Abstract
Purposes
Diabetes mellitus (DM) is thought to be an important aetiological factor in intervertebral disc degeneration. A glucose-mediated increase of oxidative stress is a major causative factor in development of diseases associated with DM. The aim of this study was to investigate the effect of high glucose on mitochondrial damage, oxidative stress and senescence of young annulus fibrosus (AF) cells.
Methods
AF cells were isolated from four-week-old young rats, cultured, and placed in either 10 % FBS (normal control) or 10 % FBS plus two different high glucose concentrations (0.1 M and 0.2 M) (experimental conditions) for one and three days. We identified and quantified the mitochondrial damage and reactive oxygen species (ROS) (oxidative stress). We also identified and quantified the occurrence of senescence and telomerase activity. Finally, the expressions of proteins were determined related to replicative senescence (p53-p21-pRB) and stress-induced senescence (p16-pRB).
Results
Two high glucoses enhanced the mitochondrial damage in young rat AF cells, which resulted in an excessive generation of ROS in a dose- and time-dependent manner for one and three days compared to normal control. Two high glucose concentrations increased the occurrence of senescence of young AF cells in a dose- and time-dependent manner. Telomerase activity declined in a dose- and time-dependent manner. Both high glucose treatments increased the expressions of p16 and pRB proteins in young rat AF cells for one and three days. However, compared to normal control, the expressions of p53 and p21 proteins were decreased in young rat AF cells treated with both high glucoses for one and three days.
Conclusions
The present study demonstrated that high glucose-induced oxidative stress accelerates premature stress-induced senescence in young rat AF cells in a dose- and time-dependent manner rather than replicative senescence. These results suggest that prevention of excessive generation of oxidative stress by strict blood glucose control could be important to prevent or to delay premature intervertebral disc degeneration in young patients with DM.
Keywords: Premature stress-induced senescence, Replicative senescence, Young annulus fibrosus cells, High glucose, Oxidative stress, Intervertebral disc degeneration
Introduction
Diabetes mellitus (DM) is a major public health problem worldwide. There are two main types of DM. Type 1 DM results from the body’s failure to produce insulin and is referred to as “insulin-dependent DM (IDDM)” or “juvenile-onset DM”. Approximately 10 % of all DM cases are type 1 and the prevalence of type 1 DM among the under 20s in the United States has recently risen by 23 % [1]. Untreated DM can cause many complications, such as cardiovascular disease, chronic renal failure, retinopathy and neuropathy [2]. DM is also considered to be an important aetiological factor in intervertebral disc degeneration [3–5]. Previous studies have reported a higher incidence of degenerative disc diseases in patients with DM than in the patients without DM [6]. It is known that DM patients with degenerative disc diseases are relatively younger than non-DM patients. A considerable portion of patients who undergo spine surgery is patients with DM. Their surgical outcome was reported to be poor compared to patients without DM [7, 8].
The intervertebral disc is a highly specialized structure that consists of an outer AF, which surrounds the inner nucleus pulposus (NP). The NP undergoes a chronological transition from a notochordal to a fibrocartilaginous NP. This transition accompanies changes in cell types from notochordal cells to so-called chondrocyte-like cells. In humans, this transition is usually completed by the second decade [9]. In contrast to the chondrocytic phenotype of young notochordal cells, young AF cells are fibroblastic, which is phenotypically different, and they don’t undergo chronological changes with age. In addition, there are some differences in the composition of the extracellular matrix produced by young notochordal cells and AF cells.
Cellular senescence is an irreversible growth arrest that can occur after repeated cell division (replicative senescence). Also it can be prematurely induced by stress conditions such as oxidative stress, DNA damage and mitogenic stress (stress-induced senescence) [10–12]. Senescent cells cannot divide even if stimulated by mitogens, but they are not physiologically inert and display altered phenotypic changes and gene expressions. Also they secrete degradative enzymes, inflammatory cytokines, and growth factors, leading to a shift from extracellular matrix synthesis to degradation. Therefore, senescence is considered as a major factor contributing to age- or disease-associated tissue dysfunction and pathology. Replicative senescence is mediated by the p53-p21-pRB pathway whereas stress-induced senescence is mediated by the p16-pRB pathway [13–15]. Senescent cells are characterized by telomere shortening and decreased telomerase activity. In addition, senescence-associated-beta-galactosidase (SA-ß-Gal) activity is used to identify the occurrence of senescence [16–18]. Recently, a few studies have started to report the association of senescence and intervertebral disc degeneration [19–24]. However, senescence of young AF cells as a biological mechanism as well as the role that senescence has in the intervertebral disc degeneration is not well understood to date.
The glucose-mediated increase in oxidative stress, such as the reactive oxygen species (ROS), is a main biochemical pathway in diseases associated with DM [25–27]. In most mammalian cell types the mitochondria are the main source of endogenous ROS [28]. ROS are thought to play a role in various cellular processes, such as senescence, which appear to cause cellular damage and lack of physiological function. Therefore, the accumulation of ROS has been reported to be associated with a variety of diseases including neurodegenerative diseases, DM, cancer, premature aging, and inflammatory disorders [29, 30]. To date, little information is available about the effect of DM on the senescence of young AF cells and premature intervertebral disc degeneration. Thus it is of paramount importance to clarify the effect of DM on the senescence of young AF cells to prevent or to delay premature intervertebral disc degeneration in young patients with DM. Therefore, the authors performed the present study to investigate the effect of DM on mitochondrial damage, oxidative stress, senescence of young rat AF cells, and intervertebral disc degeneration.
Materials and methods
Young rat AF cell culture and high glucose treatment
All lumbar intervertebral discs (L1-6) were harvested from four-week-old male Sprague Dawley young rats (Orient Bio., Seoul, Korea) immediately after they were sacrificed. The discs were carefully dissected under a microscope to obtain only the AF tissue, and the harvested AF tissue was pooled in [alpha]-minimum essential medium ([alpha]-MEM; Gibco BRL, Grand Island, NY, USA). The cells were released from the AF tissue in HBSS (Hyclone, Ottawa, Ontario, Canada) with 0.02 % pronase (Sigma-Aldrich, St. Louis, MO, USA) by vigorous pipetting. The cells were cultured in a complete medium [alpha]-MEM supplemented with 10 % fetal bovine serum (Hyclone), and 1 % penicillin-streptomycin (Gibco BRL) at 37 °C in a humidified atmosphere (95 % air, –5 % CO2). After the cells grew to confluence, they were split once (passage 1) and grew to confluence again. The cells were then trypsinized, washed, and plated on six or 12-well culture plates. When the cells reached 80–90 % confluence, the cells were placed in either 10 % fetal bovine serum (FBS) (normal control) or 10 % FBS plus two different high glucose concentrations (0.1 M and 0.2 M) (experimental conditions) for one and three days. This study was approved by the Institution’s Animal Care and Use Committee.
Detection of mitochondrial damage
Mitochondrial damage of the young AF cells was detected by Mitotracker ®Mitochondrion-selective Probes (Molecular Probes®, Invitrogen Inc., Camarillo, CA, USA). The kit utilizes Rosamine- and carbocynine-based dyes (MitoTracker®Orange CM-H2TMRos dyes) that fluoresces differentially in healthy and damaged apoptotic cells. In damaged apoptotic cells, MitoTracker dyes cannot aggregate in the mitochondria due to the altered mitochondrial transmembrane potential, and thus it remains in the cytoplasm in its monomer form, fluorescent red. The cells were seeded on a glass cover slip in 12-well culture plates and then incubated with the MitoTracker (250 nM) reagent in a pre-warmed incubation buffer in a humidified atmosphere for 30 minutes at 37 °C. Fluorescent signals were detected by fluorescence microscope (Image Pro Plus) (Olympus).
Intracellular ROS measurement
Intracellular accumulation of ROS was measured by ROS detection with H2DCF-DA (Sigma-Aldrich, St. Louis, MO, USA) according to the manufacturer’s instructions. Young AF cells were grown in 60-mm culture dishes. The medium was removed and carefully washed with a phosphate buffered saline (PBS). The cells were detached from the culture dishes and collected in 5-ml round-bottom polystyrene tubes. Then the cells were stained with 25 μM of H2DCF-DA in PBS in a humidified atmosphere (95 % air–5 % CO2) for 30 minutes at 37 °C. Fluorescence intensity was measured with BD FACS CantoTM flow cytometer (BD Biosciences, Franklin Lakes, NJ, USA).
Senescence of young rat AF cells
The SA-β-Gal activity in the young AF cells was determined using a SA-β-Gal staining kit (Cell Signaling Technology). The cells were plated onto poly (L-lysine)-coated 12-mm glass cover slips and fixed with 2 % formaldehyde and 0.2 % glutaraldehyde in phosphate buffered saline (PBS) for 15 minutes at room temperature. The slides were rinsed with PBS and then incubated for eight hours at 37 °C with fresh SA-β-gal staining solution containing 40 mM citric acid/sodium phosphate (pH 6.0), 150 mM NaCl, 2 mM MgCl2, 5 mM potassium ferrocyanide, 5 mM potassium ferricyanide, and 1 mg/ml of 5-bromo-4-chloro-3-indolyl-β-D-galactopyranoside (X-gal). After being rinsed with 70 % glycerol, blue-stained cells were identified as senescent cells under microscope. All young AF cells and SA-β-Gal-positive young AF cells on the whole section were counted (×200) and the percentage of SA-β-Gal-positive young AF cells was calculated.
Telomerase activity
The telomerase activity was analysed using a TeloTAGGG Telomerase PCR ELISA Plus Kit (Roche, Germany), according to the manufacturer’s instructions. Young rat AF cells were suspended in 100 μl of ice-cooled lysis reagent and incubated in ice for 15 minutes. The lysate was centrifuged at 14,000 rpm for 20 minutes at 4 °C. The supernatant was carefully removed and transferred into a tube for the TRAP assay; 30 μg of protein extract was used for each assay. The extended products were amplified by PCR using Taq polymerase, the P1-TS, P2 primers and nucleotides. After 30 minutes incubation at 25 °C to allow the telomerase-mediated extension of the TS primer, and five minutes at 94 °C to inactivate the telomerase, the reaction mixture was subjected to 30 PCR cycles at 94 °C for 30 seconds, 50 °C for 30 seconds, and 72 °C for 90 seconds and then on a thermocycler at 72 °C for ten minutes. Using the ELISA method, the amplified products were immobilized on streptavidin-coated microtiter plates via biotin-streptavidin interaction. Thereafter the amplifications were detected by anti-digoxigenin antibodies conjugated to peroxidase. After addition of the peroxidase substrate (3, 3', 5, 5'-tetramethyl benzidine), the amount of TRAP products was determined by measurement of absorbance at 450 nm using a microplate reader.
Expressions of p53, p21, pRB, and p16
Young rat AF cells were plated onto the poly (L-lysin)-coated 12-mm glass cover slips. The cells were fixed with 4 % paraformaldehyde in phosphate buffered saline (PBS) for 15 minutes at room temperature and washed with PBS, pH7.4. The cells were permeabilized by 0.2 % TritonX-100 in PBS for ten minutes. After incubation for 30 minutes at room temperature with PBS containing 3 % BSA (blocking solution), cells were incubated overnight at 4 °C with the primary antibody (1:100 dilution) for p53 (Novus Biologicals, CO, USA), p21 (Abcam Plc, Cambridge, UK), pRB (Biorbyt Ltd., Cambridge, UK) and p16 (Santa Cruz Biotechnology, CA, USA). After washing, the anti-rabbit Alexa Fluor®488 (Invitrogen, CA, USA) and anti-mouse Alexa Fluor®555 (Invitrogen, CA, USA) fluorescence-conjugated IgG antibodies (1:5000 dilution) in the blocking solution were added and incubated for one hour at room temperature in the dark. The cover slips were mounted onto the object glasses with mounting medium with 4, 6-diamidino-2-phenylindole (VECTOR, CA, USA). Fluorescent signals were detected by fluorescence microscopy (Olympus CO., Tokyo, Japan).
Statistical analysis
All experiments were independently conducted three times, and the results were expressed as the mean and standard deviation of the values derived with the three tests. Statistical analysis was done with the paired-samples t test. P < 0.05 was considered to be the level of significance.
Results
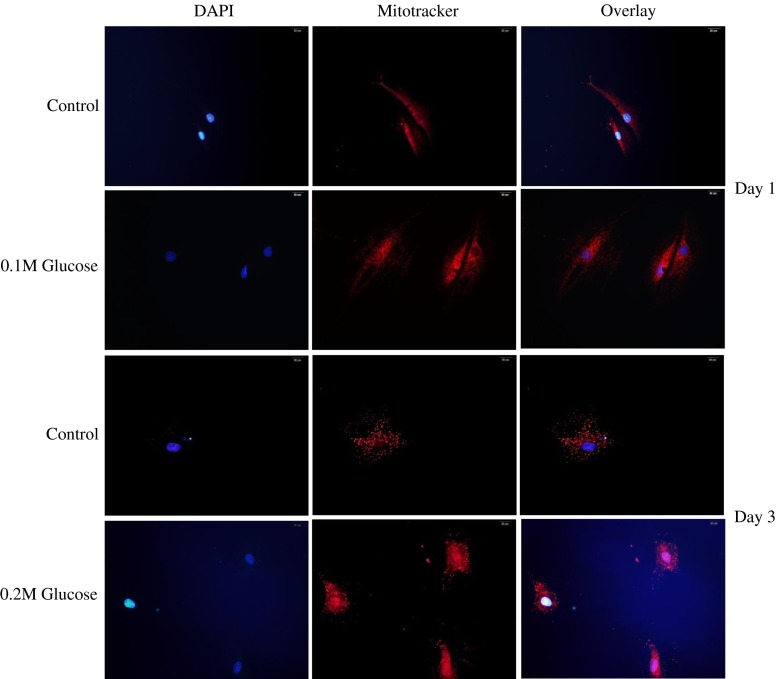
Excessive generation of ROS through mitochondrial damage
Immunofluorescence demonstrated an enhanced disruption of mitochondrial damage (red colour) in young rat AF cells treated with both high glucoses for one and three days when compared to the control (Fig. 1). In detail, the enhanced disruption of mitochondrial damage (red colour) was detected in the nuclei of young rat AF cells of normal control, whereas the enhanced disruption of mitochondrial damage was observed in not only the nuclei of young rat AF cells treated with both high glucoses for one and three days but also in the cytoplasm around the nuclei.
Fig. 1.
Immunofluorescence demonstrated an enhanced disruption of the mitochondrial damage (red colour) in young rat annulus fibrosus cells treated with both high glucose concentrations for one and three days, when compared to normal control. In detail, the enhanced disruption of mitochondrial damage (red colour) was detected in the nuclei of young rat AF cells of normal control, whereas the expression of the enhanced disruption of the mitochondrial damage was observed in not only the nuclei of young rat annulus fibrosus cells treated with both high glucoses for one and three days but also in the cytoplasm around the nuclei
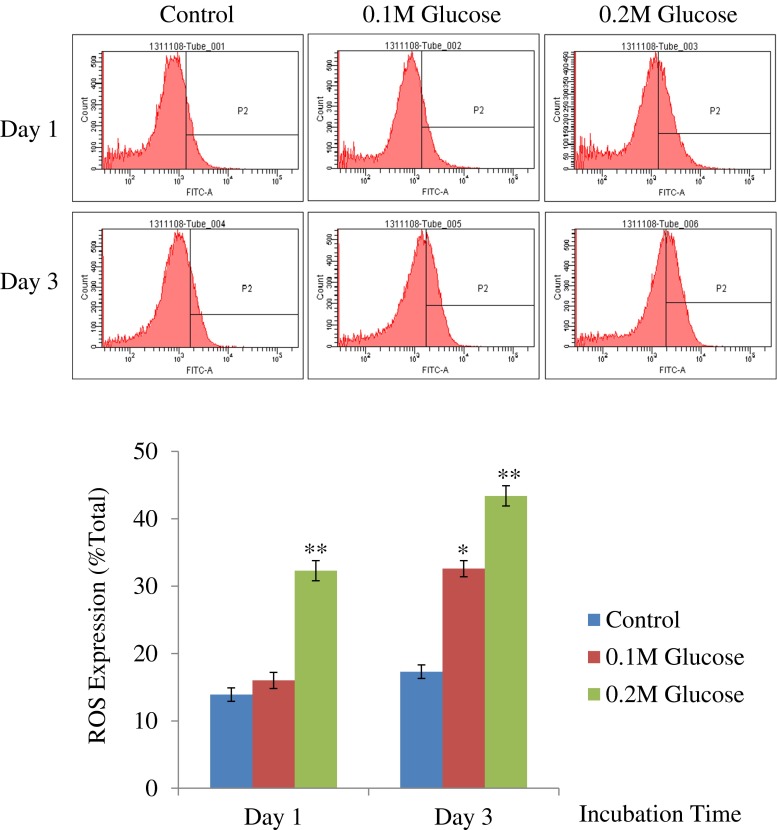
Flow cytometry showed that each high glucose concentration enhanced ROS generation in young rat AF cells over one and three days in a dose- and time-dependent manner (Fig. 2).
Fig. 2.
Flow cytometry showed that each high glucose concentration enhanced ROS generation in young rat annulus fibrosus cells in a dose- and time-dependent manner for one and three days. ** p < 0.01; * p < 0.05
Decreased telomerase activity
The mean telomerase activity (arbitrary unit [AU]) declined in young rat AF cells treated with 0.1 M high glucose (2.1 AU vs. 1.7 AU, p > 0.05) and 0.2 M high glucose (2.1 AU vs. 1.4 AU, p < 0.05) compared with those of normal control in one day. The mean telomerase activity (arbitrary unit) also declined in young rat AF cells treated with 0.1 M high glucose (1.6 AU vs. 1.0 AU, p < 0.05) and 0.2 M high glucose (1.6 AU vs. 0.75 AU, p < 0.01) compared with those of normal control for three days.
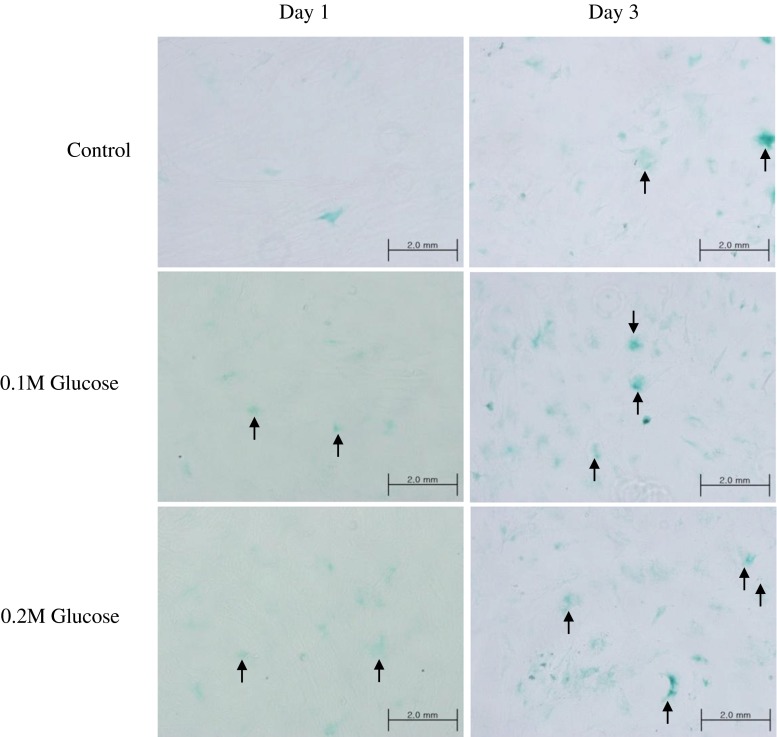
Increased senescence of young rat AF cells
The mean percentage of SA-β-Gal-positive young rat AF cells was significantly increased in young rat AF cells treated with 0.1 M high glucose (4 % vs. 15 %, p < 0.01) and 0.2 M high glucose (4 % vs. 24 %, p < 0.001) for one day, when compared to normal control (Fig. 4). The mean percentage of SA-β-Gal-positive young rat AF cells was significantly increased in young rat AF cells treated with 0.1 M high glucose (7 % vs. 23 %, p < 0.01) and 0.2 M high glucose (7 % vs. 32 %, p < 0.001) for three days, when compared to normal control (Fig. 3).
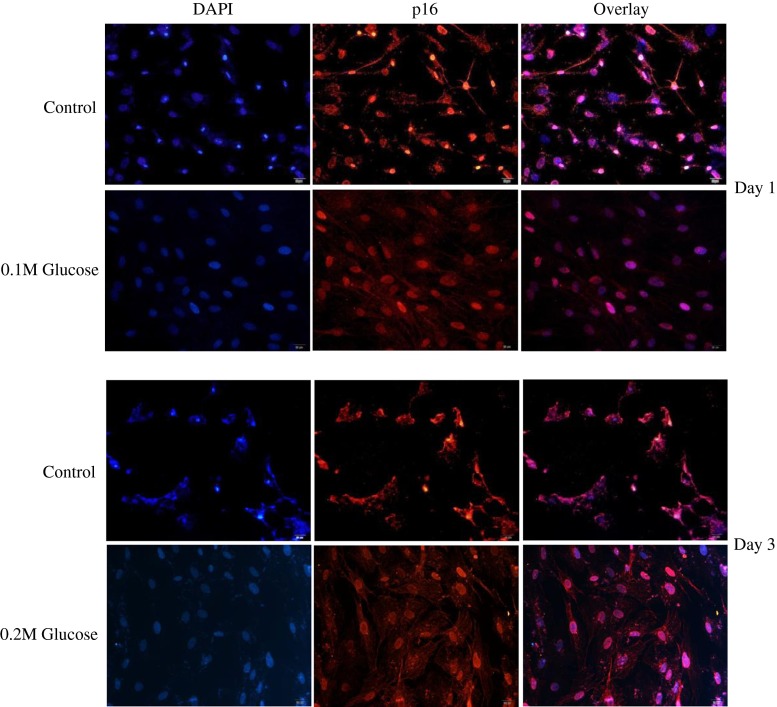
Fig. 4.
Immunofluorescence demonstrated that the two high glucose concentrations enhanced expressions of p16 (red colour) protein in young rat annulus fibrosus cells treated with both high glucose concentrations for one and three days respectively when compared to normal control
Fig. 3.
The mean SA-β-gal-positive percentage (arrows) increased in young rat annulus fibrosus cells treated with both high glucose concentrations for one and three days in a dose- and time-dependent manner, when compared to normal control. *** p < 0.001; ** p < 0.01
Premature stress-induced senescence of young rat AF cells
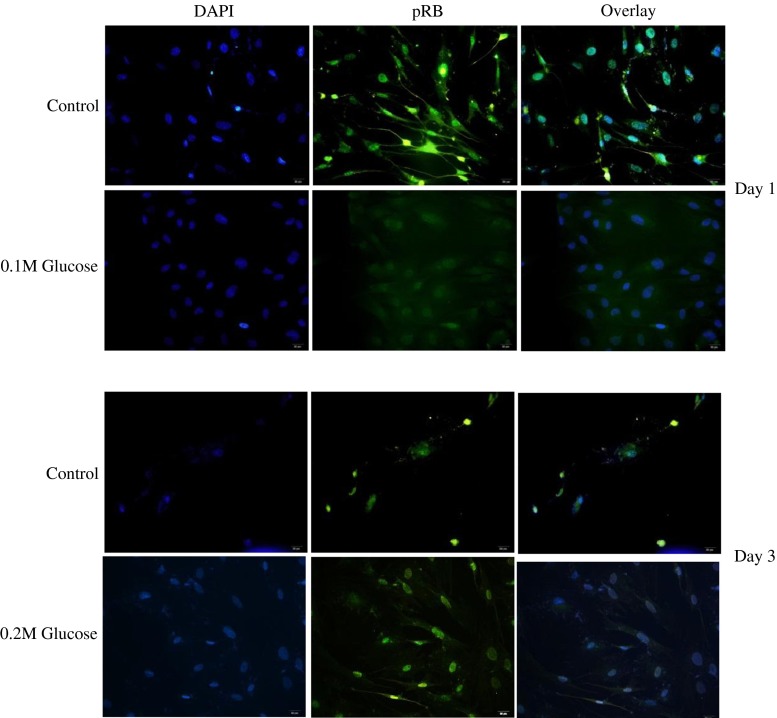
Immunofluorescence demonstrated that the two high glucose concentrations enhanced expressions of p16 (red colour) (Fig. 4) protein in young rat AF cells treated with both high glucose concentrations for one and three days respectively when compared to normal control. In addition, immunofluorescence demonstrated that the two high glucose concentrations enhanced expressions of pRB (green colour) (Fig. 5) proteins in young rat AF cells treated with both high glucose concentrations for one and three days respectively when compared to normal control.
Fig. 5.
Immunofluorescence demonstrated that the two high glucose concentrations enhanced expressions of pRB (green colour) protein in young rat annulus fibrosus cells treated with both high glucose concentrations for one and three days respectively when compared to normal control
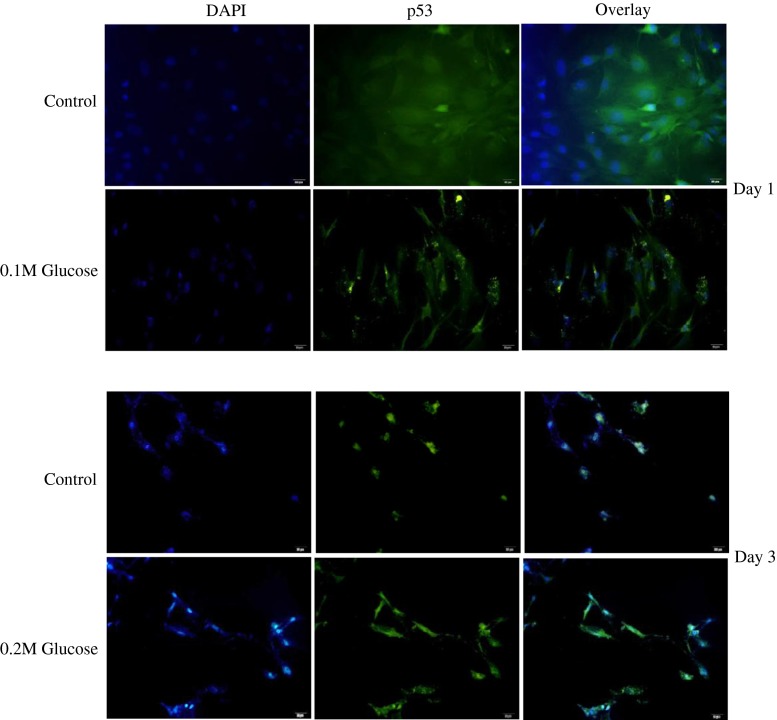
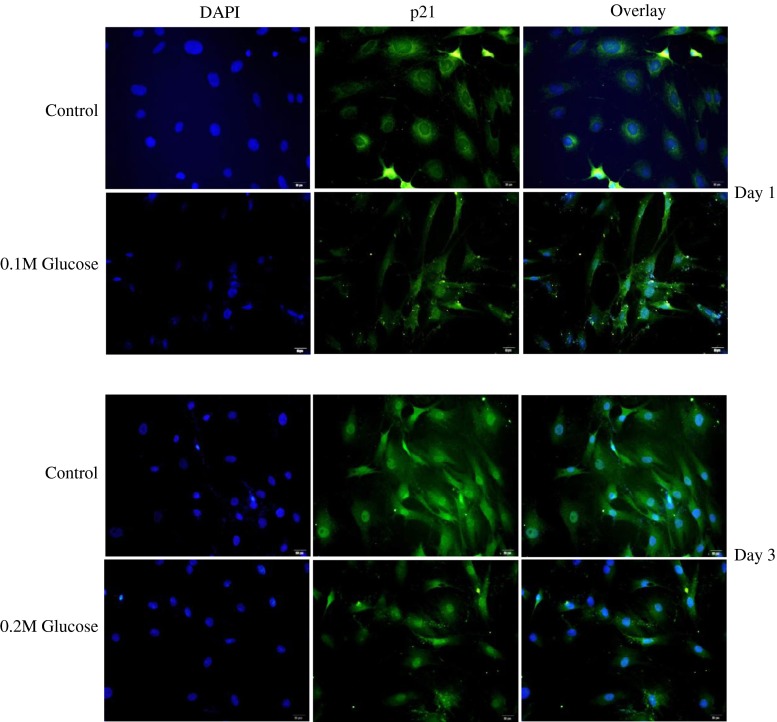
However, immunofluorescence demonstrated that the two high glucose concentrations decreased the expression of p53 (Fig. 6) (green colour) protein in young rat AF cells treated with both high glucose concentrations for one and three days respectively when compared to normal control. In addition, immunofluorescence demonstrated that the two high glucose concentrations decreased the expression of p21 (Fig. 7) (green colour) protein in young rat AF cells treated with both high glucose concentrations for one and three days respectively when compared to normal control.
Fig. 6.
Immunofluorescence demonstrated that the two high glucose concentrations decreased the expression of p53 (green colour) protein in young rat annulus fibrosus cells treated with both high glucose concentrations for one and three days respectively when compared to normal control
Fig. 7.
Immunofluorescence demonstrated that the two high glucose concentrations decreased the expression of p21 (green colour) protein in young rat annulus fibrosus cells treated with both high glucose concentrations for one and three days respectively when compared to normal control
Discussion
The present findings demonstrate that both high glucose concentrations induced mitochondrial damage and consequently increased the generation of ROS in young rat AF cells in a dose- and time-dependent manner. The occurrence of senescence was significantly enhanced in young rat AF cells treated with high glucose concentration in a dose- and time-dependent manner. Telomerase activity declined in young rat AF cells treated with both high glucoses in a dose- and time-dependent manner. The expressions of premature stress-induced senescence (p16-pRB) pathway were enhanced in young rat AF cells. However, the expressions of proteins related to replicative senescence (p53-p21) were decreased in young rat AF cells treated with both high glucose concentrations. These results suggest that high glucose-induced oxidative stress accelerates premature stress-induced senescence of young rat AF cells through mitochondrial damage in a dose- and time-dependent manner. Thus, accelerated premature stress-induced senescence of young AF cells could be proposed as an emerging risk factor for premature intervertebral disc degeneration in young patients with DM. These results point out the importance of strict blood glucose control in young patients with DM to prevent an excessive generation of oxidative stress and subsequently to prevent or to delay premature intervertebral disc degeneration in young patients with DM.
Senescence may have evolved as a mechanism to prevent cells with damaged DNA from being replicated and thus to prevent tumour formation [31, 32]. Replicative senescence is associated with changes in DNA structure and function including a telomere shortening and decrease activity of telomerase [10–12]. However, senescence appears to be much more complex than as a simple cell-cycle arrest occurring after a finite number of cell divisions. Progressive telomere shorting due to repeated cycles of cell division does not explain senescence in post-mitotic cells such as neurons or quiescent cells such as chondrocytes. Stress-induced senescence can occur due to diverse stimuli including ultraviolet radiation, oxidative damage, activated oncogenes, and chronic inflammation [13–15]. Oxidative damage to DNA can directly contribute to stress-induced senescence and can result in telomere shortening similar to that seen in replicative senescence because the ends of chromosomes are particularly sensitive to oxidative damage. Oxidative stress has been found to induce cell senescence in vitro and there is in vivo evidence for age-related oxidative stress in many tissues [13–15]. As additional evidence for a role of ROS in aging, increased expression of the antioxidant enzyme catalase in mitochondria of transgenic mice can extend life-span and reduce age-related changes in tissues such as that of the heart [10–12]. It is well known that damaged mitochondria release harmful ROS into the cytosol [25–30]. In the present study, we demonstrated an excessive generation of oxidative stress, such as ROS, through mitochondrial damage in young rat AF cells treated with high glucose concentrations with a dose- and time-dependent manner compared to normal control.
A hallmark of senescence is the expression of SA-ß-Gal. However, it is not strictly specific for senescent cells, since non-senescent cells with a high lysosomal content also stain positive in this assay [16–18]. The present study showed a higher percentage of SA-ß-Gal-positive staining, meaning a higher rate of senescence in young rat AF cells treated with both high glucose concentrations compared to normal control. To supplement shortcomings of SA-ß-Gal staining, we additionally performed the immunofluorescence staining to determine the expressions of proteins, such as p53, p21, pRB and p16-pRB, related to replicative and stress-induced senescence pathways. Immunofluorescence showed that the senescent young rat AF cells by undergoing high glucose treatments significantly expressed p16 and pRB proteins, whereas the expressions of p53 and p21 proteins were decreased compared to the normal control. We further showed that high glucose concentrations decline the telomerase activity of young rat AF cells in a dose- and time-dependent manner. These results indicate that high glucose-induced oxidative stress predominantly accelerates premature stress-induced senescence (p16-pRB) in young rat AF cells treated with high glucose concentrations. We did not investigate the compensatory expression of antioxidants, such as the manganese superoxide dismutase (MnSOD) and catalase, in young rat AF cells treated with high glucoses. However, considering the accelerated premature stress-induced senescence in young rat AF we may speculate that excessive generation of oxidative stress caused by two high glucose concentrations overwhelms the protective effect of antioxidants. Further studies are needed to confirm this speculation.
Before this study, it had not yet been confirmed that high glucose-induced oxidative stress caused diabetes-related young AF cells’ premature senescence. This study demonstrated that the percentage of premature stress-induced senescence of young rat AF cells increased in proportion to the dose and time of high glucoses treatment. This may explain the increased risk of premature intervertebral disc degeneration with severity and duration of DM that is shown in young patients with DM. It is known that 40 % of patients with DM who carefully control their blood sugar nevertheless develop neuropathy. Thus, young patients with type 1 DM will need to take insulin injections for the rest of their life to prevent or to delay premature intervertebral disc degeneration. They must also ensure proper blood glucose levels by carrying out regular blood tests and following a special diet [1, 2].
There are some limitations to the present study. First, we did not investigate the telomere length and expression of antioxidants. Telomere shortening is a characteristic finding for cellular senescence. Second, an in vitro high glucose-induced diabetic model cannot perfectly reflect in vivo aspects of intervertebral disc degeneration with DM, especially in terms of high glucose concentrations and culture period. Thus, further in vivo studies are needed to clarify these limitations.
In conclusion, the present study demonstrates that high glucose-induced oxidative stress accelerates premature stress-induced senescence of young rat AF cells in a dose- and time-dependent manner. This may result in dysfunction of young AF cells, leading to premature intervertebral disc degeneration. Thus, accelerated premature stress-induced senescence of young AF cells could be proposed as an emerging risk factor for premature intervertebral disc degeneration in young patients with DM. Therefore, the present results suggest that strict blood glucose control in young patients with DM could be important to prevent an excessive generation of oxidative stress and subsequently to prevent or to delay premature intervertebral disc degeneration in young patients with DM.
References
- 1.Alberti KG, Zimmet P, Shaw J. Metabolic syndrome—a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med. 2006;23:469–480. doi: 10.1111/j.1464-5491.2006.01858.x. [DOI] [PubMed] [Google Scholar]
- 2.McClelland AD, Kantharidis P. MicroRNA in the development of diabetic complications. Clin Sci (Lond) 2014;126:95–110. doi: 10.1042/CS20130079. [DOI] [PubMed] [Google Scholar]
- 3.Won HY, Park JB, Park EY, Riew KD. Effect of hyperglycemia on apoptosis of notochordal cells and intervertebral disc degeneration in diabetic rats. J Neurosurg Spine. 2009;11:741–748. doi: 10.3171/2009.6.SPINE09198. [DOI] [PubMed] [Google Scholar]
- 4.Park EY, Park JB. Dose- and time-dependent effect of high glucose concentration on viability of notochordal cells and expression of matrix degrading and fibrotic enzymes. Int Orthop. 2013;37:1179–1186. doi: 10.1007/s00264-013-1836-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park EY, Park JB. High glucose-induced oxidative stress promotes autophagy through mitochondrial damage in rat notochordal cells. Int Orthop. 2013;37:2507–2514. doi: 10.1007/s00264-013-2037-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mobbs RJ, Newcombe RL, Chandran KN. Lumbar discectomy and the diabetic patient: incidence and outcome. J Clin Neurosci. 2001;8:10–13. doi: 10.1054/jocn.2000.0682. [DOI] [PubMed] [Google Scholar]
- 7.Sakellaridis N. The influence of diabetes mellitus on lumbar intervertebral disk herniation. Surg Neurol. 2006;66:152–154. doi: 10.1016/j.surneu.2006.01.019. [DOI] [PubMed] [Google Scholar]
- 8.Simpson JM, Silveri CP, Balderston RA, Simeone FA, An HS. The results of operations on the lumbar spine in patients who have diabetes mellitus. J Bone Joint Surg Am. 1993;75:1823–1829. doi: 10.2106/00004623-199312000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Kim KW, Lim TH, Kim JG, Jeong ST, Masuda K, An HS. The origin of chondrocytes in the nucleus pulposus and histologic findings associated with the transition of a notochordal nucleus pulposus to a fibrocartilaginous nucleus pulposus in intact rabbit intervertebral discs. Spine. 2003;28:9829–9890. doi: 10.1097/01.BRS.0000061986.03886.4F. [DOI] [PubMed] [Google Scholar]
- 10.Tsirpanlis T. Cellular senescence, cardiovascular risk, and CKD. A review of established and hypothetical interconnections. Am J Kidney Dis. 2008;51:131–144. doi: 10.1053/j.ajkd.2007.07.035. [DOI] [PubMed] [Google Scholar]
- 11.Shimada H, Sakakima H, Tsuchimochi K, Masuda F, Komiya S, Goldring MB, Ijiri K. Senescence of chondrocytes in aging articular cartilage: GADD45 mediates p21 expression in association with C/EBP in senescence-accelerated mice. Pathol Res Pract. 2011;207:225–231. doi: 10.1016/j.prp.2011.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Unterluggauera H, Hampela B, Zwerschkea W, Jansen-Dürr P. Senescence-associated cell death of human endothelial cells: the role of oxidative stress. Exp Gerontol. 2003;38:1149–1160. doi: 10.1016/j.exger.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 13.Khan IM, Gilbert SJ, Caterson B, Sandell LJ, Archer CW. Oxidative stress induces expression of osteoarthritis markers procollagen IIA and 3B3(-) in adult bovine articular cartilage. Osteoarthritis Cartilage. 2008;16:698–707. doi: 10.1016/j.joca.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 14.Chainiaux F, Magalhaes JP, Eliaers F, Remacle J, Toussaint O. UVB-induced premature senescence of human diploid skin fibroblasts. Int J Biochem Cell Biol. 2002;34:1331–1339. doi: 10.1016/S1357-2725(02)00022-5. [DOI] [PubMed] [Google Scholar]
- 15.Gorgoulis VG, Pratsinis H, Zacharatos P, Demoliou C, Sigala F, Asimacopoulos PJ, Papavassiliou AG, Kletsas D. p53-dependent ICAM-1 overexpression in senescent human cells identified in atherosclerotic lesions. Lab Invest. 2005;85:502–511. doi: 10.1038/labinvest.3700241. [DOI] [PubMed] [Google Scholar]
- 16.Severino J, Allen RG, Balin S, Cristofalo VJ. Is b-galactosidase staining a marker of senescence in vitro and in vivo? Exp Cell Res. 2000;257:162–171. doi: 10.1006/excr.2000.4875. [DOI] [PubMed] [Google Scholar]
- 17.Dimri GP, Lee X, Basile G, Acosta M, Scott G, Roskelley C, Medrano EE, Linskens M, Rubeli I, Pereira-Smith O, Campisi J. A biomarker that identifies senescent human cells in culture and in aging skin in vivo. Proc Natl Acad Sci USA. 1995;92:9363–9367. doi: 10.1073/pnas.92.20.9363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kurz DJ, Decary S, HongY EJD. Senescence-associated (beta)-galactosidase reflects an increase in lysosomal mass during replicative ageing of human endothelial cells. J Cell Sci. 2000;13:3613–3622. doi: 10.1242/jcs.113.20.3613. [DOI] [PubMed] [Google Scholar]
- 19.Zhao CQ, Wang LM, Jiang LS, Dai LY. The cell biology of intervertebral disc aging and degeneration. Ageing Res Rev. 2007;6:247–261. doi: 10.1016/j.arr.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 20.Gruber HE, Watts JA, Hoelscher GL, Bethea SF, Ingram JA, Zinchenko NS, Hanlet EN., Jr Mitochondrial gene expression in the human annulus: in vivo data from annulus cells and selectively harvested senescent annulus cells. Spine J. 2011;11:782–791. doi: 10.1016/j.spinee.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 21.Roberts S, Evans H, Kletsas D, Jaffray DC, Eisenstein SM. Senescence in human intervertebral discs. Eur Spine J. 2006;15(Suppl 3):S312–S316. doi: 10.1007/s00586-006-0126-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gruber HE, Ingram JA, Norton HJ, Hanley EN., Jr Senescence in cells of the aging and degenerating intervertebral disc immunolocalization of senescence-associated-galactosidase in human and sand rat discs. Spine. 2007;32:321–327. doi: 10.1097/01.brs.0000253960.57051.de. [DOI] [PubMed] [Google Scholar]
- 23.Kletsas D. Senescent cells in the intervertebral disc: numbers and mechanisms. Spine J. 2009;9:677–678. doi: 10.1016/j.spinee.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 24.Kim KW, Chung HN, Ha KY, Lee JS, Kim YY. Senescence mechanisms of nuclear pulposus chondrocytes in human intervertebral discs. Spine J. 2009;9:658–666. doi: 10.1016/j.spinee.2009.04.018. [DOI] [PubMed] [Google Scholar]
- 25.Baynes JW. Role of oxidative stress in development of complications in diabetes. Diabetes. 1991;40:405–412. doi: 10.2337/diab.40.4.405. [DOI] [PubMed] [Google Scholar]
- 26.Nishikawa T, Araki E. Impact of mitochondrial ROS production in the pathogenesis of diabetes mellitus and its complications. Antioxid Redox Signal. 2007;9:343–353. doi: 10.1089/ars.2006.1458. [DOI] [PubMed] [Google Scholar]
- 27.Dorn GW., 2nd Mechanism of non-apoptotic programmed cell death in diabetes and heart failure. Cell Cycle. 2010;9:3442–3448. doi: 10.4161/cc.9.17.12944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Victor VM, Rocha M, Herance R, Hernandez-Mijares A. Oxidative stress and mitochondrial dysfunction in type 2 diabetes. Curr Pharm Des. 2011;17:3947–3958. doi: 10.2174/138161211798764915. [DOI] [PubMed] [Google Scholar]
- 29.Brandl A, Hartmann A, Bechmann V, Graf B, Nerlich M, Angele P. Oxidative stress induces senescence in chondrocytes. J Orthop Res. 2011;29:1114–1120. doi: 10.1002/jor.21348. [DOI] [PubMed] [Google Scholar]
- 30.Furukawa A, Tada-Oikawa S, Kawanishi S, Oikawa S. H2O2 accelerates cellular senescence by accumulation of acetylated p53 via decrease in the function of SIRT1 by NAD + depletion. Cell Physiol Biochem. 2007;20:45–54. doi: 10.1159/000104152. [DOI] [PubMed] [Google Scholar]
- 31.Ben-Porath I, Weinberg RA. The signals and pathways activating cellular senescence. Int J Biochem Cell Biol. 2005;37:961–976. doi: 10.1016/j.biocel.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 32.Campisi J. Cellular senescence as a tumor-suppressor mechanism. Trends Cell Biol. 2001;11:S27–S31. doi: 10.1016/S0962-8924(01)02151-1. [DOI] [PubMed] [Google Scholar]