Abstract
Parental anxiety is a risk to optimal treatment outcomes for childhood anxiety disorders. The current trial examined whether the addition of a brief parental anxiety management (BPAM) program to family cognitive behavioral therapy (CBT) was more efficacious than family CBT-only in treating childhood anxiety disorders. Two hundred nine children (aged 6–13 years, 104 female, 90% Caucasian) with a principal anxiety disorder were randomly allocated to family CBT with a five-session program of BPAM (n = 109) or family CBT-only (n = 100). Family CBT comprised the Cool Kids program, a structured 12-week program that included both mothers and fathers. Overall, results revealed that the addition of BPAM did not significantly improve outcomes for the child or the parent compared to the CBT-only group at posttreatment or 6-month follow-up. Overall, however, children with nonanxious parents were more likely to be diagnosis free for any anxiety disorder compared to children with anxious parents at posttreatment and 6-month follow-up. BPAM did not produce greater reductions in parental anxiety. The results support previous findings that parent anxiety confers poorer treatment outcomes for childhood anxiety disorders. Nevertheless the addition of BPAM anxiety management for parents in its current format did not lead to additional improvements when used as an adjunct to family CBT in the treatment of the child's anxiety disorder. Future benefits may come from more powerful methods of reducing parents’ anxiety.
Empirical data support the efficacy of cognitive behavioral therapy (CBT) for anxious youth (Cartwright-Hatton, Roberts, Chitsabesan, Fothergill, & Harrington, 2004). Despite its efficacy, the remission rate following CBT is 56.5% in anxious youth, and it is clear that a significant proportion of children and adolescents do not respond to CBT. An important challenge for clinical researchers is the identification of risk factors that impede optimal treatment response, and in targeting these factors, enhance outcomes for anxious youth.
There has been growing interest in the contribution of parental anxiety to treatment outcomes of the anxious child. This interest has been guided by studies implicating a significant positive association between child and parent anxiety (Last, Hersen, Kazdin, Francis, & Grubb, 1987; Rapee, Schniering, & Hudson, 2009; Silverman, Kurtines, Jaccard, & Pina, 2009). Moreover, there has been some evidence that the presence of untreated parental anxiety poses a significant risk to the successful short-term outcome of child-focused CBT for anxiety disorders. For example, in a large-scale clinical trial, only 38.9% of children were diagnosis free if they had one anxious parent compared to 82.4% of children without anxious parents who were diagnosis free at the end of treatment (Cobham, Dadds, & Spence, 1998). Another studyalso demonstrated that maternalanxiety obstructed optimal treatment outcomes for the child at 1-year follow-up (Kendall, Hudson, Gosch, Flannery-Schroeder, & Suveg, 2008).
A small number of studies have emerged that have concurrently targeted parental anxiety in the treatment of anxious youth (Creswell, Willetts, Murray, Singhal, & Cooper, 2008). Cobham et al. (1998) demonstrated that the addition of Parent Anxiety Management (PAM) to child CBT enhanced posttreatment diagnostic outcomes compared to child CBT without PAM, but only for children with at least one anxious parent. Of interest, this favorable result for the inclusion of PAM was not maintained at 6- and 12-month follow-up and was not apparent on any measure aside from diagnostic status. However, at the 3-year follow-up, the provision of PAM conferred significant benefits regardless of parental anxiety status. That is, children in the PAM + CBT group were more likely to be diagnosis free compared to children in the CBT-only group even if their parent was not anxious. A key limitation of this study was the reliance on self-report questionnaire measures to determine parental anxiety. The use of self-report measures is problematic for a number of reasons: (a) Parents of anxious children tend to underreport their own anxiety symptoms, potentially due to feelings of guilt that is associated with feeling responsible for the child's anxiety (Kendall & Suveg, 2006), and (b) self-report measures of anxiety tend to be less objective than clinical interviews (Bogels & Brechman-Toussaint, 2006).
The current study investigated whether adding a brief treatment for parent anxiety would enhance the efficacy of standard family CBT for anxious children. We hypothesized that the inclusion of a brief PAM (BPAM) would enhance treatment outcomes only for anxious children with at least one clinically anxious parent. The current study included the following improvements on previous studies: (a) the sample allowed sufficient power to detect a moderate effect size difference between groups, and (b) parent anxiety was determined through diagnostic interviews at pretreatment, posttreatment, and 6 month follow-up. The addition of BPAM to family CBT was expected to be superior to family CBT alone in terms of (a) diagnostic outcomes and clinical severity gleaned from posttreatment diagnostic status and (b) symptom change based on parent- and child-reported anxiety symptoms.
METHOD
Participants
Participants in the study were 209 children and their parents seeking psychological treatment for the child's anxiety. Eligible children were aged 6 to 13 years and met criteria for a principal (most impairing) anxiety disorder according to Diagnostic and Statistical Manual of Mental Disorders (4th ed. [DSM-IV]). Anxiety disorders were assessed using the Anxiety Disorders Interview Schedule for DSM-IV, Child and Parent Versions (Silverman & Albano, 1996). Exclusion criteria included intellectual and developmental disability, psychoses, disabling medical conditions, and concurrent psychological treatment. Parents who were identified during the assessment as having a psychological disorder were asked to delay any treatment until after the study was complete. Children on medication for anxiety or depression were included (n = 12) if the dose was stable for 2 weeks during treatment. Adolescents (12–13 years) with comorbid major depression were referred to an alternate program (n = 3). Children with comorbid behavioral disorders who had a clinical severity rating (CSR) of 6 or more were excluded. Figure 1 presents the flow of participants through the study.
FIGURE 1.
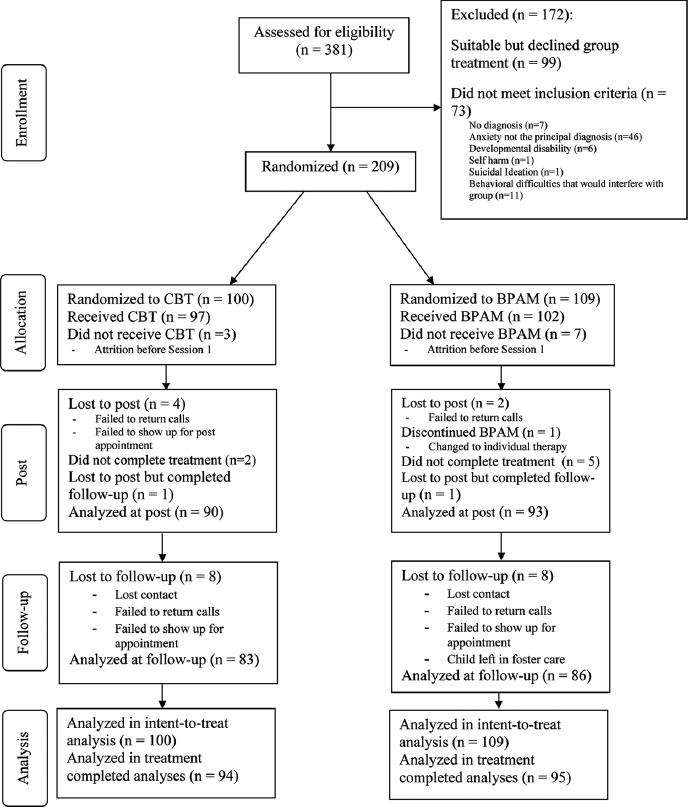
Flow of participants through the clinical trial. Note: CBT = child and family cognitive-behavioral therapy; BPAM = CBT and parental anxiety management program.
Measures
Child Psychopathology
Structured interview. Children and parents were interviewed using the Anxiety Disorder Interview Schedule for Children—Child and Parent version (ADIS-IV-C/P; Silverman & Albano, 1996). Diagnoses and CSRs (on a scale of 0 to 8) were assigned by graduate students in clinical psychology or qualified clinical psychologists based on composite parent and child report. A severity of 4 or more on the CSR indicated that diagnostic criteria were met at a clinically interfering level.1 Clinicians were trained to match anxiety diagnoses within one severity rating of each other. Fifteen participants were double coded for reliability purposes. The intraclass correlation for the total CSR among clinicians was .83. Interrater reliability (kappa) for the presence of a disorder in the child's profile was .84 for the presence of a principal anxiety diagnosis and .82 for any anxiety diagnosis.
Anxiety symptoms. The Spence Children's Anxiety Scale (Spence, 1998) was used to assess child- and mother-reported anxiety symptoms. This measure contains 38 items that load on a single factor (range = 0–114). Internal consistency and retest reliability are good (Nauta et al., 2004; Spence, 1998). The measure distinguishes anxious and nonclinical children and has adequate convergent validity. The internal consistency in the current sample was good to excellent (mother report α = .88; child report α = .91).
Parent Psychopathology
Structured interview. Parental anxiety was assessed using the ADIS-IV (Brown, Di Nardo, & Barlow, 1994). The ADIS-IV is a semistructured clinical interview for assessing anxiety disorders and other diagnoses in adults according to DSM-IV criteria. Again, a CSR of 4 or more indicated the presence of a clinical disorder. The child was considered to have an anxious parent if one or both parents met criteria for an anxiety disorder. A total of 16 parents were double coded for reliability purposes. The intraclass correlation for the total CSR was .93. Interrater reliability (kappa) for the presence of a disorder in the parent's profile was .85 for the presence of a principal anxiety diagnosis and .85 for any anxiety diagnosis.
Depression anxiety stress scales-21 items (DASS-21; lovibond & lovibond, 1995). Parents completed the DASS-21 to assess for current parental anxiety symptoms via the anxiety subscale (scores 7 and below are considered within the range of normal). The DASS-21 has demonstrated good internal consistency and concurrent validity (Antony, Bieling, Cox, Enns, & Swinson, 1998). The internal consistency for the current sample of mothers and fathers on the DASS Anxiety subscale were moderate (mother report α = .77; father report α = .71).
Treatment Conditions
Treatments for child anxiety were conducted in groups in ten 2-hr, weekly sessions. In each session, the therapist spent roughly equal time with the children, parent(s), and parents and children together. Children (n = 5–7) were allocated to a group based on age, resulting in groups of children with a range of different anxiety disorders. All treatment sessions were audiotaped for reliability purposes. The primary therapist for each group (n = 10) was a paid clinical psychologist or a postgraduate clinical student. Training and weekly supervision was provided by the clinic director or the first author.
CBT Group
The CBT condition used the Cool Kids program, which has established efficacy (e.g., Hudson et al., 2009). The manual-based program is designed for the management of broad-based childhood anxiety disorders and includes psychoeducation, cognitive restructuring, gradual exposure, child management skills, and assertiveness training. The primary focus of most sessions is on the development and evaluation of the gradual exposure and use of other strategies to support exposure. With the exception of one therapist-assisted in-group session of in vivo exposure, children completed gradual exposure under the direction of their parents for homework. Any discussion of parental anxiety was removed from the treatment manual and all treatment focused on the child's anxiety and not on the parent's.
BPAM Group
The BPAM group completed the Cool Kids program in an identical format to the CBT group and in addition received five × 45-min sessions of BPAM training. The parental anxiety management program comprised of a bibliotherapy program supplemented with five therapistled group-based sessions.2 Parents received extensive printed materials describing strategies and were encouraged by therapists to engage in extensive home practices. The program included psychoeducation about anxiety, cognitive restructuring, gradual exposure, assertiveness, problem-solving skills, and time management. The main aim of the BPAM component was to teach parents to manage their anxiety via CBT techniques. Three of the BPAM sessions focused on gradual exposure. Parents were given individualized attention in planning exposures at home.
Therapist time spent treating the child's anxiety was matched for both treatment conditions. BPAM parents received additional therapist time focused on their own anxiety (with a different therapist). BPAM sessions were held during the time the Cool Kids therapist was working with the children and parents would usually be in the waiting room (45–55 min).
Treatment Integrity
Treatment integrity was assessed in a random sample of 20% of therapy sessions using the observer-rated Protocol Adherence Checklist-Modified (Southam-Gerow & Kendall, 2002), adapted for each condition. Therapists demonstrated an average of 96% adherence to the manual for Cool Kids and 92% in the BPAM program.
Procedure
The ethical procedures of this study were approved by the Macquarie University Human Ethics Committee. After a brief telephone screen, parents signed consent forms at assessment, and the children provided verbal assent. Children who met criteria for inclusion and agreed to participate were allocated to a group based on the child's age. The first author used a schedule from a random number generator to assign each group to CBT (19 groups) or BPAM (19 groups) and to therapists. We encouraged both parents to attend wherever possible and provided child-minding services for siblings. Families completed a post- and 6-month follow-up assessment (ADIS-IV-C/P, ADIS-IV, and symptom measures for children and parents). Structured interviews were conducted by diagnosticians masked to condition. Post-and follow-up diagnoses with a CSR less than 4 were considered remitted.
Data Analyses
Based on treatment allocation and parent diagnostic status, the study consisted of four groups as follows: BPAM + Anxious Parent (n = 74), CBT + Anxious Parent (n = 70), BPAM + Non-anxious Parents (n = 21), CBT + Nonanxious Parents (n = 24). The Anxious Parent groups comprised children who had two parents with an anxiety disorder (32%), an anxious mother only (55%), or an anxious father only (13%). Due to administrative error, 27%) of parental attendance of treatment sessions in the BPAM condition was not recorded. However, of the mothers (n = 68) and fathers (n = 70) whose session attendance was recorded in the BPAM condition, 66 mothers (97%) and 57 fathers (81%) completed both the BPAM and CBT program.
Missing diagnostic data for intent-to-treat was handled via the last-point-carried-forward method. Continuous data were analyzed using a stacked database (each line represented one observation for one participant). This method ensured that missing observation did not result in deletion of the participant (Peugh & Enders, 2005). Participants in the completer sample (N = 189) included families in which the child and at least one parent completed a minimum of six sessions of the Cool Kids program, and for BPAM at least one of the parents must also have completed at least three sessions.3 This yielded a final distribution of 94 children in the CBT group and 95 children in BPAM group. From the completer sample, 98% of anxious mothers (48 of 49) and 92% of anxious fathers (22 of 24) completed the BPAM program.
The proportion of participants who no longer met criteria for the principal anxiety diagnosis and any anxiety diagnosis, at post- and 6-month follow-up in the two conditions, was examined using chi-square tests of independence. Mixed models containing random factors for subject and fixed effects for treatment group, parental anxiety status at pre-, and time (including two- and three-way interactions) were fitted to measures of child-and mother-reported symptoms and diagnostic severity.
RESULTS
Attrition
Treatment completers were compared to attrition cases on sociodemographic, diagnostic, and pretreatment measures. Children who dropped out of treatment were older than treatment completers (completers: M = 9.5 years, SD = 2.0; attrition cases: M = 10.47, SD = 1.84), t(202) = 2.01, p <.05. No other significant differences between attrition cases and completers were detected (p < .05).
Pretreatment Comparisons
The treatment groups were examined for pretreatment differences on demographic variables via a series of chi-square tests and 2 (anxious vs. nonanxious parents) × 2 (BPAM vs. CBT) univariate analyses of variance. There were no significant pretreatment differences between the groups on family sociodemographic variables (see Table 1). Results showed that there were significantly more children with externalizing disorders among nonanxious parents (17 of 45, or 37.8%) compared to anxious parents (29 of 144, or 20.1%; χ2(1, N = 189) = 5.79, p < .05. There were no other pretreatment differences for the children between groups (Table 1).
TABLE 1.
Demographic Data Across Conditions (Standard Deviations) in Treatment Completers
| Anxious | Anxious | Nonanxious | Non-Anxious | |
|---|---|---|---|---|
| Demographic | Parent + BPAMa | Parent + CBTb | Parent + BPAMc | Parent + CBTd |
| Child Sex, % Female | 55.4 | 45.7 | 52.4 | 50.0 |
| Children's M Age | 9.2 (2.0) | 9.6 (2.0) | 9.6 (2.0) | 9.5 (2.0) |
| Family Income, % | ||||
| > $80,000 | 52.1 | 52.2 | 78.9 | 57.1 |
| $40,000–80,000 | 31.5 | 31.3 | 10.5 | 28.6 |
| $20, 000–40,000 | 12.3 | 11.9 | 10.5 | 9.5 |
| $0–20,000 | 4.1 | 4.5 | 0 | 4.8 |
| No. of Siblings | 1.6(0.9) | 1.3 (0.9) | 1.3 (0.7) | 1.4(.9) |
| Ethnicitye, % | ||||
| Australian | 75.3 | 77.9 | 85.0 | 82.6 |
| Asian/Asian Australian | 6.8 | 2.9 | 5.0 | 0 |
| European/European Australian | 11.0 | 14.7 | 5.0 | 4.3 |
| American/American Australian | 1.4 | 1.5 | 0 | 0 |
| Other | 4.1 | 2.9 | 0 | 4.3 |
| Family Makeup, % | ||||
| Two Parent | 91.9 | 79.7 | 84.2 | 82.6 |
| Single Parent | 6.8 | 13.0 | 5.3 | 8.7 |
| Stepparents/Blended | 1.4 | 7.2 | 10.5 | 8.7 |
| Mothers’ M Age | 41.2(5.0) | 41.1 (5.2) | 41.8 (5.5) | 42.6 (5.4) |
| Mothers’ Education Level, | ||||
| School Certificate | 17.2 | 8.6 | 0 | 9.1 |
| Higher School Certificate | 9.4 | 6.9 | 10.5 | 9.1 |
| TAFE/Apprenticeship | 9.4 | 5.2 | 5.3 | 4.5 |
| Certificate/Diploma | 25.0 | 32.8 | 36.8 | 36.4 |
| Undergraduate Degree | 25.0 | 24.1 | 21.1 | 22.7 |
| Postgraduate Degree | 14.1 | 22.4 | 26.3 | 18.2 |
| Mothers’ Employment Status | ||||
| Stay-at-Home Parent | 27.7 | 29.3 | 26.3 | 18.2 |
| Full-Time Student | 1.5 | 0 | 5.3 | 4.5 |
| Unemployed/Illness | 1.5 | 5.2 | 0 | 0 |
| Part-Time Work | 53.8 | 46.6 | 68.4 | 63.6 |
| Full-Time Work | 13.8 | 19.0 | 0 | 13.6 |
| Retired | 1.5 | 0 | 0 | 0 |
| Fathers’ M Age | 43.2 (5.2) | 42.7 (6.7) | 44.6 (6.7) | 45 (4.0) |
| Fathers’ Education Level | ||||
| Primary School | 0 | 1.9 | 0 | 0 |
| School Certificate | 9.7 | 9.4 | 11.8 | 5.6 |
| Higher School Certificate | 8.1 | 7.5 | 11.8 | 11.1 |
| TAFE/Apprenticeship | 19.4 | 15.1 | 0 | 5.6 |
| Certificate/Diploma | 22.6 | 9.4 | 17.6 | 27.8 |
| Undergraduate Degree | 16.1 | 30.2 | 35.3 | 22.2 |
| Postgraduate Degree | 24.2 | 26.4 | 23.5 | 27.8 |
| Fathers' Employment Status | ||||
| Stay-at-Home Parent | 1.6 | 3.8 | 0 | 0 |
| Unemployed/Illness | 1.6 | 1.9 | 0 | 0 |
| Part-Time Work | 3.2 | 3.8 | 0 | 10.5 |
| Full-Time Work | 90.3 | 90.6 | 100 | 89.5 |
| Retired | 3.2 | 0 | 0 | 0 |
| Children's Principal Diagnoses, % | ||||
| GAD | 52.7 | 51.4 | 28.6 | 37.5 |
| SOC | 14.9 | 24.3 | 33.3 | 12.5 |
| SAD | 16.2 | 7.1 | 23.8 | 12.5 |
| PD | 1.4 | 0 | 0 | 4.2 |
| OCD | 8.1 | 10.0 | 14.3 | 4.2 |
| SPEC | 5.4 | 5.7 | 0 | 25.0 |
| PTSD | 1.4 | 0 | 0 | 4.2 |
| ADNOS | 0 | 1.4 | 0 | 0 |
| Children's Comorbid Diagnoses (%)f | ||||
| Anxiety | 93.2 | 94.3 | 85.7 | 95.8 |
| Externalizing | 24.3 | 15.7 | 42.9 | 33.3 |
| Mood Disorders | 8.1 | 4.3 | 4.8 | 0 |
| Otherg | 3.0 | 6.7 | 5.0 | 8.7 |
| No Comorbidity | 6.8 | 5.7 | 14.3 | 4.2 |
| No. of Comorbid Diagnoses | 3.0 (1.7) | 2.7 (1.6) | 2.3 (1.4) | 2.8 (1.6) |
| Maternal Principal Diagnoses, % | ||||
| GAD | 31.3 | 37.7 | NA | NA |
| SOC | 21.9 | 27.9 | NA | NA |
| PD | 3.1 | 1.6 | NA | NA |
| OCD | 4.7 | 1.6 | NA | NA |
| SPEC | 34.4 | 29.5 | NA | NA |
| PTSD | 1.6 | 0 | NA | NA |
| Mood Disorder | 3.1 | 1.6 | 4.7 | 0 |
| Paternal Principal Diagnoses, % | ||||
| GAD | 21.4 | 29.7 | NA | NA |
| SOC | 33.3 | 43.2 | NA | NA |
| SPEC | 23.5 | 13.5 | NA | NA |
| OCD | 2.4 | 0 | NA | NA |
| Mood Disorder | 9.5 | 8.1 | 0 | 4.7 |
| Otherh | 9.5 | 5.4 | 4.7 | 0 |
Note: BPAM = parent anxiety management and cognitive-behavioral therapy; CBT = cognitive-behavioral therapy; GAD = generalized anxiety disorder; OCD = obsessive-compulsive disorder; PD = panic disorder; SAD = separation anxiety disorder; SOC = social phobia; SPEC = specific phobia; PTSD = post-traumatic stress disorder; ADNOS = anxiety disorder not otherwise specified.
n = 74.
n = 70.
n = 21.
n = 24.
Parents were asked to record their ethnicity in an open-ended question. The majority of our participants identify as “Australian”. A smaller portion of families identify as Northwest, Southern, or Eastern European (e.g., Italian, Croatian Australian) or Southeast, Northeast, Southern, or Central Asian (Thai, Chinese Australian) heritage.
Comorbid diagnoses represent all secondary disorders with a CSR of 4 or greater in the child's diagnostic profile.
Other childhood disorders included selective mutism (n = 1), developmental disability (n = 1), and enuresis (n = 3).
Other paternal disorders included adjustment disorder (n = 2), hypochondriasis (n = 1), ADHD (n = 1), alcohol abuse/dependence (n = 1), obsessive compulsive personality disorder (n = 1), and insomnia (n = 1).
Pretreatment scores on questionnaires were examined via two-way analysis of variance. There was a main effect of parental anxiety status at pretreatment on the maternal DASS Anxiety subscale, F(1, 181) = 7.71, p < .05. No other significant main effects or interactions were observed for any of the remaining questionnaires at pretreatment.
Mixed-model analyses were conducted to determine whether therapy group4 and therapist were significant sources of variation on the main outcome variables. Results revealed that there was no clustering (all ps > .05) and the median intraclass correlation was zero, ranging from 0 to .06. Thus therapy group and therapist were not a significant source of variation and could be disregarded.
Diagnostic Changes at Posttreatment and Follow-Up Across Conditions
Child Diagnostic Status
The proportion of children who were free of their principal anxiety disorder and any anxiety disorders at posttreatment and follow-up is shown in Table 2. At posttreatment, no significant main effects for treatment condition (CBT vs. BPAM) or parental anxiety status (anxious vs. nonanxious parents at pretreatment) were found for principal anxiety diagnosis. That is, there were no differences in remission rates of principal diagnoses at posttreatment between CBT and BPAM and no difference in remission rates for children with anxious and nonanxious parents. When any anxiety diagnosis was taken into consideration at posttreatment, there was a main effect for parental anxiety status. That is, the percentage of children who were free of any anxiety diagnosis was significantly greater in the nonanxious parents group (14 of 45, or 31.1%) than in the anxious parents group (24 of 138, or 17.4%), χ2(1, N = 183) = 3.88, p < .05. No other significant differences were found for any anxiety diagnosis at posttreatment.
TABLE 2.
The Proportion of Children No Longer Meeting Criteria for Principal Anxiety Diagnosis and Any Anxiety Diagnoses at Posttreatment and Follow-Up Across the Two Conditions in the Treatment Completer Sample
|
Posttreatment |
Follow-Up |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Anxious Parent |
Nonanxious Parent |
Anxious Parent |
Nonanxious Parent |
|||||||
| BPAMa n (%) | CBTb n (%) | BPAMc n (%) | CBTd n (%) | BPAMe n (%) | CBTf n (%) | BPAMg n (%) | CBTh n (%) | |||
| Principal Diagnosis | 33 (45.8) | 22 (33.3) | 9 (42.9) | 13 (54.2) | 35 (53.0) | 31 (51.7) | 11 (55.0) | 13 (56.5) | ||
| Any Anxiety Diagnoses | 14 (19.4) | 10 (15.2) | 7 (33.3) | 7 (29.2) | 17 (25.8) | 18 (30.0) | 7 (35.0) | 12 (52.2) | ||
Note: BPAM = parent anxiety management and cognitive-behavioral therapy; CBT = cognitive-behavioral therapy.
n = 72.
n = 66.
n = 21.
n = 24.
n = 66.
n = 60.
n = 20.
n = 23.
A similar picture was found at the 6-month follow-up. No main effects were found for treatment group (CBT vs. BPAM) or parental anxiety status (anxious vs. nonanxious parents) for principal anxiety diagnosis. Again, when any anxiety diagnosis was taken into account at 6-month follow-up, children with nonanxious parents were significantly more likely to be diagnosis free (19 of 43, or 44.2%) compared to children with anxious parents (35 of 126, 27.8%) at follow-up, χ2(1, N = 190) = 3.97, p < .05. No other significant effects for principal diagnosis or any anxiety diagnoses were found at follow-up.
Intent-to-treat analyses produced comparable results for all chi-square analyses previously reported, with the exception that the main effect of parental anxiety status at the 6-month follow-up for any anxiety diagnosis revealed a trend rather than significance, χ2(1, N = 204) = 3.67, p = .058.
Parental Diagnostic Status
We examined whether treatment group affected maternal and paternal anxiety diagnostic status at post-and 6-month follow-up for anxious parents. Anxious parents were defined as parents with any anxiety diagnosis (CSR >4) at pretreatment. The proportion of anxious mothers and fathers who were diagnosis free at posttreatment and follow-up is shown in Table 3.
TABLE 3.
Proportion of Anxious Parents No Longer Meeting Criteria for Principal Anxiety Diagnosis and Any Anxiety Diagnoses at Posttreatment and Follow-Up Across the Two Conditions in the Completer Sample
| Posttreatment | Follow-Up | |||||||
|---|---|---|---|---|---|---|---|---|
|
Maternal |
Paternal |
Maternal |
Paternal |
|||||
| BPAMa n (%) | CBTb n (%) | BPAMc n (%) | CBTd n (%) | BPAMe n (%) | CBTf n (%) | BPAMg n (%) | CBTh n (%) | |
| Principal Anxiety Diagnosis | 22 (35.5) | 18 (32.7) | 15 (51.7) | 11 (34.4) | 23 (45.1) | 18 (36.0) | 15 (57.7) | 15 (51.7) |
| Any Anxiety Diagnoses | 16 (26.2) | 11 (20.0) | 6 (20.7) | 6 (18.8) | 12 (23.5) | 12 (24.0) | 8 (30.8) | 11 (37.9) |
Note: BPAM = parent anxiety management and cognitive-behavioral therapy; CBT = cognitive-behavioral therapy.
n = 61.
n = 55.
n = 29.
n = 32.
n = 51.
n = 50.
n = 26.
n = 29.
Results indicated that anxious mothers and fathers assigned to the BPAM treatment group were not significantly different from those in the CBT group at posttreatment or follow-up on principal or any anxiety diagnosis (ps > .05).
Symptoms Measures and Diagnostic Severity Across Time and Condition
Mixed-model analyses were fitted to clinical severity ratings (principal diagnosis, any anxiety diagnoses) and symptoms (child and mother report). The CSR for any anxiety diagnosis was summed across all anxiety diagnoses to give a total anxiety severity.
As can be seen in Table 4, there was a significant main effect for time. All measures observed a significant improvement from pre- to posttreatment and from pretreatment to 6mth follow-up. Only the CSR (principal) showed continued improvements from posttreatment to follow-up. In addition, there was a significant parent anxiety status effect for maternal anxiety (Table 4): Maternal anxiety was higher in the anxious parent groups than the nonanxious parent groups regardless of time or condition.5
TABLE 4.
Means for Pretreatment, Posttreatment, and Follow-Up Data Across the Four Conditions in the Completer Sample
|
CBT+ Anxious Parent |
CBT+ Non-Anxious Parent |
BPAM + Anxious Parent |
BP AM + N on-Anxious Parent |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre M | Post M | 6-Month | Pre M | Post M | 6-Month | Pre M | Post M | 6-Month | Pre M | Post M | 6-Month | ||
| Measure | (SE) | (SE) | FU M (SE) | (SE) | (SE) | FU M (SE) | (SE) | (SE) | FU M (SE) | (SE) | (SE) | FU M (SE) | F and t Values |
| CSR (Principal) | 6.49 (.18) | 4.36 (.18) | 3.66 (.19) | 6.46 (.30) | 3.71 (.30) | 3.08 (.31) | 6.37 (.17) | 3.78 (.17) | 3.65 (.18) | 6.10 (.32) | 4.05 (.32) | 3.45 (.33) | Time effect* F (2, 352) = 214.94, p <.01; t (349) = 16.05, p = .00a; t (353) = 19.30, p = .00b; t (353) = 3.44, p = .00c |
| CSR (Anxiety Diagnosis) | 18.65 (.91) | 12.88 (.92) | 11.85 (.95) | 18.33 (1.55) | 12.33 (1.55) | 9.80 (1.56) | 19.87 (.88) | 13.38 (.89) | 13.14 (.91) | 15.05 (1.62) | 10.67 (1.65) | 10.14 (1.67) | Time effect* F (2, 348) = 92.50, p = .00; t (347) = 10.74, p = .00a; t (348)= 12.54, p = .00b; t (348) = 2.01, nsc |
| SCAS (Child) | 33.94 (1.77) | 22.76 (1.85) | 21.20 (1.93) | 30.14 (3.04) | 22.13 (3.08) | 17.26 (3.08) | 35.46 (1.72) | 23.64 (1.75) | 19.74 (1.87) | 28.13 (3.25) | 21.52 (3.21) | 18.54 (3.36) | Time effect* F (2, 311) = 59.28, p = .00; t (310) = 7.94, p = .00a, t (313) = 10.35, p = .00b; t (311) = 2.71, p = .01c |
| SCAS (Mother) | 34.99 (1.43) | 22.47 (1.52) | 20.26 (1.58) | 28.29 (2.46) | 21.30 (2.46) | 19.02 (2.50) | 36.25 (1.38) | 25.10 (1.41) | 20.38 (1.51) | 32.93 (2.63) | 20.15 (2.63) | 19.17 (2.73) | Time effect* F (2, 314) = 86.88, p = .00; t (313) = 10.24, p = .00a; t (317)= 11.93, p = .00b; t (311) = 2.33, p = .02c |
| DASS Anxiety Subscale (Mother) | 7.31 (.65) | 5.00 (.69) | 5.06 (.71) | 3.56 (1.11) | 2.97 (1.11) | 2.90 (1.13) | 6.38 (.63) | 5.33 (.64) | 4.04 (.68) | 4.13 (1.19) | 2.14 (1.19) | 1.96 (1.23) | Time effect* F (2, 316) = 9.25, p = .00; t (316) = 3.32, p = .00a; t (319) = 4.01, p = .00b; t (314) = .08, nsc; Parental anxiety status effect, F (1,179) = 10.73, p = .00. |
| DASS Anxiety Sub scale (Father) | 4.09 (.58) | 3.21 (.60) | 3.68 (.63) | 4.69 (1.02) | 3.21 (1.06) | 3.08 (1.08) | 5.45 (.55) | 4.17 (.56) | 3.63 (.58) | 2.19 (1.06) | 1.65 (1.05) | 1.56 (1.08) | Time effect* F (2, 273) = 6.37, p = .00;t (273) = 3.03, p = .00a; t (276) = 3.11, p = .00b; t (271) = .19, nsc |
Note: Pre = pretreatment; Post = posttreatment; FU = follow-up; CSR principal = Clinical Severity Rating for the child's principal diagnosis; CSR anxiety diagnosis = summed Clinical Severity for all anxiety diagnoses for the child; CBT = cognitive-behavioral therapy condition; BPAM = cognitive-behavioral therapy and brief parental anxiety management condition; SCAS = Sp-Spence Children's Anxiety Scale; DASS = Depression Anxiety Stress Scale; SMF = Short Mood and Feelings Questionnaire.
Pretreatment to posttreatment.
Pretreatment to 6-month follow-up.
Posttreatment to 6-month follow-up.
Note that significance is set p <.017 for time main effect follow-up comparisons (pretreatment to posttreatment, pretreatment to 6-month follow-up, and posttreatment to 6-month follow-up) to adjust for multiple simple comparison.
DISCUSSION
The results of the current study indicate that the addition of a specific treatment component aimed at parents’ anxiety to a standard family-based treatment for child anxiety did not enhance treatment outcomes for children, even among children who had a parent with an anxiety disorder. The diagnostic outcome for parental anxiety at posttreatment and follow-up provides the most parsimonious explanation for the results. Specifically, among anxious fathers and mothers, the provision of BPAM did not improve parental anxiety diagnoses at posttreatment and 6-month follow-up compared to anxious parents who did not receive BPAM, indicating that BPAM did not have its intended effects of reducing parental anxiety. Consistent with the diagnostic patterns, there were no differences in self-reported symptoms of parental anxiety between parents who received BPAM and those that did not, nor did BPAM interact with parental anxiety status to predict child anxiety treatment outcomes. These results are consistent with the finding from Cobham et al. (1998), who also failed to show significant reductions in parents’ anxiety following their anxiety management program. The lack of effects on parents’ anxiety is surprising given the extensive evidence that self-help programs augmented with therapist contact can provide highly efficacious treatment for adult anxiety disorders (Hirai & Cium, 2006). Although the current effects may reflect an “insufficient dose” of BPAM, it is also possible that they reflect additional complications in integrating parent and child treatment. Is it possible that parents were reluctant to work on their own anxiety when seeking treatment for their child, or were they too focused on helping their child to work on their own fears? These questions need to be examined in future studies.
The lack of a significant benefit of BPAM is largely consistent with previous research (Cobham et al., 1998; Creswell et al., 2008). An apparent exception was demonstrated by Cobham et al. (1998) on only a single measure, and this effect disappeared by 6-month follow-up. Therefore the current state of evidence appears to indicate that adding parent anxiety treatment to treatment for child anxiety results in little, if any improvements. As previously noted, however, research to date has failed to alter parents’ anxiety and so this conclusion must be tempered by the caveat that the fundamental significant benefits of BPAM emerged after 3 years (Cobham, Dadds, Spence, & McDermott, 2010), despite the lack of initial anxiety reduction among parents and regardless of whether parents were anxious initially. Thus, it is possible that BPAM provides some additional components that are not necessarily related to the parent's anxiety. If parental anxiety disorders did not reduce in the current BPAM because of “insufficient dose,” it will mean that future BPAM programs may need to increase the intensity, duration, and/or number of BPAM sessions (Barlow, 2007).
It is worth noting that there was a reduction in parental anxiety symptoms in our study for all groups. However, given the significant number of parental anxiety disorders present at the end of treatment, it is unlikely that this reduction in symptoms was of clinical significance. The improvements in parental anxiety for the family-focused CBT groups may have been due to spontaneous recovery and the alleviation of family stress as a consequence of improvements in the child's anxiety. One possibility to consider is that improvements in parental anxiety may also have been due to parental deployment of strategies discussed in family-focused CBT, even without the provision of BPAM. Specifically, it is very likely that anxious parents in the family-focused CBT groups also used cognitive therapy and exposure therapy to manage his or her anxiety. The reduction of parental anxiety symptoms across time for both the CBT and BPAM group could explain the absence of group differences: All children may have benefited from the universal reduction of parental anxiety. Furthermore, the changes in child anxiety resulting from the child components of the Cool Kids program may have led to changes in parental anxiety and parental behaviors (Silverman et al., 2009). As there was not a waitlist control, it is unclear whether parental anxiety symptoms declined as a consequence of spontaneous recovery or having received CBT directly (BPAM groups) and indirectly (CBT groups) for parental anxiety. It is also worth noting that unlike Cobham et al., we did not conduct a stratified randomization (i.e., have a separate randomization list for children with and without anxious parents). Nevertheless, our randomization procedures did not result in an unbalanced design and thus the absence of stratification does not appear to have resulted in any material difference.
A finding of theoretical and practical importance in the current study was that the presence of parental anxiety diagnosis conferred poorer treatment efficacy for the child. This finding was consistent across posttreatment and 6-month follow-up, and reflects the elevated risk for child anxiety by having an anxious parent (Rapee et al., 2009). This consistent finding provides impetus to continue to search for methods to reduce parents’ anxiety within the context of treatment for childhood anxiety disorders.
Implications for Research, Policy, and Practice
The current study suggests that the inclusion of BPAM to family CBT did not enhance child treatment outcomes. The study results, however, continue to emphasize the merit of addressing parental anxiety in interventions for childhood anxiety disorders because the children in our study were less likely to be diagnosis free if they had a parent who also had an anxiety disorder. This large-scale study strongly suggests that five sessions of BPAM did not lead to an enhanced decline in parental anxiety over and above the decline observed across time for children receiving CBT. The presence of parent anxiety is clearly a risk factor that therapists working with anxious children need to consider. To date, neither our BPAM program nor Cobham et al.'s program was sufficient in reducing parental anxiety disorder in conjunction with treatment for the child. A more intensive BPAM program for parents may be needed.
Footnotes
The “or” rule was used, that is, a diagnosis was assigned when reported by either parent or child (unless the rule would result in duplicating symptoms in two diagnoses, in which case clinical judgment was used).
The manual is available from the authors.
As noted earlier, a portion of parental session attendance of treatment programs was not recorded. To manage this missing data without losing a substantial portion of our overall sample, parents whose session attendance was not recorded in = 61, about 29% of overall sample) but completed ADISes across all three time points were also considered treatment completers in = 45).
Note that therapy group refers to the group to which the child was allocated based on age and not the treatment condition. Hence age was entered as a covariate when examining cluster effects.
Intent-to-treat analyses produced comparable results for all outcomes reported in this section.
References
REFERENCES
- Antony M. M., Bieling P. J., Cox B. J., Enns M. W., Swinson R. P. Psychometric properties of the 42-item and 21-item version of the Depression Anxiety Stress Scales (DASS) in clinical groups and a community sample. Psychological Assessment. 1998;10:176–181. [Google Scholar]
- Barlow D. H. Clinical handbook of psychological disorders: A step-by-step treatment manual. New York, NY: Guilford; 2007. [Google Scholar]
- Bogels S. M., Brechman-Toussaint M. L. Family issues in child anxiety: attachment, family functioning, parental rearing and beliefs. Clinical Psychology Review. 2006;26:834–856. doi: 10.1016/j.cpr.2005.08.001. [DOI] [PubMed] [Google Scholar]
- Brown T. A., Di Nardo P. A., Barlow D. H. Anxiety Disorders Inverview Schedule for DSM-IV (ADIS-IV) [Computer software] San Antonio, TX: GPOWER; 1994. [Google Scholar]
- Cartwright-Hatton S., Roberts C., Chitsabesan P., Fothergill C., Harrington R. Systematic review of the efficacy of cognitive behaviour therapies for childhood and adolescent anxiety disorders. British Journal of Clinical Psychology. 2004;43:421–436. doi: 10.1348/0144665042388928. [DOI] [PubMed] [Google Scholar]
- Cobham V. E., Dadds M. R., Spence S. H. The role of parental anxiety in the treatment of childhood anxiety. Journal of Consulting and Clinical Psychology. 1998;66:893–905. doi: 10.1037//0022-006x.66.6.893. [DOI] [PubMed] [Google Scholar]
- Cobham V. E., Dadds M. R., Spence S. H., McDermott B. Parental anxiety in the treatment of childhood anxiety: A different story three years later. Journal of Clinical Child & Adolescent Psychology. 2010;39:410–420. doi: 10.1080/15374411003691719. [DOI] [PubMed] [Google Scholar]
- Creswell C., Willetts L., Murray L., Singhal M., Cooper P. Treatment of child anxiety: An exploratory study of the role of maternal anxiety and behaviours in treatment outcome. Clinical Psychology and Psychotherapy. 2008;15:38–44. doi: 10.1002/cpp.559. [DOI] [PubMed] [Google Scholar]
- Hirai M., Clum G. A. A meta-analytic study of self-help interventions for anxiety problems. Behavior Therapy. 2006;37:99–111. doi: 10.1016/j.beth.2005.05.002. [DOI] [PubMed] [Google Scholar]
- Hudson J. L., Rapee R. M., Deveney C., Schneiring C. A., Lyneham H. J., Bovopoulos N. Cognitive-behavioral treatment versus an active control for children and adolescents with anxiety disorders: A randomized trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:533–544. doi: 10.1097/CHI.0b013e31819c2401. [DOI] [PubMed] [Google Scholar]
- Kendall P. C., Hudson J. L., Gosch E., Flannery-Schroeder E., Suveg C. Cognitive-behavioral therapy for anxiety disordered youth: A randomized clinical trial evaluating child and family modalities. Journal of Consulting and Clinical Psychology. 2008;76:282–297. doi: 10.1037/0022-006X.76.2.282. [DOI] [PubMed] [Google Scholar]
- Kendall P. C., Suveg C. Treating anxiety disorders in youth. Child and Adolescent Therapy: Cognitive-Behavioral Procedures. 2006;3:243–294. [Google Scholar]
- Last C. G., Hersen M., Kazdın A., Francis G., Grabb H. J. Psychiatric illness in the mothers of anxious children. American Journal of Psychiatry. 1987;144:1580–1583. doi: 10.1176/ajp.144.12.1580. [DOI] [PubMed] [Google Scholar]
- Lovibond P. F., Lovibond S. H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33:335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Nauta M. H., Scholing A., Rapee R. M., Abbott M., Spence S. H., Waters A. A parent-report measure of children's anxiety: Psychometric properties and comparisons with child-report in a clinic and normal sample. Behaviour Research and Therapy. 2004;42:813–839. doi: 10.1016/S0005-7967(03)00200-6. [DOI] [PubMed] [Google Scholar]
- Peugh J. L., Enders C. K. Using the SPSS mixed procedure to fit cross-sectional and longitudinal multilevel models. Educational and Psychological Measurement. 2005;65:717–741. [Google Scholar]
- Rapee R. M., Schniering C A., Hudson J. L. Anxiety disorders during childhood and adolescence: Origins and treatment. Annual Review of Clinical Psychology. 2009;5:311–341. doi: 10.1146/annurev.clinpsy.032408.153628. [DOI] [PubMed] [Google Scholar]
- Silverman W. K., Albano A. M. The Anxiety Disorders Interview Schedule for Children for DSM-IV: Child and Parent Versions. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Silverman W. K., Kurtines W. M., Jaccard J., Pina A. A. Directionality of change in youth anxiety treatment involving parents: An initial examination. Journal of Consulting and Clinical Psychology. 2009;77:474–485. doi: 10.1037/a0015761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southam-Gerow M., Kendall P. C. Manual for the Protocol Adherence Checklist – Modified. Philadelphia, PA: Temple University; 2002. [Google Scholar]
- Spence S. H. A measure of anxiety symptoms among children. Behaviour Research and Therapy. 1998;36:545–566. doi: 10.1016/s0005-7967(98)00034-5. [DOI] [PubMed] [Google Scholar]


