Abstract
Purpose
Limited evidence exists regarding the outcomes of hip resurfacing in elderly patients. The primary study aims were to determine the survival and functional outcome following Birmingham Hip Resurfacing (BHR) in patients ≥65 years at up to ten years of follow-up. Secondary aims were to explore factors affecting survival and functional outcome.
Methods
Between 1997 and 2012, data were prospectively collected on 180 BHR (162 patients; mean age 69.2 years; 62 % male) implanted by one designing surgeon. Mean follow-up was six (range one to 14.4) years with no loss to follow-up. Outcomes of interest were implant survival, functional outcome [Oxford Hip Score (OHS)] and radiological evidence of implant failure.
Results
Three hips were revised, giving an overall cumulative survival of 96.4 % [95 % confidence interval (CI) 90.3–100] at ten years. Survival of 111 male BHR was 98.9 % (95 % CI 94.8–100) at ten years (one revision) compared with 91.9 % (95 % CI 77.0–100) in 69 female BHR (two revisions). Survival was affected by age (p = 0.014) and femoral head size (p = 0.024) but not by gender (p = 0.079). Median pre-operative OHS was 50.0 % [interquartile range (IQR) 37.5–68.8], improving to 4.4 % (IQR 0–10.4) postoperatively. Men had significantly better postoperative OHSs compared with women (median male OHS 2.1 % versus 6.3 % female OHS; p = 0.021).
Conclusions
Good survival and functional outcomes were achieved with the BHR at ten years in men and women ≥65 years. Despite registry findings to the contrary, age alone should not be a contraindication for hip resurfacing in centres with expertise in this procedure.
Keywords: Hip resurfacing, Functional outcome, Survival, Gender, Head size, Age
Introduction
Hip resurfacing is a recognised treatment for young and active patients with painful hip arthritis [1]. Good survival and functional outcome is reported for hip resurfacing in young patients at up to ten years of follow-up by both designer surgeons [1–3] and independent centres [4–11]. It was previously advised that elderly patients, typically ≥65 years, should not be considered for hip resurfacing [12, 13]. This is partly because total hip replacement (THR) is an established procedure with consistently good outcomes reported in elderly patients [14, 15]. In addition, older patients are generally considered less active and more likely to have poor bone quality compared with younger patients; this poor bone quality may increase the risk of femoral neck fracture or femoral component loosening [13, 16, 17], and therefore, excluding such patients as suitable candidates for hip resurfacing. Indeed, a report from the Australian registry demonstrated an increased risk of subsequent revision in patients undergoing hip resurfacing with increasing age, an observation contrary to the findings following conventional THR [18]. However, only a few studies have reported specifically on elderly patients undergoing hip resurfacing. These studies demonstrate good outcomes may be achieved in older patients, comparable with younger individuals undergoing the same procedure [19–21].
The primary study aims were to determine survival and functional outcome following Birmingham Hip Resurfacing (BHR) in patients ≥65 years at up to ten years of follow-up. Secondary aims were to explore factors affecting survival and functional outcome.
Patients and methods
Between August 1997 and June 2012, data were prospectively collected on all consecutive BHR (Smith & Nephew, Warwick, UK) implanted in patients ≥65 years. All operations were performed by one designing surgeon at a specialist arthroplasty centre. Information regarding all inclusion criteria, patient selection, operative technique and routine follow-up was previously described in detail [1, 22]. In all cases, patients meeting inclusion criteria for hip resurfacing were counselled pre-operatively with regards to risks and benefits of both hip resurfacing and THR. Patients subsequently made an informed decision as to whether or not they wished to proceed with hip resurfacing. Data were extracted from the institution’s prospectively maintained database (MySQL) specifically on patient demographics, primary indication for BHR and size of implanted component (Table 1). This study was approved and registered with the institutional review board.
Table 1.
Summary of the study cohort
| Study variables | Patient characteristics | Data (n = 180 hips) |
|---|---|---|
| Gender | Male | 111 (61.7 %) |
| Female | 69 (38.3 %) | |
| Age | Mean (range) in years | 69.2 (65.0–82.7) |
| Bilateral hips | Total patients | 18 (36 hips) |
| Single-stage bilateral procedures | 8 (16 hips) | |
| Two-stage bilateral procedures | 10 (20 hips) | |
| Diagnosis | Primary osteoarthritis | 180 (100 %) |
| Follow-up time | Mean (range) in years | 6.0 (1.0–14.4) |
| Surgical approach | Posterior | 180 (100 %) |
| Femoral component size | 42 mm | 11 (6.1 %) |
| 46 mm | 49 (27.2 %) | |
| 50 mm | 68 (37.8 %) | |
| 54 mm | 47 (26.1 %) | |
| 58 mm | 5 (2.8 %) |
All patients were reviewed at six weeks and six months postoperatively in the outpatient clinic and then annually from the date of index BHR procedure. Each consultation comprised clinical examination, anteroposterior pelvic radiographs and completion of the Oxford Hip Score (OHS) questionnaire [1, 22]. Patients who had not been reviewed within 12 months of study commencement were sent a postal questionnaire, with those failing to respond subsequently contacted by telephone to complete data collection. The questionnaire involved providing details on any further surgical intervention, including revision, that the patient may have had on the ipsilateral hip. If a revision procedure was performed, details of the surgery, revision indication and intra-operative findings were obtained from the treating hospital. As part of the postal questionnaire, patients were asked to complete the OHS as a measure of postoperative pain and disability [23]. The OHS is expressed as a percentage (healthy joint scoring 0 % and worst possible joint 100 %), with questionnaires considered valid if they met the minimum inclusion criteria previously described [24, 25]. All deaths were recorded; using patient case notes and details held by the general practitioner, it was possible to determine whether the death was related to the BHR surgery and whether the hip had been revised or remained in situ at the time of death.
All anteroposterior pelvic radiographs available at latest follow-up were analysed for signs suggestive of implant failure. The femoral component was considered to have evidence of loosening if there was a radiolucent line >2 mm in any of the three zones described by Amstutz et al. [26]. Acetabular loosening was defined as a radiolucent line >2 mm in two or more zones described by DeLee and Charnley [27]. Osteolysis around the femoral or acetabular components, femoral-neck narrowing [28], evidence of heterotopic ossification [29] and evidence of femoral neck to cup impingement [30] were also recorded. BHR acetabular component inclination and femoral component stem-shaft angle were measured in each radiograph, as previously described [28].
Statistical analysis
All statistical analysis was performed using the R programme [31]. Cumulative BHR survival was determined using the Kaplan–Meier method. The endpoint for survival analysis was revision surgery, defined as removal or exchange of one or both hip resurfacing components. Patients not undergoing revision surgery were censored after their last contact with the hospital, whether it was in the clinic or by completing the postal or telephone questionnaire, or after death. A Cox proportional hazards model was used to compare differences in BHR survival distributions for each covariate recorded (patient age, gender, femoral-head size). A multivariate model was constructed, and covariates that were not significantly influential were systematically removed from the model to identify those having the greatest influence on survival. Depending on data distribution, either mean and range or median and interquartile range (IQR) were reported. Mood’s test was used to compare OHS between men and women. The level of significance was set at 95 % (p < 0.05), with confidence intervals (CI) also at the 95 % level.
Results
Survival analysis and factors affecting survival
During the study period, 1,552 BHR were performed by the operating surgeon at this centre. Of these, 180 (11.6 %) were performed in 162 patients ≥65 years (Table 1). The final outcome was obtained in all patients during this study, with no patient lost to follow-up. There were 14 patient deaths (14 hips) during follow-up at a mean of 5.2 (range 1.2–11.9) years from the index procedure. All deaths were unrelated to the index BHR surgery.
Three BHR (1.7 %) in three patients underwent revision arthroplasty (Table 2). Two of the three revisions (patients 2 and 3 in Table 2) were performed at other institutions, with the third revision performed by the same surgeon as the primary BHR. Two revisions (patients 1 and 3 in Table 2) were previously described in detail [1, 22]. The other revision (patient 2 in Table 2) was a male patient previously asymptomatic but who suffered a high-energy fall whilst skiing and sustained a subtrochanteric fracture below his BHR. This was treated as described (Table 2), and during follow-up, there was radiological fracture union with no subsequent complications. Excluding these revisions, one patient developed a superficial wound infection that required surgical exploration, washout and debridement 1.5 months following primary BHR. There was no deep infection observed during re-exploration; therefore, the patient was treated with implant retention and a course of antibiotics IV, with no further complications during follow-up. Apart from this case, no further surgical interventions were performed in the remaining BHR cohort.
Table 2.
Clinical details of Birmingham Hip Resurfacings (BHR) requiring revision surgery (n = 3)
| Patient number | Age, sex, diagnosis | Femoral head size (mm) | Time to revision | Revision indication | Revision performed | Outcome after revision |
|---|---|---|---|---|---|---|
| 1 | 75 F | 46 | 1.4 years | Deep infection | Bipolar cemented Exeter stem/cemented cup/MoP | Died 4.5 years after revision |
| OA | ||||||
| 2 | 69 M | 50 | 1.7 years | Subtrochanteric fracture (high-energy) | Echelon uncemented stem with trochanteric cable plate/MoM | No complications after 2 years |
| OA | ||||||
| 3 | 73 F | 42 | 9.5 years | Adverse reaction to metal debris | Cemented Exeter stem/cemented cup/MoP | Re-revision for recurrent dislocations |
| OA |
M male, F female, OA osteoarthritis, MoM metal-on-metal, MoP metal-on-polyethylene
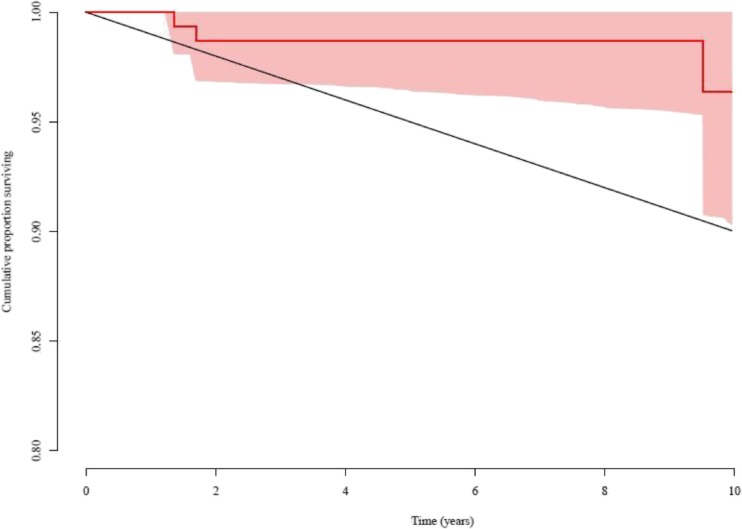
Cumulative survival for all BHR (n = 180) was 96.4 % (95 % CI 90.3–100) at ten years (34 hips at risk) (Fig. 1). The cumulative survival for 111 BHR implanted in male patients was 98.9 % (95 % CI 94.8–100) at ten years (23 hips at risk), with one hip requiring revision. The cumulative survival for 69 BHR implanted in female patients was 91.9 % (95 % CI 77.0–100) at ten years (11 hips at risk), with two hips requiring revision.
Fig. 1.
Kaplan–Meier survival curve for all Birmingham Hip Resurfacing (n = 180). Revision for any indication used as the endpoint for survival, with three hips revised. Shaded area represents the upper and lower limits of the 95 % confidence intervals. Black line represents the National Institute for Health and Clinical Excellence (NICE) recommendations for implant survival (acceptable implant failure rate of up to 1 % per year)
A Cox proportional hazard model demonstrated a significantly increased risk of BHR revision with increasing age (1.42 for each increased year of age since index surgery; p = 0.014) and a significantly decreasing risk of revision with larger femoral-head sizes (0.682 for each millimetre increase; p = 0.024). Male gender was associated with a 0.048 reduced risk of BHR revision compared with female gender; however this was not statistically significant (p = 0.079).
Functional outcome
A total of 519 OHS questionnaires meeting the inclusion criteria were completed by the cohort. The median absolute pre-operative OHS was 50.0 % (IQR 37.5–68.8) and median absolute postoperative OHS 4.4 % (IQR 0–10.4). Median male absolute postoperative OHS was 2.1 % (IQR 0–6.9) compared with 6.3 % (IQR 0–13.6) in women. This difference was statistically significant (p = 0.021).
Radiological analysis
Pelvic radiographs were available for review at the time of latest follow-up in 59 % of patients (105 of 177 hips) not requiring BHR revision surgery. Mean acetabular component inclination was 43.0° (range 28.4–60.2°), and mean femoral component stem-shaft angle was 137.2° (range 119.3º–150.0°), with a mean valgus of 4.6° (range 0º–18.5°). There was no change in any of these angles from the immediate postoperative radiographs; none of the radiographs demonstrated evidence of loosening of the femoral or acetabular components. There were ten cases (9.5 % of available radiographs) of asymptomatic heterotopic ossification (Brooker grade I = 5 hips; grade II = 3 hips; grade III = 2 hips). There were three cases (2.9 % of available radiographs) of asymptomatic nonprogressive femoral-neck osteolysis (Gruen zone 1 = 2 hips; zone 2 = 1 hip). No cases of metaphyseal stem or acetabular osteolysis were observed. There were two hips (1.9 % of available radiographs) with evidence of asymptomatic femoral-neck to cup impingement and one hip (1.0 % of available radiographs) with nonprogressive asymptomatic femoral-neck narrowing.
Blood-metal ion concentrations
In line with current recommendations, symptomatic BHR patients underwent measurement of blood metal ion concentrations [32]. Of 177 surviving BHR, 15 hips (15 patients) required blood metal ion sampling at a mean of 4.9 (range 1.3–13.0) years from index arthroplasty. All measured blood cobalt and chromium concentrations were below the recommended thresholds of seven parts per billion [32]; therefore, no patient underwent any periprosthetic imaging studies.
Discussion
Few studies to date have reported on the outcome of hip resurfacing in elderly patients (i.e. ≥65) [19–21]. This series represents the largest elderly patient cohort undergoing hip resurfacing reported in the literature. Findings demonstrate good survival and functional outcomes with the BHR in both male and female patients ≥65 at up to ten years of follow up. Overall ten year BHR survival was 96.4 %, which is comparable with that reported in a smaller designer-surgeon series (96.7 %) using a different hip resurfacing implant in elderly patients (Table 3) [21]. In addition, the ten year survival for men (98.9 %) and women (91.9 %) was not significantly different, with survival for both genders within acceptable limits recommended by the National Institute for Health and Clinical Excellence (NICE) (revision rate ≤10 % at ten years for continued use of an implant) [33]. In contrast, a previous multisurgeon series of BHR patients ≥70 years demonstrated a significantly higher revision rate in women compared with men, with all female failures due to femoral-neck fracture and occurring early following BHR [20]. The higher prevalence of femoral-neck fracture in elderly women in the previous study (15.8 %) [20] compared with this series (0 %) emphasises the importance of patient selection (especially in elderly patients who may have poor bone quality) and surgical technique, both of which can contribute to this unique complication of hip resurfacing [34, 35].
Table 3.
Comparison of study results with previous reports on elderly patients undergoing hip resurfacing
| This study | Carrothers [20] | Le Duff [21] | |
|---|---|---|---|
| Number of hip resurfacings | 180 BHR | 106 BHR | 99 Conserve Plus |
| Patients | 162 | 106 | 87 |
| Mean age (range) in years | 69 (65-83) | 73 (70-88) | 68 (65–83) |
| Male (n) | 62 % (111) | 67 % (NS) | 76 % (76) |
| Mean (range) follow-up time in years | 6.0 (1.0-14.4) | 7.1 (0.5-10.9) | 5.5 (2–13) |
| 10-year survival (95 % confidence intervals) | 96.4 % (90.3 to 100) | NS | 96.7 % (86.3–99.2) |
| Hips revised (n) | 1.7 % (3) | 3.8 % (4) | 3.0 % (3) |
| Mean (range) time to revision in years | 4.2 (1.4-9.5) | 0.41 (0.06-1.4) | 5.4 (0.13–10.8) |
| Indications for revision (n) | Deep infection (1) | Femoral-neck fracture (4) | Femoral-neck fracture (1) |
| Subtrochanteric fracture (1) | Aseptic loosening femoral component (1) | ||
| ARMD (1) | Likely ARMD (1) |
BHR Birmingham Hip Resurfacing, ARMD adverse reaction to metal debris, NS not stated
BHR survival reported in this elderly cohort at ten years (96.4 %) is comparable with that achieved by the same surgeon in patients <50 years (96.3 % at 10 years) [36] and independent reports on BHR survival [4–6, 8, 9]. The consistently good medium- to long-term BHR results reported from this centre [1, 22, 25, 36] may be a reflection of careful patient selection (including the avoidance of performing BHR in elderly patients with abnormal hip anatomy or dysplasia given previously reported poorer outcomes in younger patients with these diagnoses) [37, 38], surgical experience with a technically demanding procedure [39] and the use of an implant with more favourable outcomes than other hip-resurfacing designs [14, 18]. In this elderly cohort, larger femoral-head sizes were associated with reduced revision risk, which is similar to findings observed in younger BHR patients [5, 6, 36]. There is obviously an interaction between femoral-head size and gender with reference to implant survival. Study findings reported here concur with previous reports that femoral component size, and not gender, has the greatest influence on subsequent risk of revision [25].
The limited evidence available for hip resurfacing in elderly patients is partly because THR produces consistently good outcomes in this age group [14, 15]. In addition, the Australian registry demonstrated an increased risk of subsequent revision in patients undergoing hip resurfacing with increasing age, as well as elderly patients being more commonly revised for femoral-neck fractures [18]. A significantly increased risk of BHR revision with increasing age was also demonstrated in this elderly cohort. However, this increased risk of revision needs to be balanced with other advantages that hip resurfacing may provide to elderly patients. A recent analysis of registry data demonstrated a significantly lower mortality rate following BHR compared with uncemented and cemented THR in men of all ages [40]. These findings were subsequently independently confirmed in both male and female patients by an analysis of data from the English Hospital Episode Statistics database and Office for National Statistics [41].
Functional outcome following hip arthroplasty in elderly patients is an important consideration given the increasing ageing population. Studies suggest that elderly patients now have increased functional and activity expectations following arthroplasty, and this group may even outlive the lifespan of a standard THR [20, 42–45]. Hip resurfacing may provide an alternative in this subgroup of elderly patients wishing to maintain high levels of activity, with a previous study demonstrating patients ≥55 years were significantly more likely to participate in athletic activity following hip resurfacing than younger patients [45]. In the study reported here, functional outcome following BHR assessed using the OHS was excellent with most elderly patients being almost completely asymptomatic (median OHS 4.4 %; 25th percentile scoring 0 %). Similar functional outcomes are reported following hip resurfacing in elderly patients [19–21]. Two studies demonstrated elderly patients undergoing hip resurfacing achieved good to excellent functional outcomes comparable with younger patients [19, 20], with the latter study observing no difference in functional recovery rates between groups at up to one year [20]. Findings presented here support this observation, with an OHS (median 4.4 %) similar to that in patients up to 50 years of age undergoing BHR by the same surgeon (median OHS 4.2 %) [36]. A recent nonmatched study of patients undergoing hip resurfacing and THR demonstrated significantly better postoperative pain, function and activity scores in the resurfacing group [21]. Although there was no matched patient group undergoing THR for this study, the functional outcome in elderly BHR patients (median OHS 4.4 %) represents a clinically significant difference compared with our institution’s historic results following THR (median OHS 20.8 %) [24].
Findings presented here suggest that BHR provides an alternative to THR in carefully selected elderly patients wishing to maintain high levels of activity. In addition to routine pre-operative counseling regarding potential risks associated with metal-on-metal bearings [6, 46], elderly patients meeting the standard indications for hip resurfacing [2] must undergo assessment of bone mineral density (BMD) both pre-operatively and intra-operatively. Patients should be informed pre-operatively that THR may be required if the surgeon has concerns about BMD intra-operatively, though investigations such as dual-energy X-ray absorptiometry (DEXA) scans can be performed pre-operatively to assess this parameter in more detail [18]. However, we concur with previous recommendations that hip resurfacing in elderly patients should only be considered in institutions in which there is expertise in performing this procedure [21].
This study has some recognised limitations. This consecutive series was performed by a designing surgeon; therefore, it is important to recognise the results achieved with this technically demanding procedure may not be achievable and reproducible when the surgery is performed by others. However, the series includes the surgeon’s learning curve with the BHR and spans a period during which subtle nuances of anteversion, combined anteversion and aiming for an acetabular inclination angle <45° were not fully appreciated when performing hip resurfacing [40]. As radiographic analysis was not available in all cases at latest follow-up, it is possible that some individuals may have radiological evidence suggestive of implant failure despite implant and functional outcome determination in all cases. Previous ten year reports on resurfacing encountered similar difficulties in obtaining complete radiological review [4, 6]. Blood metal ion levels were not available for analysis for most patients in this cohort. However, this is in line with current recommendations that state asymptomatic hip resurfacing patients do not require such sampling [32].
In conclusion, this study demonstrates good survival and functional outcomes with the BHR in male and female patients ≥65 at up to ten years of follow-up. These findings support the limited evidence in the literature regarding the use of hip resurfacing in elderly patients [19–21]. As implant survival was within NICE recommendations, even for female patients, we consider the BHR provides an alternative to THR in carefully selected elderly patients who wish to maintain high levels of activity. However, hip resurfacing in elderly patients should only be performed by surgeons with expertise in this procedure. It is therefore recommended that age alone should not be used as a contraindication for hip resurfacing.
Acknowledgments
All work presented was carried out by the five listed authors.
Conflict of interest
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article. In addition, benefits have been or will be directed to a research fund, foundation, educational institution or other nonprofit organisation with which one or more of the authors are associated.
References
- 1.Treacy RB, McBryde CW, Shears E, Pynsent PB. Birmingham hip resurfacing: a minimum follow-up of ten years. J Bone Joint Surg [Br] 2011;93-B:27–33. doi: 10.1302/0301-620X.93B1.24134. [DOI] [PubMed] [Google Scholar]
- 2.McMinn DJ, Daniel J, Ziaee H, Pradhan C. Indications and results of hip resurfacing. Int Orthop. 2011;35:231–237. doi: 10.1007/s00264-010-1148-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amstutz HC, Le Duff MJ, Campbell PA, Gruen TA, Wisk LE. Clinical and radiographic results of metal-on-metal hip resurfacing with a minimum ten-year follow-up. J Bone Joint Surg Am. 2010;92-A:2663–2671. doi: 10.2106/JBJS.I.01715. [DOI] [PubMed] [Google Scholar]
- 4.Coulter G, Young DA, Dalziel RE, Shimmin AJ. Birmingham hip resurfacing at a mean of ten years: results from an independent centre. J Bone Joint Surg [Br] 2012;94-B:315–321. doi: 10.1302/0301-620X.94B3.28185. [DOI] [PubMed] [Google Scholar]
- 5.Holland JP, Langton DJ, Hashmi M. Ten-year clinical, radiological and metal ion analysis of the Birmingham Hip Resurfacing: from a single, non-designer surgeon. J Bone Joint Surg [Br] 2012;94-B:471–476. doi: 10.1302/0301-620X.94B4.27895. [DOI] [PubMed] [Google Scholar]
- 6.Murray DW, Grammatopoulos G, Pandit H, Gundle R, Gill HS, McLardy-Smith P. The ten-year survival of the Birmingham hip resurfacing: an independent series. J Bone Joint Surg [Br] 2012;94-B:1180–1186. doi: 10.1302/0301-620X.94B9.29462. [DOI] [PubMed] [Google Scholar]
- 7.Myers GJ, Morgan D, McBryde CW, O’Dwyer K. Does surgical approach influence component positioning with Birmingham Hip Resurfacing? Int Orthop. 2009;33:59–63. doi: 10.1007/s00264-007-0469-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ollivere B, Duckett S, August A, Porteous M. The Birmingham Hip Resurfacing: 5-year clinical and radiographic results from a District General Hospital. Int Orthop. 2010;34:631–634. doi: 10.1007/s00264-009-0821-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reito A, Puolakka T, Pajamäki J. Birmingham hip resurfacing: five to eight year results. Int Orthop. 2011;35:1119–1124. doi: 10.1007/s00264-010-1066-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Malek IA, Hashmi M, Holland JP. Socio-economic impact of Birmingham hip resurfacing on patient employment after ten years. Int Orthop. 2011;35:1467–1470. doi: 10.1007/s00264-010-1168-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schuh R, Neumann D, Rauf R, Hofstaetter J, Boehler N, Labek G. Revision rate of Birmingham Hip Resurfacing arthroplasty: comparison of published literature and arthroplasty register data. Int Orthop. 2012;36:1349–1354. doi: 10.1007/s00264-012-1502-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hing C, Back D, Shimmin A. Hip resurfacing: indications, results, and conclusions. Instr Course Lect. 2007;56:171–178. [PubMed] [Google Scholar]
- 13.Nunley RM, Valle Della CJ, Barrack RL. Is patient selection important for hip resurfacing? Clin Orthop Relat Res. 2009;467:56–65. doi: 10.1007/s11999-008-0558-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.No authors listed (2012) National Joint Registry for England and Wales. 9th Annual Report.http://www.njrcentre.org.uk/NjrCentre/Portals/0/Documents/England/Reports/9th_annual_report/NJR%209th%20Annual%20Report%202012.pdf (date last accessed 12 November 2013)
- 15.Garellick G, Kärrholm J, Rogmark C, Herberts P (2010) Swedish Hip Arthroplasty Register. Annual Report 2010. http://www.shpr.se/Libraries/Documents/AnnualReport-2010-2-eng.sflb.ashx (date last accessed 12 November 2013)
- 16.Mont MA, Seyler TM, Ulrich SD, et al. Effect of changing indications and techniques on total hip resurfacing. Clin Orthop Relat Res. 2007;465:63–70. doi: 10.1097/BLO.0b013e318159dd60. [DOI] [PubMed] [Google Scholar]
- 17.Gross TP, Liu F. Risk factor analysis for early femoral failure in metal-on-metal hip resurfacing arthroplasty: the effect of bone density and body mass index. J Orthop Surg Res. 2012;7:1. doi: 10.1186/1749-799X-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Prosser GH, Yates PJ, Wood DJ, Graves SE, de Steiger RN, Miller LN. Outcome of primary resurfacing hip replacement: evaluation of risk factors for early revision. Acta Orthop. 2010;81:66–71. doi: 10.3109/17453671003685434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McGrath MS, Desser DR, Ulrich SD, Seyler TM, Marker DR, Mont MA. Total hip resurfacing in patients who are sixty years of age or older. J Bone Joint Surg Am. 2008;90-A:27–31. doi: 10.2106/JBJS.H.00464. [DOI] [PubMed] [Google Scholar]
- 20.Carrothers AD, Gilbert RE, Richardson JB. Birmingham hip resurfacing in patients who are seventy years of age or older. Hip Int. 2011;21:217–224. doi: 10.5301/HIP.2011.6500. [DOI] [PubMed] [Google Scholar]
- 21.Le Duff MJ, Takamura KB, Amstutz HC. Metal-on-metal hip resurfacing in patients aged 65 or older. Hip Int. 2012;22:648–654. doi: 10.5301/HIP.2012.10350. [DOI] [PubMed] [Google Scholar]
- 22.Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty: a minimum follow-up of five years. J Bone Joint Surg [Br] 2005;87-B:167–170. doi: 10.1302/0301-620X.87B2.15030. [DOI] [PubMed] [Google Scholar]
- 23.Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg [Br] 1996;78-B:185–190. [PubMed] [Google Scholar]
- 24.Pynsent PB, Adams DJ, Disney SP. The Oxford hip and knee outcome questionnaires for arthroplasty. J Bone Joint Surg [Br] 2005;87-B:241–248. doi: 10.1302/0301-620X.87B2.15095. [DOI] [PubMed] [Google Scholar]
- 25.McBryde CW, Theivendran K, Thomas AM, Treacy RB, Pynsent PB. The influence of head size and sex on the outcome of Birmingham hip resurfacing. J Bone Joint Surg Am. 2010;92-A:105–112. doi: 10.2106/JBJS.I.00197. [DOI] [PubMed] [Google Scholar]
- 26.Amstutz HC, Beaule PE, Dorey FJ, Le Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Joint Surg Am. 2004;86-A:28–39. [PubMed] [Google Scholar]
- 27.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 28.Hing CB, Back DL, Bailey M, et al. Narrowing of the neck in resurfacing arthroplasty of the hip: a radiological study. J Bone Joint Surg [Br] 2007;89-B:1019–1024. doi: 10.1302/0301-620X.89B8.18830. [DOI] [PubMed] [Google Scholar]
- 29.Brooker AF, Bowerman JW, Robinson RA, Riley LH., Jr Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55-A:1629–1632. [PubMed] [Google Scholar]
- 30.Gruen TA, Le Duff MJ, Wisk LE, Amstutz HC. Prevalence and clinical relevance of radiographic signs of impingement in metal-on-metal hybrid hip resurfacing. J Bone Joint Surg Am. 2011;93-A:1519–1526. doi: 10.2106/JBJS.I.01723. [DOI] [PubMed] [Google Scholar]
- 31.R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2013. [Google Scholar]
- 32.No authors listed (2012) Medical and Healthcare products Regulatory Agency (MHRA). Medical Device Alert: All metal-on-metal (MoM) hip replacements. MDA/2012/036. http://www.mhra.gov.uk (date last accessed 12 November 2013)
- 33.No authors listed (2003) Guidance in the selection of prostheses for primary total hip replacement. Technology appraisal guidance – No.2. National Institute for Health and Clinical Excellence. 6th January 2003. http://www.nice.org.uk (date last accessed 12 November 2013)
- 34.Beaul’e PE, Dorey FJ, LeDuff M, Gruen T, Amstutz HC. Risk factors affecting outcome of metal-on-metal surface arthroplasty of the hip. Clin Orthop Relat Res. 2004;418:87–93. doi: 10.1097/00003086-200401000-00015. [DOI] [PubMed] [Google Scholar]
- 35.Marker DR, Seyler TM, Jinnah RH, Delanois RE, Ulrich SD, Mont MA. Femoral neck fractures after metal-on-metal total hip resurfacing: a prospective cohort study. J Arthroplasty. 2007;22:66–71. doi: 10.1016/j.arth.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 36.Matharu GS, McBryde CW, Pynsent WB, Pynsent PB, Treacy RB. The outcome of the Birmingham Hip Resurfacing in patients aged < 50 years up to 14 years post-operatively. Bone Joint J. 2013;95-B:1172–1177. doi: 10.1302/0301-620X.95B9.31711. [DOI] [PubMed] [Google Scholar]
- 37.McBryde CW, Shears E, O’Hara JN, Pynsent PB. Metal-on-metal hip resurfacing in developmental dysplasia: a case–control study. J Bone Joint Surg [Br] 2008;90-B:708–714. doi: 10.1302/0301-620X.90B6.20026. [DOI] [PubMed] [Google Scholar]
- 38.Glyn-Jones S, Pandit H, Kwon YM, Doll H, Gill HS, Murray DW. Risk factors for inflammatory pseudotumour formation following hip resurfacing. J Bone Joint Surg [Br] 2009;91-B:1566–1574. doi: 10.1302/0301-620X.91B12.22287. [DOI] [PubMed] [Google Scholar]
- 39.Nunley RM, Zhu J, Brooks PJ, et al. The learning curve for adopting hip resurfacing among hip specialists. Clin Orthop. 2010;468:382–391. doi: 10.1007/s11999-009-1106-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McMinn DJ, Snell KI, Daniel J, Treacy RB, Pynsent PB, Riley RD. Mortality and implant revision rates of hip arthroplasty in patients with osteoarthritis: registry based cohort study. BMJ. 2012;344:e3319. doi: 10.1136/bmj.e3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kendal AR, Prieto-Alhambra D, Arden NK, Carr A, Judge A (2013) Mortality rates at 10 years after metal-on-metal hip resurfacing compared with total hip replacement in England: retrospective cohort analysis of hospital episode statistics. BMJ 347:f6549 [DOI] [PMC free article] [PubMed]
- 42.Crowninshield RD, Rosenberg AG, Sporer SM. Changing demographics of patients with total joint replacement. Clin Orthop Relat Res. 2006;443:266–272. doi: 10.1097/01.blo.0000188066.01833.4f. [DOI] [PubMed] [Google Scholar]
- 43.Wylde V, Blom A, Dieppe P, Hewlett S, Learmonth I. Return to sport after joint replacement. J Bone Joint Surg [Br] 2008;90-B:920–923. doi: 10.1302/0301-620X.90B7.20614. [DOI] [PubMed] [Google Scholar]
- 44.Jourdan C, Poiraudeau S, Descamps S, et al. Comparison of patient and surgeon expectations of total hip arthroplasty. PLoS ONE. 2012;7:e30195. doi: 10.1371/journal.pone.0030195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Naal FD, Maffiuletti NA, Munzinger U, Hersche O. Sports after hip resurfacing arthroplasty. Am J Sports Med. 2007;35:705–711. doi: 10.1177/0363546506296606. [DOI] [PubMed] [Google Scholar]
- 46.Langton DJ, Joyce TJ, Jameson SS, et al. Adverse reaction to metal debris following hip resurfacing: the influence of component type, orientation and volumetric wear. J Bone Joint Surg [Br] 2011;93-B:164–171. doi: 10.1302/0301-620X.93B2.25099. [DOI] [PubMed] [Google Scholar]