Abstract
Human behaviour, emotions, and cognition are complex to understand and explain. It is even more difficult to understand the basis for abnormal behaviour, disturbed emotions, and impaired cognitions, something mental health professionals are trying for long. In these pursuits, psychiatry has traversed through eras of humours, witchcraft, spirits, psychoanalysis, and gradually deviated from other medical specialities. Now, with recent biological breakthroughs like advances in psychopharmacology, neuroimaging and genetics, increasingly more emphasis is being given to the biological model of psychiatric disorders.
These new biological models have given a more scientific appearance to the speciality. It has also revolutionised the management strategies and outcome of many psychiatric disorders. However, this rapid development in biological understanding of psychiatry also leads to a new wave of reductionism. In an attempt to deduce everything in terms of neurons, neurochemicals, and genes, can we neglect psychosocial aspects of mental health? Patients’ personality, expectations, motives, family background, sociocultural backgrounds continue to affect mental health no matter how much ‘biological’ psychiatry gets.
Biological and psychosocial approaches are not mutually exclusive but complementary. Integrating them harmoniously is the skill psychiatry demands for comprehensive understanding of mental and behavioural disorders.
Keywords: Aetiology, Biological psychiatry, Psychosocial, Reductionist approach
Introduction
Controversies are not new to psychiatry. In fact controversies have been constant companions of this speciality, only the areas of controversy change. Conceptual controversies bring dilemmas in clinical practice. One such controversy today's psychiatrist faces is — whether to embark on the new, reductionist “pure biological” attitude, or stick to the age-old “psychosocial” approach.
The journey of psychiatry dates back to 460 BC, when Hippocrates gave the concept of humours. Middle Ages heralded the concept that supernatural forces lead to mental illness; and witchcraft was blamed during the Renaissance (Colp, 2009[8]). Path breaking work on “Psychoanalysis” by Sigmund Freud added a new dimension to psychiatry, and by 1960 psychoanalytically oriented psychiatry had become the prevailing model for understanding mental illness (Grebb and Carlson, 2009[16]).
It was in the last few decades that psychiatry witnessed major biological breakthroughs in the form of effective psychopharmacology, genetics, and advanced neuro-imaging, questioning the credibility of the psychosocial approach. In an influential paper published in 1998, Eric Kandel outlined the beginning of a new intellectual framework for psychiatry that emphasised the neurobiological basis of the brain-mind relation (Kandel, 1998[21]). Together with advances in genetics, this helped to establish biological psychiatry as the model for diagnosing and treating disorders of the mind. This development is hoped to improve treatment options and eliminate the stigma attached to mental disorders (Glannon, 2008[14]). It is also hoped that this new neurobiological dimension attracts more talented, young medical graduates towards psychiatry.
The question, however, remains: Is psychiatry only about neurons and neuronal messengers?
Psychiatry is unique amongst the medical specialities, for it deals with the constant interplay of brain, mind and body with each other and with the external milieu. ‘… though (the psychiatrist) makes common cause with medicine on the one hand – considering, genetic, constitutional, biochemical, and other physical influences – he has perchance to consider as well, sociological, cultural and cross-cultural, environmental, theological and mythical phenomena, and he utilises his psychological frame of reference to explain these’ (Singh and Singh, 2004[38]). Psychiatrist cannot just treat the brain but the whole person, his conflicts, both internal and external, and the faulty interplay between him and his environment. Particularly, culture continues to exert its effect on all aspects of mental illness from patient-doctor relationship to the treatment outcome.
In this review we will try to find an answer to the question that agitates today's psychiatrists: Which approach to follow?
The “synaptic self”: The biological breakthroughs and their implications
Insight into the relation between functional alteration in neuronal circuits and behavioural abnormalities was obtained with the introduction of effective psychotropics like lithium, imipramine and haloperidol in the 1950s. Further researches lead to more effective and tolerable alternatives. But the growth of biological psychiatry was slow due to the complexity of the human brain (Grebb and Carlson, 2009[16]), lack of interest on the part of researchers, and lack of technological aids.
Eric Kandel, recipient of Noble prize for his work on the neurophysiology of memory, published his much known paper in 1998. This paper successfully tried to re-establish the neurobiological dimension of psychiatry which was neglected for decades by the then dominant psychodynamically oriented psychiatrists (Kandel, 1998[21]). He summarised his “new intellectual framework” using five principles which are explained below with supporting research data wherever available.
All mental processes derive from operations of the brain: The action of brain underlies all voluntary processes from simple eating to complex cognitive actions such as thinking, speaking, etc. All social actions have biological underpinning. Hence, behavioural disorders are due to disturbance in the brain.
-
Genes can contribute importantly to mental function and can contribute to mental illness: Genes code for protein either structural or functional. These proteins aid in the development, regulation, and maintenance of neural circuits which in turn determine behaviour. This concept is supported by twin studies. Compared to controls, monozygotic twins separated early in life and raised in different environments have been shown to share remarkable number of behavioural traits like taste, religious preference, and vocational interests that are considered to be socially determined and distinctive features of a person (Kandel, 1998[21]). A meta-analysis of twin studies in schizophrenia concluded that schizophrenia has 81% heritability (Sullivan et al., 2003[41]) and a recent review of twin studies in major depression estimated a heritability of 37% (Lohoff, 2010[27]).
At the same time, many environmental factors like obstetric complications, parental age, and cerebral hypoxia have also been shown to have strong aetiological role in schizophrenia, stressing the importance of the early environment in determining behaviour (Gejman et al., 2010[13]). The fact that concordance rate for none of the psychiatric illness is 100% also supports role of the environment.
Behaviour itself can modify gene expressions: Research has shown that development, stress, and social experience affect the gene expression by modifying the binding of transcriptional regulators to each other and to regulatory regions of the genes (Kandel, 1998[21]; Roth and Sweatt, 2011[34]). It is also proposed that some neurotic illnesses result from reversible defects in gene regulation (Kandel, 1998[21]).
Maintenance of learned alterations in gene expressions by structural alterations in neural circuits of brain: Studies have shown that maps of somatic sensory cortex are not similar in all animals. Moreover within an individual, these maps are dynamic and change depending upon the use and disuse of a specific organ. Monkeys, which were encouraged to use only three fingers to handle food at the cost of other two fingers, showed overdeveloped brain areas corresponding to those three fingers at the cost of region representing the other two fingers (Jenkins et al., 1990[19]). A recent study reported a large-scale reorganisation of somatosensory cortex and thalamus in monkeys with surgical lesions of dorsal column at cervical region, with the expansion of face representation into the areas corresponding to hands (Jain et al., 2008[18]). Since each of us has grown up in different environments, exposed to different combination of stimuli and developed motor skills in different ways, our brains are modified in unique ways. Along with unique genetic makeup, this constitutes the biological basis for individuality (Kandel, 1998[21]).
Psychotherapy and pharmacotherapy may induce alterations in gene expression and structural changes in brain: Research has revealed that behavioural therapy in neurotic disorders lead to changes in the brain (Feinstein et al., 2010[10]). An example is Obsessive Compulsive Disorder (OCD). In patients of OCD, functional hyperactivity of head of the right caudate nucleus is observed. After successful treatment of OCD, with either SSRI alone or behavioural therapy alone, there was substantial decrease in the activity of head of the right caudate nucleus among treatment responders compared to non-responders (Schwartz et al., 1996[35]; Linden, 2008[25]). Researchers have reported decrease in prefrontal lobe activity after interpersonal therapy and antidepressant medication in depressed patients (Martin et al., 2001[29]), and normalised frontal lobe metabolism after successful Cognitive Behaviour Therapy in patients of specific phobia (Paquette et al., 2003[33]).
A recent meta-analysis on the neural correlates of psychotherapy concluded that findings of studies in anxiety and depression report changes in the dorsomedial prefrontal cortex and in the posterior cingulated gyrus/precuneus, and some changes in temporal lobes (Messina et al., 2013[31]).
Neuroimaging of psychiatric disorders is another recent development which has generated the hope of better diagnostic and therapeutic options in future. Though not consistent, studies have come up with some preliminary observations like decreased volume of prefrontal, anterior temporal, and perisylvian regions, and of the anteromedial thalamus in Magnetic Resonance Images (MRI), and abnormal activation in the prefrontal and cingulate cortex and the medial temporal lobe in Functional MRI (fMRI) of schizophrenic patients (Masdeu, 2011[30]). Patients of major depressive disorder are found to have elevated metabolism and reduced volume of subgenual region of the medial frontal lobe (Masdeu, 2011[30]).
Hence, advances in psychopharmacology have opened new avenue for understanding behaviour in terms of circuits, neurons, synapses, and neurotransmitters. With genetics and functional image techniques, strengthening the hope of explaining mental phenomenon in pure biologist's language has emerged the reductionist approach — “we are nothing but our brain” (Glannon, 2009[15]).
This biological framework has its own implications. On one hand it demands, from today's psychiatrists, a thorough knowledge of structure and functions of brain; on the other hand, it brings more scientific and rational outlook to the speciality of psychiatry. This scientific outlook is expected to attract more talented medical students into the field of psychiatry, as currently many of them believe that Psychiatry is unscientific and imprecise (Lingeswaran, 2010[26]). Also precision and clarity in diagnostic and investigative techniques in the branch is the way forward, which promise the biological framework alone holds at present (Singh, 2013[37]). As far as patients are concerned, biological breakthroughs improve the diagnostic and therapeutic armamentarium. It reduces the stigma associated with psychiatric disorders by discarding the concept of “all in the mind”. It also helps to reduce the guilt that the patient himself is responsible for the behavioural disorder, and increases treatment acceptance.
But are we just our brains? Are all complex brain functions, like interpersonal and social interactions, reducible to neurobiological phenomenon?
Treat the brain, attend to the sick: Psychosocial insight and its implications
Social psychiatry was at its peak during the 1960s and 1970s, when mental health care shifted from the asylum to community-based hospitals. Since then, with focus shifting towards neurobiology, it is being gradually neglected, raising concern about the future of social psychiatry. But social psychiatrists have reasons to believe that obituaries to the branch are premature, and are hopeful of a change in attitude. In fact, if advances in our understanding of the human genome and the brain have told us anything, it is the degree to which the external environment has impact on what is a flexible and adaptive biological system (Bhugra and Morgan, 2010[3]). Leon Eisenberg (Eisenberg, 2004[9]) notes:’. . . social psychiatry . . . is alive and well precisely because of genomics’.
In following sections we try to reinforce some basic concepts of social psychiatry and to justify why the psychosocial model can never be obsolete in clinical practice.
-
Each patient is different: Biological reductionist model asks the clinician to know ‘what the patient is?’ — is it a case of moderate depression, or social phobia, or chronic alcohol dependence? It does not attempt to understand ‘who the patient is?’ — what is his temperament, his beliefs, wishes and drives? In contrast, research shows that each patient is different and exerts his/her own impact on treatment. Patients of depression with neuroticism and sociotropy are shown to have poor pharmacotherapy outcome in contrast to patients with autonomy (Mintz and Flynn, 2012[32]). Patients with secure attachments show earlier response to antidepressants than those with fearful attachments (Mintz and Flynn, 2012[32]).
Patients’ expectations also matter. Patients who expect more from pharmacotherapy are more likely to be benefitted from it. Study enrolled patients who know they are getting placebo show less response compared to those who know they are receiving antidepressants (Mintz and Flynn, 2012[32]).
These issues are of practical importance as knowing and correcting patients’ beliefs and trying to neutralise faulty attachment styles by effective communication can improve clinical outcome (Mintz and Flynn, 2012[32]).
-
Family and its role in mental health: Family play an important role in mental health and ill health. A beautiful example is a traditional Indian family. Indian joint families are tolerant of deviant behaviour and allow diffusion of burden of care which can lead to good course and outcome of major mental disorder (Avasthi, 2010[2]). This is a possible reason for better outcome in some countries, including India, in studies like International Pilot Study of Schizophrenia (IPSS) and Determinants of Outcome of Severe Mental Disorders (DOSMED) (Kulhara and Chakrabarti, 2001[24]).
In countries like India, the family forms a circle of intimacy and is almost inseparable from the individual. Hence considering managing the patients of mental illness without involving family is impossible. With current status of poor mental health resources and infrastructure, family holds a greater responsibility in mental health care than the government.
Family also can have negative impact on mental health. Families with critical attitude towards patient and expressed emotions have shown to be associated with poor treatment outcome (Butzlaff and Hooley, 1998[5]; Heru, 2006[17]). Maladaptive parental behaviour and child abuse is associated with increased psychiatric problems (Johnson et al., 2001[20]). Burden of care is another area that needs to be addressed in all cases.
Hence it is also important to consider family dynamics, apart from clinical features and individual characteristics of the patient, for effective treatment of psychiatric disorders.
Culture and mental health: Culture, in simple terms, is the way of life. Culture influences the behaviour of its members and also determines boundary between normal and abnormal behaviour. Hence diagnosis in psychiatry cannot remain uninfluenced by the interviewer and client's socio-cultural beliefs and interpretations.
Culture is known to play a vital role in the personality characters, coping strategies, epidemiology, clinical presentation, treatment seeking behaviour, choice of treatment and treatment outcome of an illness (Avasthi, 2011[1]). Persons of different culture have different basic personality characters. Compared to westerners, Indians prefer interdependence rather than independence. Indian self is lodged in ‘circle of intimacy’ or family. With such close ties, Indians can communicate freely, they have less fear of rejection and they get emotional support without considering it as charity (Avasthi, 2011[1]).
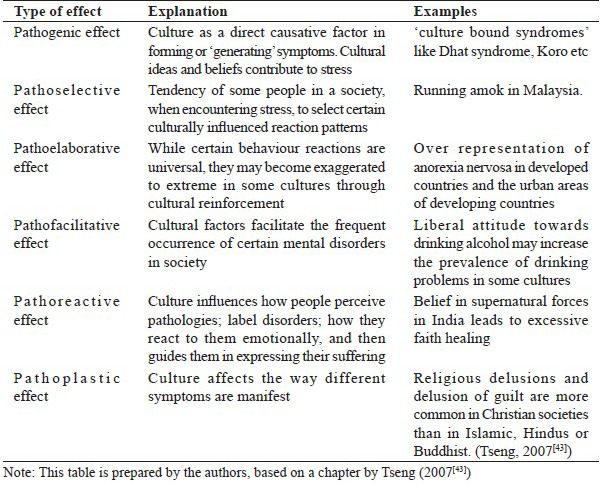
Culture affects the psychopathology in various ways [Table 1].
Table 1.
Effect of culture on psychopathology
Clinical presentations of mental illness differ across cultures. In psychotic illnesses, delusions and hallucinations are often coloured by culture in terms of paranormal phenomenon (Kulhara et al., 2000[23]). In affective disorders, Indian depressive patients, for example, tend to have more somatic symptoms, as this is a culturally accepted manifestation of psychic stress, and also associated with unconscious desire to undermine the psychic distress (Teja et al., 1971[42]; Avasthi, 2011[1]). Guilt is rare in eastern compared to western patients of depression (Teja et al., 1971[42], Avasthi, 2011[1]). Manic episodes are more frequent than depressive and they are short lasting in Indian patients (Chopra, 2006[7]). In neurotic disorders, trance and possession states are more common in Indian patients than multiple personality, dissociative amnesia, and fugue (Chaturvedi, 1993[6]; Avasthi, 2011[1]).
These differences cannot be explained by neurons, neurotransmitters or circuits. Considering the cultural background of the patients is an essential clinical skill, as culture also determines what sort of treatment in more acceptable, pharmacotherapy or psychotherapy.
For example, in the Indian set up, the physical concept of mental illness prevalent among Indian patients leads to an expectation that the therapist would follow a ‘medical’ rather than ‘psychological’ approach towards the management of their problems. The Indian patient expects the therapist to play an active and authoritarian role, making the maintenance of “therapeutic neutrality” difficult (Sethi and Trivedi, 1982[36]; Manickam, 2010[28]). During psychotherapeutic interventions, Indian psychiatrist is expected to play a more active role, with use of suggestions, sympathetic manipulation of the environment along with teaching and reassurance in most cases. Hence, psychotherapy in India should be short, crisis oriented, supportive, flexible, eclectic, and tuned to cultural and social conditions (Sethi and Trivedi, 1982[36]; Manickam, 2010[28]).
From the above discussion, it is apparent that psychosocial model is as important as the biological framework. One cannot only treat the brain but should consider the personal, interpersonal, and social factors, and their interplay, in order to provide a holistic therapeutic benefit.
Moreover, psychosocial approaches can inspire more biological breakthroughs. As Freud expressed, psychoanalytic principles, which he accepted as provisional, would be more convincing if they had neurobiological explanations (Freud, 1987[11]; Singh and Singh, 2004[38]; Brockman, 2011[4]). Hence researches in this direction are welcome. Kendal hopes that the new branch of cognitive neuroscience can, hopefully, give a more research based, biological, dimension to psychotherapies, including psychoanalysis (Kandel, 1999[22]). He further lists eight areas in which neurobiology could join with psychoanalysis to make important contributions:
The nature of unconscious mental processes;
The nature of psychological causality;
Psychological causality and psychopathology;
Early experience and the predisposition to mental illness;
The preconscious, the unconscious, and the prefrontal cortex;
Sexual orientation;
Psychotherapy and structural changes in the brain; and 8) psychopharmacology as an adjunct to psychoanalysis (Kandel, 1999[22]; Singh and Singh, 2004[38]; Brockman, 2011[4]).
Conclusion [See also Figure 1: Flowchart of the paper]
Figure 1.
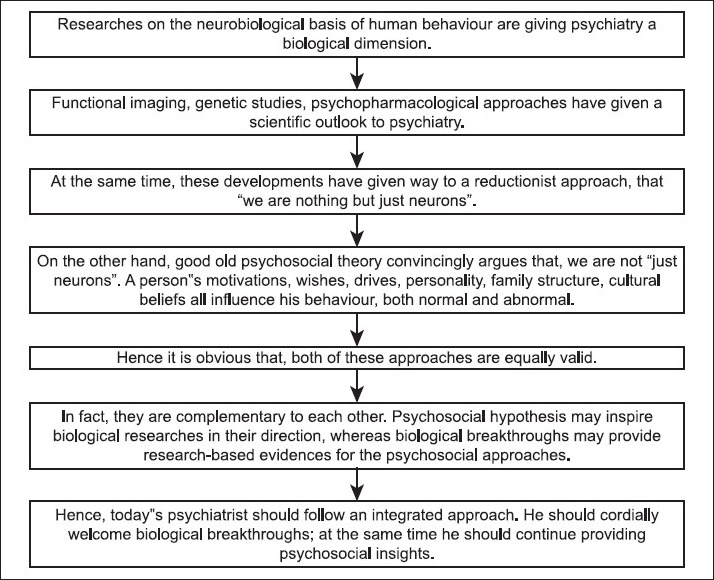
Flowchart of paper
Today psychiatry is at a position where both biological and psychosocial models of mental illness are equally valid and essential, and collaborative approach is warranted rather than an exclusivist one. Psychiatrists should understand the positive and negative aspects of both approaches. These are not mutually exclusive but complementary, and integrating them is a necessity (Singh, 2007[39]; Singh, 2014[40]). Accepting the biological breakthroughs enthusiastically and, at the same time, nurturing the zeal to provide psychosocial insight is what we need to incorporate in our researches, our day-to-day clinical practice for the benefit of our patients, in ourselves, and in the field of psychiatry.
To quote Gabbard:
Just as physicist must simultaneously think in terms of particles and waves, the psychiatrist must speak of motives, wishes and meanings in the same breath as genes, neurochemistry and pharmacokinetics. (Gabbard, 1999[12])
Take home message
Psychiatry today is at a juncture where a new, strong biological dimension is being added to an already existing psychosocial approach.
This is a welcome change, as it gives more evidence-based approaches and a scientific outlook.
However, that doesn't mean the psychosocial model is no more relevant.
Psychiatrists of today should be comfortable with both approaches, as they are mutually complementary.
Questions that this Paper Raises
With advances in biological research and greater inclination of psychiatrists towards psychopharmacology, will psychiatry lose its psychosocial
dimension?
How can biological breakthroughs become a boon rather than a bane for those who advocate a psychosocial approach?
Will these two apparently antagonistic approaches work together in a complementary manner to make Psychiatry a more holistic speciality?
How should a psychiatrist, working in the clinic and the community, incorporate these two approaches in a judicious manner in his day-to-day practice?
About the Author

Bheemsain Tekkalaki MD finished his post-graduation in Psychiatry from King George Medical University Lucknow, in the year 2013. He is currently working as Assistant Professor of Psychiatry at Navodaya Medical College, Raichur, Karnataka, India. His areas of interest are Cognitive Behavioural Therapy, Consultation Liaison Psychiatry and Culture and Psychiatry. He has three publications in National/International Journals.
About the Author

Adarsh Tripathi MD is currently working as an Assistant Professor of Psychiatry at the King George's Medical University, Lucknow, India. He has more than 30 national and international publications and four book chapters to his credit and has worked in several international and national researches of repute. His areas of interest include Addictions, Bipolar Disorder, Cognition, Human Sexuality, Adult ADHD and Psychopharmacology.
About the Author
Late Jitendra Kumar Trivedi was a Professor in the Department of Psychiatry, King George Medical University, Lucknow, India. He was a member of The Royal College of Psychiatrists, U.K. since 2005. He was the Fellow member of the American Psychiatric Association since 2007, and nominated Honorary Member of the World Psychiatric Association in 2008, and Fellow of the National Academy of Medical Sciences. He was a principal investigator for more than 25 multinational clinical trials as well as ICMR and WHO sponsored projects. He had around 260 publications in national and international Journals as well as chapters in books. He had been an Editor, in the Indian Journal of Psychiatry, President of the Indian Psychiatric Society, and a Zonal Representative for Southern Asia - Zone-XVI of the World Psychiatric Association. At the time of his demise, he was President-Elect of Indian Association for Social Psychiatry, member of Executive Council of Preventive Psychiatry Section of World Psychiatric Association and Chairman- Preventive Psychiatry Section of World Association of Social Psychiatry.
Footnotes
Conflict of interest: None declared.
Declaration
This article is our original unpublished work, not submitted for publication elsewhere.
CITATION: Tekkalaki B, Tripathi A, Trivedi JK. Welcome Biological Breakthroughs, Supply Psychosocial Insights. Mens Sana Monogr 2014;12:79-91.
Peer Reviewers for this paper: Anon
References
- 1.Avasthi A. Indianizing Psychiatry-Is there a case enough? Indian J Psychiatry. 2011;53:111–20. doi: 10.4103/0019-5545.82534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Avasthi A. Preserve and strengthen family to promote mental health. Indian J Psychiatry. 2010;52:113–26. doi: 10.4103/0019-5545.64582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhugra D, Morgan C. Social psychiatry: Alive and kicking. In: Morgan C, Bhugra D, editors. Principles of Social Psychiatry. USA: Wiley-Blackwell; 2010. pp. 15–6. [Google Scholar]
- 4.Brockman R. Aspects of psychodynamic neuropsychiatry II: psychosocial locality and biology: Toward the neurobiology of psychotherapy. J Am Acad Psychoanal Dyn Psychiatry. 2011;39:285–311. doi: 10.1521/jaap.2011.39.2.285. [DOI] [PubMed] [Google Scholar]
- 5.Butzlaff RL, Hooley JM. Expressed emotion and psychiatric relapse. Arch Gen Psychiatry. 1998;55:547–52. doi: 10.1001/archpsyc.55.6.547. [DOI] [PubMed] [Google Scholar]
- 6.Chaturvedi SK. Neurosis across the cultures. Int Rev Psychiatry. 1993;5:179–91. [Google Scholar]
- 7.Chopra MP, Kishore Kumar KV, Subbakrishna DK, Jain S, Murthy RS. The course of bipolar disorder in rural India. Indian J Psychiatry. 2006;48:254–7. doi: 10.4103/0019-5545.31559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Colp R., Jr . History of psychiatry. In: Sadock BJ, Sadock VA, Pedro R, editors. Kaplan & Sadock's Comprehensive Text Book of Psychiatry. Philadelphia, US: Lippincott Williams & Wilkins; 2009. pp. 4474–509. [Google Scholar]
- 9.Eisenberg L. Social psychiatry and the human genome: Contextualising heritability. Br J Psychiatry. 2004;184:101–3. doi: 10.1192/bjp.184.2.101. [DOI] [PubMed] [Google Scholar]
- 10.Feinstein D, Church D. Modulating gene expression through psychotherapy: Contribution of noninvasive somatic interventions. Rev Gen Psychol. 2010;14:283–95. [Google Scholar]
- 11.Freud S. On Narcissism: An Introduction. On Metapsychology. The Theory Of Psychoanalysis. In: Stratchey J, editor. Pelican Books 1984. Reprinted Harmondsworth: Penguin Books; 1987. p. 67. [Google Scholar]
- 12.Gabbard GO. Mind and brain in psychiatric treatment. In: Gabbard GO, editor. Treatments of psychiatric disorders. Vol. 1. New Delhi, India: Jaypee Bros; 1999. pp. 22–34. [Google Scholar]
- 13.Gejman PV, Sanders AR, Duan J. The role of genetics in the etiology of schizophrenia. Psychiatr Clin N Am. 2010;33:35–56. doi: 10.1016/j.psc.2009.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glannon W. The blessing and burden of biological psychiatry. JEMH. 2008;3(2):1–4. [Google Scholar]
- 15.Glennon W. Our brains are not us. Bioethics. 2009;22:321–9. doi: 10.1111/j.1467-8519.2009.01727.x. [DOI] [PubMed] [Google Scholar]
- 16.Grebb JA, Carlsonn A. introduction and considerations for brain based diagnostic system in psychiatry. In: Sadock BJ, Sadock VA, Pedro R, editors. Kaplan & Sadock's Comprehensive Text Book of Psychiatry. Philadelphia, US: Lippincott Williams & Wilkins; 2009. pp. 1–6. [Google Scholar]
- 17.Heru AM. Family psychiatry: From research to practice. Am J Psychiatry. 2006;163:962–8. doi: 10.1176/ajp.2006.163.6.962. [DOI] [PubMed] [Google Scholar]
- 18.Jain N, Qi HX, Collins CE, Kaas JH. Large-scale reorganization in the somatosensory cortex and thalamus after sensory loss in macaque monkeys. J Neurosci. 2008;28:11042–60. doi: 10.1523/JNEUROSCI.2334-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jenkins WM, Merzenich MM, Ochs MT, Allard R, Guic-Robles E. Functional reorganization of primary somatosensory cortex in adult owl monkeys after behaviorally controlled tactile stimulation. J Neurophysiol. 1990;63:82–104. doi: 10.1152/jn.1990.63.1.82. [DOI] [PubMed] [Google Scholar]
- 20.Johnson JG, Cohen P, Kasen S, Smailes E, Brook JS. Association of maladaptive parental behaviour with psychiatric disorder among parents and their offspring. Arch Gen Psychiatry. 2001;58:453–60. doi: 10.1001/archpsyc.58.5.453. [DOI] [PubMed] [Google Scholar]
- 21.Kandel ER. A new intellectual framework of psychiatry. Am J Psychiatry. 1998;155:457–69. doi: 10.1176/ajp.155.4.457. [DOI] [PubMed] [Google Scholar]
- 22.Kandel ER. Biology and the future of psychoanalysis: A new intellectual framework for psychiatry revisited. Am J Psychiatry. 1999;156:505–24. doi: 10.1176/ajp.156.4.505. [DOI] [PubMed] [Google Scholar]
- 23.Kulhara P, Avasthi A, Sharma A. Magico-religious beliefs in schizophrenia: A study from North India. Psychopathology. 2000;33:62–8. doi: 10.1159/000029122. [DOI] [PubMed] [Google Scholar]
- 24.Kulhara P, Chakrabarti S. Culture and Schizophrenia and other psychotic disorders. Psychiatr Clin North Am. 2001;24:449–64. doi: 10.1016/s0193-953x(05)70240-9. [DOI] [PubMed] [Google Scholar]
- 25.Linden D. Brain imaging and psychotherapy: Methodological considerations and practical implications. Eur Arch Psychiatry Clin Neurosci. 2008;258(Suppl 5):S71–5. doi: 10.1007/s00406-008-5023-1. [DOI] [PubMed] [Google Scholar]
- 26.Lingeswaran A. Psychiatric curriculum and its impact on the attitude of Indian undergraduate medical students and interns. Indian J Psychol Med. 2010;32:119–27. doi: 10.4103/0253-7176.78509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lohoff FW. Overview of the genetics of major depressive disorder. Curr Psychiatry Rep. 2010;12:539–46. doi: 10.1007/s11920-010-0150-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Manickam L. Psychotherapy in India. Indian J Psychiatry. 2010;52:366–70. doi: 10.4103/0019-5545.69270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martin SD, Martin E, Rai SS, Richardson MA, Royall R. Brain blood flow changes in depressed patients treated with interpersonal psychotherapy or venlafaxine hydrochloride: Preliminary findings. Arch Gen Psychiatry. 2001;58:641–8. doi: 10.1001/archpsyc.58.7.641. [DOI] [PubMed] [Google Scholar]
- 30.Masdeu JC. Neuroimaging in psychiatric disorders. Neurotherapeutics. 2011;8:93–102. doi: 10.1007/s13311-010-0006-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Messina I, Sambin M, Palmieri A, Viviani R. Neural correlates of psychotherapy in anxiety and depression: A meta-analysis. PLoS One. 2013;8:e74657. doi: 10.1371/journal.pone.0074657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mintz DL, Flynn DF. How (Not what) to prescribe: Non pharmacological aspects of pharmacology. Psychiatr Clin North Am. 2012;35:143–64. doi: 10.1016/j.psc.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 33.Paquette V, Lévesque J, Mensour B, Leurox JM, Beaudoin G, Bourgouin P, et al. ’Change the mind and you change the brain’: Effects of cognitive-behavioral therapy on the neural correlates of spider phobia. NeuroImage. 2003;18:401–9. doi: 10.1016/s1053-8119(02)00030-7. [DOI] [PubMed] [Google Scholar]
- 34.Roth TL, Sweatt JD. Epigenetic mechanisms and environmental shaping of the brain during sensitive periods of development. J Child Psychol Psychiatry. 2011;52:398–408. doi: 10.1111/j.1469-7610.2010.02282.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schwartz JM, Stoessel PW, Baxter LR, Martin KM, Phelps ME. Systematic changes in cerebral glucose metabolic rate after successful behavior modification treatment of obsessive-compulsive disorders. Arch Gen Psychiatry. 1996;53:109–13. doi: 10.1001/archpsyc.1996.01830020023004. [DOI] [PubMed] [Google Scholar]
- 36.Sethi BB, Trivedi JK. Psychotherapy for the economically less privileged classes (with special reference to India) Indian J Psychiatry. 1982;24:318–21. [PMC free article] [PubMed] [Google Scholar]
- 37.Singh AR. Psychiatry's catch 22, need for precision, and placing schools in perspective (Editorial) Mens Sana Monogr. 2013;11:42–58. doi: 10.4103/0973-1229.109304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Singh AR, Singh SA. Resolution of the polarisation of ideologies and approaches in psychiatry. Mens Sana Monogr 2004. 2005;2:1–32. [PMC free article] [PubMed] [Google Scholar]
- 39.Singh AR. The task before psychiatry today. Indian J Psychiatry. 2007;49:60–5. doi: 10.4103/0019-5545.31521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Singh AR. The task before psychiatry today redux: STSPIR. Mens Sana Monogr. 2014;12:35–70. doi: 10.4103/0973-1229.130295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sullivan PF, Kendler KS, Neale MC. Schizophrenia as a complex trait: Evidence from a meta-analysis of twin studies. Arch Gen Psychiatry. 2003;60:1187–92. doi: 10.1001/archpsyc.60.12.1187. [DOI] [PubMed] [Google Scholar]
- 42.Teja S, Narang RL, Aggarwal AK. Depression across cultures. Br J Psychiatry. 1971;119:253–60. doi: 10.1192/bjp.119.550.253. [DOI] [PubMed] [Google Scholar]
- 43.Tseng WS. Culture and psychopathology: A general vew. In: Bhugra D, Bhui KS, editors. Textbook of Cultural Psychiatry. Cambridge, UK: Cambridge University Press; 2007. pp. 96–112. [Google Scholar]