Abstract
Purpose
The purpose of this study was to compare the clinical outcomes of patients undergoing total hip arthroplasty (THA) who had been using narcotic medications prior to surgery to those who had not used them.
Methods
Fifty-four patients (62 hips) who had required opioid analgesia for hip pain in the three months prior to THA were compared to a matched group of opioid-naïve patients. Narcotic consumption was converted to a standardized morphine equivalent dose and compared between both groups of patients during their hospital stay, after six weeks, and at final follow-up. Other outcome measures included clinical outcome scores and the proportion of patients remaining on narcotic pain medication at final follow-up.
Results
The narcotic group required significantly higher total daily opioid doses as inpatients had a longer hospital stay and a higher proportion of patients who remained on opioids at six weeks and at final follow-up. Of the patients who were taking opioids pre-operatively, 81 % were able to wean off opioids at final follow-up. At a mean post-operative follow-up of 58 months (range, 24–258 months), Harris hip scores were lower in the narcotic group, with a mean of 84 compared to 91 points in the matching group. However, in both cohorts, there were significant improvements in Harris hip scores compared to pre-operative outcomes.
Conclusions
Patients who use narcotics prior to total hip arthroplasty may be more likely to suffer from opioid-induced hyperalgesia after surgery and have worse clinical outcomes. When possible, efforts should be made to use other modes of analgesia or wean patients from their use prior to total hip arthroplasty.
Keywords: Opioid, Total hip arthroplasty, Clinical outcomes, Implant survivorship, Narcotics, Harris hip score, Pain, Total hip replacement
Introduction
Osteoarthritis of the hip currently affects as many as 9.2 % of all adults in the United States [1, 2]. Several professional societies have released treatment recommendations to manage the broad spectrum of symptoms associated with this disease [3–6]. Most agree on a multifactorial regimen beginning with physical therapy, strengthening exercises, and pain medications such as acetaminophen and non-steroidal anti-inflammatory drugs. When these measures are no longer effective, recommendations are for the use of stronger pain medications, such as opioid derivatives, and eventually performing surgical procedures, such as total hip arthroplasty. The use of opioids is becoming more generally accepted for the treatment for osteoarthritis after other medications have failed [7]. The American Geriatric Society has advocated for their use for the long-term management of chronic pain associated with osteoarthritis, due to the high risk of developing gastric ulcers with long-term non-steroidal anti-inflammatory use [3].
A number of patients presenting to their orthopaedic surgeon for total hip arthroplasty have previously been managed with opioid-derived medications. Some reports have concluded that chronic narcotic use prior to any surgery is an independent predictor of poorer outcomes [8, 9]. Lawrence et al. found that chronic narcotic users had worse outcomes after cervical spine fusion procedures when compared to other patients [9]. The reason for this is not completely understood, but is thought to be multifactorial and may result in opioid-induced hyperalgesia and poorly controlled post-operative pain [10–12]. Patients with severe pain that is not appropriately managed post-operatively have been shown to have worse outcomes [13–15]. However, there is a paucity of literature that specifically addresses the effects of narcotic use on outcomes in total hip arthroplasty despite the increasing use of these medications.
The purpose of this study was to evaluate chronic narcotic users who underwent total hip arthroplasty and compare their outcomes to a matched group of patients who had a hip arthroplasty and were not on narcotic medications prior to surgery. We compared: (1) consumption of narcotics immediately after surgery, (2) continued narcotic use at the six-week post-operative visit and at approximately five-year follow-up, (3) length of hospital or rehabilitation stay, (4) Harris hip score, and (5) radiographic outcomes.
Methods
Fifty-four patients (62 hips) who had used narcotics prior to total hip arthroplasty were identified from the entire prospectively collected database at two institutions that specialize in lower extremity total joint arthroplasty. These patients were compared to a matched group of patients who had not used opioid medications pre-operatively. Institutional review board approval was obtained for this study.
Inclusion criteria was patients who had a minimum of six weeks of narcotic use that was greater than, or equal, to 30 mg of morphine a day (equivalent to slightly more than one hydromorphone 5 mg tab per day) [10]. This was based on the findings of Chu et al. that opioid hyperalgesia may develop in as little as four weeks of daily opioid use [16, 17]. Narcotic dose and usage was collected and verified through clinic charts, in-patient hospital medication administration records, prescription documentation, and phone interviews.
The daily total consumption of narcotic medication was summed and converted to a morphine equivalent dose. This was adapted and standardized for all patients based on the recommendations and guidelines released by Pereira et al., the American Pain Society, and the American Academy of Pain Medicine (Table 1) [17–20]. No specific morphine equivalent dose has been reported for transdermal fentanyl and, therefore, the means of the ranges reported in the literature were used for different doses (Table 2) [18]. The morphine equivalent dose was calculated for all patients within one month prior to surgery, every day during hospital admission, at a six-week post-operative follow-up appointment, and at their most recent follow-up.
Table 1.
Morphine equivalent dosage conversions
| Opioid | Administration | Morphine equivalent dose (mg) |
|---|---|---|
| Morphine (30 mg) | PO | – |
| Codeine | PO | 3 |
| Hydrocodone | PO | 30 |
| Hydromorphone | IV | 150 |
| Methadone | PO | 3.75 |
| Morphine | IV | 1.5 |
| Meperdidine | PO | 300 |
| IV | 10 | |
| Oxycodone | PO | 20 |
| IV | 75 | |
| Propoxyphenea | PO | 130 |
| Tramadol | PO | 3 |
PO per os, IV intravenous
aCurrently not available in the United States
Table 2.
Conversion of fentanyl patch dosage to morphine equivalent dose
| Fentanyl patch dose (mcg/hr) |
Reported range (mg/d) |
Morphine equivalent dose (mg) |
|---|---|---|
| 25 | 60–134 | 97 |
| 50 | 135–224 | 128 |
| 75 | 225–314 | 269 |
| 100 | 315–404 | 359 |
| 125 | 405–494 | 449 |
| 150 | 495–584 | 539 |
| 175 | 585–674 | 629 |
mcg microgram, hr hour, d day, mg milligram
In the narcotic use group, there were 27 men and 27 women who had a mean age of 55 years (range, 27–83 years), a mean body mass index of 30.2 m/kg² (range, 18.3–62.0 m/kg²), and had a mean follow-up of 58 months (range, 24–258 months). Two additional narcotic using patients who met the threshold for inclusion were excluded because they lacked the appropriate follow-up (both lived over 500 miles away).
Patients in the comparison (non-narcotic) group, who did not take narcotics prior to total hip arthroplasty, were matched by gender, unilateral or bilateral total hip arthroplasty (exact), age (within five years), and body mass index (within 4 kg/m²) (Table 3). Two patients in the non-narcotic group were using minimal doses of narcotics that did not meet the inclusion criteria for this study (morphine equivalent doses of 7.5 and 15); the remaining patients in the non-narcotic group had no recorded use of narcotic medications prior to surgery. In an attempt to eliminate any possible confounding factors, additional comorbidities and demographic factors (insurance type, tobacco use ≥0.5 packs per day, history of psychiatric disorders, history of back pain or surgery), were matched when possible.
Table 3.
Comparison of narcotic users to matched non-narcotic user group
| Variable | Narcotic group | Non-narcotic group | p-value |
|---|---|---|---|
| Hips (patients) | 62 (61) | 62 (61) | – |
| Age (years) | 55 | 55 | – |
| Men:women | 33:28 | 33:28 | – |
| Body mass index (kg/m²) | 30.2 | 29.9 | – |
| Pre-operative Harris hip score (points) | 43 | 45 | 0.26 |
| Pre-operative UCLA activity score (points) | 3.2 | 3.9 | 0.002 |
| Demographic information | |||
| Active smoker (≥ 0.5 PPD) Back pain Back surgery Psychiatric condition Corticosteroid use Alcohol abuse Workers compensation |
14 11 7 16 10 7 2 |
12 14 10 7 6 6 1 |
0.83 0.24 0.6 0.03 0.42 0.77 0.56 |
| ASA score | |||
| Class I Class II Class III Class IV |
12 31 18 0 |
16 34 11 0 |
0.39 0.72 0.13 – |
UCLA University of California, Los Angeles
All patients underwent a standardized hospital course for total hip arthroplasty. All procedures were performed though an antero-lateral approach with general anaesthesia. Post-operatively, pain was managed with either a patient-controlled analgesia device using either morphine (2 mg/h) or hydromorphone (0.3 mcg/h). An epidural catheter was required for pain control in five patients (narcotic group = 3, non-narcotic group = 2). Prior to discharge, all patients were transitioned to oral pain medications (oxycodone 20 mg and oxycodone/acetaminophen 5/235 mg) and discharged home or to an acute rehabilitation facility.
Hospital charts were reviewed to determine the type of anaesthesia used, length of hospital stay, and narcotic usage during admission. Narcotic consumption was recorded and grouped by post-operative day until time of discharge. The total narcotic doses were then converted to morphine equivalent doses to quantify the daily narcotic usage during admission. Patients whose pain was initially controlled with an epidural were excluded from analysis during the days that the epidural was in place.
Patients were seen in the office at post-operative follow-up visits at approximately six weeks, three months, six months, and annually thereafter, to evaluate for any complications or need for revision. Patients’ pain was routinely assessed at all visits and documented in office charts, regardless of whether the patient was given a prescription for a pain medication. Daily use of medication was re-verified at subsequent visits based on patient reported use and how often prescription medications required refills. Patients requiring pain medications for more than 90 days post-operatively were referred to pain management specialists.
Outcomes were assessed by the senior author with Harris hip scores, range-of-motion, and University of California, Los Angeles activity scores at all post-operative visits [21, 22]. Antero-posterior and cross-table lateral radiographs were obtained during post-operative visits and evaluated for any signs of progressive radiolucencies or component migration.
Demographic information was collected on all patients to control for possible confounders [23–26]. These variables included, age, tobacco use, alcohol use, history of back pain or back surgery, history of any psychiatric conditions, corticosteroid use, and workers’ compensation status (Table 3). The narcotic group had a significantly higher amount of patients with concurrent psychiatric disorders (p = 0.036). There were no significant differences in tobacco use, history of back pain/surgery, corticosteroid use, alcohol abuse, or worker’s compensation insurance type between the two groups. There was no significant difference in the prevalence of major comorbidities in the two groups (Table 4).
Table 4.
Total comorbidities for each study group
| Variable | Narcotic group | Non-narcotic group | p-value |
|---|---|---|---|
| Total comorbidities | 109 | 104 | - |
| Hypertension | 27 | 24 | 0.5 |
| Hyperlipidemia | 4 | 10 | 0.1 |
| Diabetes | 6 | 3 | 0.5 |
| Coronary artery disease | 3 | 4 | 0.7 |
| Asthma | 6 | 6 | 1.0 |
| COPD | 3 | 2 | 1.0 |
| GERD | 10 | 8 | 0.8 |
| Hypothyroidism | 3 | 6 | 0.3 |
COPD chronic obstructive pulmonary disease, GERD gastro-esophageal reflux disease
Statistical methods
All data were collected and analysed using SPSS Statistics v17.0.1 (SPSS Inc., Chicago, Illinois) and GraphPad Prism software version 5.01 (GraphPad Software Inc., La Jolla, California). Differences between the narcotic and non-narcotic groups in terms of length of hospitalization, Harris hip scores, University of California, Los Angeles scores, and daily morphine equivalent doses were compared using paired and unpaired t-tests where appropriate. Pearson’s exact test was used to determine significance between demographic characteristics between the groups where appropriate. A p value of <0.05 was used to determine significance.
Results
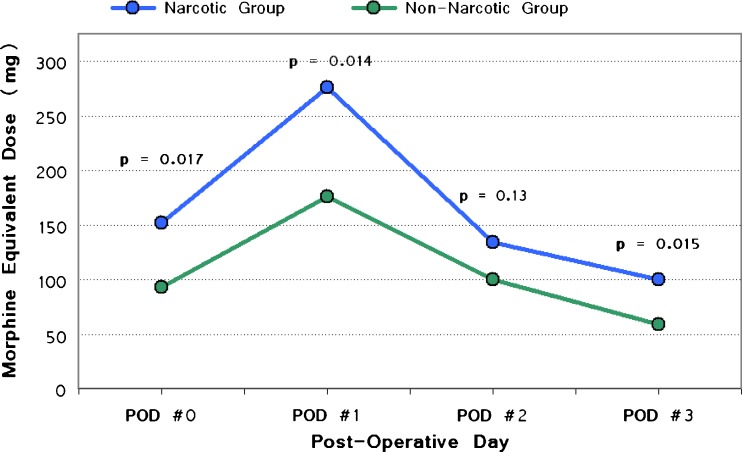
Patients in the narcotic group used a significantly greater amount of narcotics during post-operative day zero (p = 0.017), one (p = 0.014), and three (p = 0.015) (Fig. 1). Narcotic consumption was higher in the opioid group on post-operative day two, although this was not statistically significant (p = 0.13).
Fig. 1.
Mean total morphine equivalent dose (MED) consumption in milligrams during hospital admission. P value for each post-operative day denoted above corresponding data point
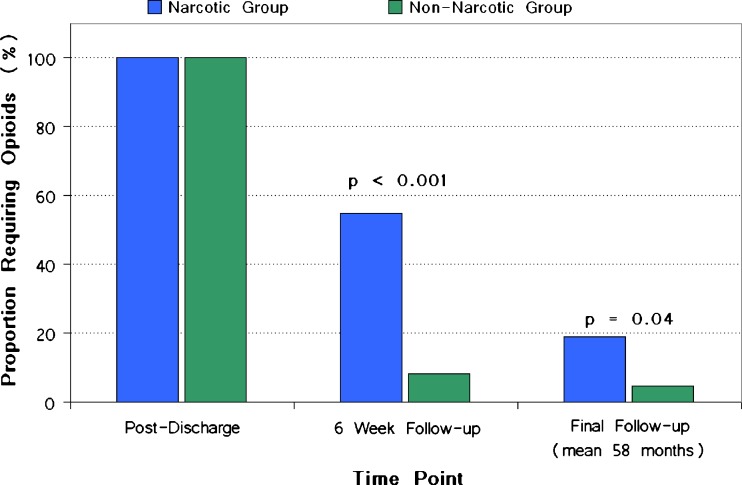
Following discharge, there were a significantly higher number of patients in the narcotic group who were still using opioids at six week follow-up (Fig. 2). The morphine equivalent doses were significantly higher in this group compared to the non-narcotic group (p < 0.001). The mean morphine equivalent dose of the narcotic group at six weeks was 63 mg/day, compared to the non-narcotic group, which was 2 mg/day. A significantly higher proportion of patients in the narcotic group continued to use opioids at final follow-up (19 % versus 4 %; p = 0.04) (Fig. 2).
Fig. 2.
Proportion of patients requiring narcotics for pain control following primary total hip arthroplasty
The mean hospital stay in the narcotic group was four days (range, two to ten days) compared to three days (range, two to eight days) in the non-narcotic group, which was statistically significant (p = 0.01). No difference was observed in the frequency of patients being discharged to acute care rehabilitation facilities (p = 0.37, narcotic group = 30 versus the non-narcotic group = 24), or between the length of stay among the patients at these facilities (p = 0.9).
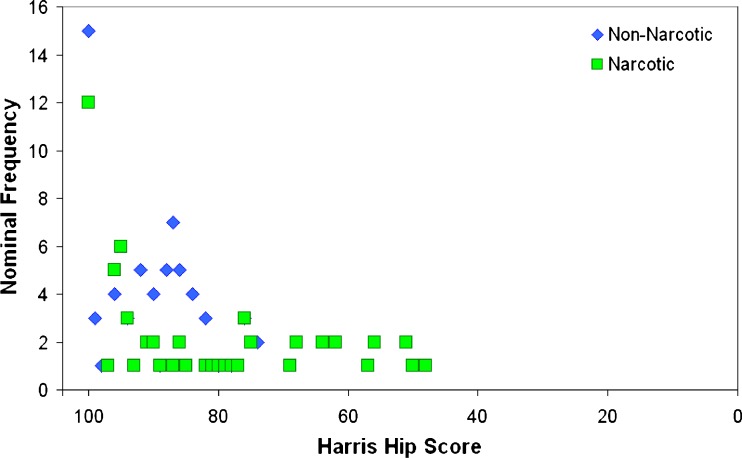
Clinical outcomes diverged with patients in the narcotic group demonstrating lower Harris hip scores at final follow-up (Fig. 3). At six week follow-up, no significant difference was seen in the Harris hip score between the two groups (p = 0.7); however, at final follow-up, the narcotic group had significantly worse clinical outcomes (Fig. 3). In the narcotic cohort, the mean Harris hip score at final follow-up was 84 points (range, 48–100 points) and significantly lower than 91 points (range, 74–100 points) in the comparison cohort (p = 0.002). However, in both cohorts, there were significant improvements when these outcomes were compared to pre-operative values (p = 0.01) (Table 3). The mean University of California, Los Angeles activity score in the narcotic group was 7 points (range, 3–10 points), compared to 8 points (range, 5–10 points) in the non-narcotic group (p = 0.14). No significant difference was observed in clinical scores at final follow-up when patients were sub-stratified by the presence of a psychiatric history (Table 5).
Fig. 3.
Distribution of mean post-operative Harris hip scores at final follow-up for the narcotic and non-narcotic group
Table 5.
Comparison of mean Harris hip scores at long-term follow-up in patients with an underlying psychiatric disease
| Group | Harris hip score | p-value | |
|---|---|---|---|
| Psychiatric history | No psychiatric history | ||
| Narcotic group (n = 16) | 79 (51–100) | 86 (48–100) | 0.2 |
| Non-narcotic group (n = 7) | 91 (78–100) | 91 (74–100) | 0.9 |
The mean radiographic follow-up was 42 months (range, 24–108 months). Radiographic evaluation demonstrated stable femoral component position in all patients. Radiolucencies were observed around the acetabular cup in two hips for the narcotic group and one hip in the non-narcotic group, all of which required a revision.
In total there were four revisions during the study period. Two revision surgeries were performed in both the narcotic and non-narcotic group. The mean time between index arthroplasty and revision was 17 months (range, 1–50 months). Three revisions were due to failure of the acetabular component due to loosening and one secondary to recurrent dislocations (three dislocations within one month after surgery). No patient underwent revision for pain alone.
Discussion
Patients suffering from osteoarthritis of the hip often undergo several different non-operative treatments before presenting to an orthopaedic surgeon for consult. Jordan et al. found that at the time of presentation, 28 % of patients with hip pain already had advanced stages of osteoarthritis on radiographic analysis [27]. Additionally, the use of opioid medications as a first-line treatment is becoming more prevalent among patients with osteoarthritis even though their use for an extended period of time prior to surgery may more likely cause opioid-induced hyperalgesia and a prolonged recovery [10, 11]. This study demonstrated that patients using opioid medications prior to surgery may be more likely to have a longer hospital course, have worse clinical outcomes, and use a significantly higher amount of narcotics post-operatively. However, even in a group of patients who required pre-operative opioid analgesia, 81 % were able to wean themselves off narcotics.
There were some inherent limitations with the retrospective design of this study. While patients were interviewed as objectively as possible, there is still the potential for recall bias concerning how much narcotic medications they were taking prior to or after surgery. Additionally, patients may have concealed narcotic medication usage from other sources, such as primary care physicians. However, the authors of this study believe that these factors would minimally affect the overall results since the data for all opioid medications are reported to a state regulatory body to prevent duplicative prescriptions. An additional limitation to this study was that the pre-operative University of California, Los Angeles activity scores were found to be lower in the narcotic compared non-narcotic group (mean 3 versus 4 points, respectively). Because of the small differences of these scores and the similarity between the two groups in terms of Harris hip scores, we do not believe that this altered our results or conclusions.
Similar results have been reported in the orthopaedic literature, although not necessarily in the total joint arthroplasty literature. Lawrence et al. retrospectively reviewed 47 patients undergoing cervical spinal fusion who were on opioid medications for greater than six months prior to surgery and compared them to a similar group of 44 patients who had not used these medications [9]. At a mean follow-up of 31 months (range, 24–64 months), 16 patients (34 %) from the narcotic group were still on some form of opioid medication to control their pain compared to three patients (7 %) in the non-narcotic group. Additionally, the narcotic group had fewer patients who reported good or excellent results after surgery and had a significantly higher number of patients who reported a worse result after surgery (p < 0.001). Franklin et al. retrospectively reviewed the use of narcotics prior to total knee arthroplasty on 6,364 patients and found that at a mean follow-up of 12 months, patients who had been using narcotics prior to surgery were more likely to still be on some form of narcotic for knee pain and be dissatisfied with their surgery [28].
Apart from delayed hospital discharge, patient dissatisfaction, and poorer clinical outcomes, chronic opioid use has been well documented to negatively impact patient ability to return to work and lead a productive, independent life [29–32]. Kidner et al. evaluated 1,226 patients at acute rehabilitation facilities who were admitted for treatment of chronic musculoskeletal conditions and were treated with opioid analgesics [33]. At one year follow-up, they found that patients in the higher narcotic dosage groups were less likely to return to work, more likely to be receiving Social Security Disability Income, and that chronic opioid use was a predictor of less successful outcomes.
The effect of psychiatric conditions also cannot be understated. We observed that patients using narcotics prior to surgery were significantly more likely to have an underlying psychiatric condition compared to other patients, and that these patients had lower post-operative clinical scores. Similar results were observed by Singh and Lewallen who determined that a history of depression was a significant independent predictor of functional limitation and narcotic use after revision total hip arthroplasty [26].
Although the data in the present study clearly shows worse long-term clinical results, higher in-hospital opioid dose requirements, and greater levels of continued narcotic use following total hip arthroplasty in patients who utilized opioid analgesics pre-operatively, we believe there are some positive conclusions. Most importantly, 81 % of the patients who had been on chronic narcotic pain medications were able to wean themselves off, with 50 % requiring no further pain control within six weeks of hospital discharge. However, it is our recommendation that efforts be made to taper patients from using opioid-derived medications as much as possible prior to undergoing total hip arthroplasty, which may decrease the incidence of opioid-induced hyperalgesia, decrease narcotic use during hospital stay, and increase the likelihood of a successful recovery. At the present time in our practice, we do attempt to wean patients off narcotics prior to surgery. In particular, we work closely with pain management specialists and counsel patients at their pre-operative visit regarding the importance of decreased opioid use. Since many of our patients are initially managed with a course of rehabilitation therapy which includes both injections and physical therapy, we do attempt to educate and encourage patients to decrease their opioid use. We are currently looking at our data regarding the success of decreasing opioid consumption and will report on these findings in a future study.
Acknowledgments
Disclosures
RP is a paid consultant for DJO.
BHK is a consultant for Sage products Inc.
PMB receives royalties from Arthrocare; Stryker; Synthes; Biomet; Joint Active Systems, Inc., Acacia Research Group, LLC, is a consultant for Stryker and Biomet, and has Stock or Stock options in Joint Active Systems, Inc.
MAM receives royalties from Stryker Orthopaedics; is a paid consultant for Johnson & Johnson, Sage Products, Medtronic, TissueGene, Stryker Orthopaedics, OnGoing Care Solutions, Inc. and Wright Medical Technologies, Inc.; and receives research support from National Institutes of Health (NIAMS and NICHD), Sage Products, Stryker Orthopaedics, TisseGene, and Wright Medical Technologies, Inc.
KI and QN have no disclosures.
References
- 1.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58(1):26. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Helmick CG, Felson DT, Lawrence RC, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis Rheum. 2008;58(1):15. doi: 10.1002/art.23177. [DOI] [PubMed] [Google Scholar]
- 3.American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons Pharmacological management of persistent pain in older persons. Pain Medicine. 2009;10(6):1062. doi: 10.1111/j.1526-4637.2009.00699.x. [DOI] [PubMed] [Google Scholar]
- 4.Gloth FM. Pharmacological management of persistent pain in older persons: focus on opioids and nonopioids. J Pain. 2011;12(3 Suppl 1):S14. doi: 10.1016/j.jpain.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 5.Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage. 2008;16(2):137. doi: 10.1016/j.joca.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 6.Jordan KM, Arden NK, Doherty M, et al. Standing Committee for International Clinical Studies Including Therapeutic Trials E. EULAR Recommendations 2003: an evidence based approach to the management of knee osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT) Ann Rheum Dis. 2003;62(12):1145. doi: 10.1136/ard.2003.011742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glauser TA, Salinas GD, Roepke NL, et al. Management of mild-to-moderate osteoarthritis: a study of the primary care perspective. Postgrad Med. 2011;123(1):126. doi: 10.3810/pgm.2011.01.2254. [DOI] [PubMed] [Google Scholar]
- 8.Webster BS, Verma SK, Gatchel RJ, et al. Relationship between early opioid prescribing for acute occupational low back pain and disability duration, medical costs, subsequent surgery and late opioid use. Spine (Phila Pa 1976) 2007;32(19):2127. doi: 10.1097/BRS.0b013e318145a731. [DOI] [PubMed] [Google Scholar]
- 9.Lawrence JT, London N, Bohlman HH, et al. Preoperative narcotic use as a predictor of clinical outcome: results following anterior cervical arthrodesis. Spine (Phila Pa 1976) 2008;33(19):2074. doi: 10.1097/BRS.0b013e3181809f07. [DOI] [PubMed] [Google Scholar]
- 10.Lee M, Silverman SM, Hansen H, et al. A comprehensive review of opioid-induced hyperalgesia. Pain Physician. 2011;14(2):145. [PubMed] [Google Scholar]
- 11.Guignard B, Bossard AE, Coste C, et al. Acute opioid tolerance: intraoperative remifentanil increases postoperative pain and morphine requirement. Anesthesiology. 2000;93(2):409. doi: 10.1097/00000542-200008000-00019. [DOI] [PubMed] [Google Scholar]
- 12.Chia YY, Liu K, Wang JJ, et al. Intraoperative high dose fentanyl induces postoperative fentanyl tolerance. Can J Anaesth. 1999;46(9):872. doi: 10.1007/BF03012978. [DOI] [PubMed] [Google Scholar]
- 13.Ready LB. Postoperative pain management–beyond basics. Can J Anaesth. 1996;43(2):193. doi: 10.1007/BF03011264. [DOI] [PubMed] [Google Scholar]
- 14.Jamison RN, Taft K, O'Hara JP, et al. Psychosocial and pharmacologic predictors of satisfaction with intravenous patient-controlled analgesia. Anesth Analg. 1993;77(1):121. [PubMed] [Google Scholar]
- 15.Lee A, Tsang CK, Siu HK, et al. Management of osteoarthritic pain in Hong Kong. Aust Fam Physician. 2008;37(10):874. [PubMed] [Google Scholar]
- 16.Chu LF, Clark DJ, Angst MS, et al. Opioid tolerance and hyperalgesia in chronic pain patients after one month of oral morphine therapy: a preliminary prospective study. J Pain. 2006;7(1):43. doi: 10.1016/j.jpain.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 17.Pereira J, Lawlor P, Vigano A, et al. Equianalgesic dose ratios for opioids. a critical review and proposals for long-term dosing. J Pain Symptom Manage. 2001;22(2):672. doi: 10.1016/S0885-3924(01)00294-9. [DOI] [PubMed] [Google Scholar]
- 18.Principles of analgesic use in the treatment of acute pain and cancer pain. Glenview: American Pain Society; 2003. p. 74. [Google Scholar]
- 19.Chou R, Fanciullo GJ, Fine PG, et al. American Pain Society-American Academy of Pain Medicine Opioids Guidelines P. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):113. doi: 10.1016/j.jpain.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 20.Pergolizzi J, Boger RH, Budd K, et al. Opioids and the management of chronic severe pain in the elderly: consensus statement of an International Expert Panel with focus on the six clinically most often used World Health Organization Step III opioids (buprenorphine, fentanyl, hydromorphone, methadone, morphine, oxycodone) Pain Pract. 2008;8(4):287. doi: 10.1111/j.1533-2500.2008.00204.x. [DOI] [PubMed] [Google Scholar]
- 21.Amstutz HC, Thomas BJ, Jinnah R, et al. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66(2):228. [PubMed] [Google Scholar]
- 22.Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Rel Res. 1986;213:20. [PubMed] [Google Scholar]
- 23.Carragee EJ, Alamin TF, Miller JL, et al. MRI and psychosocial determinants of low back pain disability and remission: a prospective study in subjects with benign persistent back pain. Spine J. 2005;5(1):24. doi: 10.1016/j.spinee.2004.05.250. [DOI] [PubMed] [Google Scholar]
- 24.Buer N, Linton SJ. Fear-avoidance beliefs and catastrophizing: occurrence and risk factor in back pain and ADL in the general population. Pain. 2002;99(3):485. doi: 10.1016/S0304-3959(02)00265-8. [DOI] [PubMed] [Google Scholar]
- 25.IJzelenberg W, Burdorf A. Risk factors for musculoskeletal symptoms and ensuing health care use and sick leave. Spine (Phila Pa 1976) 2005;30(13):1550. doi: 10.1097/01.brs.0000167533.83154.28. [DOI] [PubMed] [Google Scholar]
- 26.Singh JA, Lewallen D. Age, gender, obesity, and depression are associated with patient-related pain and function outcome after revision total hip arthroplasty. Clin Rheumatol. 2009;28(12):1419. doi: 10.1007/s10067-009-1267-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jordan JM, Linder GF, Renner JB, et al. The impact of arthritis in rural populations. Arthritis Care Res. 1995;8(4):242. doi: 10.1002/art.1790080407. [DOI] [PubMed] [Google Scholar]
- 28.Franklin PD, Karbassi JA, Li W, et al. Reduction in narcotic use after primary total knee arthroplasty and association with patient pain relief and satisfaction. J Arthroplasty. 2010;25(6 Suppl):12. doi: 10.1016/j.arth.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 29.Post ZD, Restrepo C, Kahl LK, et al. A prospective evaluation of 2 different pain management protocols for total hip arthroplasty. J Arthroplasty. 2010;25(3):410. doi: 10.1016/j.arth.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 30.Busch CA, Whitehouse MR, Shore BJ, et al. The efficacy of periarticular multimodal drug infiltration in total hip arthroplasty. Clin Orthop Rel Res. 2010;468(8):2152. doi: 10.1007/s11999-009-1198-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kahl L, Parvizi J, Viscusi ER, et al. Lessons learned with extended-release epidural morphine after total hip arthroplasty. Clin Orthop Rel Res. 2010;468(4):1082. doi: 10.1007/s11999-009-1181-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Frassanito L, Rodola F, Concina G, et al. The efficacy of the psoas compartment block versus the intrathecal combination of morphine, fentanyl and bupivacaine for postoperative analgesia after primary hip arthroplasty: a randomized single-blinded study. Eur Rev Med Pharmacol Sci. 2008;12(2):117. [PubMed] [Google Scholar]
- 33.Kidner CL, Mayer TG, Gatchel RJ, et al. Higher opioid doses predict poorer functional outcome in patients with chronic disabling occupational musculoskeletal disorders. J Bone Joint Surg Am. 2009;91(4):919. doi: 10.2106/JBJS.H.00286. [DOI] [PMC free article] [PubMed] [Google Scholar]