Abstract
Purpose
Mid- and long-term follow-up of Charnley total hip arthroplasty (THA) demonstrated good functional results with 85 % survivorship at 25-year follow-up. However, dislocation still remains an unsolved problem. Dislocation may occur throughout the patient’s and implant’s life. The aim of this study is to answer the question: does a dual mobility cup (DMC) decrease the dislocation risk?
Methods
We report comparative results at ten years of follow-up of two groups of primary cemented Charnley-type THA, one with a standard polyethylene cup (group 1, n = 215) and the other one with a DMC (group 2, n = 105).
Results
In group 1, 26 dislocations (12.9 %) occurred. In group 2 only one dislocation (0.9 %) occurred. This dislocation was successfully reduced by closed reduction, without any recurrence. This difference was statistically significant (p = 0.0018). In group 1, the reason for revision was recurrent dislocation in 21 cases. Five patients were revised for other reasons. The global revision rate was 12.9 %. In group 2, two patients needed revision surgery for aseptic loosening. The global revision rate was 2.1 %. This difference was statistically significant (p = 0.054). The goal was reached for the patients of group 2 who had more risks factors for dislocation (age, aetiology, American Society of Anesthesiologists and Devane scores) than those of group 1.
Conclusions
When using a DMC, we observed a low rate of dislocation in primary THA (0.9 %). This surgical choice seems to be a safe and effective technique in Charnley-type THA, especially in a high-risk population.
Keywords: Arthroplasty replacement hip, Joint instability/prevention and control, Dislocation, Prosthesis design, Charnley total hip arthroplasty, Dual mobility cup
Introduction
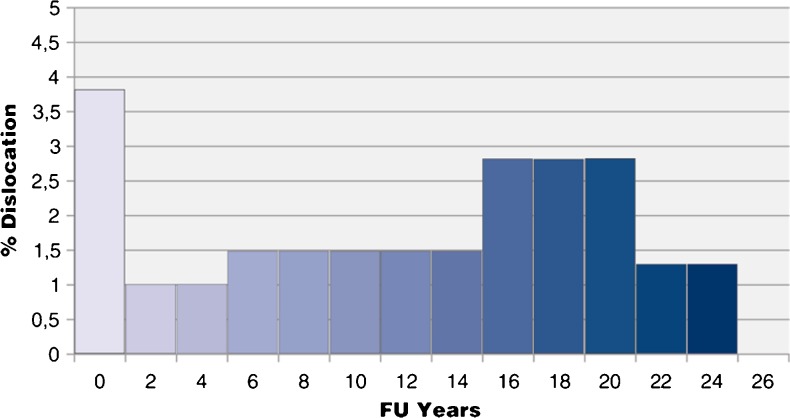
Mid- and long-term follow-up of Charnley total hip arthroplasty (THA) demonstrated good functional results as shown in different studies by ourselves in 2011 [1] with 85 % survivorship at 25-year follow-up. However, dislocation still remains an unsolved concern. Dislocation may occur throughout the patient’s and implant’s life and has been described as the cumulative risk of dislocation. This cumulative long-term risk of dislocation after primary Charnley THA was defined in 2004 by Caton and Merabet [2] (Fig. 1) and also by Berry et al. [3]. For Caton and Merabet [2] the dislocation rate was 3.8 % the first year and then rose to a rate of 1.39 % every five years to 10.4 % at 25 years with 6.9 % revision. For Berry et al., the cumulative risk of a first time dislocation was 1.9 % at one year and then increased at a crescent rate of 1 % every five years to 7 % at 25 years for patients who were still alive.
Fig. 1.
Cumulative risk of THA dislocation according to Caton and Merabet [2]
Today in the United States the main reason for revision in THA is dislocation, which represents 22.5 % [4] of revisions. In France, the dislocation rate commonly admitted is 8.5 % for primary and revision THA, but dislocation is the fourth cause for revision [5] (10.4 % of revisions due to recurrent dislocation).
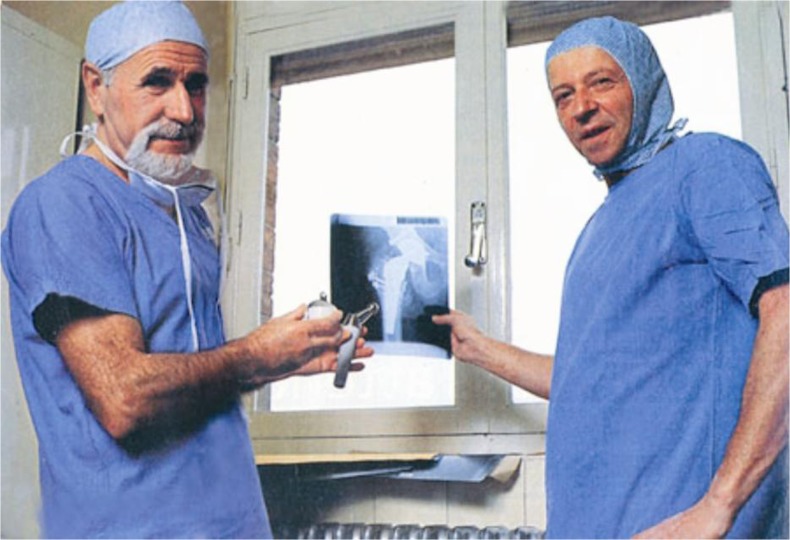
Compared to the data of Bozic et al. [4], the proportion of THA revision due to dislocation is lower in France. This could be explained by development of a dual mobility cup (DMC) in 1976 in Saint Etienne, France by Prof. Gilles Bousquet [6, 7] and engineer André Rambert (Fig. 2). The goals of this particular dual articulation were to decrease the dislocation risk by acting like a big ball and to preserve a normal range of motion. The aim of this study is to answer this question: does a DMC decrease the dislocation risk?
Fig. 2.
André Rambert (left) and Prof. Gilles Bousquet (right) presenting the first DMC (1976) (courtesy of L. Doursounian, Maîtrise orthopédique)
Materials and methods
In order to evaluate the efficiency of a DMC on dislocation risk, we report comparative results of two groups of primary cemented Charnley-type THA, one with a standard polyethylene cup (group 1: MBA®, Groupe Lépine, Genay, France) and the other one with a DMC (group 2: Quattro®, Groupe Lépine, Genay, France, previously reported [8]). This is a retrospective study of 306 patients (320 THAs) operated on from April 2000 to September 2002 by one senior surgeon (J.L. Prudhon) with a minimum follow-up of ten years.
Femoral implants used were cemented (Charnley Stallion®, Groupe Lépine, Genay, France) with a stem roughness of 0.6 μm and with a round highly polished 10-mm neck. The modular femoral head was stainless steel with a diameter of 22.2 mm. In group 1, the acetabular cup was a cementless hydroxyapatite (HA)-coated metal back with a fixed ultrahigh molecular weight polyethylene (UHMWPE) insert in 215 cases (Fig. 3a). In group 2, a cementless HA-coated metal back with a mobile UHMWPE insert was used in 105 cases (Fig. 3b). The DMC is an acetabular cup including two articular surfaces, one large and one small (Fig. 4). The femoral head is snapped in a retentive polyethylene liner; this liner moves freely inside the metallic cup. These THAs represent a consecutive series of primary hip replacement. All our THAs were recorded in a computer database (FileMaker Pro®).
Fig. 3.
Cemented Charnley-type stem with standard polyethylene MBA cup (a) or Quattro® DMC (b)
Fig. 4.

Quattro® DMC with four apical spikes, six fins and bilayer titanium and HA coating
In both groups THAs were performed through a posterolateral approach preserving the piriformis and quadratus femoris muscles and capsular repair. The femoral stem was cemented using a second-generation cementing technique. The target for cup positioning was 45° of abduction and 25° of anteversion. Full weight-bearing was allowed, and patients were discharged at day 7.
In 2012, an attempt to reach all the patients by mail or phone call was carried out. If the patient was reached and accepted an outpatient visit, an appointment was set up, otherwise data were collected by mail or phone call. If the patient could not be reached, data of the last outpatient visit were used. We have considered as lost to follow-up any patients who never returned to any routine visits.
Preoperative data consisted of age at index surgery, gender, American Society of Anesthesiologists (ASA) score, Charnley grade, Postel-Merle d’Aubigné (PMA) [9] score, Devane [10] activity score, side affected, specifications of the implants and surgical approach.
Post-operative data comprised the occurrence of complications (requiring or not requiring revision surgery), Devane activity score, complications, vital status, PMA score and radiological evaluation at the longest follow-up (pelvis in the frontal plane and hip in a sagittal plane). Specific criteria evaluated were: femoral head migration according to the centre of the metal back, lucent lines and osteolysis.
Statistical analysis
The comparison of qualitative variables was performed by chi-square test (or Fisher’s exact test according to validity conditions). The comparison of quantitative variables was performed by sample t test. The significance threshold was set at 0.05. Qualitative variables were presented as percentage and quantitative variables as mean or median, standard deviation and range.
Results
Pre-operative population
The mean age of the patients in group 1 was lower at 70.8 years (n = 204, range 50–88) than in group 2 at 78.0 years (n = 102, range 39.8–93.5) (p < 0.001). A comparison of gender, aetiology, ASA score, Charnley’s classification, Devane score and acetabular cup size in the two series is presented in Table 1. Charnley’s classification, acetabular cup size and sex ratio were comparable between the two groups, with a majority of female patients in both groups (57.5 % in group 1 and 59.8 % in group 2). However, there was a difference between the mean pre-operative PMA score (7.2 of 18 points in group 1 and 5.9 of 18 points in group 2), ASA score (83.6 % ASA 2 in group1 and 73.2 % ASA 2 in group 2), Devane score (64 patients were grade 4 in group 1 and only three patients were grade 4 in group 2) and aetiology. Aetiologies are presented in Table 1 with osteoarthritis in the majority of cases (97 % in group 1 and 90.4 % in group 2). There was no neck fracture operated on in group 1 and 3.8 % of neck fractures in group 2.
Table 1.
Comparability of groups 1 and 2
| Parameters | Group 1 (n = 215) | Group 2 (n = 105) | p |
|---|---|---|---|
| Gender, % | |||
| Women | 57.5 % | 59.8 % | NS |
| Age, years | |||
| Mean (min.–max.) | 70.8 (50–88) | 78.0 (39.8–93.5) | <0.001 |
| ASA score, % | |||
| 1 | 4.1 | 9.9 | <0.01 |
| 2 | 83.6 | 73.2 | |
| 3 | 12.3 | 16.9 | |
| Devane score, % | |||
| 1 | 0.0 | 1.0 | <0.001 |
| 2 | 5.9 | 55.1 | |
| 3 | 56.2 | 40.8 | |
| 4 | 37.9 | 3.1 | |
| Charnley classification, % | |||
| A | 66.0 | 54.8 | NS |
| B | 29.8 | 41.3 | |
| C | 5.0 | 3.8 | |
| PMA preoperative, points | |||
| Mean (min.–max.) | 7.2 (3–10) | 5.9 (3–9) | <0.001 |
| Aetiology, % | |||
| Osteoarthritis | 97.0 | 90.4 | <0.001 |
| Osteonecrosis | 1.0 | 5.8 | |
| Neck fracture | 0.0 | 3.8 | |
| Rheumatoid arthritis | 2.0 | 0.0 | |
| Acetabular cup size, % | |||
| 48 mm | 10.7 | 11.4 | NS |
| 50 mm | 31.2 | 32.4 | |
| 52 mm | 24.7 | 23.8 | |
| 54 mm | 21.4 | 21.0 | |
| 56 mm | 9.3 | 9.5 | |
| 58 or 60 mm | 2.8 | 1.9 | |
NS not significant
In group 1, 10 patients (4.9 %) died since the index surgery of unrelated causes and 14 patients were lost to follow-up (6.8 %). In group two, 24 patients (23.5 %) died since the index surgery of unrelated causes and nine patients were lost to follow-up (8.8 %).
Post-operative results
Results regarding dislocation at ten years of follow-up
In group 1, 26 dislocations (12.9 %) occurred. Five dislocations occurred before the three months after surgery had occurred and five were recurrent. The acetabular cup size in this group did not influence the dislocation rate: cup size smaller than 56 mm (23 cups, 12.1 %) and equal to or higher than 56 mm (three cups, 11.5 %); the difference was not statistically significant (p = 0.82). Only one dislocation (0.9 %) occurred in group 2 in a patient who fell down one month after the index surgery. This dislocation was successfully reduced by closed reduction, without any recurrence. This difference between the two groups was statistically significant (p = 0.0018).
Results regarding revision at 10 years of follow-up
In group 1, 26 patients (12.9 %) were revised. The reason for revision was recurrent dislocation in 21 cases and loosening of one or both components in five cases (two cups with wear and three stems). In group 2, two patients (2.1 %) needed revision surgery (infection excluded): none for dislocation and two for aseptic loosening (one cup and one femur). This difference was statistically significant (p = 0.054). There was no septic revision in group 1 and one in group 2.
Discussion
Risk factors for dislocation have been described by Woolson and Rahimtoola [11] and Peter et al. [12] considering patient factors, implant factors and surgical factors. According to Guyen et al. [13], we may consider that all the patients of group 2 had higher risk for dislocation than patients of group 1 (age, aetiology, pre-operative PMA score and Devane score).
The goal was reached for the patients of group 2 with the Quattro DMC: only one dislocation occurred. However, patients were older and had higher dislocation risk factors compared to the patients of group 1 [mean age of 78 years compared to 70 years for group 1 (p < 0.001) and 3.8 % of neck fractures in group 2, but no neck fracture in group 1].
Vielpeau et al. [14, 15] published the same results in 2011 regarding dislocation with a rate of 1.15 % in a series of cemented non-modular Charnley-type THA with a 22.2-mm metallic head and a Bousquet-type DMC (SERF). Leclercq et al. [15] recently published the same results with the Evora chromium-cobalt DMC. At a minimum follow-up of ten years, they had no dislocation and 0.5 % revision rate (n = 200 DMC).
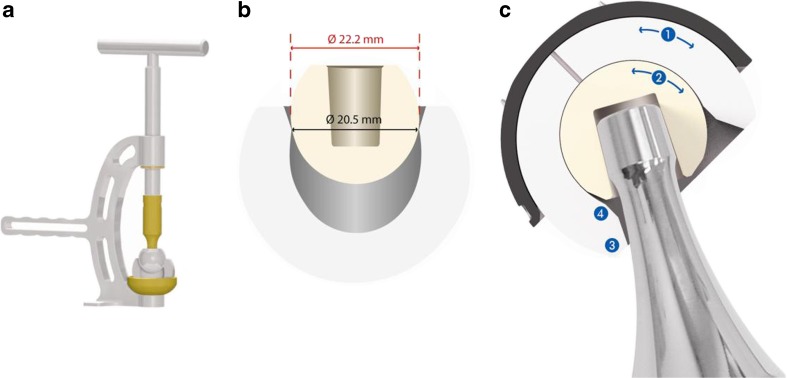
Regarding the wear process, three indirect radiological signs could appear with standard cups: femoral head migration and osteolysis with or without loosening. A more specific wear process in the DMC is polyethylene wear located at the third joint (Fig. 5). This specific wear could weaken the retaining device and induce pseudo-dislocation, a so-called intra-prosthetic dislocation as reported by Lecuire et al. [16].
Fig. 5.
a Head impactor. b Dual mobility retaining mechanism. c DMC three joints: 1 larger joint, 2 smaller joint, 3 third joint, 4 chamfer
So, in our series we did not report intra-prosthetic dislocation due to wear of the PE insert as described by Vielpeau et al. [14], Lecuire et al. [16] and Philippot et al. [17] on the first generation of the Bousquet-type DMC. Four main reasons may be advocated: (1) the retentive mechanism has been designed with an entry diameter of 20.5 mm for a head diameter of 22.22 mm, (2), the snapping mechanism needs a force of 145 daN for impaction or extraction of the 22.22-mm head (Fig. 5), (3) the PE inlay has a high covering collar to obtain 50 % more resistance to deformation and to avoid plastic deformation when snapping the metallic head and (4) contact at the third joint was optimised thanks to a specific design of the PE inlay (chamfer) and a 10-mm reduced and highly polished round neck.
We noted only one cup loosening at the ten year follow-up. This could be due to a reproducible and reliable fixation: (1) four spikes prevent tilting and improve primary stability, and (2) bilayer coating of porous titanium and HA provides an anchorage volume to achieve secondary fixation. These specifications have been developed to prevent failures (3.3 % revision rate for cup loosening) of the first generation of the Novae Bousquet-type DMC coated with alumina [17].
As known, the rate of revision for dislocations is high and increases with the worldwide incidence of primary THA. This rate (10.4 %) is lower in France [5, 18] compared to 27.0 % observed in the New Zealand Joint Registry [19]. The literature about the DMC has been mainly in French since 1993 [5–8, 12–16], but not only since 2012 [20–22].
Excluding primary THA, in France the DMC is widely used (62 %) in revision surgery as noted by Delaunay et al. [5]. The rate of dislocation after revision surgery is quite low (4 %) [18] compared to the usual rate in other surveys without a DMC (5–30 %) [5]. This “French cultural trend in the choice of implants” could be considered as a “new French paradox”.
In this study, we observed a low rate of dislocation in primary THA (less than 1.0 %) when using a Quattro® DMC. This surgical choice seems to be a safe and effective technique in Charnley-type THA, especially for high-risk patients.
Acknowledgments
Disclosures
Jacques H. Caton, Jean-Louis Prudhon and André Ferreira are consultants of Groupe Lépine. Thierry Aslanian and Régis Verdier are employed by Groupe Lépine.
References
- 1.Caton J, Prudhon JL. Over 25 years survival after Charnley’s total hip arthroplasty. Int Orthop. 2011;35:185–188. doi: 10.1007/s00264-010-1197-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Caton J, Merabet Z (2004) Hip dislocation and outcome. In: MCI France (ed) La prothèse totale de hanche, pp 223–227. Lyon
- 3.Berry DJ, von Knoch M, Schleck CD, Harmsen WS. The cumulative long-term risk of dislocation after primary Charnley total hip arthroplasty. J Bone Joint Surg Am. 2004;86-A:9–14. doi: 10.2106/00004623-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:128–133. doi: 10.2106/JBJS.H.00155. [DOI] [PubMed] [Google Scholar]
- 5.Delaunay C, Hamadouche M, Girard J, Duhamel A, SoFCOT Group What are the causes for failures of primary hip arthroplasties in France? Clin Orthop Relat Res. 2013;471:3863–3869. doi: 10.1007/s11999-013-2935-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aubriot JH, Lesimple P, Leclercq S. Study of Bousquet’s non-cemented acetabular implant in 100 hybrid total hip prostheses (Charnley type cemented femoral component). Average 5-year follow-up. Acta Orthop Belg. 1993;59(Suppl 1):267–271. [PubMed] [Google Scholar]
- 7.Philippot R, Adam P, Farizon F, Fessy M-H, Bousquet G. Survie à dix ans d'une cupule double mobilité non cimentée. Rev Chir Orthop. 2006;92:326–331. doi: 10.1016/s0035-1040(06)75762-2. [DOI] [PubMed] [Google Scholar]
- 8.Prudhon JL, Ferreira A, Verdier R. Dual mobility cup: dislocation rate and survivorship at ten years of follow-up. Int Orthop. 2013;37:2345–2350. doi: 10.1007/s00264-013-2067-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.D’Aubigne RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–475. [PubMed] [Google Scholar]
- 10.Devane PA, Horne JG, Martin K, Coldham G, Krause B. Three-dimensional polyethylene wear of a press-fit titanium prosthesis. Factors influencing generation of polyethylene debris. J Arthroplasty. 1997;12:256–266. doi: 10.1016/S0883-5403(97)90021-8. [DOI] [PubMed] [Google Scholar]
- 11.Woolson ST, Rahimtoola ZO. Risk factors for dislocation during the first 3 months after primary total hip replacement. J Arthroplasty. 1999;14:662–668. doi: 10.1016/S0883-5403(99)90219-X. [DOI] [PubMed] [Google Scholar]
- 12.Peter R, Lübbeke A, Stern R, Hoffmeyer P. Cup size and risk of dislocation after primary total hip arthroplasty. J Arthroplasty. 2011;26:1305–1309. doi: 10.1016/j.arth.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 13.Guyen O, Pibarot V, Vaz G, Chevillotte C, Carret JP, Bejui-Hugues J. Unconstrained tripolar implants for primary total hip arthroplasty in patients at risk for dislocation. J Arthroplasty. 2007;22:849–858. doi: 10.1016/j.arth.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 14.Vielpeau C, Lebel B, Ardouin L, Burdin G, Lautridou C. The dual mobility socket concept: experience with 668 cases. Int Orthop. 2011;35:225–230. doi: 10.1007/s00264-010-1156-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leclercq S, Benoit JY, de Rosa JP, Tallier E, Leteurtre C, Girardin PH. Evora chromium-cobalt dual mobility socket: results at a minimum 10 years’ follow-up. Orthop Traumatol Surg Res. 2013;99:923–928. doi: 10.1016/j.otsr.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 16.Lecuire F, Benareau I, Rubini J, Basso M. Intra-prosthetic dislocation of the Bousquet dual mobility socket. Rev Chir Orthop Reparatrice Appar Mot. 2004;90:249–255. doi: 10.1016/S0035-1040(04)70101-4. [DOI] [PubMed] [Google Scholar]
- 17.Philippot R, Camilleri JP, Boyer B, Adam P, Farizon F. The use of a dual-articulation acetabular cup system to prevent dislocation after primary total hip arthroplasty: analysis of 384 cases at a mean follow-up of 15 years. Int Orthop. 2009;33:927–932. doi: 10.1007/s00264-008-0589-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Girard J, Kern G, Migaud H, Delaunay C, Ramdane N, Hamadouche M. Primary total hip arthroplasty revision due to dislocation: prospective French multicenter study. Orthop Traumatol Surg Res. 2013;99:549–553. doi: 10.1016/j.otsr.2013.03.026. [DOI] [PubMed] [Google Scholar]
- 19.(2013) The New Zealand Joint Registry. Fourteen year report. January 1999 to December 2012. In New Zealand Joint Registry
- 20.Lachiewicz PF, Watters TS. The use of dual-mobility components in total hip arthroplasty. J Am Acad Orthop Surg. 2012;20:481–486. doi: 10.5435/JAAOS-20-08-481. [DOI] [PubMed] [Google Scholar]
- 21.McArthur BA, Nam D, Cross MB, Westrich GH, Sculco TP. Dual-mobility acetabular components in total hip arthroplasty. Am J Orthop (Belle Mead NJ) 2013;42:473–478. [PubMed] [Google Scholar]
- 22.Plummer DR, Haughom BD, Della Valle CJ. Dual mobility in total hip arthroplasty. Orthop Clin North Am. 2014;45:1–8. doi: 10.1016/j.ocl.2013.08.004. [DOI] [PubMed] [Google Scholar]