Abstract
Purpose
A few studies focused on the methods of treatment for displaced distal tibial shaft fractures have been published, all of which compared two different methods. In this randomized, prospective study, we aimed to compare minimally invasive plate osteosynthesis, locking intramedullary nail stabilization and external fixation combined with limited open reduction and absorbable internal fixation for distal tibial shaft fractures by assessing complications and secondary procedures.
Methods
From November 2002 to June 2012, 137 skeletally mature patients with displaced distal tibial shaft fractures with or without fibula fracture were randomized to be treated by minimally invasive plate osteosynthesis (group A, n = 46), locking intramedullary nail (group B, n = 46) or external fixation combined with limited open reduction and absorbable internal fixation (group C, n = 45). Age, gender, mechanism of injury, fracture pattern and presence of open fracture were equally distributed among the three groups. Indexes for evaluation included hospital stay, operative time, time to radiographic union, union status, infection and the incidence of re-operation. Mazur ankle score was introduced for functional evaluation. Statistics Analysis System (SAS) 9.2 was used for analysis.
Results
A total of 121 patients were included in the final analysis (group A 42, group B 40 and group C 39) and evaluated after a mean of 14.8 months follow-up. There was no significant difference (P > 0.05) in hospital stay, time to radiographic union and the incidence of union status among the three groups. Although group C was associated with less secondary procedures versus groups A and B, it was related with more pin tract infections (15.4 %). Anterior knee pain occurred frequently after locking intramedullary nailing (37.5 %) and the irritation symptoms were more frequently encountered in group A (59.5 %). There was no difference in ankle function between the three methods after operation (P > 0.05).
Conclusions
We consider that the minimally invasive plate osteosynthesis, locking intramedullary nail stabilization and external fixation combined with limited open reduction and absorbable internal fixation techniques are all efficient methods for treating distal tibia fractures. With its wide indications, external fixation combined with limited open reduction and absorbable internal fixation leads to minimal soft tissue complication, good functional result and no local soft tissue irritation or implant removal.
Keywords: Tibial shaft fracture, Minimally invasive plate osteosynthesis, Intramedullary nail, External fixation, Absorbable internal fixation
Introduction
In the past few years, several studies focussing on the methods of treatment for displaced distal tibial shaft fractures have been published [1–7]. Plates, intramedullary nails and external fixations are three well-accepted and effective methods, but each has been historically related to complications. Infections, wound complications and implant prominence are frequently reported after tibial plating [1, 2, 8–10], whereas malalignment and knee pain have been associated with nailing in other studies [11–15]. Frequent need for secondary operations, prolonged healing time and pin tract infection are inherent problems in external fixation [16, 17].
Although previous studies have compared plates with intramedullary nails [1–5, 10], plates with external fixation [7] and intramedullary nails with external fixation [6], few data are available on the three methods above. The minimally invasive plate osteosynthesis (MIPO) technique has gained prevalence in recent years. This percutaneous plating technique uses indirect reduction methods and allows stabilisation of distal tibial fractures while preserving the vascularity of the soft tissue envelope. As a result, the MIPO technique has gradually become the preferred option for some surgeons [8, 18–20]. Because of frequent need for secondary operations by traditional treatment with external fixation, we used an external fixator combined with limited open reduction and absorbable internal fixation to treat these patients.
The purpose of this study was to compare minimally invasive plate osteosynthesis, locking intramedullary nail stabilization and external fixation combined with limited open reduction and absorbable internal fixation for distal tibial shaft fractures by assessing complications and secondary procedures. We postulated that external fixation combined with limited open reduction and absorbable internal fixation leads to less secondary operations, the same functional outcome, and no increase in complications versus minimally invasive plate osteosynthesis and locking intramedullary nail stabilization.
Patients and methods
The criteria for inclusion of the study were being aged at least 18 years and having a closed or grade I–II open fracture of the distal third of the tibial diaphysis. Exclusion criteria were associated proximal intra-articular or distal intra-articular fractures of the tibia, tibia plafond fractures, fractures associated with vascular injury requiring repair, and suspected pathologic fractures. The location and AO classification of the fractures were determined by radiographs.
From November 2002 to June 2012, 137 skeletally mature patients with displaced distal tibia shaft fractures (Orthopaedic Trauma Association 42)[21] with or without fibula fracture were treated with minimally invasive plate osteosynthesis (group A, n = 46), locking intramedullary nail (group B, n = 46) or external fixation combined with limited open reduction and absorbable internal fixation (group C, n = 45) by fellowship-trained traumatologists at the department of Orthopaedic Trauma Surgery of Changzheng Hospital, Shanghai, according to inclusion criteria and exclusion criteria. Ethical approval was obtained (ethical committee, the Second Military Medical University). Type of treatment was randomized by computer allocation and assigned to patients prospectively through sequentially numbered opaque envelopes. All fractures were extra-articular distal diaphyseal fractures, which were located between 4 cm and 11 cm from the tibial plafond. Demographic information is reported in Table 1. Age, gender, mechanism of injury, fracture pattern and presence of open fracture were equally distributed among the three groups by computer randomization. The mean age was 43 (range 18–79) years in group A, 44 (range 18–78) years in group B and 43 (range 20–82) in group C. All operations were performed under spinal anaesthesia by orthopaedic surgeons of the same surgical team.
Table 1.
Demographic information
| Group | Patients, n | Males, n | Mean age, years | Open fractures | Closed fractures | Mechanism of injury | OTA classification | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Traffic injuries | Fall | Crush | Others | 42-A | 42-B | 42-C | ||||||
| A | 46 | 38 | 43 | 14 | 32 | 24 | 10 | 6 | 6 | 37 | 7 | 2 |
| B | 46 | 41 | 44 | 17 | 29 | 22 | 11 | 9 | 4 | 33 | 8 | 5 |
| C | 45 | 37 | 43 | 13 | 32 | 22 | 10 | 5 | 8 | 34 | 7 | 4 |
OTA Orthopaedic Trauma Association
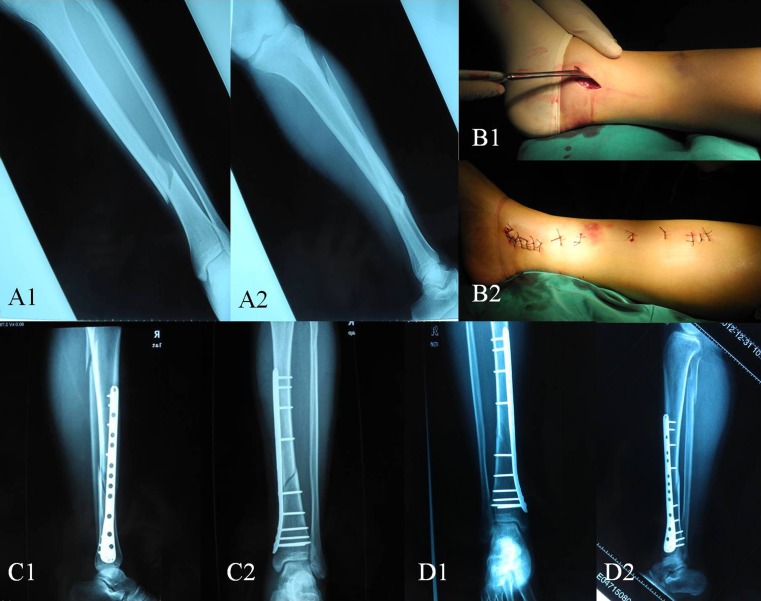
Tibial plating was performed with minimally invasive plate osteosynthesis. An anterior-medial curved incision (about 3–6 cm) was made for exposing and protecting the saphenous vein. After closed reduction, the premoulded plate is inserted upward from the distal end without periosteal resection. Next, a proximal incision about three holes long is made to expose the upper part of the plate and the plate position is adjusted as needed. Intra-operative use of the image intensifier helps to accomplish closed reduction. The anterior-posterior and lateral views should both be checked and rotary restoration should be confirmed. Care should be taken with fibula reduction as it plays an important role in the restoration of rotational alignment. Once functional reduction is accomplished, the locking screws are driven in (Fig. 1).
Fig. 1.
a1-a2 Plain radiographic anteroposterior and lateral views of a distal tibial shaft fracture. b1-b2 Minimally invasive surgery incision. c1-c2 Plain radiographic anteroposterior and lateral views two days after operation. d1-d2 Plain radiographic anteroposterior and lateral views 12 months after operation
We used reamed nail and static locking in all fractures treated by locking intramedullary nail. The patients were positioned supine on the traction table with calcaneal pin traction and 90° of flexion of the knee joint. Access to the proximal tibia was provided by a transtendinous approach. All surgeons adhered to the same protocol. First, the surgeon reamed the intramedullary canal until the first detection of “cortical chatter”, forming the basis for the nail diameter. Following the appearance of “cortical chatter”, the surgeon reamed 1–1.5 mm larger than the chosen nail’s diameter. This study required interlocking of all nails, both proximally and distally, as well as the use of at least one proximal locking screw and one distal locking screw (Fig. 2).
Fig. 2.
a1-a2 Plain radiographic anteroposterior and lateral views of a distal tibial shaft fracture. b Plain radiographic anteroposterior and lateral views two days after operation. c1-c2 Plain radiographic anteroposterior and lateral views 24 months after operation
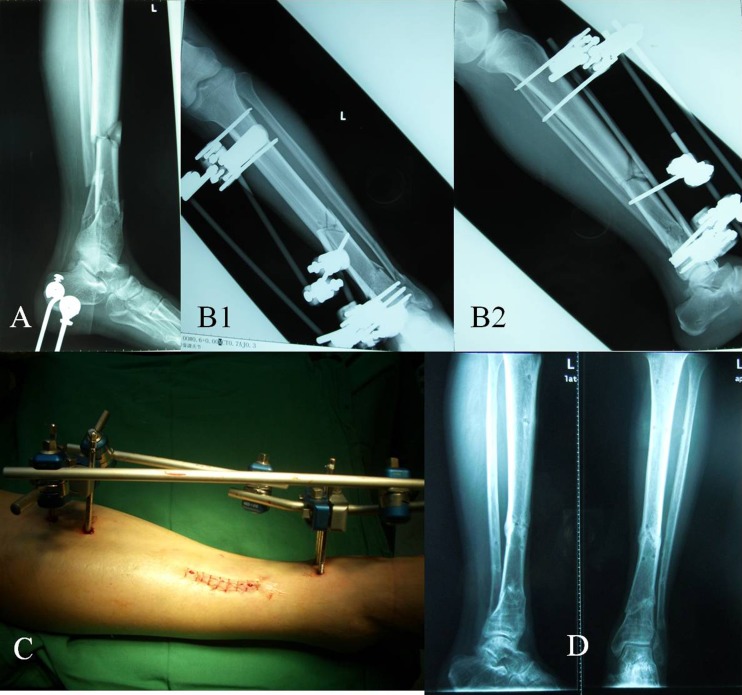
External fixation combined with limited open reduction and absorbable internal fixation was conducted in group C. An incision about 3–4 cm was made for cleaning soft tissue and blood clots embedded in the fracture site under direct vision. Any anteroposterior or medial-lateral displacement was reduced and provisionally stabilized by large AO reduction clamps and K-wires. The fractures were fixed with absorbable screws of 3.5-, 4.5-, or 5.5-mm diameter or absorbable rods of 2.4- or 3.0-mm diameter (poly-d,l-lactic acid, DIKFIX, Dikang, Inc, Chengdu, China), depending on the size of the fracture. Last, we fixed pins paralled in the proximal and distal fracture throughout the tibia bone diaphysis and connected them with a unilateral external fixator (Hoffmann II, Stryker, Inc, Kalamazoo, MI) adjusted and fastened (Fig. 3).
Fig. 3.
a Plain radiographic lateral view of a distal tibial shaft fracture. b1-b2 Plain radiographic anteroposterior and lateral views two days after operation. c Limited incision in operation. d Plain radiographic anteroposterior and lateral views 12 months after operation
Intravenous antibiotics consisting of a first-generation cephalosporin or alternative were administered pre-operatively and for 24 hours postoperatively. We encouraged patients to try early movement of knee and ankle joints and muscular exercises in each group. Total weight-bearing was not recommended for eight to 12 weeks postoperatively for all groups. The progression of weight-bearing was determined by the surgeon cautiously, based on the fracture configuration, soft tissue injury and patient comorbidities. Weight-bearing was usually advanced before fractures were completely radiographically united. Patients were followed up for a minimum of 12 months postoperatively.
Data were obtained during clinical and radiographic examinations postoperatively at two, six, 12, 26 and 52 weeks. If the fracture didn’t heal at 12 weeks, additional radiographs were often necessary between 12 and 26 weeks. Fracture healing was assessed by standard radiographic projections, and union was defined as dense callus bridging at least three of four cortices on biplanar radiographs. Delayed union was defined as radiographic union after >12 weeks. Nonunion was defined as lack of any healing within six months. Malunion was defined as angular deformity of greater than 5°, translation or shortening greater than 1 cm, or rotational malalignment of greater than or equal to 15°. Angular deformity, translation and shortening were assessed from the radiographs. Rotational deformities were judged clinically by the thigh foot angle. Range of movement of the knee and ankle were measured. Anterior knee pain, fracture site pain and ankle pain were noted. Ankle function was measured using Mazur ankle score [22]. The maximum score was 100 points. A value of more than 92 points was considered an excellent result, 82–92 good, 65–86 fair, and <65 was considered poor.
All of the data analyses were performed using the SAS software package (version 9.2; SAS Institute) at Second Military Medical University (Shanghai, China). Continuous variables during the study period are presented as mean ± SD and differences in continuous variables among (between) groups were examined using analysis of variance (ANOVA) and/or Wilcoxon rank–sum test. Frequency distributions for category variables and excellent and/or good rate were compared among (between) groups using the chi-squared analysis and/or Fisher’s exact test. Significance was set at P < 0.05 unless otherwise indicated.
Results
A total of 137 patients were prospectively randomized to group A, group B or group C for their tibia fractures. Fifteen patients were lost to follow-up due to moving, death and other reasons. At last, 121 patients were included in the final analysis of complications (group A 42, group B 40 and group C 39) and were evaluated after a mean of 14.8 months follow-up.
The results are presented in Table 2. The group treated with MIPO was assessed at a mean time of 15.2 months (range 13–18 months), intramedullary nail of 14.6 months (range 13–17 months) and external fixation combined with limited open reduction and absorbable internal fixation of 14.6 months (range 12–17 months). Patients stayed in the hospital for an average of 10.5 days (mean: group A 10.2 days [range four to15], group B 9.8 days [range four to 20] and group C 11.2 days [range six to 19]). Operative management of a distal tibial fracture with MIPO took a mean total operation time (inclusive anaesthesia) of 114.4 minutes (range 65–186), operative management with intramedullary nail took a mean time of 87.5 minutes (range 70–190) and external fixation combined with limited open reduction and absorbable internal fixation of 85.8 minutes (range 65–178). There was a significant different between the three groups for operation time.
Table 2.
Comparison of statistic data for major results after operation in the three groups
| Group | Patients, n | Hospital stay, days | Operation time, mins | Time to radiographic union, weeks | Union status, n | Infection, n | Incidence of reoperation | Ankle function (excellent or good rates) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Delayed union | Malunion | Nonunion | Soft tissue infection | Deep infection | Pin tract infection | |||||||
| A | 42 | 10.2 ± 3.3 | 114.4 ± 26.1 | 15 ± 3.4 | 4 | 3 | 1 | 7 | 1 | 0 | 0.52 (22/42) | 0.90 (38/42) |
| B | 40 | 9.8 ± 2.7 | 87.5 ± 22.7a | 15.6 ± 3.2 | 5 | 4 | 1 | 1a | 2 | 0 | 0.63 (25/40) | 0.87 (35/40) |
| C | 39 | 11.2 ± 3.1 | 85.8 ± 21.3a | 15.2 ± 3.5 | 3 | 1 | 0 | 2 | 0 | 6a,b | 0.08 (3/39)a,b | 0.92 (35/39) |
| P value | - | >0.05 | <0.05 | >0.05 | >0.05 | >0.05 | >0.05 | <0.05 | >0.05 | <0.05 | <0.05 | >0.05 |
a P < 0.05 compared with group A
b P < 0.05 compared with group B
The mean time to radiographic union was 15 weeks (range 13–34 weeks) in group A versus 15.6 weeks (range 13–29 weeks) in group B and 15.2 weeks (range 14–36 weeks) in group C. Delayed union occurred in four patients (9.5 %) managed with MIPO, in five patients (12.5 %) who had an intramedullary nail and in three patients (7.7 %) who had external fixation combined with limited open reduction and absorbable internal fixation. Malunion and nonunion rates did not show significant differences between each group.
In the MIPO group, one case with deep infection and seven cases with soft tissue infection developed. Twenty-five cases (59.5 %) of soft tissue irritation symptoms occurred with slight influence on daily life and in another case a locking screw broke. Secondary operation was performed on 22 patients (52.4 %) to remove the plates. In the intramedullary nail group, two cases developed postoperative tibial osteomyelitis and one of them had nonunion, which resolved after secondary surgery. Six cases had local soft tissue irritation symptoms from the implants and 15 patients still felt knee pain one year later after the operation. Secondary operations were performed on 25 patients (62.5 %) to remove the intramedullary nail. In group C, no deep infection and nonunion developed, and three others received secondary operations for inflammatory foreign-body reaction. Among the 39 patients who received external fixation combined with limited open reduction and absorbable internal fixation, six patients (15.4 %) had pin tract infection. At one-year follow-up, there were no significant differences in ankle function.
Discussion
The optimal treatment of unstable distal tibia without articular involvement remains controversial, despite the variety of treatment options which have been suggested for these injuries, including nonoperative treatment, plate fixation, intramedullary nailing, and external fixation. However, each of these treatment options has certain defects. Nonoperative treatment can be applied to stable extra-articular fractures with minimal shortening which may be complicated by loss of reduction, subsequent malunion, motion restriction and osteoarthritis [23, 24]. Open reduction and internal fixation results in extensive soft tissue dissection and large periosteal elevation, which may be associated with wound complications and infections [3, 25, 26]. There is some concern about the use of intramedullary nails in distal tibia fractures because of technical difficulties with distal nail fixation, the risk of nail propagation into the ankle joint and the discrepancy between the diaphyseal and metaphyseal diameter of the intramedullary canal. External fixation of distal tibia fractures may result in insufficient reduction, malunion and pin tract infection [27, 28].
In recent years, numerous reports have shown that the MIPO technique is a safe and worthwhile method of managing such fractures, whilst avoiding some of the complications associated with conventional open plating methods. The aim of MIPO is to preserve the osteogenic haematoma of the fracture and the nutritional arteries of the bone while preventing iatrogenic soft tissue damage [29]. Aksekili et al. [30], in a study treating 35 distal and diaphyseal tibial fractures with the MIPO technique, suggested that MIPO is an effective treatment for tibial diaphysis and distal tibia fractures with low complication and high union rates. High primary union rate (90.5 %) and only one patient with nonunion was observed in the MIPO group in our study, which is consistent with other studies [8, 30–32]. Although we found the irritation symptoms were more frequently encountered in the MIPO group, the symptoms had no effect on their daily life. Similar results were reported by Lau et al. whereby 52 % (25/48) of distal tibia fracture cases treated by MIPO had the implants removed due to skin impingement [33]. This could be related to the thin subcutaneous tissue and suboptimal premoulding of plates. Furthermore, the residual malreduction also contributes to the inexactness of plate and bone contouring.
Infection rates vary between 0 % and 50 % following the surgical treatment of distal tibial fractures [10, 15, 25, 34]. The highest infection rate is seen in patients treated with open reduction and internal fixation. MIPO, intramedullary nail and external fixation lead to a serious decrease in the infection rates [5, 6, 15, 31, 35, 36]. Results from this present study show that deep infection does not have a significant difference between the three groups. A higher soft tissue infection rate has been seen in patients treated with minimally invasive plate osteosynthesis, which may be explained by the extended operation time. Moreover, pin tract infection is an inherent problem in external fixation [6, 35]. Our results are in line with previous reports, and pin tract infection occurred frequently in the external fixation combined with limited open reduction and absorbable internal fixation group. No patients showed signs of persistent pin tract infection after six months or one year.
We observed a high frequency of anterior knee pain after intramedullary nailing, which is consistent with early studies [6, 14, 37]. A tendon-splitting approach was used in our study. Keating et al. [37] reported reduced pain problems using a paratendinous approach, whereas Toivanen et al. [13], in a prospective, randomised study failed to detect any differences between the two methods. A percutaneous approach aiming to avoid prepatellar scarring and injury to the infrapatellar nerve was described by Karladani and Styf [38], but any benefit from this method has not been demonstrated so far in any prospective randomised study. According to Keating et al. [37], the aetiology for anterior knee pain after intramedullary nailing is multifactorial, and proximal nail protrusion was not found to be an important factor. Nail removal will, however, relieve symptoms in many cases [14, 37], as the patients who had been re-operated in our study.
External fixation was another traditional treatment for distal tibial fracture, which may lead to lots of postoperative complications, such as prolonged healing time, malunion, nonunion, frequent need for secondary operation and pin tract infection[16, 17]. Although a circular external fixator is biomechanically more rigid than a unilateral external fixator, pin site infection is one of the major drawbacks of the circular external fixation technique [39]. In our study, pin tract infection remained the most common complication, with an incidence of 15.4 %, which is much less than that for circular external fixators reported in the literature [39], and no case of deep infection occurred in our patients.
Use of an external fixator can decrease soft tissue necrosis and deep infection rate, but when used as a definite fixation device, even a circular external fixator has a relatively high rate of malunion because of insufficient rigidity. It was reported that malunion developed in 25.6 % of tibial shaft fractures treated by indirect reduction by stabilization with an external fixator [6]. Therefore, an open reduction under direct vision and internal fixation of the tibial shaft fracture fragments is necessary. If an implant is bulky, it may need an extended incision and extensive stripping of soft tissue such that wound healing may be compromised. Soft tissue complications have always been a concern. In addition, the implant has to be removed surgically in some symptomatic patients. In our practice, most patients want the metallic implants removed following fracture healing, which increases treatment costs, may be challenging, and can lead to complications [40]. For these reasons, we used absorbable screws and rods as devices for limited internal fixation. The biggest advantage of absorbable material is that it does not require implant removal [41]. We have conducted a study to evaluate the clinical outcome of the treatment of type C pilon fractures by using an external fixator combined with limited open reduction and absorbable internal fixation and found that this was a reliable treatment for closed and open AO/OTA type C pilon fractures of the distal tibia[42]. The external fixator combined with limited open reduction and absorbable internal fixation used in our study also leads to excellent results.
The limitations of the present study are that: (1) the sample size was small, and (2) the average follow-up was only 14.8 months, which is a relatively short evaluation period and thus most cases of posttraumatic arthritis would not have developed yet. A larger sample size and longer follow-up would be helpful in a future study.
Finally, we consider that the minimally invasive plate osteosynthesis, locking intramedullary nail stabilization and external fixation combined with limited open reduction and absorbable internal fixation techniques are all efficient methods for treating distal tibia fractures. With its wide indications, external fixation combined with limited open reduction and absorbable internal fixation leads to minimal soft tissue complication, good functional result and no local soft tissue irritation or implant removal.
Footnotes
Yongchuan Li, Xi Jiang and Qinghe Guo contributed equally to this work.
References
- 1.Im GI, Tae SK. Distal metaphyseal fractures of tibia: a prospective randomized trial of closed reduction and intramedullary nail versus open reduction and plate and screws fixation. J Trauma. 2005;59:1219–1223. doi: 10.1097/01.ta.0000188936.79798.4e. [DOI] [PubMed] [Google Scholar]
- 2.Janssen KW, Biert J, van Kampen A. Treatment of distal tibial fractures: plate versus nail: a retrospective outcome analysis of matched pairs of patients. Int Orthop. 2007;31:709–714. doi: 10.1007/s00264-006-0237-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vallier HA, Le TT, Bedi A. Radiographic and clinical comparisons of distal tibia shaft fractures (4 to 11 cm proximal to the plafond): plating versus intramedullary nailing. J Orthop Trauma. 2008;22:307–311. doi: 10.1097/BOT.0b013e31816ed974. [DOI] [PubMed] [Google Scholar]
- 4.Yang SW, Tzeng HM, Chou YJ, Teng HP, Liu HH, Wong CY. Treatment of distal tibial metaphyseal fractures: Plating versus shortened intramedullary nailing. Injury. 2006;37:531–535. doi: 10.1016/j.injury.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 5.Vallier HA, Cureton BA, Patterson BM. Randomized, prospective comparison of plate versus intramedullary nail fixation for distal tibia shaft fractures. J Orthop Trauma. 2011;25:736–741. doi: 10.1097/BOT.0b013e318213f709. [DOI] [PubMed] [Google Scholar]
- 6.Braten M, Helland P, Grontvedt T, Aamodt A, Benum P, Molster A. External fixation versus locked intramedullary nailing in tibial shaft fractures: a prospective, randomised study of 78 patients. Arch Orthop Trauma Surg. 2005;125:21–26. doi: 10.1007/s00402-004-0768-0. [DOI] [PubMed] [Google Scholar]
- 7.Bach AW, Hansen ST Jr (1989) Plates versus external fixation in severe open tibial shaft fractures. A randomized trial. Clin Orthop Relat Res 241:89–94 [PubMed]
- 8.Borg T, Larsson S, Lindsjo U. Percutaneous plating of distal tibial fractures. Preliminary results in 21 patients. Injury. 2004;35:608–614. doi: 10.1016/j.injury.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 9.Joveniaux P, Ohl X, Harisboure A, Berrichi A, Labatut L, Simon P, Mainard D, Vix N, Dehoux E. Distal tibia fractures: management and complications of 101 cases. Int Orthop. 2010;34:583–588. doi: 10.1007/s00264-009-0832-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li Y, Liu L, Tang X, Pei F, Wang G, Fang Y, Zhang H, Crook N. Comparison of low, multidirectional locked nailing and plating in the treatment of distal tibial metadiaphyseal fractures. Int Orthop. 2012;36:1457–1462. doi: 10.1007/s00264-012-1494-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Larsen LB, Madsen JE, Hoiness PR, Ovre S. Should insertion of intramedullary nails for tibial fractures be with or without reaming? A prospective, randomized study with 3.8 years' follow-up. J Orthop Trauma. 2004;18:144–149. doi: 10.1097/00005131-200403000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Obremskey WT, Medina M. Comparison of intramedullary nailing of distal third tibial shaft fractures: before and after traumatologists. Orthopedics. 2004;27:1180–1184. doi: 10.3928/0147-7447-20041101-15. [DOI] [PubMed] [Google Scholar]
- 13.Toivanen JA, Vaisto O, Kannus P, Latvala K, Honkonen SE, Jarvinen MJ. Anterior knee pain after intramedullary nailing of fractures of the tibial shaft. A prospective, randomized study comparing two different nail-insertion techniques. J Bone Joint Surg Am. 2002;84-A:580–585. doi: 10.2106/00004623-200204000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Court-Brown CM, Gustilo T, Shaw AD. Knee pain after intramedullary tibial nailing: its incidence, etiology, and outcome. J Orthop Trauma. 1997;11:103–105. doi: 10.1097/00005131-199702000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Salem KH. Unreamed intramedullary nailing in distal tibial fractures. Int Orthop. 2013;37:2009–2015. doi: 10.1007/s00264-013-1998-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Emami A, Mjoberg B, Karlstrom G, Larsson S. Treatment of closed tibial shaft fractures with unilateral external fixation. Injury. 1995;26:299–303. doi: 10.1016/0020-1383(95)00037-A. [DOI] [PubMed] [Google Scholar]
- 17.Helland P, Boe A, Molster AO, Solheim E, Hordvik M (1996) Open tibial fractures treated with the Ex-fi-re external fixation system. Clin Orthop Relat Res 326:209–220 [DOI] [PubMed]
- 18.Maffulli N, Toms AD, McMurtie A, Oliva F. Percutaneous plating of distal tibial fractures. Int Orthop. 2004;28:159–162. doi: 10.1007/s00264-004-0541-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Collinge C, Protzman R. Outcomes of minimally invasive plate osteosynthesis for metaphyseal distal tibia fractures. J Orthop Trauma. 2010;24:24–29. doi: 10.1097/BOT.0b013e3181ac3426. [DOI] [PubMed] [Google Scholar]
- 20.Hazarika S, Chakravarthy J, Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia–results in 20 patients. Injury. 2006;37:877–887. doi: 10.1016/j.injury.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 21.(1996) Fracture and dislocation compendium. Orthopaedic Trauma Association Committee for Coding and Classification. J Orthop Trauma 10 Suppl 1:v-ix, 1–154 [PubMed]
- 22.Kopp FJ, Banks MA, Marcus RE. Clinical outcome of tibiotalar arthrodesis utilizing the chevron technique. Foot Ankle Int. 2004;25:225–230. doi: 10.1177/107110070402500406. [DOI] [PubMed] [Google Scholar]
- 23.Othman M, Strzelczyk P. Results of conservative treatment of "pilon" fractures. Ortop Traumatol Rehabil. 2003;5:787–794. [PubMed] [Google Scholar]
- 24.Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg (Br) 2002;84:1093–1110. doi: 10.1302/0301-620X.84B8.13752. [DOI] [PubMed] [Google Scholar]
- 25.Frigg R. Locking Compression Plate (LCP). An osteosynthesis plate based on the Dynamic Compression Plate and the Point Contact Fixator (PC-Fix) Injury. 2001;32(Suppl 2):63–66. doi: 10.1016/S0020-1383(01)00127-9. [DOI] [PubMed] [Google Scholar]
- 26.Drosos G, Karnezis IA, Bishay M, Miles AW. Initial rotational stability of distal tibial fractures nailed without proximal locking: the importance of fracture type and degree of cortical contact. Injury. 2001;32:137–143. doi: 10.1016/S0020-1383(00)00157-1. [DOI] [PubMed] [Google Scholar]
- 27.Sarmiento A, Latta LL (2004) 450 closed fractures of the distal third of the tibia treated with a functional brace. Clin Orthop Relat Res 428:261–271 [DOI] [PubMed]
- 28.Bahari S, Lenehan B, Khan H, McElwain JP. Minimally invasive percutaneous plate fixation of distal tibia fractures. Acta Orthop Belg. 2007;73:635–640. [PubMed] [Google Scholar]
- 29.Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis and vascularity: preliminary results of a cadaver injection study. Injury. 1997;28(Suppl 1):A7–A12. doi: 10.1016/S0020-1383(97)90110-8. [DOI] [PubMed] [Google Scholar]
- 30.Aksekili MA, Celik I, Arslan AK, Kalkan T, Ugurlu M. The results of minimally invasive percutaneous plate osteosynthesis (MIPPO) in distal and diaphyseal tibial fractures. Acta Orthop Traumatol Turc. 2012;46:161–167. doi: 10.3944/AOTT.2012.2597. [DOI] [PubMed] [Google Scholar]
- 31.Cheng W, Li Y, Manyi W. Comparison study of two surgical options for distal tibia fracture-minimally invasive plate osteosynthesis vs. open reduction and internal fixation. Int Orthop. 2011;35:737–742. doi: 10.1007/s00264-010-1052-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury. 2007;38:365–370. doi: 10.1016/j.injury.2006.10.024. [DOI] [PubMed] [Google Scholar]
- 33.Lau TW, Leung F, Chan CF, Chow SP. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int Orthop. 2008;32:697–703. doi: 10.1007/s00264-007-0384-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Blauth M, Bastian L, Krettek C, Knop C, Evans S. Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. J Orthop Trauma. 2001;15:153–160. doi: 10.1097/00005131-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Leung F, Kwok HY, Pun TS, Chow SP. Limited open reduction and Ilizarov external fixation in the treatment of distal tibial fractures. Injury. 2004;35:278–283. doi: 10.1016/S0020-1383(03)00172-4. [DOI] [PubMed] [Google Scholar]
- 36.Zou J, Shi ZM, Zhang W, Zhang CQ. Open reduction and internal fixation better than percutaneous plate osteosynthesis in distal tibial fractures. J Invest Surg. 2012;25:326–329. doi: 10.3109/08941939.2011.648048. [DOI] [PubMed] [Google Scholar]
- 37.Keating JF, Orfaly R, O'Brien PJ. Knee pain after tibial nailing. J Orthop Trauma. 1997;11:10–13. doi: 10.1097/00005131-199701000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Karladani AH, Styf J. Percutaneous intramedullary nailing of tibial shaft fractures: a new approach for prevention of anterior knee pain. Injury. 2001;32:736–739. doi: 10.1016/S0020-1383(01)00038-9. [DOI] [PubMed] [Google Scholar]
- 39.Cavusoglu AT, Er MS, Inal S, Ozsoy MH, Dincel VE, Sakaogullari A. Pin site care during circular external fixation using two different protocols. J Orthop Trauma. 2009;23:724–730. doi: 10.1097/BOT.0b013e3181abbc31. [DOI] [PubMed] [Google Scholar]
- 40.Busam ML, Esther RJ, Obremskey WT. Hardware removal: indications and expectations. J Am Acad Orthop Surg. 2006;14:113–120. doi: 10.5435/00124635-200602000-00006. [DOI] [PubMed] [Google Scholar]
- 41.Podeszwa DA, Wilson PL, Holland AR, Copley LA. Comparison of bioabsorbable versus metallic implant fixation for physeal and epiphyseal fractures of the distal tibia. J Pediatr Orthop. 2008;28:859–863. doi: 10.1097/BPO.0b013e31818e19d7. [DOI] [PubMed] [Google Scholar]
- 42.Zhao L, Li Y, Chen A, Zhang Z, Xi J, Yang D. Treatment of type C pilon fractures by external fixator combined with limited open reduction and absorbable internal fixation. Foot Ankle Int. 2013;34:534–542. doi: 10.1177/1071100713480344. [DOI] [PubMed] [Google Scholar]