Abstract
We live in a world that is increasingly complex, intense, and stressful. Most people, at some time or other in their lives, can make good use of psychiatry as they map their course and steer their way through it. While this holds true, there also exists a very disturbing trend. No other branch of medicine suffers a similar, constant criticism, scrutiny and quite often downright vehement protest. Even the service users, who have been greatly benefitted, choose to stay mum for fear of stigmatization that may follow if they admit to have undergone therapy.
The onus lies on both, the service users and providers alike, to take the positive contributions of psychiatry to the masses at large.
All of us, especially medical professionals, need to consider our own attitudes and awareness. The recognition that anyone will break down if mental stress is high enough should help free us from a ‘them and us’ attitude.
Reading about people's own experience of mental illness can promote understanding: Examples include a successful actress and a prize-winning author.
For mental health practitioners, enabling service users to influence service development is another strong anti-stigma move. A cognitive behavior therapy approach can help individuals overcome the stigma felt and also cope better with discrimination. Also, we need to stand up against mental health discrimination wherever it is encountered.
Keywords: Criticism, Positive aspects, Psychiatry, Solutions, Stigma
Introduction
We live in a world that is increasingly complex and stressful. Most people, at some time or other in their lives, can make good use of psychiatry as they map their course and steer their way through it.
While this holds true, there also exists a very disturbing trend. Historically, no other branch of medicine has seen a similar and constant barrage of criticism, scrutiny, stigma and even downright vehement protests, as has psychiatry (Burns, 2006[3], Singh, 2007[16], Singh, 2014[18]).
There also exist widespread misconceptions about the therapeutic tools and methods, for example, ECT, which is still looked upon as barbaric; psychotherapy as something mystic; and psychiatric drugs as extremely dangerous (Burns, 2006[3])
An internet search with the word ‘psychiatry’ today yields equally, if not more or less, disparaging articles as the affirmative ones.
While people may flaunt their utilization of latest cutting edge developments in healthcare, they tend to shy away from acknowledging psychiatry, irrespective of the amount of positive impact it may have had on their lives.
There exists a very limited array of people who are aware of, let alone acknowledge, the positive aspects of psychiatry. Even members of the healthcare fraternity are often in the dark.
The criticism
Key criticism of mainstream psychiatry include:
Inappropriate use and overuse of medical concepts and tools to understand the mind and society, including the mis-categorization of normal reactions to extreme situations as psychiatric disorders
Scientifically and/or clinically ill-founded system of categorical diagnoses, which stigmatizes patients
Unwillingness to develop and use objective tests, and lack of precision (Singh, 2013[17])
Unexamined abuse or misuse of power over patients who are too often treated against their will.
The specific definitions of, or criteria for, many of the current psychiatric diagnoses or disorders are vague and arbitrary (Singh, 2007[16], Singh 2013[17]
Relation of power between patients and psychiatrists, as well as the institutional environment, is too often experienced by patients as demeaning and controlling;
Compromise of medical and ethical integrity because of financial and professional links with pharmaceutical companies and insurance companies in countries where these are a considerable force (Moynihan et al., 2006[12])
While not all criticism can be dismissed as ignorant vitriol, a major part of anti-psychiatry movement emanates from misconceptions and half-known facts. The most vigorous critics of psychiatry are often past, unsatisfied service users who tend to place the blame on psychiatry and the psychiatrist.
The stigma
The word stigma referred originally to a mark or brand on Greek slaves, clearly separating them from free men. In common usage, the word signifies a disgrace or defect. This definition, however, is flawed, as it puts the blame on the person stigmatized. Stigma is rampant to such an extent that the successful patients tend to keep mum for fear of social reprisal that may occur (Byrne, 1997[4], Singh, 2007[16], Singh, 2014[18]). It is accepted that stigma plays a negative role at every stage of mental illness — presentation, diagnosis, treatment and outcome (Byrne, 1997[4], Reeder and Pryor, 2008[14], Srivastava et al., 2012a[19], 2012b[20]). Societies have always linked ideas of morality and virtue with health and reason, and early Christian societies tainted madness with images of the demonic, the perverse, the promiscuous and the sinful (Schlosberg, 1993[15]). Service users who are also health professionals report a lot of prejudice from the medical profession. Medical students and doctors agree that psychiatric patients are ‘not easy to like’ (Holmes et al., 2008[7]). Among patients who did not comply with a referral to a psychiatrist, the most frequently mentioned reason was the fear of mental illness stigma, rather than negative expectations about the treatment and its quality (Ben-Noun, 1996[2]).
The stigmatisation of the psychiatrist
Medical students often report overhearing negative, disparaging remarks about psychiatrists by teachers in medical school and during clerkship (Holmes et al., 2008[7]).
Medical students sometimes perceive psychiatrists as more emotionally unstable or neurotic than other health professionals (Moos and Yalom, 1996[11]). Within the medical community, the status of psychiatrists is usually described as low. Some authors suggest that there is a “lack of respect among the medical community” (Fink and Tasman, 1983[6]).
The solutions
It is necessary for both clients (service users) and therapists (service providers) to speak up against the stigma and misconceptions prevalent in society, and not just be content with the fact that they themselves are well informed. The positive contributions need to be conveyed to masses at large and their fears and misconceptions allayed (Singh, 2007[16], Singh, 2014[18]).
One of the goals included in the WPA Action Plan 2008-2011, adopted by the WPA General Assembly, was an improvement of the image of psychiatry and psychiatrists in the eyes of health professionals, the general public, health decision makers and students of health professions (Maj, 2008[10]).
Concerning the stigma towards psychiatric treatment, there is evidence that improving people's knowledge about mental disorders during a “mental health first aid course” improves concordance with generally recommended therapies (Kitchener and Jorm, 2004[8]).
It was found that a presentation given by a psychiatrist on mental health issues for high school students not only improved knowledge about mental health, but also improved help-seeking attitudes and appreciation of psychiatrists, possibly due to greater familiarity (Battaglia et al., 1990[1]).
Changing the depiction of psychiatry in the media is an important prerequisite for changing public opinion, particularly by promoting realistic expectations about treatment modalities and their success (Williams et al., 2001[23])
It has been suggested that mental health professionals as well as patients should be more present in the media, in order to provide a more accurate picture of psychiatric treatments and their consumers (Stuart, 2006[21]). For example, The Royal College of Psychiatrists (UK) ran a 5-year campaign ‘Changing Minds, every family in the land’ (Crisp, 2004[5]). The aim was to reduce the stigma of mental illness through activities such as road shows, local events and a cinema trailer. The Royal College of Psychiatrists also has a network of Divisional Public Education Officers, whose role is to support the local media in presenting accurate information on mental health, writing articles, being a contact point for journalists, writing to complain about discrimination and supporting others in protesting.
Among the healthcare personnel, tackling the negative image of psychiatry should start in medical school and continue in junior doctor training. The interested medical students should have the opportunity to gain more experience in psychiatric internships before pursuing a long-term career in psychiatry (Lambert et al., 2006[9]).
As a national body, the Indian Psychiatric Society should seek to establish and maintain sound working relationships with the media. In collaboration with relevant academic institutions, we should revise the curricula for undergraduate and postgraduate medical training, establish closer links and collaboration with other professional societies, with patient and family associations, and with other organizations that can be involved in the provision of mental health care and rehabilitation of the mentally ill.
As individuals, all of us, especially medical professionals, need to consider our own attitudes and awareness. The recognition that anyone will break down if stress is high enough should help free us from a ‘them and us’ attitude.
Reading about people's own experience of mental illness can promote understanding; examples include a successful actress (Pagett and Swannell, 1997[13]) and a prize-winning author (Styron, 1990[22]). These present a first hand, instead of an analytical, account, which helps a reader connect easily, without any previous knowledge of psychopathology. Experiences like these can go a long way in reducing stigma.
For mental health practitioners, enabling service users to influence service development is another strong anti-stigma move.
We should stand up against mental health discrimination wherever it is encountered. This means challenging people who use disrespectful language or tell a ‘nutter on the bus’ joke. It means being willing to befriend and work with someone who has a history of mental illness.
Most of all it means being honest about our own experiences. We should refrain from sensationalizing or creating an aura around our experiences with patients and should treat them as any other interaction that would occur in the normal wake of life. We should speak up when we experience or see the stigma and prejudice that seems to have penetrated most aspects of mental health care.
Conclusion [See also Figure 1. Flowchart of the paper]
Figure 1.
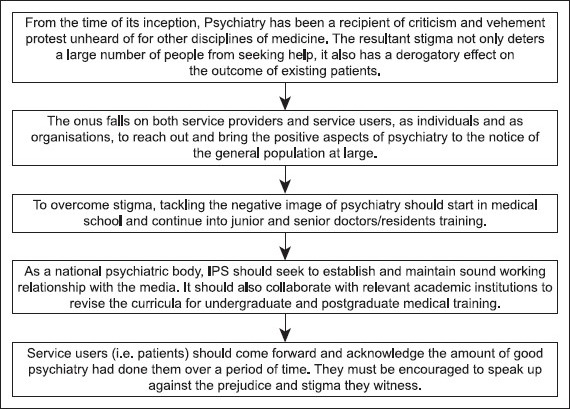
Flowchart of paper
Psychiatry has historically been under attack from various quarters of society due to lack of knowledge and misconceptions.
A largely negative outlook exists among the general public, the media and even the healthcare professionals towards psychiatry, psychiatrists and psychiatric patients
This has over the years kept a large number of patients away from seeking appropriate help while it has also negatively affected the quality of care provided and the quality of life led by the known patients. The need of the hour is to speak up about the positive aspects and the contributions of psychiatry to both the individual and the society at large. This is not a job for the therapist alone; it requires the participation of the other medical professionals, the media, policy makers and most important of all, participation of the service users, i.e. the patients who avail of psychiatric help and derive benefit in their lives, but choose to stay mum due to the fear of prejudice and stigma.
Take home message
The discipline of psychiatry has always been shrouded in mystery and stigma, not only in the eyes of the general public but also the other medical personnel. It is the need of the hour for the psychiatrists, the patients and the medical fraternity in general to bring forward the positive aspects of psychiatry and its role in the improvement in the quality of life of its clients.
Questions that this Paper Raises
What are the main reasons for stigma and prejudice against psychiatric patients and psychiatry in general?
What variations exist, if any, in the outlook of people to psychiatry across various socio economic and educational strata?
What are the major challenges facing the psychiatrists in our region today?
What are the effective steps that could be taken to counter them?
About the Author

U. C. Garg, MD, Consultant Psychiatrist practicing since 1987 at Garg Medical Complex, Agra. India. Has been Immediate past Honorary General Secretary, Indian Psychiatric Society (2010-2011), Secretary General, Indian Asso.of Bio. Psychiatry (2009-2011). President, Indian psychiatric Society, Central Zone (2006), Org. Secretary, National Mid Term CME, Indian Psychiatric Society- 2002 Agra, Org. Secretary, 1st International Conference of SAARC Psychiatric Federation- 2005 Agra.
About the Author

Kabir Garg, MBBS has completed his MBBS from the King George Medical University, Lucknow, India and is currently pursuing his postgraduate degree in psychiatry from the same institute.
Footnotes
Conflict of interest: None declared.
Declaration
This is the authors’ original unpublished work, and has not been submitted for publication elsewhere.
CITATION: Garg UC, Garg K. Speaking to a Wider Audience about the Positive Contributions of Psychiatry. Mens Sana Monogr 2014;12:71-8.
Peer Reviewers for this paper: Anon
References
- 1.Battaglia J, Coverdale JH, Bushong CP. Evaluation of a mental illness awareness week program in public schools. Am J Psychiatry. 1990;147:324–9. doi: 10.1176/ajp.147.3.324. [DOI] [PubMed] [Google Scholar]
- 2.Ben-Noun L. Characterization of patients refusing professional psychiatric treatment in a primary care clinic. Isr J Psychiatry Relat Sci. 1996;33:167–74. [PubMed] [Google Scholar]
- 3.Burns T. Oxford: Oxford University Press; 2006. Psychiatry: A very short introduction. [Google Scholar]
- 4.Byrne P. Psychiatric stigma: Past, passing and to come. J R Soc Med. 1997;90:618–20. doi: 10.1177/014107689709001107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crisp AH, editor. London: Royal Society of Medicine Press; 2004. Every family in the land: Understanding prejudice and discrimination against people with mental illness. [Google Scholar]
- 6.Fink PJ, Tasman A. Stigma and mental illness. The enigma of stigma and its relation to psychiatric education. Psychiatr Ann. 1983;13:669–90. [Google Scholar]
- 7.Holmes D, Tmuuliel-Berhalter LM, Zayas LE. “Bashing” of medical specialities: Student's experiences and recommendation. Fam Med. 2008;40:400–6. [PubMed] [Google Scholar]
- 8.Kitchener BA, Jorm AF. Mental health first aid training in a workplace setting: A randomized controlled trial. BMC Psychiatry. 2004;4:23. doi: 10.1186/1471-244X-4-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lambert TW, Turner G, Fazel S, Goldacre MJ. Reasons why some UK medical graduates who initially choose psychiatry do not pursue it as a long-term career. Psychol Med. 2006;36:679–84. doi: 10.1017/S0033291705007038. [DOI] [PubMed] [Google Scholar]
- 10.Maj M. The WPA Action Plan 2008-2011. World Psychiatry. 2008;7:129–30. doi: 10.1002/j.2051-5545.2011.tb00043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moos RH, Yalom ID. Medical students’ attitudes toward psychiatry and psychiatrists. Ment Hyg. 1966;50:246–56. [PubMed] [Google Scholar]
- 12.Moynihan R, Cassels A. USA: Nation Books; 2006. Selling sickness: How the world's biggest pharmaceutical companies are turning us all into patients. [Google Scholar]
- 13.Pagett N, Swannell G. London: Gollanz; 1997. Diamonds Behind my Eyes. [Google Scholar]
- 14.Reeder GD, Pryor JB. Dual psychological processes underlying public stigma and the implications for reducing stigma. Mens Sana Monogr. 2008;6:175–86. doi: 10.4103/0973-1229.36546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schlosberg A. Psychiatric stigma and mental health professionals (stigmatizers and destigmatizers) Med Law. 1993;12:409–16. [PubMed] [Google Scholar]
- 16.Singh AR. The task before psychiatry today. Indian J Psychiatry. 2007;49:60–5. doi: 10.4103/0019-5545.31521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singh AR. Psychiatry's catch 22, lack of precision, and placing schools in perspective. Mens Sana Monogr. 2013;11:42–58. doi: 10.4103/0973-1229.109304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singh AR. The task before psychiatry today redux: STSPIR. Mens Sana Monogr. 2014;12:35–70. doi: 10.4103/0973-1229.130295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shrivastava A, Johnston M, Bureau Y. Stigma of mental illness-1: Clinical reflections. Mens Sana Monogr. 2012;10:70–84. doi: 10.4103/0973-1229.90181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shrivastava A, Johnston M, Bureau Y. Stigma of Mental Illness-2: Non-compliance and Interventions. Mens Sana Monogr. 2012;10:85–97. doi: 10.4103/0973-1229.90276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stuart H. Review Media portrayal of mental illness and its treatments: What effect does it have on people with mental illness? CNS Drugs. 2006;20:99–106. doi: 10.2165/00023210-200620020-00002. [DOI] [PubMed] [Google Scholar]
- 22.Styron W. New York: Random House; 1990. Darkness Visible: A Memoir of Madness. [Google Scholar]
- 23.Williams A, Cheyne A, Macdonald S. The public's knowledge of psychiatrists: questionnaire survey. Psychiatr Bull. 2001;25:429–32. [Google Scholar]