Abstract
Background
Injection drug use remains a significant risk for acquiring HIV infection. The mechanisms by which morphine enhances HIV infection of human immune cells are largely unknown.
Objective
In this study, we sought to determine the possible mechanisms by which morphine upregulates HIV infection of human blood monocyte-derived macrophages (MDM).
Methods
In this study, MDM were infected with the R5, X4, and R5X4 HIV strains. HIV replication was determined by performing reverse transcriptase activity assays. HIV receptors were determined by performing reverse transcriptase polymerase chain reactions and flow cytometry assays. β-chemokines were analyzed by performing enzyme-linked immunosorbent assays. In addition, HIV R5 strain and murine leukemia virus envelope-pseudotyped HIV infection was performed to determine whether morphine affects HIV infection of macrophages at entry level.
Results
Morphine significantly enhanced HIV R5 strain infection of MDM but had little effect on X4 strain infection. The macrophage-tropic R5 strain envelope-pseudotyped HIV infection was markedly increased by morphine, whereas murine leukemia virus envelope-pseudotyped HIV infection was not significantly affected. Furthermore, morphine significantly upregulated CCR5 receptor expression and inhibited the endogenous production of β-chemokines in MDM. The opioid receptor antagonist naltrexone blocked the effects of morphine on the production of β-chemokines.
Conclusion
Opiates enhance HIV R5 strain infection of macrophages through the downregulation of β-chemokine production and upregulation of CCR5 receptor expression and may have an important role in HIV immunopathogenesis.
Keywords: CCR5, β-chemokines, macrophages, morphine, opioid
INTRODUCTION
Injection drug use (IDU) remains a significant risk for acquiring HIV infection.1 In fact, IDU represents one of the largest reservoirs of HIV in the United States and contributes to the fastest spread of the virus.2 Approximately 30% of patients with AIDS have a history of IDU, and their IDU frequently involves the abuse of opiates. Opioids exert profound effects on the function of cells of the human immune system3–5 and thus have been implicated as cofactors in the immunopathogenesis of HIV.1,2,4,6 Treatment with opioids in vitro or in vivo alters cytokine production and cell trafficking, enhances the susceptibility of the immune cells to HIV infection, and leads to increased viral titers in the brain.7
Studies in which cells have been used in vitro have demonstrated that morphine activates and enhances HIV replication in human immune cells.8–11 We recently showed that methadone, a synthetic opiate with pharmacologic properties similar to those of morphine, enhances HIV infection of human immune cells.11 Morphine trans-activates HIV-long terminal repeat promoters in human neuroblastoma cells.12 Although the in vitro data clearly demonstrate a correlation between opioids and HIV infection of human immune cells, the clinical implication of these in vitro findings remains unknown. Early epidemiologic studies have generated contradictory data regarding the role of IDU in the progression of HIV infection.6,13 Early studies reported that survival after an AIDS diagnosis was shorter among individuals with IDU and HIV infection than among other individuals with HIV infection.13 In addition, individuals with IDU who have the HIV infection have substantial pre-AIDS morbidity and mortality.14 The cessation of IDU has been positively correlated with a decrease in the rate of progression from HIV to AIDS.2,15,16 These data strongly indicate that opioids compromise the function of the human immune system and promote HIV infection of the immune cells. However, the mechanisms by which opioids enhance HIV infection of human immune cells are largely unknown.
In this study, we sought to determine the possible mechanisms by which morphine upregulates HIV infection of human blood monocyte-derived macrophages (MDM). Because β-chemokines (regulated upon activation, normal T-cell expressed and secreted [RANTES], macrophage inflammatory protein-1α [MIP-1α], and MIP-1β) and their receptor CCR5 play a crucial role in HIV infection of immune cells,17,18 we investigated whether morphine affects HIV infection of human blood MDM through the modulation of β-chemokine production and HIV primary co-receptor CCR5 expression.
METHODS
Monocyte Isolation and Culture
Peripheral blood was obtained from healthy adult donors without known history of drug abuse. Heparinized blood samples were identified as HIV antibody-negative by anonymous testing on the basis of enzyme-linked immunosorbent assay (ELISA; Beckman Coulter, Inc., Hialeah, Fla). Informed consent was obtained, and the Institutional Research Board of our institution approved our study. Monocytes were purified according to our previously described technique.19 In brief, heparinized blood was separated by centrifugation over lymphocyte separation medium (Organon Teknika Corp., Durham, NC) at 400–500×g for 45 min. The mononuclear cell layer was collected and incubated with Dulbecco modified Eagle medium (DMEM; Life Technologies, Grand Island, NY) in a 2% gelatin-coated flask for 45 minutes at 37°C, followed by removal of the nonadherent cells with DMEM. Adherent monocytes were detached with 10 mM ethylenediamine tetra-acetic acid. After the initial purification, more than 97% of the cells were monocytes, as determined by nonspecific esterase staining and flow cytometric analysis with the use of monoclonal antibody against CD14, a marker specific for monocytes and macrophages. Freshly isolated monocytes were plated in 48-well culture plates at a density of 5×105 cells/well in DMEM containing 10% fetal calf serum. MDM were 7-day-cultured monocytes in vitro. Monocyte and MDM viability was monitored by trypan blue exclusion and maintenance of cell adherence.
Reagents
Fluorescein isothiocyanate (FITC)-conjugated antibodies against CD14, CD4, and CCR5 were obtained from PharMingen (San Diego, Calif). FITC-conjugated antibody against CXCR4 was obtained from R&D Systems (Minneapolis, Minn). In addition, FITC-conjugated isotype-matched immunoglobulin G controls were purchased from PharMingen. Morphine sulfate was obtained from Elkins-Sinn, Inc. (Cherry Hill, NJ). Naltrexone was obtained from Sigma Chemical Co. (St. Louis, Mo).
HIV Strains
On the basis of their differential use of the major HIV co-receptors (CCR5 and CXCR4), HIV isolates have been referred to as R5, X4, or R5X4 strains.20 The macrophage-tropic R5 strains (Bal and BL-4), dual tropic R5X4 strain (DH12), and T cell-tropic X4 strain (UG024) were obtained from the AIDS Research and Reference Reagent Program (National Institutes of Health, Bethesda, Md). HIV Bal strain was isolated from human infant lung tissue. Primary macrophage-tropic strain (BL-4) was isolated from the blood of an individual with AIDS with the use of coculture with seronegative donor peripheral blood mononuclear cells stimulated with phytohemagglutinin activation and interleukin-2.
Preparation of Pseudotyped HIV
Recombinant luciferase-encoding HIV virions were pseudotyped with the envelopes (Env) from macrophage-tropic (ADA) or amphotropic murine leukemia virus (MLV). Human embryonic kidney cell line (293T) was cotransfected with the plasmids encoding either ADA Env or MLV Env and the plasmid-containing luciferase-encoding NL4-3 HIV backbone. Supernatants were collected as virus stock 48 hours later. The plasmids encoding HIV ADA or MLV Env were provided by John Moore (Aaron Diamond AIDS Research Center, New York, NY), and the plasmid with luciferase-encoding NL4-3 HIV backbone was provided by Ned Landau (Aaron Diamond AIDS Research Center). All virus stocks were assayed for p24 antigen and stored at −70°C as cell-free virus after filtration through a 0.22-µm-pore-size filter.
Reverse Transcriptase Assay
HIV reverse transcriptase (RT) activity was determined by performing the technique of Willey et al21 with modification. In brief, 10 µl collected culture supernatants were added to a cocktail containing poly(A), oligodeoxythymidine (Pharmacia, Inc., Piscataway, NJ), MgCl2, and 32P deoxythymidine triphosphate (Amersham Corp., Arlington Heights, Ill) and then incubated for 20 hours at 37°C. Then 30 µl of the cocktail were spotted onto DE81 paper and then dried and washed 5 times with 2× saline-sodium citrate buffer and once with 95% ethanol. The filter paper was then air-dried. Radioactivity was measured with a liquid scintillation counter (Packard Instrument, Inc., Palo Alto, Calif).
Flow Cytometry
To determine whether morphine affects the expression of CD14, CD4, CXCR4, and CCR5 on MDM, cells were incubated with or without morphine (10−10 M) for 24 h. The cells were then removed from the culture plate and resuspended in 100 µl phosphate-buffered saline (PBS). After incubation with 20 µl FITC-conjugated antibodies against CD14, CD4, CXCR4, and CCR5 for 45 min at 4°C, the cells were washed twice with PBS and fixed with 1% paraformaldehyde in PBS. FITC-conjugated control immunoglobulin G was isotype-matched for the antibodies described above. Fluorescence was analyzed with an Epics Elite flow cytometer (Beckman Coulter, Inc.).
β-Chemokine Titration
β-chemokine ELISA kits for MIP-1α, MIP-1β, and RANTES were purchased from Endogen, Inc. (Cambridge, Mass). The assay was performed as instructed in the protocol provided by the manufacturer. In brief, 50 µl supernatant was added to antibody-coated wells and incubated for 1 hour at room temperature. The plate was washed with the provided buffer solution and incubated with 100 µl biotinylated antibody reagent for 1 hour at room temperature. The plate was washed again, treated with 100 µl prepared streptavidin horseradish peroxidase solution, and incubated for 30 min at room temperature. After an additional wash, 100 µl tetramethyl benzidine substrate solution was added to each well, and color was allowed to develop at room temperature for 30 minutes. The reaction was stopped by the addition of 100 µl stop solution to each well. The plate was read with a microplate reader (ELX800; Bio-Tek Instruments, Inc., Winooski, Vt).
RNA Extraction and Reverse Transcription
Total cellular RNA was isolated from MDM (106 cells) with Tri-reagent (Molecular Research Center, Cincinnati, Ohio). In brief, the total RNA was extracted by performing a single-step, guanidium thiocyanate-phenol-chloroform extraction. After centrifugation at 13,000×g for 15 min at 4°C, the RNA-containing aqueous phase was precipitated in isopropanol. RNA precipitates were then washed once in 75% ethanol and resuspended in 30 µl RNase-free water. A total of 1 µg RNA was subjected to reverse transcription with the use of the reverse transcription system (Promega Corp., Madison, Wisc) with specific primers (antisense) for HIV receptor genes (CD4, CCR5, and CXCR4; see below for primer sequences) for 1 hour at 42°C. The reaction was terminated by incubating the reaction mixture at 99°C for 5 min and then kept at 4°C. The resulting cDNA was ready to serve as a template for polymerase chain reaction (PCR) amplification.
PCR Analysis
PCR amplification of HIV receptors (CD4, CCR5, and CXCR4) cDNA was performed with one-tenth of the resultant cDNA for 35 cycles with the use of AmpliTaq Gold (PerkinElmer-Cetus, Foster City, Calif) in a GeneAmp PCR System 2400 (PerkinElmer-Cetus). The specific oligonucleotide primers used were as follows: CD4 gene primers, 5'-GTGAACCTGGTGGTGATGAGAGC-3' (sense) and 5'-GGGCTACATGTCTTCTGAAACCGGTG-3' (antisense); CCR5 gene primers, 5'-CAAAA-AGAAGGTCTTCATTACACC-3' (sense) and 5'-CCTGTGCCTCTTCTTCTC-ATTTCG-3' (antisense); CXCR4 gene primers, 5'-GACCGCTACCTGGCCATT-3' (sense) and 5'-GTTGT-AGGGCAGCCAGCA-3' (antisense); and β-actin gene primers, 5'-ATGTGGCAC-CACACCTTCT-ACAATGAGCTGCG-3' (sense) and 5'-CGTCATACTCCTGCTTGCTGA-TCCACATCTGC-3' (antisense) (Clontech, Palo Alto, Calif). β-actin was used as a control to monitor the amount and the integrity of RNA in each sample. The oligonucleotide primers were synthesized by Integrated DNA Technologies, Inc. (Coralville, Iowa). The PCR mixture contained 0.2 mM diethylnitrophenyl thiophosphate, 20 pM of each of two primers, and 1.5 U AmpliTaq Gold in 1× reaction buffer (PerkinElmer-Cetus). Each of the PCR amplifications consisted of heat activation of AmpliTaq Gold for 9 minutes at 94°C followed by 35 cycles of 94°C for 30 seconds, 50°C for 30 seconds, and 72°C for 45 seconds, and further elongation at 72°C for 7 minutes. We performed electrophoresis on ethidium bromide-stained 3% NuSieve 3:1 agarose gel (FMC BioProducts, Rockland, Me) with the PCR-amplified products.
Pseudotyped Reporter Virus Entry Assay
Seven-day-cultured MDM in 48-well plates (5×105 cells/well) were incubated for 24 hours with or without morphine (10−10 M–10−8 M) and then infected with 20 ng of P24 Gag antigen equivalent of each pseudotyped HIV per well in the presence of polybrene (4 µg/ml). At 72 hours after infection, the cells were lysed in 150 µl 1× Reporter Lysis Buffer (Promega Corp.). Lysate (50 µl) was mixed with an equal volume of luciferase substrate (Promega Corp.), and luciferase activity was then assessed in a Wallac Trilux Microbeta Luminometer (Wallac, Turku, Finland). Data were presented as relative light units.
Morphine Treatment and HIV Infection
Seven-day-cultured MDM (5×105 cells/well in 48-well plates) were incubated for 12 hours with or without morphine (10−14 M–10−8 M) and/or naltrexone (10−8 M) before infection with different strains of HIV. In the case of morphine and naltrexone combination treatment of cells, naltrexone was added to the MDM cultures 30 minutes before the addition of morphine. The cells were infected with equal amounts of cell-free HIV based on p24 protein content (20 ng/106 cells) for 2 hours at 37°C in the presence or absence of morphine. The cells were then washed three times with DMEM to remove unabsorbed virus, and fresh medium containing morphine and/or naltrexone was added to cell cultures. The final wash was tested for viral RT activity and shown to be free of residual inoculum. Untreated cells severed as controls. The cells were treated with or without morphine every 4 days after infection. Culture supernatants were harvested for β-chemokine production by performing ELISA 96 hours after infection, and supernatants were also collected for the purpose of performing HIV RT activity assays on Day 8 after infection.
Statistical Analysis
Where appropriate, data were expressed as mean±SD. For comparison of the means of two groups (morphinetreated vs. untreated controls), statistical significance was assessed by using Student’s t test. Calculations were performed with the use of Stata statistical software (Stata Corp., College Station, Tex). Statistical significance was defined as p<0.05.
RESULTS
Effect of Morphine on Different HIV Tropic Strains
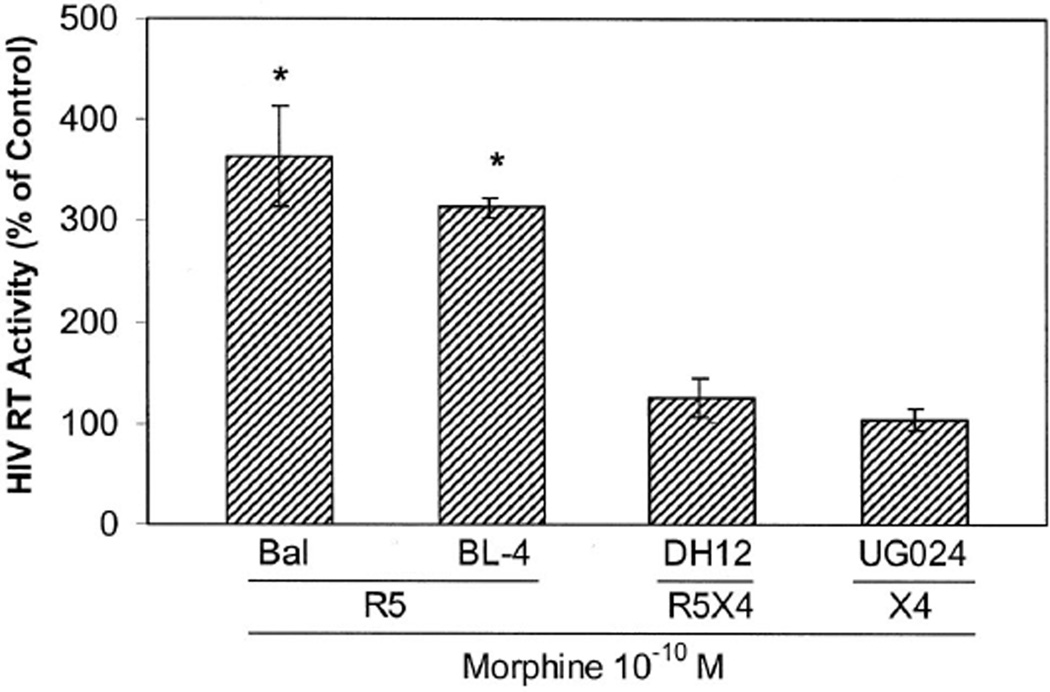
To determine the effect of morphine on the infection of human blood MDM by different HIV tropic strains (R5, X4, and R5X4), 7-day-cultured MDM were incubated with or without morphine (10−10 M) for 12 hours and challenged with R5 strains (Bal and BL-4), R5X4 strain (DH12), or X4 strain (UG024). Morphine significantly enhanced infection of the R5 strains, but R5X4 and X4 strains’ infection of MDM cultures were affected little (Fig. 1), suggesting that morphine affects HIV entry into MDM.
Figure 1.
Bar graph illustrating the effect of morphine on different HIV strains’ infection of MDM. Different HIV strains were used to infect MDM cultured for 7 days with or without morphine (10−10 M). HIV RT activity in the morphine-treated and HIV-infected MDM was expressed as the percentage of the activity of untreated and HIV (corresponding strains)-infected MDM controls, which were defined as 100%. The data shown are presented as the mean±SD of triplicate cultures and are representative of three experiments. *, p<0.01, morphine v control; R5, CCR5 tropic stains; X4, CXCR4 tropic strain; R5X4, dual tropic strain.
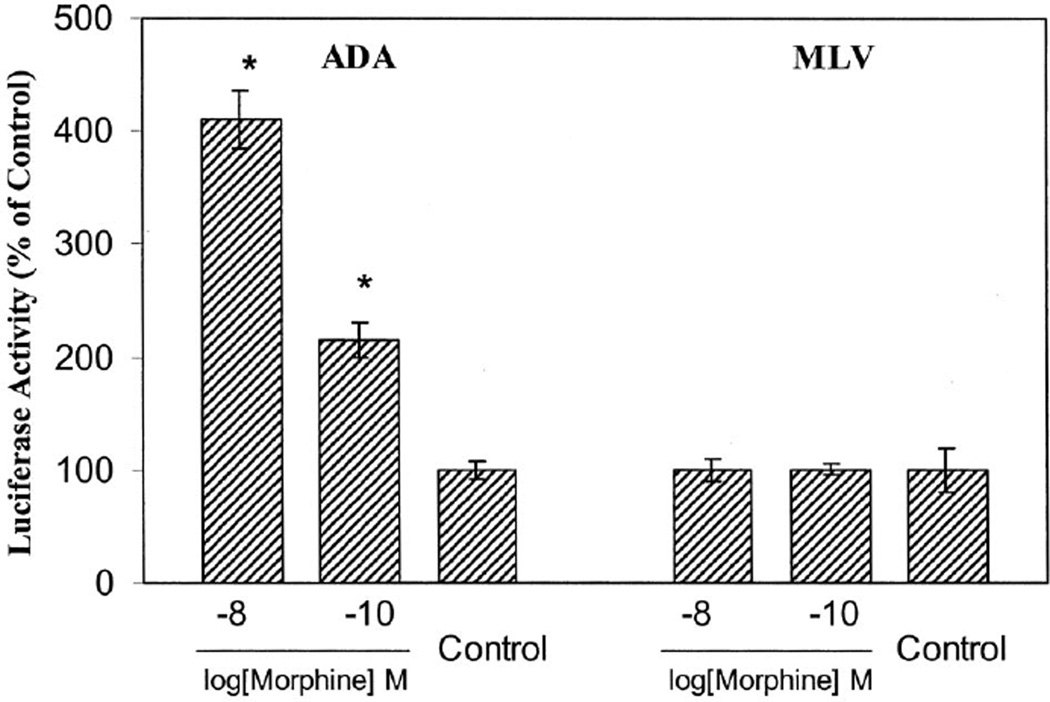
Effect of Morphine on Pseudotyped HIV Infection of MDM
To examine the hypothesis that morphine enhances HIV infection of MDM by affecting viral entry, we examined the effect of morphine on ADA (CCR5-dependent and macrophage-tropic) Env- or MLV (HIV receptor-independent) Env-pseudotyped HIV infection of MDM. This pseudotyped HIV genome that encodes a luciferase reporter gene allows for the quantitative measure of the levels of single-round infection.18 MDM incubated with or without morphine (10−10 M–10−8 M) were infected with recombinant luciferase-encoding HIV particles pseudotyped with ADA Env or MLV Env in the presence of polybrene (4 µg/ml). The cells were lysed and then luciferase activity was determined 72 hours postinfection as described in the Methods section. When infected with the ADA Env-pseudotyped virus, a significant increase (4.1-and 2.1-fold at 10−8 M and 10−10 M, respectively) in luciferase activity was observed in the morphine-treated MDM as compared with the untreated MDM (Fig. 2). Morphine did not affect MLV Env-pseudotyped HIV infection of MDM (Fig. 2), however, confirming that morphine enhances HIV R5 strain infection of MDM by affecting HIV entry.
Figure 2.
Graph illustrating the effect of morphine on pseudotyped HIV infection of MDM. Seven-day-cultured MDM were treated with morphine at the concentrations as indicated for 24 hours and then challenged with recombinant luciferase-encoding HIV pseudotyped with either ADA Env or MLV Env. Luciferase activity was quantitated in the cell lysates 72 hours postinfection. The data are expressed in relative light units as the proportion of morphine-treated cells to controls incubated without morphine. The data demonstrated are mean±SD of triplicate cultures and representative of six experiments. *, p<0.01, morphine vs. control.
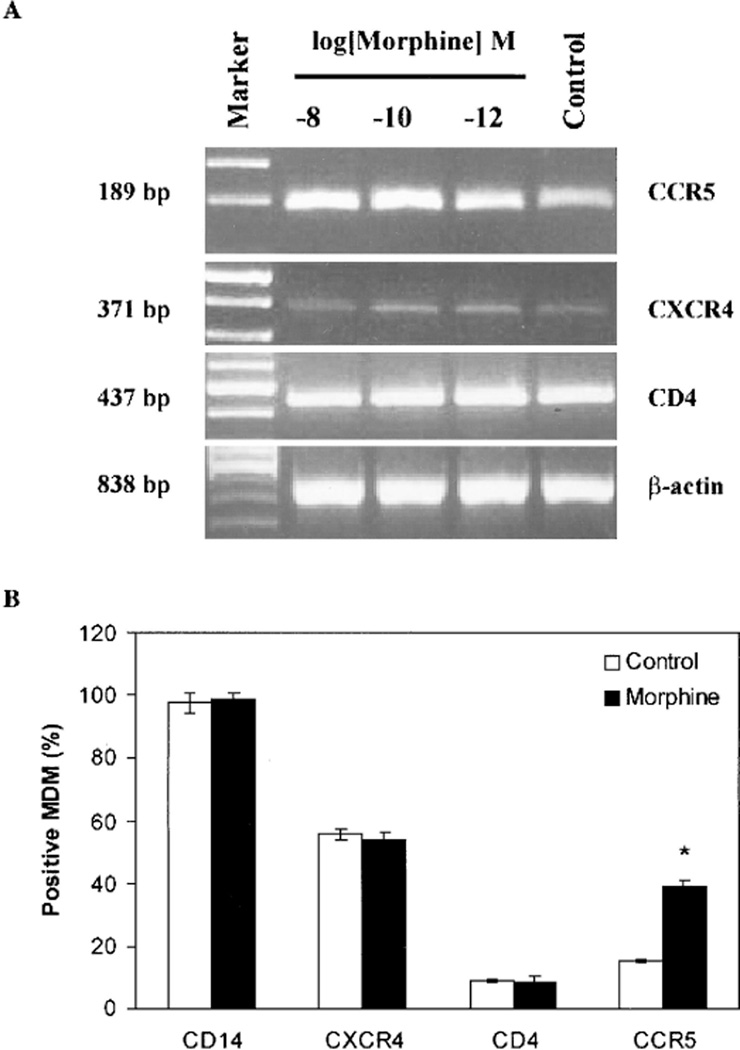
Effect of Morphine on HIV Receptor Expression
We have shown that morphine enhanced the infection of the HIV R5 strains but not the X4 strain. We also have shown that morphine promoted ADA Env-pseudotyped HIV but not MLV Env-pseudotyped HIV infection of MDM. Therefore, we speculated that morphine, through its receptors on MDM, modulates the expression of CCR5 receptor, a primary co-receptor for HIV R5 strain entry into macrophages. We examined the ability of morphine to modulate the expression of HIV receptors on MDM. CCR5 mRNA was upregulated in MDM by morphine (10−12 M–10−8 M) (Fig 3A). CD4 (a primary receptor for HIV) and CXCR4 (a primary co-receptor for HIV X4 strain entry into CD4+ T lymphocytes) mRNA were not affected by the morphine treatment (Fig. 3A). Among the CCR5, CXCR4, and CD4 receptors, only CCR5 receptor expression was upregulated by morphine (Fig 3B). To further determine the specificity of the morphine effect, we also studied the effect of morphine on the CD14 receptor, a marker of monocytes and macrophages. Morphine had no effect on CD14 expression (Fig 3B).
Figure 3.
Effect of morphine on HIV receptor expression in MDM. (A) MDM cultured for 7 days were incubated with or without morphine at the indicated concentrations for 4 hours. Total cellular RNA was extracted from the cell cultures and subjected to RT-PCR using the primer pairs for CCR5, CXCR4, and CD4 receptor genes. Marker, 100 base pair DNA ladder. The amplified PCR products (189 base pairs for CCR5, 371 bp for CXCR4, and 437 bp for CD4) were visualized on an ethidium bromide-stained 3% agarose gel. β-actin was used to monitor the amount and integrity of RNA in each sample. (B) MDM cultured for 7 days were incubated with or without morphine at 10−10 M for 24 hours, and the expression of CCR5, CD4, CXCR4, and CD14 on MDM were determined by performing direct immunofluorescence cytometry. The results shown are the percentages of MDM positive for the receptors analyzed and are representative of four experiments. *, p<0.05, morphine vs. control.
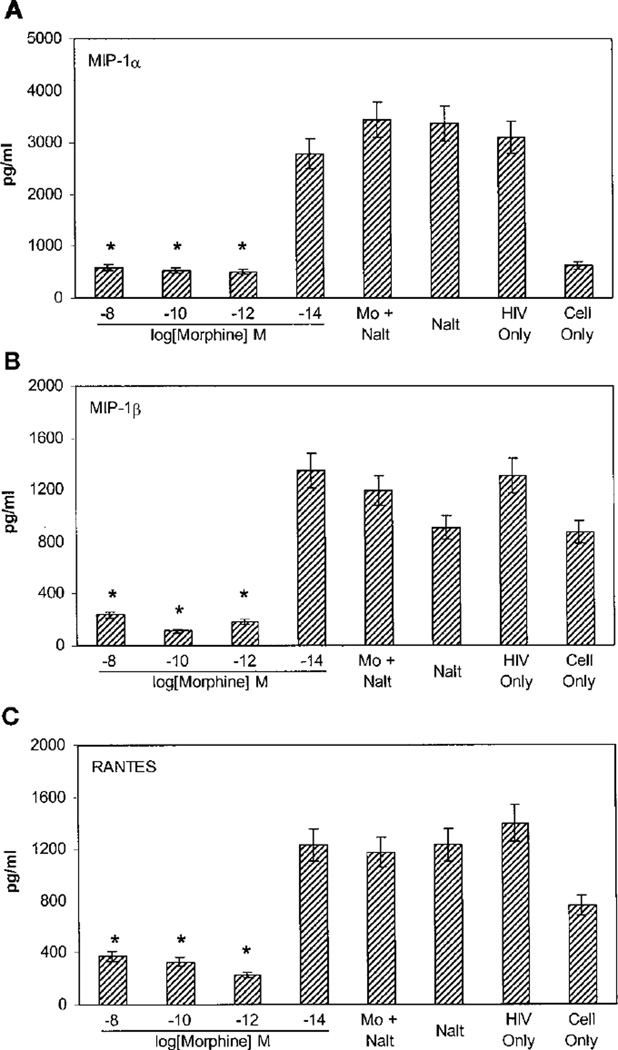
Effect of Morphine on β-Chemokine Production
Because MIP-1α, MIP-1β, and RANTES, the natural ligands for the CCR5 receptor, have been identified as the HIV-suppressive factors,17 we studied whether morphine affected these β-chemokines’ production in HIV-infected MDM. Macrophages cultured for 7 days in 48-well plates were incubated with or without morphine (10−14 M to 10−8 M) and/or naltrexone for 12 hours and then challenged with the HIV Bal strain. Culture supernatants were collected 96 hours postinfection for endogenous production of MIP-1α, MIP-1β, and RANTES and then were analyzed by performing ELISA. Morphine significantly inhibited the production of MIP-1α (81.1, 82.8, and 83.5% of downregulation at 10−8 M, 10−10 M, and 10−12 M, respectively), MIP-1β (81.9, 91.5, and 85.9% of downregulation at 10−8 M, 10−10 M, and 10−12 M, respectively), and RANTES (72.9, 76.4, and 83.5% of downregulation at 10−8 M, 10−10 M, and 10−12 M, respectively) in HIV-infected MDM (Fig 4). Morphine at the concentration of 10−14 M had little effect on β-chemokine production in HIV-infected MDM (Fig 4). In addition, β-chemokine production was upregulated in HIV-infected MDM as compared with uninfected cells (Fig 4). The inhibitory effect of morphine on β-chemokine production was reversed by pretreating MDM with naltrexone, but naltrexone alone had no effect on β-chemokine production (Fig 4).
Figure 4.
Graphs illustrating the effect of morphine on β-chemokine production in infected MDM. MDM cultured for 7 days were incubated with or without morphine and/or naltrexone at the indicated concentrations for 12 hours. The cells were also treated either with morphine (Mo, 10−10 M) and naltrexone (Nalt, 10−8 M) or with naltrexone (Nalt, 10−8 M) only. The cells were then infected with the HIV Bal strain. HIV-infected (HIV only) and uninfected MDM (cell only) were used as controls. Culture supernatants were collected 96 hours postinfection for MIP-1α (A), MIP-1β (B), and RANTES (C) production as determined by performing ELISA. The data shown are presented as the mean±SD of triplicate cultures. *, p<0.05, morphine vs. control; representative of six experiments.
DISCUSSION
Endogenous and exogenous opioids and opiate abuse modulate immune function in both in vitro and in vivo systems,4,22,23 including a variety of effects on macrophages. 23 Evidence for the expression of opiate receptors on immune cells, in particular receptors for morphine and the metabolites of heroin, has further strengthened the link between opiates and the cells of the human immune system. 24,25 Opioid receptors (μ, κ, and δ) as well as non-classic opioid-like receptors are present on cells of the human immune system.26–29 Binding sites for the novel morphine receptor designated μ3 were initially reported to be detectable in human peripheral blood-isolated monocytes. 30 Chao et al31 demonstrated that opioid receptor mRNA was also constitutively expressed in highly purified human microglia. The receptor density in macrophages and other immunocytes containing the μ3 receptor, as well as in the N18 neuroblastoma cell line, is considerably higher than that generally found for classic peptide-sensitive neuronal opioid receptor subtypes. Furthermore, opioid receptors cloned from mRNA isolated from lymphocytes and macrophages are identical to those in the central nervous system.32–34 There is therefore considerable interest in determining whether opiates, through their receptors, compromise the function of the human immune cells that are the primary targets for HIV, thus promoting the rate of progression of HIV infection to AIDS. Opioids promote the growth of HIV in human immune cells in vitro.8–10 Individuals with HIV infection and IDU may have an accelerated rate of progression to AIDS.13,14 Therefore, opioids could play a role as cofactors in immunopathogenesis in people with HIV infection and IDU.
Opiate use induces several potential general mechanisms that may effectively enhance HIV infection.8,35,36 First, direct action on viral replication through interaction with opioid receptors may lead to increased infection. A second possibility involves indirect effects such as the modulation of cytokine or chemokine production as well as the regulation of chemokine receptor (e.g., CCR5) expression. In this study, we analyzed the impact of morphine on HIV infection of human blood-isolated mononuclear phagocytes. Monocytes and macrophages play an important role in HIV infection during all stages of disease. They serve as major target cells, reservoirs, vehicles to other tissues, and transmitters of virus to CD4+ T cells.37 Most important, we explored the potential mechanisms by which morphine may enhance HIV infection of MDM.
Our data strongly support the notion that morphine is a modulator of immunoregulation and has the ability to enhance HIV infection. We demonstrated that morphine significantly enhanced HIV R5 strain infection of human blood MDM (Fig 1), whereas HIV X4 strain and MLV Env-pseudotyped HIV (HIV receptor-independent) were affected little (Figs. 1 and 2). Morphine had a partial effect on HIV dual tropic strain (R5X4) infection of MDM (Fig 1). We also showed that morphine upregulated the expression of the CCR5 receptor (Fig 3), a primary co-receptor for HIV R5 strain infection of macrophages. In addition, we demonstrated that morphine significantly inhibited the production of β-chemokines in HIV-infected MDM (Fig 4). This finding is supported by a recent report in which it was demonstrated that morphine potently inhibited RANTES production by lipopolysaccharide- and interleukin-1β-stimulated microglia cells.38 In contrast, Wetzel et al39 reported that DAMGO (a μ-selective agonist) pretreatment of either activated or naïve peripheral blood mononuclear cells (PBMC) resulted in a significant increase in monocyte chemoattractant protein 1 and RANTES mRNA and protein expression. The observed discrepancies between the observations of Hu et al,38 our group, and Wetzel et al39 may be attributable to differences in the target cells and the different μ-selective agonists used in these studies. For example, we investigated the effect of morphine on HIV infection of purified human blood MDM, and Hu et al38 studied the effect of morphine on human microglial cells. Wetzel et al,39 however, examined the effect of DAMGO on chemokine production by PBMC. To determine whether the modulating effect of morphine on β-chemokine production could be blocked by the opioid receptor antagonist, we incubated MDM with or without naltrexone before morphine treatment. We showed that the effects of morphine on the function of MDM were mediated through the specific opioid receptors because the opioid receptor antagonist naltrexone was able to block these effects. It is highly possible that the specific opioid receptor involved is the μ receptor, because morphine has a high affinity and selectivity for the μ receptor.40–42
One of the possible mechanisms by which morphine potentiates HIV infection of human blood mononuclear phagocytes is that morphine enhances the expression of the CCR5 receptor on MDM (Fig 3) and inhibits the production of endogenous β-chemokines (Fig 4). The increased CCR5 expression induced by morphine cannot be due to the effect of morphine-mediated downregulation of β-chemokines. We demonstrate that morphine induced CCR5 mRNA expression within 4 hours posttreatment (Fig 3). The effect of morphine on β-chemokine mRNA was not observed until 6 hours posttreatment, however (data not shown). Because β-chemokines interfere with HIV infection of MDM by competing for the CCR5 receptor, a primary co-receptor for HIV entry into macrophages, morphine-mediated upregulation of the CCR5 receptor and downregulation of β-chemokine production by MDM are likely to be responsible for the effect of morphine on HIV macrophage-tropic infection of these cells. This hypothesis is further supported by the findings that morphine significantly enhanced the replication of the HIV R5 strains (Bal and BL-4) but not the X4 strain (UG024) (Fig 1) and that only ADA (macrophage-tropic strain) Env-pseudotyped HIV infection of MDM was potentiated by morphine (Fig 2).
Nair et al43 recently reported that cocaine selectively downregulates endogenous MIP-1β secretion and upregulates CCR5 expression by normal PBMC, which suggests a mechanism by which cocaine increases the susceptibility of PBMC to HIV infection. Miyagi et al44 recently showed that morphine induced CCR5 expression in a human T lymphoid cell line (CEMx174). This increased CCR5 expression was correlated with the observation45 that morphine treatment led to the increased susceptibility of the cells to HIV infection. We and other investigators have demonstrated that methadone, a synthetic opiate with pharmacologic properties similar to those of morphine, induces CCR5 expression in human immune cells and promotes HIV infection.11,46 Taken together, our data and data reported by others provide information that is important to the understanding of potential mechanisms by which opiates mediate the immunoregulation of HIV infection.
ACKNOWLEDGMENTS
This work was supported by National Institutes of Health Grants DA 12815 (to W.Z.H.) and MH 49981 (to S.D.D.).
REFERENCES
- 1.Risdahl JM, Khanna KV, Peterson PK, Molitor TW. Opiates and infection. J Neuroimmunol. 1998;83:4–18. doi: 10.1016/s0165-5728(97)00216-6. [DOI] [PubMed] [Google Scholar]
- 2.Alcabes P, Friedland G. Injection drug use and human immunodeficiency virus infection. Clin Infect Dis. 1995;20:1467–1479. doi: 10.1093/clinids/20.6.1467. [DOI] [PubMed] [Google Scholar]
- 3.Nair MP, Schwartz SA, Polasani R, Hou J, Sweet A, Chadha KC. Immunoregulatory effects of morphine on human lymphocytes. Clin Diagn Lab Immunol. 1997;4:127–132. doi: 10.1128/cdli.4.2.127-132.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCarthy L, Wetzel M, Sliker JK, Eisenstein TK, Rogers TJ. Opioids, opioid receptors, and the immune response. Drug Alcohol Depend. 2001;62:111–123. doi: 10.1016/s0376-8716(00)00181-2. [DOI] [PubMed] [Google Scholar]
- 5.Kulkarni-Narla A, Walcheck B, Brown DR. Opioid receptors on bone marrow neutrophils modulate chemotaxis and CD11b/CD18 expression. Eur J Pharmacol. 2001;414:289–294. doi: 10.1016/s0014-2999(01)00727-0. [DOI] [PubMed] [Google Scholar]
- 6.Donahoe RM, Falek A. Neuroimmunomodulation by opiates and other drugs of abuse: Relationship to HIV infection and AIDS. Adv Biochem Psychopharmacol. 1988;44:145–158. [PubMed] [Google Scholar]
- 7.Stefano GB, Scharrer B, Smith EM, Hughes TK, Jr, Magazine HI, Bilfinger TV, Hartman AR, Fricchione GL, Liu Y. Makman MH: Opioid and opiate immunoregulatory processes. Crit Rev Immunol. 1996;16:109–144. doi: 10.1615/critrevimmunol.v16.i2.10. [DOI] [PubMed] [Google Scholar]
- 8.Peterson PK, Sharp BM, Gekker G, Portoghese PS, Sannerud K, Balfour HH., Jr Morphine promotes the growth of HIV-1 in human peripheral blood mononuclear cell cocultures. AIDS. 1990;4:869–873. doi: 10.1097/00002030-199009000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Peterson PK, Gekker G, Hu S, Anderson WR, Kravitz F, Portoghese PS, Balfour HH, Jr, Chao CC. Morphine amplifies HIV-1 expression in chronically infected promonocytes cocultured with human brain cells. J Neuroimmunol. 1994;50:167–175. doi: 10.1016/0165-5728(94)90043-4. [DOI] [PubMed] [Google Scholar]
- 10.Chao CC, Gekker G, Hu S, Sheng WS, Portoghese PS, Peterson PK. Upregulation of HIV-1 expression in cocultures of chronically infected promonocytes and human brain cells by dynorphin. Biochem Pharmacol. 1995;50:715–722. doi: 10.1016/0006-2952(95)00176-z. [DOI] [PubMed] [Google Scholar]
- 11.Li Y, Wang X, Tian S, Guo CJ, Douglas SD, Ho WZ. Methadone enhances human immunodeficiency virus infection of human immune cells. J Infect Dis. 2002;185:118–122. doi: 10.1086/338011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Squinto SP, Mondal D, Block AL, Prakash O. Morphine-induced transactivation of HIV-1 LTR in human neuroblastoma cells. AIDS Res Hum Retroviruses. 1990;6:1163–1168. doi: 10.1089/aid.1990.6.1163. [DOI] [PubMed] [Google Scholar]
- 13.Rothenberg R, Woelfel M, Stoneburner R, Milberg J, Parker R, Truman B. Survival with the acquired immunodeficiency syndrome: Experience with 5833 cases in New York City. N Engl J Med. 1987;317:1297–1302. doi: 10.1056/NEJM198711193172101. [DOI] [PubMed] [Google Scholar]
- 14.Selwyn PA, Alcabes P, Hartel D, Buono D, Schoenbaum EE, Klein RS, Davenny K, Friedland GH. Clinical manifestations and predictors of disease progression in drug users with human immunodeficiency virus infection. N Engl J Med. 1992;327:1697–1703. doi: 10.1056/NEJM199212103272401. [DOI] [PubMed] [Google Scholar]
- 15.Ronald PJ, Robertson JR, Elton RA. Continued drug use and other cofactors for progression to AIDS among injecting drug users. AIDS. 1994;8:339–343. doi: 10.1097/00002030-199403000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Specter S. Drugs of abuse and infectious diseases. J Fla Med Assoc. 1994;81:485–487. [PubMed] [Google Scholar]
- 17.Cocchi F, DeVico AL, Garzino-Demo A, Arya SK, Gallo RC, Lusso P. Identification of RANTES, MIP-1α, and MIP-1β as the major HIV-suppressive factors produced by CD8+ T cells. Science. 1995;270:1811–1815. doi: 10.1126/science.270.5243.1811. [DOI] [PubMed] [Google Scholar]
- 18.Deng H, Liu R, Ellmeier W, Choe S, Unutmaz D, Burkhart M, Di Marzio P, Marmon S, Sutton RE, Hill CM, Davis CB, Peiper SC, Schall TJ, Littman DR, Landau NR. Identification of a major co-receptor for primary isolates of HIV-1. Nature. 1996;381:661–666. doi: 10.1038/381661a0. [DOI] [PubMed] [Google Scholar]
- 19.Hassan NF, Campbell DE, Douglas SD. Purification of human monocytes on gelatin-coated surfaces. J Immunol Methods. 1986;95:273–276. doi: 10.1016/0022-1759(86)90415-1. [DOI] [PubMed] [Google Scholar]
- 20.Berger EA, Doms RW, Fenyo EM, Korber BT, Littman DR, Moore JP, Sattentau QJ, Schuitemaker H, Sodroski J, Weiss RA. A new classification for HIV-1. Nature. 1998;391:240. doi: 10.1038/34571. (letter) [DOI] [PubMed] [Google Scholar]
- 21.Willey RL, Smith DH, Lasky LA, Theodore TS, Earl PL, Moss B, Capon DJ, Martin MA. In vitro mutagenesis identifies a region within the envelope gene of the human immunodeficiency virus that is critical for infectivity. J Virol. 1988;62:139–147. doi: 10.1128/jvi.62.1.139-147.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Donahoe RM, Vlahov D. Opiates as potential cofactors in progression of HIV-1 infections to AIDS. J Neuroimmunol. 1998;83:77–87. doi: 10.1016/s0165-5728(97)00224-5. [DOI] [PubMed] [Google Scholar]
- 23.Eisenstein TK, Hilburger ME. Opioid modulation of immune responses: Effects on phagocyte and lymphoid cell populations. J Neuroimmunol. 1998;83:36–44. doi: 10.1016/s0165-5728(97)00219-1. [DOI] [PubMed] [Google Scholar]
- 24.Madden JJ, Whaley WL, Ketelsen D. Opiate binding sites in the cellular immune system: Expression and regulation. J Neuroimmunol. 1998;83:57–62. doi: 10.1016/s0165-5728(97)00221-x. [DOI] [PubMed] [Google Scholar]
- 25.Sharp BM, Roy S, Bidlack JM. Evidence for opioid receptors on cells involved in host defense and the immune system. J Neuroimmunol. 1998;83:45–56. [PubMed] [Google Scholar]
- 26.Mehrishi JN, Mills IH. Opiate receptors on lymphocytes and platelets in man. Clin Immunol Immunopathol. 1983;27:240–249. doi: 10.1016/0090-1229(83)90074-0. [DOI] [PubMed] [Google Scholar]
- 27.Falke NE, Fischer EG, Martin R. Stereospecific opiate binding in living human polymorphonuclear leucocytes. Cell Biol Int Rep. 1985;9:1041–1047. doi: 10.1016/0309-1651(85)90071-2. [DOI] [PubMed] [Google Scholar]
- 28.Carr DJ, DeCosta BR, Kim CH, Jacobson AE, Guarcello V, Rice KC, Blalock JE. Opioid receptors on cells of the immune system: Evidence for δ- and κ-classes. J Endocrinol. 1989;122:161–168. doi: 10.1677/joe.0.1220161. [DOI] [PubMed] [Google Scholar]
- 29.Carr DJ, DeCosta BR, Jacobson AE, Rice KC, Blalock JE. Enantioselective κ opioid binding sites on the macrophage cell line, P388d1. Life Sci. 1991;49:45–51. doi: 10.1016/0024-3205(91)90578-y. [DOI] [PubMed] [Google Scholar]
- 30.Stefano GB, Digenis A, Spector S, Leung MK, Bilfinger TV, Makman MH, Scharrer B, Abumrad NN. Opiate-like substances in an invertebrate, an opiate receptor on invertebrate and human immunocytes, and a role in immunosuppression. Proc Natl Acad Sci U S A. 1993;90:11099–11103. doi: 10.1073/pnas.90.23.11099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chao CC, Hu S, Shark KB, Sheng WS, Gekker G, Peterson PK. Activation of μ opioid receptors inhibits microglial cell chemotaxis. J Pharmacol Exp Ther. 1997;281:998–1004. [PubMed] [Google Scholar]
- 32.Chuang LF, Chuang TK, Killam KF, Jr, Chuang AJ, Kung HF, Yu L, Chuang RY. δ opioid receptor gene expression in lymphocytes. Biochem Biophys Res Commun. 1994;202:1291–1299. doi: 10.1006/bbrc.1994.2071. [DOI] [PubMed] [Google Scholar]
- 33.Belkowski SM, Zhu J, Liu-Chen LY, Eisenstein TK, Adler MW, Rogers TJ. Sequence of κ-opioid receptor cDNA in the R1.1 thymoma cell line. J Neuroimmunol. 1995;62:113–117. doi: 10.1016/0165-5728(95)00116-j. [DOI] [PubMed] [Google Scholar]
- 34.Sedqi M, Roy S, Ramakrishnan S, Elde R, Loh HH. Complementary DNA cloning of a μ-opioid receptor from rat peritoneal macrophages. Biochem Biophys Res Commun. 1995;209:563–574. doi: 10.1006/bbrc.1995.1538. [DOI] [PubMed] [Google Scholar]
- 35.Donahoe RM. Neuroimmunomodulation by opiates: Relationship to HIV infection and AIDS. Adv Neuroimmunol. 1993;3:31–46. [PubMed] [Google Scholar]
- 36.Chao CC, Gekker G, Hu S, Sheng WS, Shark KB, Bu DF, Archer S, Bidlack JM, Peterson PK. κ opioid receptors in human microglia downregulate human immunodeficiency virus 1 expression. Proc Natl Acad Sci U S A. 1996;93:8051–8056. doi: 10.1073/pnas.93.15.8051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Levy JA. Pathogenesis of human immunodeficiency virus infection. Microbiol Rev. 1993;57:183–289. doi: 10.1128/mr.57.1.183-289.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hu S, Chao CC, Hegg CC, Thayer S, Peterson PK. Morphine inhibits human microglial cell production of, and migration towards, RANTES. J Psychopharmacol (Oxf) 2000;14:238–243. doi: 10.1177/026988110001400307. [DOI] [PubMed] [Google Scholar]
- 39.Wetzel MA, Steele AD, Eisenstein TK, Adler MW, Henderson EE, Rogers TJ. μ-opioid induction of monocyte chemoattractant protein-1, RANTES, and IFN-γ-inducible protein-10 expression in human peripheral blood mononuclear cells. J Immunol. 2000;165:6519–6524. doi: 10.4049/jimmunol.165.11.6519. [DOI] [PubMed] [Google Scholar]
- 40.Herz A. Endogenous opioid systems and alcohol addiction. Psychopharmacology (Berl) 1997;129:99–111. doi: 10.1007/s002130050169. [DOI] [PubMed] [Google Scholar]
- 41.Peterson PK, Molitor TW, Chao CC. The opioid-cytokine connection. J Neuroimmunol. 1998;83:63–69. doi: 10.1016/s0165-5728(97)00222-1. [DOI] [PubMed] [Google Scholar]
- 42.Peterson PK, Gekker G, Hu S, Lokensgard J, Portoghese PS, Chao CC. Endomorphin-1 potentiates HIV-1 expression in human brain cell cultures: Implication of an atypical μ-opioid receptor. Neuropharmacology. 1999;38:273–278. doi: 10.1016/s0028-3908(98)00167-1. [DOI] [PubMed] [Google Scholar]
- 43.Nair MPN, Chadha KC, Hewitt RG, Mahajan S, Sweet A, Schwartz SA. Cocaine differentially modulates chemokine production by mononuclear cells from normal donors and human immunodeficiency virus type 1-infected patients. Clin Diagn Lab Immunol. 2000;7:96–100. doi: 10.1128/cdli.7.1.96-100.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Miyagi T, Chuang LF, Doi RH, Carlos MP, Torres JV, Chuang RY. Morphine induces gene expression of CCR5 in human CEMx174 lymphocytes. J Biol Chem. 2000;275:31305–31310. doi: 10.1074/jbc.M001269200. [DOI] [PubMed] [Google Scholar]
- 45.Chuang LF, Killam KF, Jr, Chuang RY. Increased replication of simian immunodeficiency virus in CEM x174 cells by morphine sulfate. Biochem Biophys Res Commun. 1993;195:1165–1173. doi: 10.1006/bbrc.1993.2167. [DOI] [PubMed] [Google Scholar]
- 46.Suzuki S, Carlos MP, Chuang LF, Torres JV, Doi RH, Chuang RY. Methadone induces CCR5 and promotes AIDS virus infection. FEBS Lett. 2002;519:173–177. doi: 10.1016/s0014-5793(02)02746-1. [DOI] [PubMed] [Google Scholar]