Abstract
Purpose
The objective of this study was to compare the safety and efficacy of minimally invasive discectomy (MID) with standard discectomy (SD) and determine whether the use of the MID technique could decrease the recurrence of lumbar disc herniation (LDH) after the surgery.
Methods
In February 2014, a comprehensive search was performed in PubMed, EMBASE, Web of Science, Cochrane Library and the Chinese Biological Medicine Database. Only randomised controlled trials (RCT) that compared MID with SD for the surgical management of LDH were included. These trials were carefully picked out following the inclusion and exclusion criteria. Using the Cochrane Collaboration guidelines, two authors independently extracted data and assessed these trials’ quality. The age of the patients, size of incision, surgical time, blood loss, visual analogue scale (VAS) score after the surgery, hospital stay, disc herniation recurrence, X-ray exposure and surgical costs in these studies were abstracted and synthesised by a meta-analysis with RevMan 5.2.0 software, and the main results (VAS score after the surgery and disc herniation recurrence) of publication bias were examined by Stata 12.0.
Results
Overall, 16 trials involving 2,139 patients meeting our criteria were included and analysed. Comparing MID and SD, the former was more likely to increase disc herniation recurrence [relative risk (RR) = 1.95, 95 % confidence interval (CI) 1.19–3.19, p = 0.008], and it involved a smaller size of incision [mean difference (MD) = −1.91, 95 % CI −3.33 to −0.50, p = 0.008], shorter hospital stay, longer operating time (MD = 11.03, 95 %C I 6.62–15.44, p < 0.00001) and less blood loss (MD = −13.56, 95 % CI −22.26 to −4.87, p = 0.002), while no statistical difference appeared with regard to the age of the patients, VAS score after the surgery, X-ray exposure, hospital stay and surgical costs.
Conclusions
Based on available evidence, MID results in less suffering for patients during the hospital course with a similar clinical efficacy compared to SD. This makes MID a promising procedure for patients with LDH; however, to popularise it greater effort is required to reduce disc herniation recurrence.
Keywords: Meta-analysis, Minimally invasive discectomy, Standard discectomy, Lumbar disc herniation, Randomised controlled trial, Surgical procedures
Introduction
Lumbar disc herniation (LDH) is generally thought to be the main cause of discogenic low back pain (LBP). It is reported that almost 60 %–80 % of people will suffer back pain during their lifetime [1]. According to the statistics from the World Health Organisation, LBP has become one of the most important causes of disability as expressed in disability-adjusted life years both in developed and developing countries [2].
There are as many as 80 %–90 % of patients who suffer from LDH who could have their symptoms relieved (such as LBP) by conservative treatment [3]. The main symptom of LDH is LBP and it is due to the existence of neural tissue around the intervertebral disc. The other chief complaint from patients with LDH after LBP is sciatica [4]; when these symptom occur and persist for six weeks after conservative therapy, discectomy should be regarded as a good treatment option for LDH.
There are two main methods for intervertebral disc surgery. One is standard open discectomy (OD) which involves partial laminectomy and partial removal of the disc, which was first reported by Mixter and Barr in 1934 [5]. From then on, standard OD became the standard method for LDH surgical treatment. The other is minimally invasive discectomy (MID) [such as percutaneous endoscopic lumbar discectomy (PELD) and microendoscopic discectomy (MED)], which was first introduced in 1977 by Yasargil and Caspar [6]. Compared with standard OD, MID enabled the use of smaller incisions of the skin and facilitated a less traumatic surgical procedure.
However, a recent large sample multicentre randomised controlled trial (RCT) reported that MID may result in more leg and back pain [7], and another RCT revealed that this procedure may bring about higher complications and surgical costs [8].
There are only a small number of RCT studies comparing MID and standard discectomy (SD), and no recent meta-analysis has been published on this subject. Therefore, before MID becomes more widely adopted, we should systematically evaluate MID’s recurrence risk and its safety and efficacy.
Materials and methods
Study inclusion and exclusion criteria
A comprehensive search was performed in PubMed, EMBASE, Web of Science, Cochrane Library and the Chinese Biological Medicine Database. Only RCT comparing MID and SD for the surgical management of patients with LDH were included.
Based on the predefined criteria, the following eligibility criteria were applied: all genders, age 18 or above, no spinal surgery before, a condition which had been diagnosed as single segmental intervertebral disc herniation based on physical examinations and imaging tests (computed tomography, magnetic resonance imaging and/or X-ray), and no response to conservative management for over six weeks. Exclusion criteria included non-RCT trials, cauda equina syndrome, neoplasm, spondylolisthesis, rheumatoid arthritis, degenerative spinal canal stenosis, re-operations and herniated disc involving more than one anatomical level. The publication language was confined to English and Chinese.
The MID group included these similar traits: use of microendoscopy, tissue retractors and specialised instruments that enabled surgeons to perform procedures through small incisions, such as PELD or MED etc., and the SD group involved traditional OD, partial laminectomy, hemilaminectomy and removal of the herniated disc by the standard procedure.
Search strategy for identification of studies
Relevant published papers of RCT in any language, up to 1 February 2014, were identified by the following search strategies: (1) computer-aided search in PubMed, EMBASE, Web of Science, Cochrane Library and the Chinese Biological Medicine Database; (2) manual search of Spine, European Spine Journal, Chinese Journal of Spine and meeting abstracts of most major spine societies from 1977; and (3) personal communications for unpublished literature such as conference papers.
Study quality
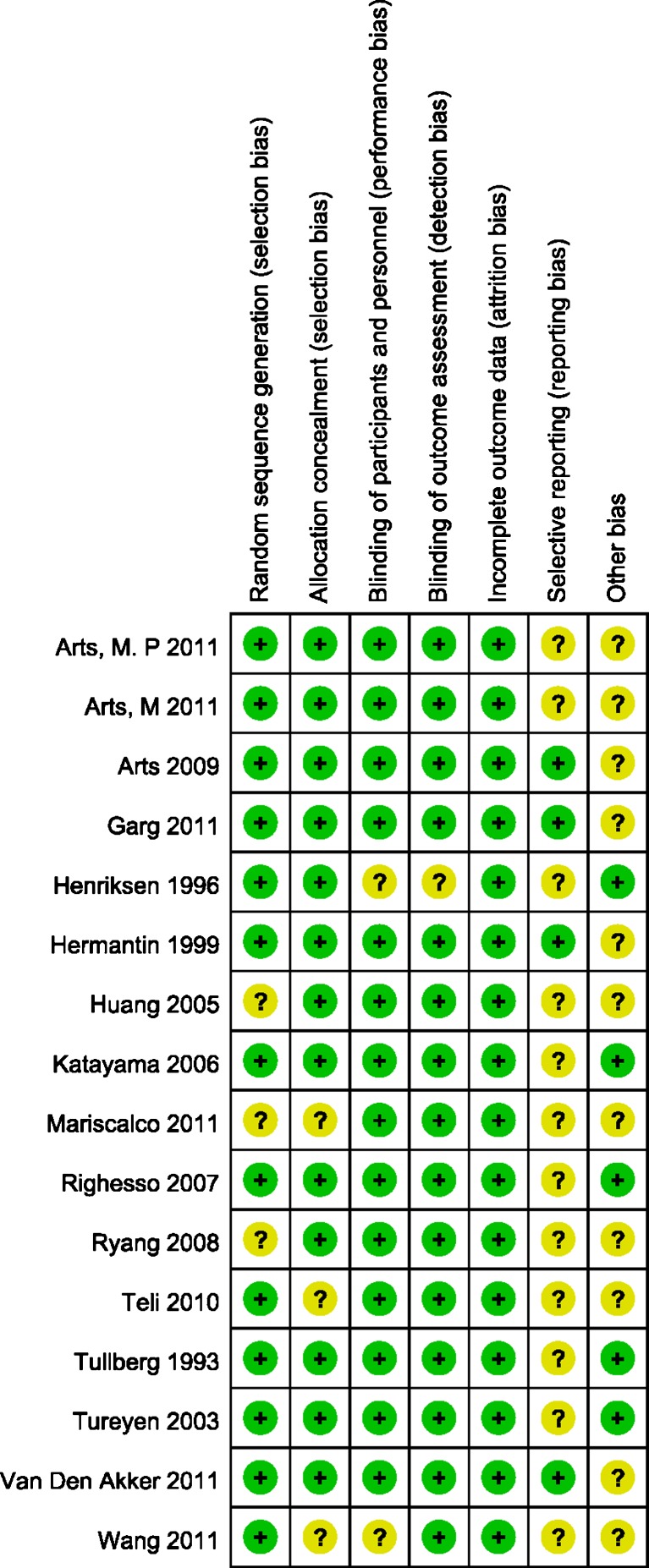
Two authors read the full articles and assessed these trials’ quality independently. Quality ratings were made according to the Cochrane Collaboration guidelines [9]: (1) random sequence generation (selection bias), (2) allocation concealment (selection bias), (3) blinding of participants and personnel (performance bias), (4) blinding of outcome assessment (detection bias), (5) incomplete outcome data (attrition bias), (6) selective reporting (reporting bias) and (7) other bias. All discrepancies were resolved by consensus.
Data extraction and meta-analysis
The data were extracted by two authors and then gathered and checked. The primary outcomes were the age of the patients, size of incision, surgical time, blood loss, visual analogue scale (VAS) score after the surgery, hospital stay, disc herniation recurrence, X-ray exposure and surgical costs. RevMan 5.2.0 was used for data analysis. Continuous outcome data were summarised by the mean difference (MD) and 95 % confidence intervals (CIs). Binary outcome data were summarised using relative risk (RR) and 95 % CIs. The level of significance was set at p < 0.05.
The χ2 test and I2 statistics were used to evaluate heterogeneity. Fixed effect models were applied when the statistical heterogeneity was not significant, or else the random effects model should be used. The main results of publication bias were examined by Stata 12.0 software [10].
Results
Search results and study quality
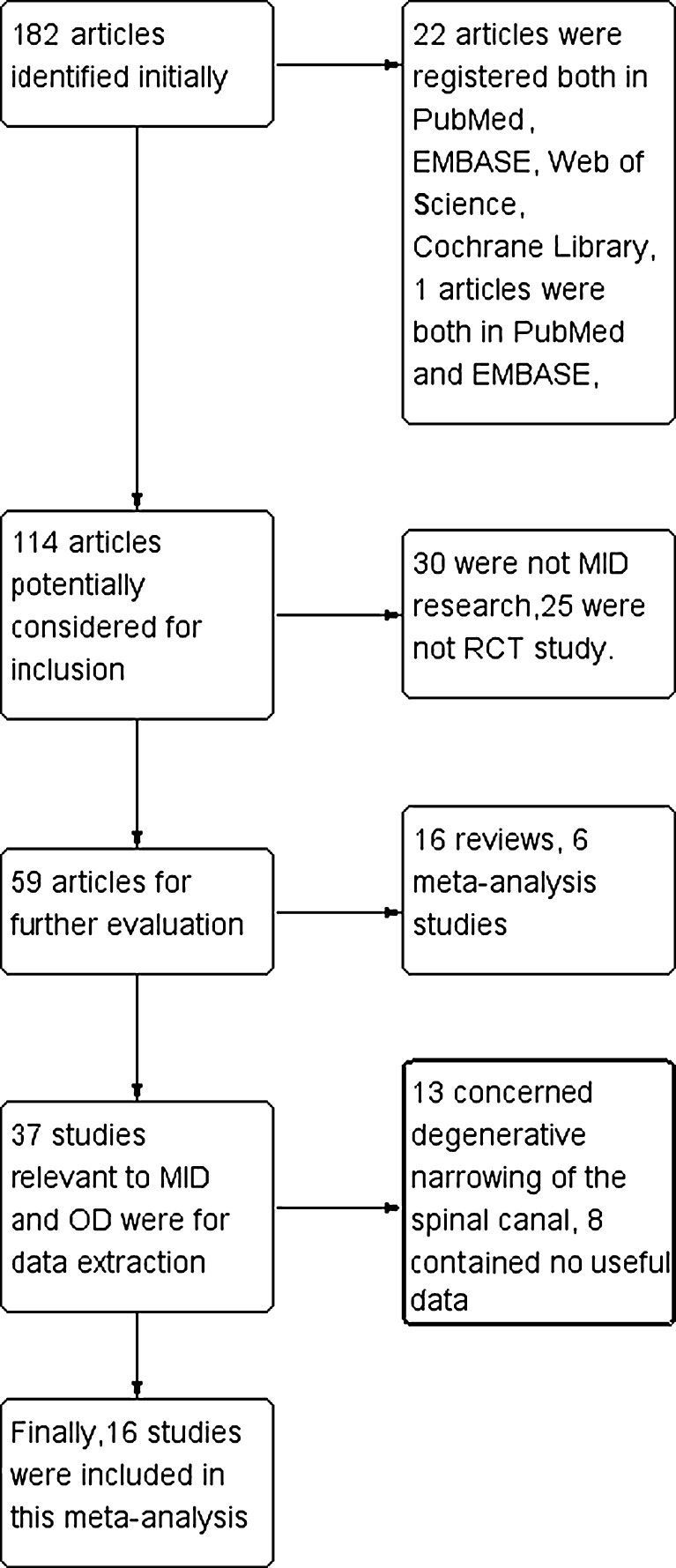
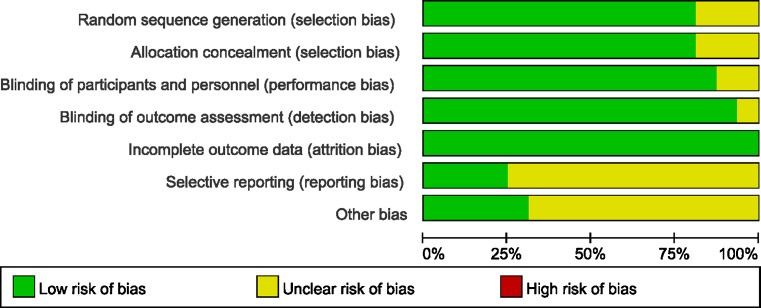
With the search strategy (Fig. 1), 16 studies were identified and met our inclusion criteria. They were all in English including 2,139 cases (1,085 of MID and 1,054 of SD). Thus, this systematic review was based on 16 articles: Tullberg et al. [11], Henriksen et al. [12], Hermantin et al. [13], Türeyen [14], Huang et al. [15], Katayama et al. [16], Righesso et al. [17], Ryang et al. [18], Arts et al. [7], Teli et al. [8], Arts et al. [19], Arts et al. [20], Garg et al. [21], Mariscalco et al. [22], van den Akker et al. [23] and Wang et al. [24]. The basic information of these trials are presented in Table 1. With the help of the Cochrane Collaboration’s tool, the risk of bias was assessed. When there was no bias, it was denoted with “+”, otherwise “?” was listed, all showed in Figs. 2 and 3. Selective reporting was doubtful in most studies. Only one study’s protocols could be found [25].
Fig. 1.
Flow chart for inclusion of studies
Table 1.
Summary of the research articles included in this review
| Study | Year | No. of patients (MID:SD) | Mean age | Results |
|---|---|---|---|---|
| Tullberg et al. [11] | 1993 | 60 (30:30) | 40 | Blood loss, VAS score after the surgery |
| Henriksen et al. [12] | 1996 | 79 (39:40) | 41.3 | Surgical time, size of incision |
| Hermantin et al. [13] | 1999 | 60 (30:30) | 39.5 | Complications |
| Türeyen [14] | 2003 | 114 (63:51) | 41.5 | VAS score after the surgery, size of incision |
| Huang et al. [15] | 2005 | 22 (10:12) | 39.7 | Surgical time, blood loss, VAS score after the surgery, size of incision |
| Katayama et al. [16] | 2006 | 119 (57:62) | 37.5 | Surgical time, blood loss, VAS score after the surgery, hospital stay, disc herniation recurrence |
| Righesso et al. [17] | 2007 | 40 (21:19) | 43.9 | Surgical time, blood loss, VAS score after the surgery, size of incision, disc herniation recurrence |
| Ryang et al. [18] | 2008 | 60 (30:30) | 38.5 | Surgical time, blood loss, VAS score after the surgery, hospital stay, complications, disc herniation recurrence |
| Arts et al. [7] | 2009 | 328 (167:161) | 41.6 | Surgical time, hospital stay, complications, disc herniation recurrence |
| Teli et al. [8] | 2010 | 140 (70:70) | 39.3 | VAS score after the surgery, hospital stay, surgical costs, complications, disc herniation recurrence |
| Arts et al. [19] | 2011 | 216 (110:106) | 41 | Surgical time, hospital stay |
| Arts et al. [20] | 2011 | 325 (166:159) | 41.6 | Surgical time, hospital stay, complications, disc herniation recurrence |
| Garg et al. [21] | 2011 | 112 (55:57) | 37 | Hospital stay, complications, disc herniation recurrence |
| Mariscalco et al. [22] | 2011 | 60 (30:30) | 46.3 | X-ray exposure |
| van den Akker et al. [23] | 2011 | 325 (166:159) | – | VAS score after the surgery, surgical costs |
| Wang et al. [24] | 2011 | 79 (41:38) | 51.4 | Surgical time, blood loss, VAS score after the surgery, hospital stay, X-ray exposure, complications |
Fig. 2.
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study
Fig. 3.
Risk of bias: review authors’ judgements about each risk of bias item presented as percentages across all included studies
Age of the patients
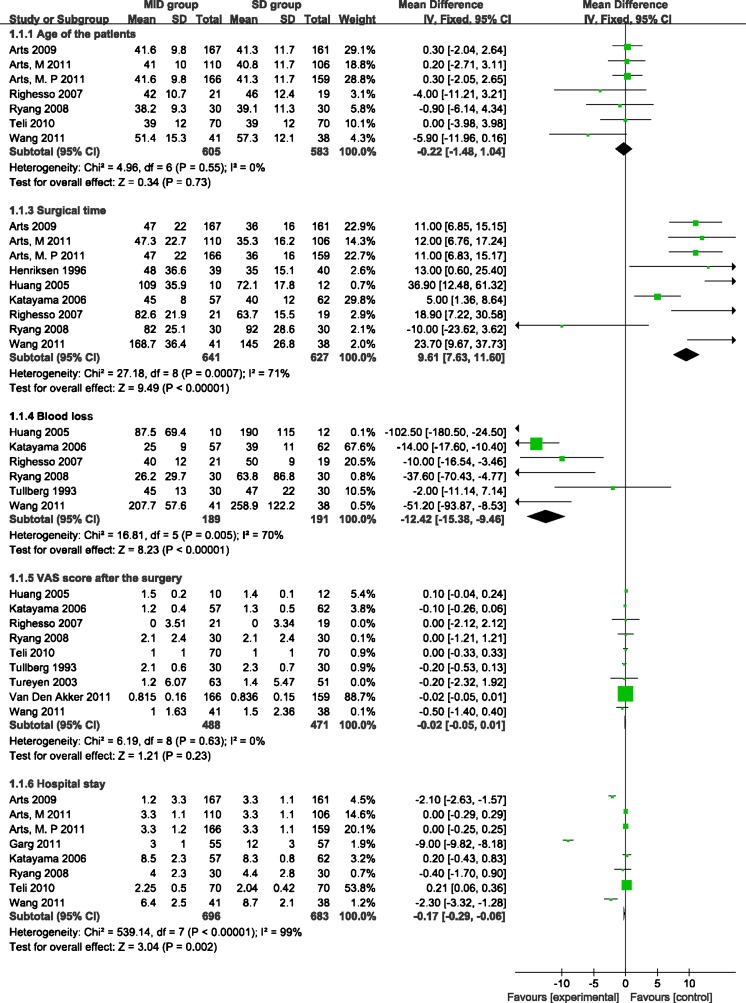
Clinical studies have shown that age has a large impact on clinical signs and symptoms in patients with LDH, so the ages of the two groups were analysed. After reading the literature, we found that seven of the 16 studies reported the age of the patients. All of them offered adequate data about the mean and standard deviation. The pooled estimate showed that the MID group was associated with an insignificant statistical difference compared with the SD group [weighted mean difference (WMD) = −0.22, 95 % CI −1.48 to 1.04, p = 0.73]. There was no evidence for significant heterogeneity (I2 = 0 %, p = 0.55) (Fig. 4).
Fig. 4.
Forest plot (fixed effects model) illustrating age of the patients, surgical time, blood loss, VAS score of the leg after the surgery and hospital stay of meta-analysis comparing MID with SD
Size of incision
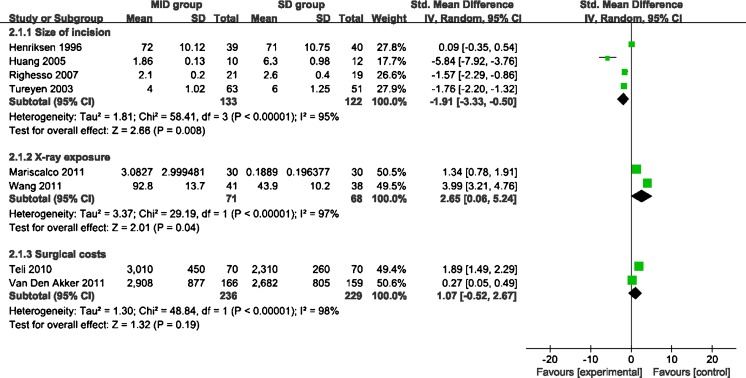
Four trials concerned the size of the incision. As it is known to all, the advantage of microscopy is to enable surgeons to perform procedures through small incisions. Three of them reported the existence of a statistically significant difference between the MID and SD groups, while the other study found no difference. Overall, comparing MID with SD, the standardised mean difference (SMD) was −1.91 (95 % CI −3.33 to −0.5, p = 0.008 ), showing the former has a much smaller incision size. Significant heterogeneity was detected among the studies (I2 = 95 %, p < 0.00001). The size of incision is one of the most important parameters. It is well known that a longer incision could increase the risk of negative complications, such as bleeding, healing more slowly or even infection. Viewed through these lenses, it can be confirmed that the smaller size of incision in MID is good for patients (Fig. 5).
Fig. 5.
Forest plot (random effects model) illustrating size of incision, X-ray exposure and surgical costs of meta-analysis comparing MID with SD
Surgical time
Nine studies reported the mean surgical time and the standard deviation. Eight of the nine trails revealed the surgical time of the MID group is longer than the SD group, and only Ryang et al. reported that MID needs less time to complete. Overall, the statistical results showed the WMD was statistically significant (WMD = 9.61, 95 % CI 7.63–11.60, p < 0.00001), suggesting MID required more time for the surgical procedure. This result is in accordance with prior assumptions. Moderate heterogeneity existed between these studies (I2 = 71 %, p = 0.0007) (Fig. 4).
Blood loss
The intra-operative blood loss was assessed in six studies. Five of them reported less blood loss in the MID group, but Tullberg et al.’s research denoted the perioperative bleeding was the same in both groups. From the statistics of the data summed up, the WMD was statistically significant (WMD = −12.42, 95 % CI −15.38 to −9.46, p < 0.00001) in favour of the MID group. Moderate heterogeneity were detected among the studies (I2 = 70 %, p = 0.005). From the data presented previously, it can be concluded that MID causes less bleeding and also means the surgery causes fewer traumas (Fig. 4).
VAS score after the surgery
VAS score is one of the leading indicators for verifying the effects of interventions. LBP has multiple causes, while sciatica is a unique symptom of LDH. So sciatica could always be relieved after the surgery. Thus, compared with LBP, the relief of sciatica (leg pain) would be a more appropriate choice to evaluate the effects of the surgery. In the studies we found, nine trails reported the VAS score of the leg pain after surgery. Overall, the comprehensive statistics showed that there was no obvious statistically significant difference between MID and SD (WMD = −0.02, 95 % CI −0.05 to 0.01, p = 0.23). χ2 tests indicated no heterogeneity existed among these trails (I2 = 0 %, p = 0.63) (Fig. 4). The results indicated to us that for LDH both MID and SD are appropriate, as long as the surgeons have mastery of the procedures.
Hospital stay
Data regarding hospital stay were available in eight studies. All reported a significant difference between the MID and SD groups. The overall estimate revealed that the SMD was 0.17 days longer in the SD group (95 % CI −0.29 to −0.06, p = 0.002). The heterogeneity was significant among the studies (I2 = 99 %, p < 0.00001) (Fig. 4). The length of hospital stay varies widely. In different reports the post-operative stay ranged from 1.1 to 8.5 days. According to the report by Teli et al. [8], most of the patients who stay in hospital more than two days after surgery were always people with a dural tear, so the hospital stay cannot truly reflect the difference between the two surgeries.
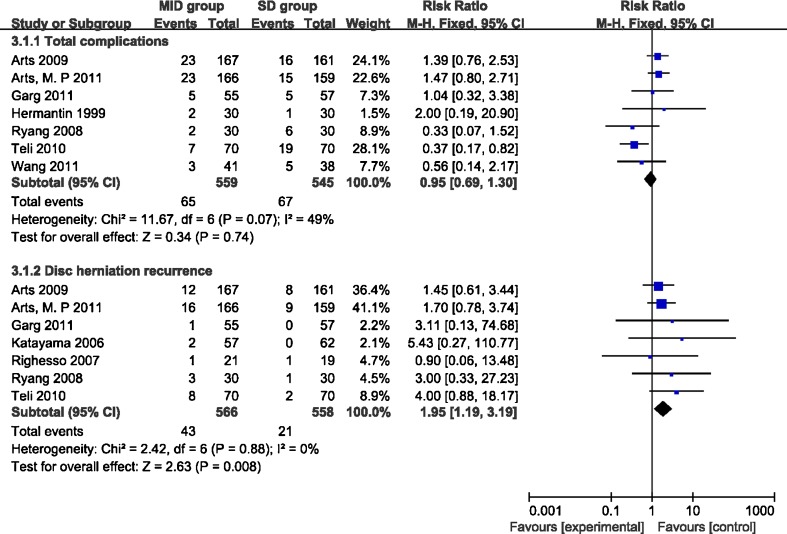
Total complications
Arts et al. [7], Garg et al. [21] and Hermantin et al. [13] compared patients allocated to the MID and SD groups and found MID had more complications during and after the procedure. However, the studies by Ryang et al. [18], Teli et al. [8] and Wang et al. [24] showed the opposite, while Garg et al.’s study revealed the two groups had an insignificant difference. The overall complication rate was similar between the MID and SD groups (RR = 0.95, 95 % CI 0.69–1.30, p = 0.74). Moderate heterogeneity existed among the trials (I2 = 49 %, p = 0.07) (Fig. 6). From the trials included in this article, little difference about complications between the two groups could be determined.
Fig. 6.
Forest plot illustrating total complications and disc herniation recurrence of meta-analysis comparing MID with SD
Disc herniation recurrence
Seven studies reported the rate of recurrence after different surgical procedures. All seven indicated a higher recurrence with MID. The overall estimate also revealed that the MID group showed a higher statistically significant recurrence rate than the SD group (RR = 1.95, 95 % CI 1.19–3.19, p = 0.008). The χ2 test indicated no statistical evidence of heterogeneity (I2 = 0 %, p = 0.88) (Fig. 6).
X-ray exposure
Details concerning X-ray exposure were available in two studies. Both trials reported obviously reduced X-ray exposure in the OD group for both patients and the surgeon. The SMD was 2.65 (95 % CI 0.06–5.24, p < 0.05) in support of the SD group having less X-ray exposure. Significant heterogeneity was detected among the two studies (I2 = 97 %, p < 0.00001) (Fig. 5).
Surgical costs
The surgical costs had rarely been the target of the meta-analysis, for the RCT trials concerning this subject were very rare. We found two studies concerned with surgical costs. The overall estimate revealed that the two group had a statistically insignificant difference when compared with each other (SMD = 1.07, 95 % CI −0.52 to 2.67, p = 0.19). The heterogeneity was significant among the trials (I2 = 98 %, p < 0.00001) (Fig. 5).
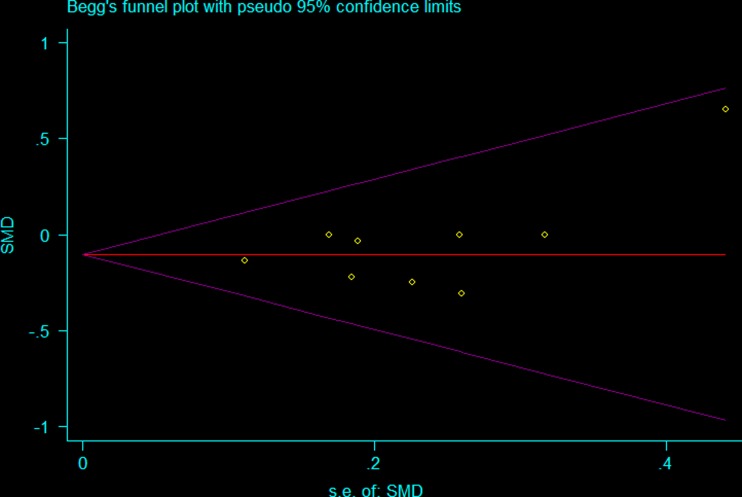
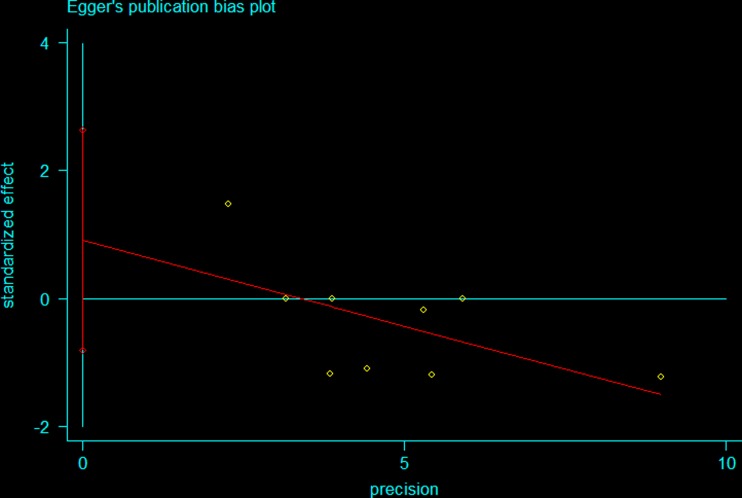
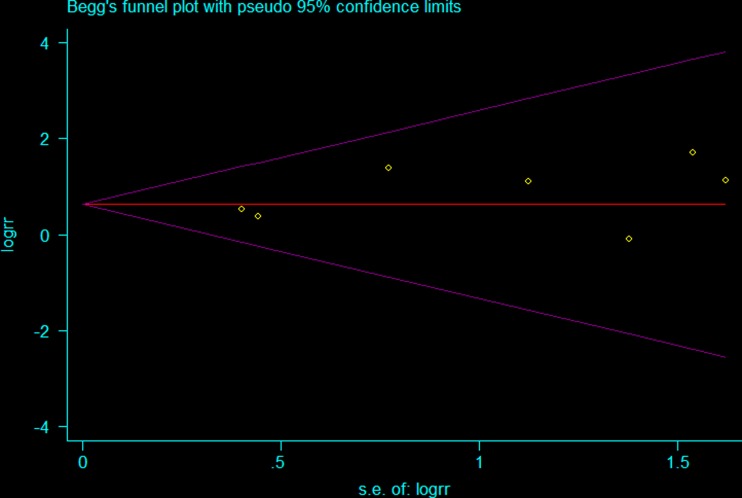
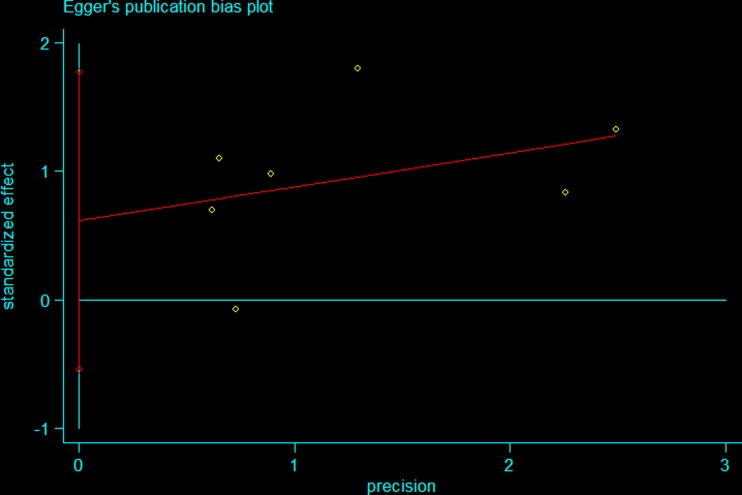
Publication bias
The Stata 12.0 software was used to examine the publication bias of the main results. Both Begg’s and Egger’s tests showed a statistically difference. The results indicated that no statistically significant publication bias existed regarding VAS [(Pr > |z| =0.754 > 0.05 (continuity corrected)] (Figs. 7 and 8) and disc herniation recurrence after surgery [(Pr > |z| = 0.764 > 0.05 (continuity corrected)] (Figs. 9 and 10).
Fig. 7.
Begg’s test illustrating the publication bias of VAS of the leg pain after the surgery
Fig. 8.
Egger’s test illustrating the publication bias of VAS of the leg pain after the surgery
Fig. 9.
Begg’s test illustrating the publication bias of disc herniation recurrence after surgery
Fig. 10.
Egger’s test illustrating the publication bias of disc herniation recurrence after surgery
Discussion
LDH is a common disease in modern society, the incidence of which is second only to upper respiratory tract infections in the USA. Treatment of LDH still remains a great challenge to clinical physicians. For those patients who fail to respond to extensive conservative treatment, surgical treatment should be considered.
In general, there are two methods for intervertebral disc surgery: one is MID and the other is SD. Compared with SD, MID enables the use of smaller incisions of the skin and fascia and facilitates a less traumatic surgical procedure. Firstly, it can hardly cause the muscle, ligament and lumbar stability to suffer from any impairment. Secondly, in some types of MID methods, the patients are kept awake during the procedure, enabling complete removal of the fragment while avoiding considerable nerve root injury. Thirdly, it has the merits of a small wound and early recovery. So they were widely admired since their inception.
However, the latest large sample multicentre RCT revealed that MID could hardly relieve the symptoms of the waist and leg. One study even argued that MID can help to increase the recurrence of disc herniation. In order to determine whether the use of the MID technique decreases the recurrence and compare its safety and efficacy with SD, we collected the documents and performed a standard meta-analysis.
In this paper, more than 2,000 patients were included and analysed; the statistical results indicated that the two methods have the same effect in alleviating pain (the VAS score had no statistically significant difference) and both are effective methods.
Since more time is needed to do sufficient preoperative preparation (such as measurement and placement of the surgical incision) and precisely insert the working tube [24], MID calls for more surgical time. That is consistent with our statistical findings.
According to our results, the MID group was more likely to experience increased disc herniation recurrence. The Ryang et al. and Teli et al. studies also showed this trend. Actually most scholars agree that MID surgical procedures have a very steep learning curve and call for accumulation of clinical experience. Improper use may be the main reason for some sorts of complications and directly affect the clinical effects. Another reason could be insufficient removal of the herniated disc or degenerative changes of disc tissue [26], which may explain why the MID group was more likely to experience increased disc herniation recurrence.
A previous meta-analysis comparing MID and SD had not focused on the economic evaluation and X-ray exposure for both patients and the operators; we therefore performed a cost utility and radiation analysis from RCT. The pooled estimate showed that the two groups were associated with an insignificant statistical difference when compared with each other.
Our findings suggest that MID and SD are both effective methods, obtaining similar VAS score of the leg pain after the surgery, X-ray exposure, hospital stay and surgical costs. MID had a smaller size of incision, a shorter hospital stay, but more effort should be put into reducing herniation recurrence and surgical time. High-quality, large studies are needed to do further comparison of the two techniques.
So although MID is a relatively safe minimally invasive procedure, the much higher possibility of recurrence after surgery still calls for our attention. Only when we can recognise the causative mechanisms and prevent these correctly and fully, master the basic knowledge, improve the surgical technique and be familiar with preventive measures can we ensure that the MID spine technique has a wider application and more promotion in the clinical setting.
References
- 1.Campbell P, Wynne-Jones G, Muller S, Dunn KM. The influence of employment social support for risk and prognosis in nonspecific back pain: a systematic review and critical synthesis. Int Arch Occup Environ Health. 2013;86:119–137. doi: 10.1007/s00420-012-0804-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoy DG, Smith E, Cross M, Sanchez-Riera L, Buchbinder R, Blyth FM, Brooks P, Woolf AD, Osborne RH, Fransen M, Driscoll T, Vos T, Blore JD, Murray C, Johns N, Naghavi M, Carnahan E, March LM. The global burden of musculoskeletal conditions for 2010: an overview of methods. Ann Rheum Dis. 2014 doi: 10.1136/annrheumdis-2013-204344. [DOI] [PubMed] [Google Scholar]
- 3.Gautschi OP, Hildebrandt G, Cadosch D. Acute low back pain–assessment and management. Praxis. 2008;97:58–68. doi: 10.1024/1661-8157.97.2.58. [DOI] [PubMed] [Google Scholar]
- 4.Saleem S, Aslam HM, Rehmani MA, Raees A, Alvi AA, Ashraf J. Lumbar disc degenerative disease: disc degeneration symptoms and magnetic resonance image findings. Asian Spine J. 2013;7:322–334. doi: 10.4184/asj.2013.7.4.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schoenfeld AJ. Historical contributions from the Harvard system to adult spine surgery. Spine. 2011;36:E1477–E1484. doi: 10.1097/BRS.0b013e3181f2d52c. [DOI] [PubMed] [Google Scholar]
- 6.Koebbe CJ, Maroon JC, Abla A, El-Kadi H, Bost J. Lumbar microdiscectomy: a historical perspective and current technical considerations. Neurosurg Focus. 2002;13:E3. doi: 10.3171/foc.2002.13.2.4. [DOI] [PubMed] [Google Scholar]
- 7.Arts MP, Brand R, van den Akker ME, Koes BW, Bartels R, Peul WC, Leiden-The Hague Spine Intervention Prognostic Study Group (SIPS) Tubular diskectomy vs conventional microdiskectomy for sciatica: a randomized controlled trial. JAMA. 2009;302:149–158. doi: 10.1001/jama.2009.972. [DOI] [PubMed] [Google Scholar]
- 8.Teli M, Lovi A, Brayda-Bruno M, Zagra A, Corriero A, Giudici F, Minoia L. Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur Spine J. 2010;19:443–450. doi: 10.1007/s00586-010-1290-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Tulder M, Furlan A, Bombardier C, Bouter L, et al. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine. 2003;28:1290–1299. doi: 10.1097/01.BRS.0000065484.95996.AF. [DOI] [PubMed] [Google Scholar]
- 10.Sterne JA, Egger M, Smith GD. Systematic reviews in health care: investigating and dealing with publication and other biases in meta-analysis. BMJ. 2001;323:101–105. doi: 10.1136/bmj.323.7304.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tullberg T, Isacson J, Weidenhielm L. Does microscopic removal of lumbar disc herniation lead to better results than the standard procedure? Results of a one-year randomized study. Spine. 1993;18:24–27. doi: 10.1097/00007632-199301000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Henriksen L, Schmidt K, Eskesen V, Jantzen E. A controlled study of microsurgical versus standard lumbar discectomy. Br J Neurosurg. 1996;10:289–293. doi: 10.1080/02688699650040160. [DOI] [PubMed] [Google Scholar]
- 13.Hermantin FU, Peters T, Quartararo L, Kambin P. A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J Bone Joint Surg Am. 1999;81:958–965. doi: 10.2106/00004623-199907000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Türeyen K. One-level one-sided lumbar disc surgery with and without microscopic assistance: 1-year outcome in 114 consecutive patients. J Neurosurg. 2003;99:247–250. doi: 10.3171/spi.2003.99.3.0247. [DOI] [PubMed] [Google Scholar]
- 15.Huang TJ, Hsu RW, Li YY, Cheng CC (2005) Less systemic cytokine response in patients following microendoscopic versus open lumbar discectomy. J Orthop Res 23:406–411 [DOI] [PubMed]
- 16.Katayama Y, Matsuyama Y, Yoshihara H, Sakai Y, Nakamura H, Nakashima S, Ito Z, Ishiguro N. Comparison of surgical outcomes between macro discectomy and micro discectomy for lumbar disc herniation: a prospective randomized study with surgery performed by the same spine surgeon. J Spinal Disord Tech. 2006;19:344–347. doi: 10.1097/01.bsd.0000211201.93125.1c. [DOI] [PubMed] [Google Scholar]
- 17.Righesso O, Falavigna A, Avanzi O. Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: results of a randomized controlled trial. Neurosurgery. 2007;61:545–549. doi: 10.1227/01.NEU.0000290901.00320.F5. [DOI] [PubMed] [Google Scholar]
- 18.Ryang YM, Oertel MF, Mayfrank L, Gilsbach JM, Rohde V. Standard open microdiscectomy versus minimal access trocar microdiscectomy: results of a prospective randomized study. Neurosurgery. 2008;62:174–181. doi: 10.1227/01.NEU.0000311075.56486.C5. [DOI] [PubMed] [Google Scholar]
- 19.Arts M, Brand R, van der Kallen B, Lycklama à Nijeholt G, Peul W. Does minimally invasive lumbar disc surgery result in less muscle injury than conventional surgery? A randomized controlled trial. Eur Spine J. 2011;20:51–57. doi: 10.1007/s00586-010-1482-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arts MP, Brand R, van den Akker ME, Koes BW, Bartels RHA, Tan W, Peul WC. Tubular diskectomy vs conventional microdiskectomy for the treatment of lumbar disk herniation: 2-year results of a double-blind randomized controlled trial. Neurosurgery. 2011;69:135–144. doi: 10.1227/NEU.0b013e318214a98c. [DOI] [PubMed] [Google Scholar]
- 21.Garg B, Nagraja UB, Jayaswal A. Microendoscopic versus open discectomy for lumbar disc herniation: a prospective randomised study. J Orthop Surg (Hong Kong) 2011;19:30–34. doi: 10.1177/230949901101900107. [DOI] [PubMed] [Google Scholar]
- 22.Mariscalco MW, Yamashita T, Steinmetz MP, Krishnaney AA, Lieberman IH, Mroz TE (2011) Radiation exposure to the surgeon during open lumbar microdiscectomy and minimally invasive microdiscectomy: a prospective, controlled trial. Spine 36:255–260 [DOI] [PubMed]
- 23.van den Akker ME, Arts MP, van den Hout WB, Brand R, Koes BW, Peul WC. Tubular diskectomy vs conventional microdiskectomy for the treatment of lumbar disk-related sciatica: cost utility analysis alongside a double-blind randomized controlled trial. Neurosurgery. 2011;69:829–835. doi: 10.1227/NEU.0b013e31822578f6. [DOI] [PubMed] [Google Scholar]
- 24.Wang HL, Lü FZ, Jiang JY, Ma X, Xia XL, Wang LX. Minimally invasive lumbar interbody fusion via MAST quadrant retractor versus open surgery: a prospective randomized clinical trial. Chin Med J. 2011;124:3868–3874. [PubMed] [Google Scholar]
- 25.Arts MP, Peul WC, Brand R, Koes BW, Thomeer RTWM. Cost-effectiveness of microendoscopic discectomy versus conventional open discectomy in the treatment of lumbar disc herniation: a prospective randomised controlled trial [ISRCTN51857546] BMC Musculoskelet Disord. 2006;7:42. doi: 10.1186/1471-2474-7-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Suk KS, Lee HM, Moon SH, Kim NH. Recurrent lumbar disc herniation: results of operative management. Spine. 2001;26:672–676. doi: 10.1097/00007632-200103150-00024. [DOI] [PubMed] [Google Scholar]