comparison of risk behaviors of non-gay-identified with gay-identified black men who have sex with men at Historically Black College and University settings. Presented at the American Public Health Association 137th Annual Meeting and Exposition; 2009 Nov 7–11; Philadelphia. [cited 2014 Jan 29]. Also available from: URL: https://apha.confex.com/apha/137am/webprogram/Paper209233.html. [Google Scholar]
- 28.Pant Pai N, Balram B, Shivkumar S, Martinez-Cajas JL, Claessens C, Lambert G, et al. Head-to-head comparison of accuracy of a rapid point-of-care HIV test with oral versus whole-blood specimens: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:373–80. doi: 10.1016/S1473-3099(11)70368-1. [DOI] [PubMed] [Google Scholar]


