Abstract
Purpose
The purpose of the present epidemiologic study is to record the radiographic presence of trochlear dysplasia and patella alta in patients who undergo anterior cruciate ligament (ACL) reconstruction as a potential underlying factor for post-operative anterior knee pain (AKP).
Methods
All consecutive cases of skeletally-mature ACL-deficient knees that would undergo ACL reconstruction in three different hospitals were prospectively included during a six-month period. Inclusion criteria were acute and sub-acute ACL injury with no previous ipsilateral knee operation. Patients with chronic ACL tears, prior-to-ACL-injury history of patellar instability or other PF disorders were excluded from the study.
Results
A total of 299 knees were included (mean age 32 ± ten years). Forty-four (14.7 %) knees had a positive ‘crossing sign’ in the lateral X-rays and 255 (85.3 %) had no sign of trochlear dysplasia (p < 0.01). Among the cases with trochlear dysplasia, 41 (93 %) had type A trochlear dysplasia with the presence only of the ‘crossing sign’ and three (7 %) had type C trochlear dysplasia. Patellar height results included a mean Caton-Deschamps index of 1.0 ± 0.14 (0.5–1.4). Twenty (6.6 %) knees had an index of less than 0.8, and two (0.6 %) knees had an index less than 0.6. In contrast, 15 (5.0 %) knees had an abnormal value of more than 1.2, indicating patella alta.
Conclusions
The most important finding of the study is the increased prevalence of trochlear dysplasia and patella alta in patients with ACL injury, when compared to the incidence of trochlear dysplasia and patella alta in the general population in the literature. This finding could sound as an alert of a possible additional risk factor for post-operative anterior knee pain after ACL reconstruction.
Keywords: Anterior cruciate ligament, Trochlear dysplasia, Patella alta, Anterior knee pain, Patellofemoral
Introduction
The success rate of anterior cruciate ligament (ACL) reconstructions is good to excellent, yet the increased number of ACL reconstructions leads inevitably to a rise in complications [1–4]. One of the common complications following ACL reconstruction is anterior knee pain (AKP) [1, 2]. AKP can interfere negatively with the post-operative rehabilitation program and may reduce patient satisfaction and be a cause for re-operation [5]. Identifying the underlying factors under this frequent complication, and finding the means to prevent or correct them can increase patient satisfaction, improve functional scores and reduce the need for re-admission [4–6]. The causes of AKP after ACL reconstruction are multifactorial, but key factors such as range-of-motion deficit due to tunnel malpositioning or Cyclops lesions, increased body mass index, older patient’s age, infrapatellar nerve injury and autograft type have been identified [4–6]. Other authors have failed to correlate AKP with previous epidemiologic studies and have recorded the same prevalence of AKP among patients of different age and sex [7]. This can be attributed to reasons other than patients’ age or donor-site morbidity in the persistence of AKP [5, 8].
AKP can be a challenging diagnosis and the differential is vast for other than post-operative ACL reconstruction. There are a group of patients with patellofemoral (PF) disorders who have underlying non-anatomic factors and they present with a wide range of symptoms from patellar dislocation to pain [9–12]. In these patients, AKP is the result of patellar maltracking, PF impingement and subsequent increased PF pressures or cartilaginous lesions [13]. The importance of extensor mechanism deficiency, lower-limb malalignment and soft-tissue imbalance has been studied extensively, but the most persistent anatomic findings in patients with PF disorders are trochlear dysplasia and patella alta [14–16]. Trochlear dysplasia is a developmental condition in which the distal femur loses its normal concave shape and turns to an abnormal flat or even convex geometry. Dejour has classified trochlear dysplasia in four distinctive types according to the presence of the crossing sign, the supratrochlear spur and/or the double-contour sign (Fig. 1) [17]. Trochlear dysplasia has been directly associated with both recurrent patellar dislocation [18–20] and AKP [21, 22] in patients with patellar instability, since it has been observed in 96 % of patients with PF disorders and in only 3 % of controls [15, 22]. The surgical correction of trochlear dysplasia is done with the sulcus-deepening trochleoplasty procedure, in which the elevated groove is eliminated and the abnormal sulcus is deepened [23–25]; this can also rarely be enriched by the addition of patellar osteotomy in order to achieve a better congruency between the two articulating bones [26]. Some authors have also suggested that trochlear dysplasia may extend more distally to the intercondylar notch and therefore could be more frequent in patients with ACL tears due to a reduced intercondylar notch size that predisposes to ACL injury (Fig. 2) [27].
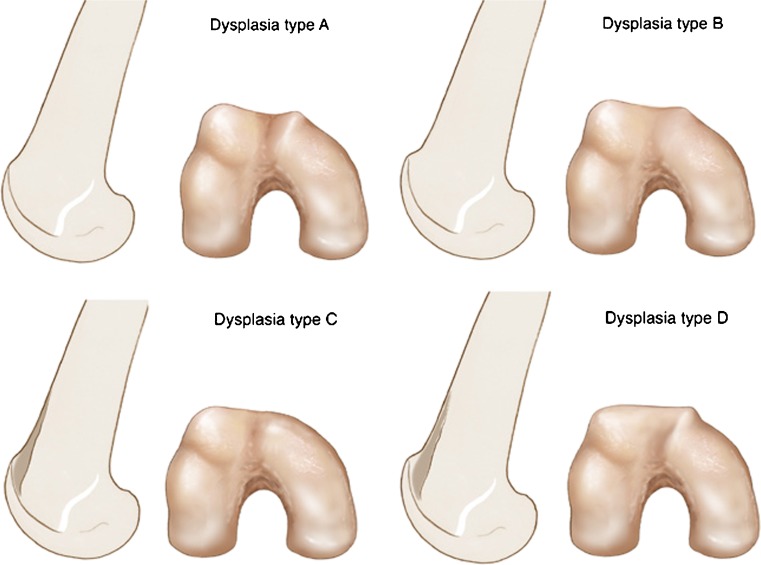
Fig. 1.
Dejour’s classification of trochlear dysplasia in four types: type A with the crossing sign (the groove is flush with the facets), type B with the crossing sign and the supratrochlear spur (“bump”), type C with the crossing sign and the double-contour sign (medial hypoplastic condyle), and type D with all three signs
Fig. 2.
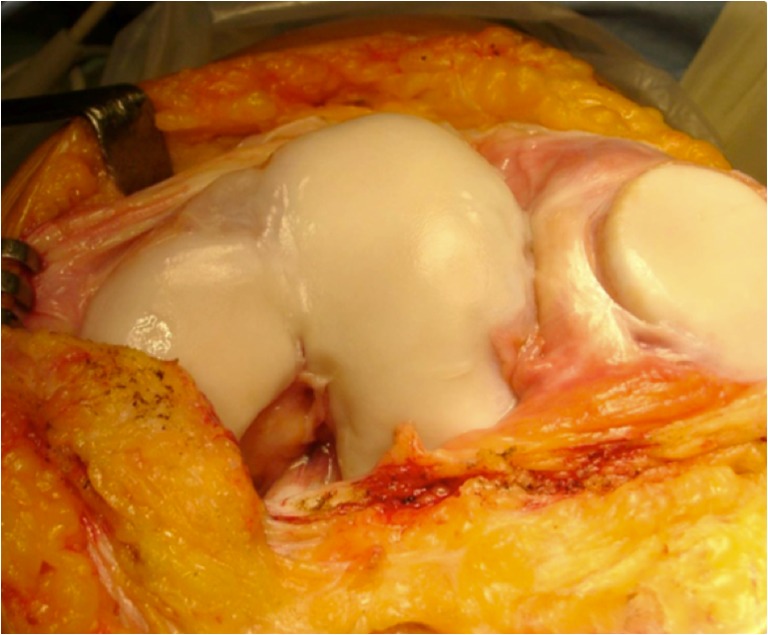
Intra-operative view of the distal femur with a dysplastic trochlea, that may continue into the intercondylar notch
Furthermore, patella alta has been biomechanically and clinically linked to increased incidence of AKP [28–31] and present in 30 % of patients with PF disorders and in 0 % of controls [15, 22]. There are also reports of a group of patients with ‘potential patellar instability’, in whom trochlear dysplasia and/or patella alta are present and causing AKP but with no history of patellar dislocation [15].
A potential increased prevalence of signs of PF anatomic anomalies could advise the surgeon to pre-operatively evaluate the PF joint in the ACL-deficient patient or identify an additional source of probable post-operative AKP. The purpose of the present epidemiologic study was to record the radiographic presence of trochlear dysplasia and patella alta in patients who undergo ACL reconstruction as a potential underlying factor for post-operative AKP. The authors tested the hypothesis that the imaging findings of trochlear dysplasia and abnormal patellar height are more frequent in ACL reconstruction patients than those previously recorded in the average population.
Materials and methods
All consecutive cases of skeletally-mature ACL-deficient knees that would undergo ACL reconstruction in three different hospitals were prospectively included from January 2012 to May 2012. Inclusion criteria were: acute and sub-acute (less than six months) ACL injury with no previous ipsilateral knee operation. Patients with chronic ACL tears, prior-to-ACL-injury history of patellar instability or other PF disorders were excluded from the study.
In every case, AP and axial views at 30° flexion were performed while the sagittal weight bearing views were done under fluoroscopy with the posterior femoral condyles superimposed. The presence of trochlear dysplasia was rated using the Dejour’s classification in four distinct types, A to D [17] with the use of true lateral knee X-rays. Patellar height was measured with the use of Caton-Deschamps index on lateral knee X-rays, where values over 1.2 are indicative of patella alta (Fig. 3) [32]. The three chief surgeons who performed the ACL reconstructions and three independent examiners evaluated the X-rays for the diagnosis of trochlear dysplasia and the measurement of patellar height. The type of ACL injury was diagnosed both clinically and subsequently confirmed during arthroscopy to categorize them to full or partial tears.
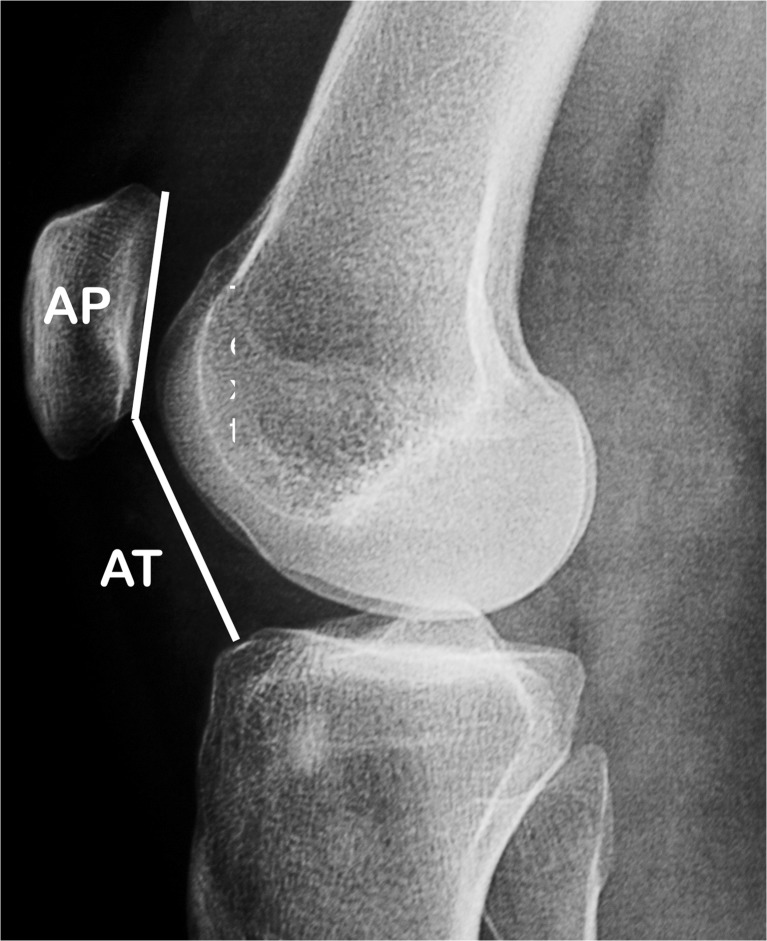
Fig. 3.
The Caton-Deschamps index for the evaluation of patellar height is the ratio of AT:AP and has a normal value range of 0.6–1.2. Values less than 0.6 are indicative of patella infera and values greater than 1.2 are indicative of patella alta
Statistical analysis included the use of chi-square test for qualitative parameters (trochlear dysplasia type) and the use of Mann–Whitney for quantitative parameters (Caton-Deschamps index). Level of statistical significance was set to p < 0.05.
Results
Two hundred sixty-four patients (299 knees) were included throughout the study period. Mean age was 32 ± ten years (range, 17–56). Female to male ratio was 0.4. Thirty-five patients (13.2 %) had bilateral ACL injury. Two hundred seventy-eight (92.9 %) knees had isolated ACL tear. Among them, 254 (84.9 %) had a complete ACL injury and 24 (8.0 %) had a partial ACL tear, which was confirmed during arthroscopy. In 21 cases (7.1 %) there was a concomitant collateral ligament injury.
The evaluation of lateral X-rays for trochlear dysplasia revealed the following findings: 44 (14.7 %) knees had a positive ‘crossing sign’ in the lateral X-rays and 255 (85.3 %) had no sign of trochlear dysplasia (p < 0.01). Among the cases with trochlear dysplasia, 41 (93 %) had type A trochlear dysplasia with the presence only of the ‘crossing sign’ and three (7 %) had type C trochlear dysplasia. There was no significant correlation between the cases with trochlear dysplasia and bilateral ACL injury (p = 0.35).
Patellar height results in the study group included mean Caton-Deschamps index of 1.0 ± 0.14 (range, 0.5–1.4). Twenty (6.6 %) knees had an index of less than 0.8 and two (0.6 %) knees had an index less than 0.6. In contrast, 15 (5.0 %) knees had an abnormal value of more than 1.2, indicating patella alta. The correlation between Caton-Deschamps index > 1.2 and the presence of trochlear dysplasia was non-significant (p = 0.48).
Discussion
The present study records some pre-operative epidemiologic data of patients with ACL injury with emphasis on the imaging of the PF joint. The most important finding of the study is the increased prevalence of trochlear dysplasia in patients with ACL injury, when compared to the incidence of trochlear dysplasia in the general population in the literature.
The prevalence of trochlear dysplasia and patella alta in the control population have been documented before. Dejour et al. showed that trochlear dysplasia with a positive ‘crossing sign’ is present in 96 % of patients with PF disorders, while they recorded it only in 3 % of 194 controls [15]. More recently, Keser et al. studied the occurrence of trochlear dysplasia using the lateral trochlea inclination index of Carrillion [18], in patients with AKP with no apparent aetiology, and found that it was present in 16.5 % of the 109 cases and in 2.7 % of the control group, which consisted of patients for meniscal pathology [21]. In this study, the authors recorded the same prevalence of trochlea dysplasia in controls with the study of Dejour, which was published 14 years ago. Botchu et al. evaluated the presence of trochlear dysplasia in patients with ‘knee pathology’, and found 58 out of 95 cases with trochlear dysplasia [27]. Although the authors confirm that this high prevalence of dysplasia does not correspond to the general population, and that their study population was biased, they found an 8.8-fold increased risk for ACL tear in patients with Dejour type A dysplasia than in patients without dysplasia [27].
In a different study, Dejour et al. reported the prevalence of the ‘crossing sign’ in 18 % of people with ‘potential patellar instability’ [15, 22] who had AKP but no history of patellar dislocation [22]. Our findings suggest that the radiographic prevalence of trochlear dysplasia in ACL-deficient patients (14.7 %) is higher than the one recorded in control groups in different studies (3 % and 2.7 %) and similar to the increased prevalence found in patients with ‘potential patellar instability’ (18 %). On the other hand, patella alta is present in 30 % of patients with ‘objective patellar instability’ with a history of true patellar dislocation, yet in 0 % of controls with no AKP and no PF instability [15, 22]. In the present study, the authors documented the presence of patella alta in 5 % of patients with ACL tears and no history of PF disorders.
The evaluation of the PF joint before ACL reconstruction is not routinely included in the everyday clinical practice and, furthermore, the diagnosis of trochlear dysplasia on X-rays requires specifically true lateral views [33]. If the lateral X-rays have not absolutely superimposed posterior femoral condyles, even small rotation of the femur up to 5° can result in significant under-estimation of the dysplasia [34]. Additionally, the presence of trochlear dysplasia should be evaluated on the sagittal plane (lateral X-rays) or transverse MRI slices rather than axial views of the patella [17, 33]. This is because dysplasia occurs in the most proximal part of the femoral trochlea [15], and the axial views of the patella in 30° of knee flexion, or more, show the tangent view of the more distal part of the trochlea which is usually deep and normal, even in knees with dysplasia [15, 17, 35, 36]. The femoral trochlear can deepen quickly for proximal to distal and therefore, axial patella views may give false-negative results of trochlear dysplasia.
There are patient-related or intrinsic factors affecting the incidence of AKP after ACL reconstruction and surgery-related or extrinsic factors. According to the literature, the most important extrinsic factors affecting AKP after ACL reconstruction are the type of autograft, pathology of the patellar tendon (e.g. ‘tendinitis’ and donor-site morbidity from BPTB harvesting), infrapatellar nerve injury, range-of-motion deficit (e.g. Cyclop’s lesion), aggressive rehabilitation protocols and pre-existing patellofemoral cartilage injuries [3, 5, 8, 37]. These sources of AKP are often a matter of controversy in literature. Some authors document a higher prevalence of AKP after reconstruction with bone-patellar tendon-bone (BPTB) grafts, especially in the early post-operative period, while others record a similar long-term prevalence of AKP among BPTB and hamstring tendon autografts [8, 37, 38]. A recent multicentric study showed that AKP is more frequent among patients treated with BPTB grafts when compared with hamstrings, but the level and the intensity of recorded pain measured in a visual analogue scale, is higher in patients receiving a hamstrings autograft [39].
In general these factors can be a cause of early AKP after ACL reconstruction. On the other hand, important intrinsic factors are increased body mass index, female gender and increased age [40, 41]. Additional intrinsic factors of AKP could be potentially the presence of trochlear dysplasia and patella alta, which in the present study showed an increased incidence among patients undergoing ACL reconstruction.
Post-operative AKP is very often attributed to patellar tendon tendinitis. The authors’ belief is that such a diagnosis should not be made lightly, because ‘tendinitis’ is in fact a diagnosis with specific histological findings and not only clinical symptoms of pain over the patellar tendon. There is not always an easy correlation to the graft used. Some articles report that AKP may occur from 42.0 % to 62 % in the early post-operative period [5, 42] and can remain in up to 20 % of these patients in the long-term, even in cases where the hamstrings were harvested [5, 43, 44]. Most authors agree that the long-term incidence of AKP is not crucially dependent on donor-site-morbidity [45]. BPTB harvesting results in higher AKP, mostly in the early post-operative period [37, 38]. Feller et al. compared the presence of AKP between BPTP and hamstring autografts and found the same incidence at two months post-operatively, but more pain and a significant quadriceps deficit in the BPTB group at four months [42]. This quadriceps muscle deficit and especially the lack of co-ordination between anterior and posterior thigh muscles has been associated with AKP by other authors. Shelbourne et al. recorded the same AKP between ACL reconstruction patients with BPTP and controls when they followed a rehabilitation program focused on quadriceps strengthening and early full extension [46]. They attributed the source of AKP not in donor side morbidity but in flexion contracture and quadriceps muscle weakness. On the other hand, Condouret et al. recorded the same incidence of AKP between BPTB and hamstrings grafts, while finding greater muscle deficit at two years post-operatively in hamstrings (17 %) compared to quadriceps (3 %) [47].
The increased prevalence of trochlear dysplasia in patients with ACL injury that the authors recorded in the present study is considered as an intrinsic factor for which the course cannot be altered by ACL surgery. In this study, the authors did not evaluate the correlation between post-operative AKP and trochlear dysplasia, and therefore safe conclusions for the aetiology of AKP in ACL-deficient patients with dysplasia cannot be made. The rationale of the study was rather an epidemiologic documentation of a sign that is usually found in patients with PF disorders like trochlear dysplasia, in a different group of ACL-deficient patients.
But both the presence of trochlear dysplasia and ACL surgery have been directly or indirectly correlated to the long-term progression to PF arthritis, whose chief complaint is AKP. More specifically, PF arthritis presents constantly with AKP, and other authors have documented that patients with established PF arthritis that required surgical treatment had a history of significantly higher AKP than controls (22 % vs 6 %, p < 0.001) [48]. The risk of long-term arthritis after ACL reconstruction has been questioned in the literature, and the possibility of PF arthritis following ACL reconstruction has been recently re-emphasized [49–51]. Järvelä et al. documented mild to severe PF osteoarthritis in 88.6 % of their patients seven years after ACL reconstruction [49] and also correlated the increased incidence of AKP in this group but, unfortunately, without evaluating for the presence of trochlear dysplasia in these patients [6]. Oiestad et al. documented 26 % of established PF arthritis 12 years after ACL reconstruction, again without checking for the pre-operative presence of similar radiological findings such as trochlear dysplasia [51]. Most recently, Culvenor et al. reviewed the increased incidence of PF arthritis with ACL reconstruction and recommended prevention and treatment strategies with attention to rehabilitation protocols and quadriceps and hamstring muscles coordination in order to minimize this complication [50]. Trochlear dysplasia has been found to be a strong associating factor for future PF arthritis [12, 52–54]. Many authors document the increased incidence of PF arthritis after high-grade dysplasia that may lead to patellar dislocation. But the risk of future PF arthritis from even low-grade dysplasia that does not necessarily lead to patellar dislocation cannot be under-estimated [55, 56]. Further studies that evaluate the correlation of post-operative AKP and future PF arthritis after ACL reconstruction with the presence of trochlear dysplasia, that seems to be increased in these patients, are required.
The clinical importance from the previous data lies on the possible association between post-operative AKP in ACL-deficient patients and the increased presence of trochlear dysplasia. The pre-operative evaluation of the PF joint with true lateral X-rays with attention to the presence of trochlear dysplasia is advised in the ACL-deficient patient. Post-operative AKP should not be dogmatically attributed to ‘tendinitis’, or aggressive rehabilitation. Trochlear dysplasia could probably be an additional risk for post-operative AKP, but cannot weaken the significance of other well-documented concomitant factors of AKP. The presence of dysplasia may adjust the rehabilitation protocols with emphasis on the conservative treatment of PF disorders, in order to attenuate the risk of AKP in the early post-operative period.
Limitations of the study include that there was no control group but we compared our results with previously published data about the prevalence of trochlea dysplasia in controls. Furthermore, there is no correlation between the presence of trochlea dysplasia and AKP, but this is just an epidemiologic study on the prevalence of radiographic signs of trochlear dysplasia in patients undergoing ACL reconstruction.
Conclusions
The most important finding of the study is the increased prevalence of trochlear dysplasia and patella alta in patients with ACL injury, when compared to the incidence of trochlear dysplasia and patella alta in the general population in the literature. This finding could sound as an alert of a possible additional risk factor for post-operative anterior knee pain after ACL reconstruction.
References
- 1.Li S, Chen Y, Lin Z, Cui W, Zhao J, Su W. A systematic review of randomized controlled clinical trials comparing hamstring autografts versus bone-patellar tendon-bone autografts for the reconstruction of the anterior cruciate ligament. Arch Orthop Trauma Surg. 2012;132(9):1287–1297. doi: 10.1007/s00402-012-1532-5. [DOI] [PubMed] [Google Scholar]
- 2.Kartus J, Magnusson L, Stener S, Brandsson S, Eriksson BI, Karlsson J. Complications following arthroscopic anterior cruciate ligament reconstruction. A 2-5-year follow-up of 604 patients with special emphasis on anterior knee pain. Knee Surg Sports Traumatol Arthrosc. 1999;7(1):2–8. doi: 10.1007/s001670050112. [DOI] [PubMed] [Google Scholar]
- 3.Safran MR, Greene HS. Avoidance and management of intra-articular complications of anterior cruciate ligament reconstruction. Instr Course Lect. 2006;55:475–488. [PubMed] [Google Scholar]
- 4.Tjoumakaris FP, Herz-Brown AL, Bowers AL, Sennett BJ, Bernstein J. Complications in brief: Anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 2012;470(2):630–636. doi: 10.1007/s11999-011-2153-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Niki Y, Hakozaki A, Iwamoto W, Kanagawa H, Matsumoto H, Toyama Y, Suda Y. Factors affecting anterior knee pain following anatomic double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20(8):1543–1549. doi: 10.1007/s00167-011-1746-z. [DOI] [PubMed] [Google Scholar]
- 6.Jarvela T, Kannus P, Jarvinen M. Anterior knee pain 7 years after an anterior cruciate ligament reconstruction with a bone-patellar tendon-bone autograft. Scand J Med Sci Sports. 2000;10(4):221–227. doi: 10.1034/j.1600-0838.2000.010004221.x. [DOI] [PubMed] [Google Scholar]
- 7.Barber-Westin SD, Noyes FR, Andrews M. A rigorous comparison between the sexes of results and complications after anterior cruciate ligament reconstruction. Am J Sports Med. 1997;25(4):514–526. doi: 10.1177/036354659702500415. [DOI] [PubMed] [Google Scholar]
- 8.Kartus J, Movin T, Karlsson J. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy. 2001;17(9):971–980. doi: 10.1053/jars.2001.28979. [DOI] [PubMed] [Google Scholar]
- 9.Arendt EA, Fithian DC, Cohen E. Current concepts of lateral patella dislocation. Clin Sports Med. 2002;21(3):499–519. doi: 10.1016/S0278-5919(02)00031-5. [DOI] [PubMed] [Google Scholar]
- 10.Sanchis-Alfonso V, Rosello-Sastre E, Martinez-Sanjuan V. Pathogenesis of anterior knee pain syndrome and functional patellofemoral instability in the active young. Am J Knee Surg. 1999;12(1):29–40. [PubMed] [Google Scholar]
- 11.Fulkerson JP, Arendt EA. Anterior knee pain in females. Clin Orthop Relat Res. 2000;372:69–73. doi: 10.1097/00003086-200003000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Andrish J. The management of recurrent patellar dislocation. Orthop Clin North Am. 2008;39(3):313–327. doi: 10.1016/j.ocl.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 13.Eckhoff DG, Montgomery WK, Kilcoyne RF, Stamm ER. Femoral morphometry and anterior knee pain. Clin Orthop Relat Res. 1994;302:64–68. [PubMed] [Google Scholar]
- 14.Colvin AC, West RV. Patellar instability. J Bone Joint Surg Am. 2008;90(12):2751–2762. doi: 10.2106/JBJS.H.00211. [DOI] [PubMed] [Google Scholar]
- 15.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 16.Fucentese SF, von Roll A, Koch PP, Epari DR, Fuchs B, Schottle PB. The patella morphology in trochlear dysplasia—a comparative MRI study. Knee. 2006;13(2):145–150. doi: 10.1016/j.knee.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 17.Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc. 2007;15(1):39–46. doi: 10.1097/JSA.0b013e31803035ae. [DOI] [PubMed] [Google Scholar]
- 18.Carrillon Y, Abidi H, Dejour D, Fantino O, Moyen B, Tran-Minh VA. Patellar instability: assessment on MR images by measuring the lateral trochlear inclination-initial experience. Radiology. 2000;216(2):582–585. doi: 10.1148/radiology.216.2.r00au07582. [DOI] [PubMed] [Google Scholar]
- 19.McNally EG. Imaging assessment of anterior knee pain and patellar maltracking. Skeletal Radiol. 2001;30(9):484–495. doi: 10.1007/s002560100401. [DOI] [PubMed] [Google Scholar]
- 20.Bollier M, Fulkerson JP. The role of trochlear dysplasia in patellofemoral instability. J Am Acad Orthop Surg. 2011;19(1):8–16. doi: 10.5435/00124635-201101000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Keser S, Savranlar A, Bayar A, Ege A, Turhan E. Is there a relationship between anterior knee pain and femoral trochlear dysplasia? Assessment of lateral trochlear inclination by magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc. 2008;16(10):911–915. doi: 10.1007/s00167-008-0571-5. [DOI] [PubMed] [Google Scholar]
- 22.Dejour H, Walch G, Neyret P, Adeleine P. Dysplasia of the femoral trochlea. Rev Chir Orthop Reparatrice Appar Mot. 1990;76(1):45–54. [PubMed] [Google Scholar]
- 23.Dejour D, Byn P, Ntagiopoulos PG. The Lyon’s sulcus-deepening trochleoplasty in previous unsuccessful patellofemoral surgery. Int Orthop. 2013;37(3):433–439. doi: 10.1007/s00264-012-1746-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dejour D, Saggin P. The sulcus deepening trochleoplasty-the Lyon’s procedure. Int Orthop. 2010;34(2):311–316. doi: 10.1007/s00264-009-0933-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ntagiopoulos PG, Byn P, Dejour D. Midterm results of comprehensive surgical reconstruction including sulcus-deepening trochleoplasty in recurrent patellar dislocations with high-grade trochlear dysplasia. Am J Sports Med. 2013;41(5):998–1004. doi: 10.1177/0363546513482302. [DOI] [PubMed] [Google Scholar]
- 26.Pecina M, Ivkovic A, Hudetz D, Smoljanovic T, Jankovic S. Sagittal osteotomy of the patella after Morscher. Int Orthop. 2010;34(2):297–303. doi: 10.1007/s00264-009-0923-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Botchu R, Obaid H, Rennie WJ. Correlation between trochlear dysplasia and the notch index. J Orthop Surg. 2013;21(3):290–293. doi: 10.1177/230949901302100305. [DOI] [PubMed] [Google Scholar]
- 28.Luyckx T, Didden K, Vandenneucker H, Labey L, Innocenti B, Bellemans J. Is there a biomechanical explanation for anterior knee pain in patients with patella alta?: influence of patellar height on patellofemoral contact force, contact area and contact pressure. J Bone Joint Surg Br. 2009;91(3):344–350. doi: 10.1302/0301-620X.91B3.21592. [DOI] [PubMed] [Google Scholar]
- 29.Kujala UM, Osterman K, Kvist M, Aalto T, Friberg O. Factors predisposing to patellar chondropathy and patellar apicitis in athletes. Int Orthop. 1986;10(3):195–200. doi: 10.1007/BF00266208. [DOI] [PubMed] [Google Scholar]
- 30.Lancourt JE, Cristini JA. Patella alta and patella infera. Their etiological role in patellar dislocation, chondromalacia, and apophysitis of the tibial tubercle. J Bone Joint Surg Am. 1975;57(8):1112–1115. [PubMed] [Google Scholar]
- 31.Kannus PA. Long patellar tendon: radiographic sign of patellofemoral pain syndrome–a prospective study. Radiology. 1992;185(3):859–863. doi: 10.1148/radiology.185.3.1438776. [DOI] [PubMed] [Google Scholar]
- 32.Caton J, Deschamps G, Chambat P, Lerat JL, Dejour H. Patella infera. Apropos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot. 1982;68(5):317–325. [PubMed] [Google Scholar]
- 33.Pfirrmann CW, Zanetti M, Romero J, Hodler J. Femoral trochlear dysplasia: MR findings. Radiology. 2000;216(3):858–864. doi: 10.1148/radiology.216.3.r00se38858. [DOI] [PubMed] [Google Scholar]
- 34.Koeter S, Bongers EM, de Rooij J, van Kampen A. Minimal rotation aberrations cause radiographic misdiagnosis of trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):713–717. doi: 10.1007/s00167-005-0031-4. [DOI] [PubMed] [Google Scholar]
- 35.Laprade J, Culham E. Radiographic measures in subjects who are asymptomatic and subjects with patellofemoral pain syndrome. Clin Orthop Relat Res. 2003;414:172–182. doi: 10.1097/01.blo.0000079269.91782.f5. [DOI] [PubMed] [Google Scholar]
- 36.Walker C, Cassar-Pullicino VN, Vaisha R, McCall IW. The patello-femoral joint–a critical appraisal of its geometric assessment utilizing conventional axial radiography and computed arthro-tomography. Br J Radiol. 1993;66(789):755–761. doi: 10.1259/0007-1285-66-789-755. [DOI] [PubMed] [Google Scholar]
- 37.Samuelsson K, Andersson D, Karlsson J. Treatment of anterior cruciate ligament injuries with special reference to graft type and surgical technique: an assessment of randomized controlled trials. Arthroscopy. 2009;25(10):1139–1174. doi: 10.1016/j.arthro.2009.07.021. [DOI] [PubMed] [Google Scholar]
- 38.Bach BR, Jr, Tradonsky S, Bojchuk J, Levy ME, Bush-Joseph CA, Khan NH. Arthroscopically assisted anterior cruciate ligament reconstruction using patellar tendon autograft. Five- to nine-year follow-up evaluation. Am J Sports Med. 1998;26(1):20–29. doi: 10.1177/03635465980260012101. [DOI] [PubMed] [Google Scholar]
- 39.Gaudot F, Chalencon F, Nourissat G, Dejour D, Potel JF, Frischty D, Beaufils P, Societe francaise da [Impact of anterior knee pain on mid term outcome after anterior cruciate ligament reconstruction] Rev Chir Orthop Reparatrice Appar Mot. 2008;94(8):372–374. doi: 10.1016/j.rco.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 40.Aglietti P, Buzzi R, D’Andria S, Zaccherotti G. Patellofemoral problems after intraarticular anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 1993;288:195–204. [PubMed] [Google Scholar]
- 41.Stapleton TR. Complications in anterior cruciate ligament reconstructions with patellar tendon grafts. Sports Med Arthrosc Rev. 1997;5:156–162. doi: 10.1097/00132585-199700520-00011. [DOI] [Google Scholar]
- 42.Feller JA, Webster KE, Gavin B. Early post-operative morbidity following anterior cruciate ligament reconstruction: patellar tendon versus hamstring graft. Knee Surg Sports Traumatol Arthrosc. 2001;9(5):260–266. doi: 10.1007/s001670100216. [DOI] [PubMed] [Google Scholar]
- 43.Zaffagnini S, Bruni D, Marcheggiani Muccioli GM, Bonanzinga T, Lopomo N, Bignozzi S, Marcacci M. Single-bundle patellar tendon versus non-anatomical double-bundle hamstrings ACL reconstruction: a prospective randomized study at 8-year minimum follow-up. Knee Surg Sports Traumatol Arthrosc. 2011;19(3):390–397. doi: 10.1007/s00167-010-1225-y. [DOI] [PubMed] [Google Scholar]
- 44.Lewis PB, Parameswaran AD, Rue JP, Bach BR., Jr Systematic review of single-bundle anterior cruciate ligament reconstruction outcomes: a baseline assessment for consideration of double-bundle techniques. Am J Sports Med. 2008;36(10):2028–2036. doi: 10.1177/0363546508322892. [DOI] [PubMed] [Google Scholar]
- 45.Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE., Jr Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med. 2004;32(8):1986–1995. doi: 10.1177/0363546504271211. [DOI] [PubMed] [Google Scholar]
- 46.Shelbourne KD, Trumper RV. Preventing anterior knee pain after anterior cruciate ligament reconstruction. Am J Sports Med. 1997;25(1):41–47. doi: 10.1177/036354659702500108. [DOI] [PubMed] [Google Scholar]
- 47.Condouret J, Cohn J, Ferret JM, Lemonsu A, Vasconcelos W, Dejour D, Potel JF, Societe francaise da [Isokinetic assessment with two years follow-up of anterior cruciate ligament reconstruction with patellar tendon or hamstring tendons] Rev Chir Orthop Reparatrice Appar Mot. 2008;94(8):375–382. doi: 10.1016/j.rco.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 48.Utting MR, Davies G, Newman JH. Is anterior knee pain a predisposing factor to patellofemoral osteoarthritis? Knee. 2005;12(5):362–365. doi: 10.1016/j.knee.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 49.Jarvela T, Paakkala T, Kannus P, Jarvinen M. The incidence of patellofemoral osteoarthritis and associated findings 7 years after anterior cruciate ligament reconstruction with a bone-patellar tendon-bone autograft. Am J Sports Med. 2001;29(1):18–24. doi: 10.1177/03635465010290010701. [DOI] [PubMed] [Google Scholar]
- 50.Culvenor AG, Cook JL, Collins NJ, Crossley KM. Is patellofemoral joint osteoarthritis an under-recognised outcome of anterior cruciate ligament reconstruction? A narrative literature review. Br J Sports Med. 2013 doi: 10.1136/bjsports-2012-091490. [DOI] [PubMed] [Google Scholar]
- 51.Oiestad BE, Holm I, Engebretsen L, Aune AK, Gunderson R, Risberg MA. The prevalence of patellofemoral osteoarthritis 12 years after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):942–949. doi: 10.1007/s00167-012-2161-9. [DOI] [PubMed] [Google Scholar]
- 52.Mulford JS, Wakeley CJ, Eldridge JD. Assessment and management of chronic patellofemoral instability. J Bone Joint Surg Br. 2007;89(6):709–716. doi: 10.1302/0301-620X.89B6.19064. [DOI] [PubMed] [Google Scholar]
- 53.Von Knoch F, Bohm T, Burgi ML, Von Knoch M, Bereiter H. Trochleaplasty for recurrent patellar dislocation in association with trochlear dysplasia. A 4- to 14-year follow-up study. J Bone Joint Surg Br. 2006;88(10):1331–1335. doi: 10.1302/0301-620X.88B10.17834. [DOI] [PubMed] [Google Scholar]
- 54.Maenpaa H, Lehto MU. Patellofemoral osteoarthritis after patellar dislocation. Clin Orthop Relat Res. 1997;339:156–162. doi: 10.1097/00003086-199706000-00021. [DOI] [PubMed] [Google Scholar]
- 55.Delanois RE, McGrath MS, Ulrich SD, Marker DR, Seyler TM, Bonutti PM, Mont MA. Results of total knee replacement for isolated patellofemoral arthritis: when not to perform a patellofemoral arthroplasty. Orthop Clin North Am. 2008;39(3):381–388. doi: 10.1016/j.ocl.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 56.Newman JH. Patellofemoral arthritis and its management with isolated patellofemoral replacement: a personal experience. Orthopedics. 2007;30(8 Suppl):58–61. [PubMed] [Google Scholar]