Abstract
Given dramatic racial disparities in rates of HIV/STDs among African Americans, understanding broader structural factors that increase the risk for HIV/STDs is crucial. This study investigated incarceration history and unstable housing as two structural predictors of HIV risk behavior among 293 African Americans (159 men/134 women, Mage=27). Participants were recruited from an urban STD clinic in the southeastern U.S. Approximately half the sample had been incarcerated in their lifetime (54%), and 43% had been unstably housed in the past 6 months. Incarceration was independently associated with number of sex partners and the frequency of unprotected sex. Unstable housing was independently associated with the frequency of unprotected sex. However, these main effects were qualified by significant interactions: individuals with a history of incarceration and more unstable housing had more sex partners and more unprotected sex in the past three months than individuals without these structural barriers. Implications for structural-level interventions are discussed.
Keywords: HIV/AIDS, sexual risk behavior, structural factors, housing, incarceration, racial disparities
Introduction
Rates of sexually transmitted diseases (STDs), including HIV, are higher among African Americans than any other racial group in the United States.1 Although African Americans represent approximately 14% of the population, they acquire over 40% of all new HIV infections and account for nearly half of all AIDS diagnoses.1 Individual risk behaviors, alone, are not enough to explain these striking disparities. Instead, it has become clear that broader structural and contextual factors (e.g., poverty, homelessness, incarceration) increase the risk for HIV and STDs among African Americans.2-5 HIV-related structural factors have been defined as the economic, social, policy, organizational, or environmental barriers to, or facilitators of, an individual’s HIV prevention behaviors.5 Although it is clear that these structural factors are important, the way in which structural barriers drive vulnerability to disease is not completely understood.6,7
A history of incarceration and a lack of stable housing are two structural factors that are associated with poor health outcomes, including the transmission of HIV and other STDs.2,4 Both factors lead to social isolation and disruption in social and sexual networks, which impede the formation of stable relationships.2 This disruption may help explain why sexual risk behaviors, such as multiple partnerships, casual sex, exchange sex, and unprotected sex, have been frequently documented among individuals who lack stable housing,8,9 and formerly incarcerated individuals.10 These structural risk factors also disproportionately affect African Americans. For example, Black men are two and a half times more likely to be arrested and between 5 to 7 times more likely to be incarcerated than White men.11,12 Poverty, homelessness, and limited access to safe, affordable housing are also more prevalent social problems among African Americans than Caucasian individuals in the United States.13
Although we know that incarceration and unstable housing are each, individually, risk factors for HIV vulnerability among African Americans, we do not know if these factors work in isolation (i.e., each independently predicting increased risk), or if these factors work in combination, such that people with a history of incarceration and unstable housing are most likely to engage in sexual behaviors that place them at risk for acquiring STDs. Mounting evidence suggest incarceration and unstable housing may result in overlapping vulnerabilities to negative health outcomes among minority groups, including HIV/STDs,4 but we are unaware of any studies that have explicitly examined the interaction between these two powerful social forces and individuals’ sexual risk behavior. Thus, the purpose of the current study was to examine the individual and interactive effects of incarceration and unstable housing on risky sexual behaviors of African American STD clinic patients.
Method
Participants and Procedures
We recruited participants from a large, publicly funded urban STD clinic in a Southeastern U.S. city as part of a cross-sectional, computer-based survey study of sexual risk behavior among African Americans.14 African-American adults who came to the clinic were referred by clinic staff to a trained recruiter who described the study and asked if they might be interested in being screened. Individuals showing interest and meeting eligibility criteria (identify as Black/African-American, heterosexually active in the past three months, aged 18-44, and not knowingly HIV positive) using a 1-page screening form completed an audio computer-assisted self-interview (ACASI). The ACASI was designed with low literacy populations in mind and an African-American narrator’s voice read all questions and response options. The informed consent and survey administration were conducted in a private room within the clinic. To encourage honest responding, and as a part of the informed consent process, participants were assured that their individual responses were confidential and would not be shared with their treatment providers. The survey was conducted one participant at a time, it took approximately 30 minutes to complete, and participants were compensated with $30. The University Institutional Review Board approved all study procedures.
A total of n=331 individuals visiting the STD clinic were screened for the study over an 11-month period. Of these individuals, n=22 were ineligible and n=16 were eligible but declined to participate. Thus, a total of n=293 individuals (159 men, 134 women) were enrolled (293/309 = 95% response rate). The average age of participants was 26.9 (SD=6.9). The majority of participants were single (n=222, 75.8%). The highest level of education attained was as follows: high school diploma/GED (n=141, 48.1%); less than 11th grade education (n=85, 29.1%); 2-year technical degree/some college (n=48, 16.4%); or a four-year bachelors or graduate degree (n=19, 6.5%). Participants were primarily low-income: in the past year, 68% (n=198) indicated their individual income was less than $10,000, 15% (n=44) made between $10,000-20,000, and 17% (n=51) indicated they made more than $20,000 in the past year. Finally, 44% (n= 128) of participants indicated they had an STD in the past 6 months.
Measures
Demographics and Substance Use
We assessed participants’ gender, age, highest level of education completed, and the frequency of substance use (i.e., binge drinking, marijuana use, cocaine use) in the past year.
Incarceration History
We assessed incarceration history by asking participants the number of times they had ever been incarcerated in a detention center or prison (0=never, 1=once, 2=2 times, 3=3-5 times, 4=6 or more times).
Unstable Housing
We assessed unstable housing by asking participants how many different places they had lived over the past 6 months (1=1 place, 2=2 places, 3=3 or more places).
Sexual Behavior
Risky sexual behavior was assessed with two items: one assessing the number of sex partners in the past three months and a second assessing the number of unprotected sex acts in the past three months. Data points that were over three standard deviations from the mean were winsored to fit the normal distribution15 (n=5 for number of partners; n=6 for unprotected sex). We also assessed the type of partners (primary versus casual) with whom participants’ engaged in intercourse over the past 3 months. Primary partners were defined as a “main or steady sex partner”; casual sex partners were defined as any person with whom the participant had sex who was not a main or steady partner.
Analysis
First, we conducted descriptive analyses to determine the frequency of incarceration, unstable housing, and risky sexual behavior. Then, we used multivariate Poisson regression models to test the main effects of incarceration and unstable housing and the interaction between these variables to predict either: a) number of sex partners or b) number of unprotected sex acts, controlling for age, gender, education, substance abuse, and partner type (primary versus casual).
Results
Descriptives
Incarceration and Unstable Housing
The majority of participants (54%, n=157) had been incarcerated in their lifetime. Of those incarcerated, 27% (n=42) had been incarcerated once, 24% (n=37) had been incarcerated twice, 27% (n=43) had been incarcerated 3-5 times, and 22% (n=35) had been incarcerated six or more times. Further, nearly half the sample (42%, n=123) had been unstably housed in the past six months. Of those who had been unstably housed, 55% (n=68) had lived in two places and 45% (n=55) had lived in three or more places.
Risky Sexual Behavior
In the past 3 months, 150 participants (51%) had sex with casual/non-primary sexual partners, whereas 143 participants (49%) had sex exclusively with a primary relationship partner. The mean number of sex partners in the past three months was 3.37 (SD=4.81; range=0-25). Fifty-five percent (n=161) of participants had more than 1 sex partner and 14% (n=52) had 5 or more sex partners in the past three months. On average, participants engaged in 9.25 acts of unprotected sex in the past three months (SD=15.83, range=0-75). Most participants (71%, n=208) had engaged in unprotected sex at least once, and 26% (n=87) had unprotected sex 10 or more times in the past three months. The number of sex partners was moderately positively correlated with the number of acts of unprotected sex (r = .23, p < .001), suggesting these risk behaviors are related but also contain a considerable amount of unshared variance.
Are Incarceration and Unstable Housing Associated with Risky Sex?
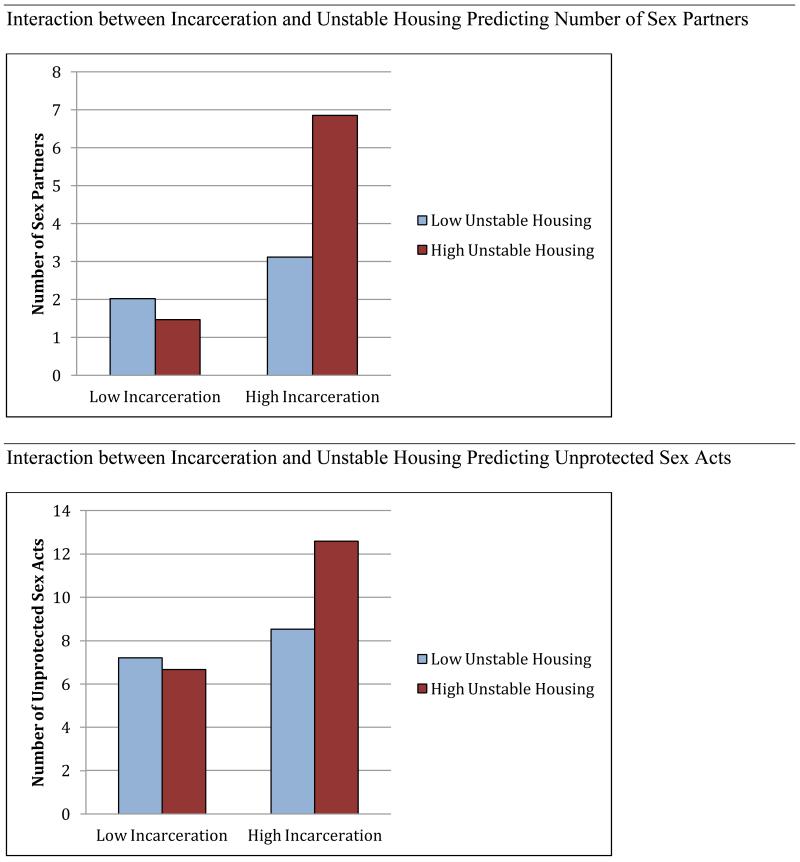
Consistent with past research, we found several main effects (see Table 1). Specifically, individuals with more frequent incarceration histories had significantly more sex partners and more unprotected sex. Further, individuals with more unstable housing had more unprotected sex. However, these main effects were qualified by significant interactions: compared to individuals without a history of incarceration or unstable housing, individuals with a history of incarceration and more unstable housing, had 1) significantly more sex partners, and 2) significantly more unprotected sex acts (all p values<0.05; See Figure 1). Age, gender, education, substance abuse, and partner type were controlled in each model.
Table 1. Poisson Regressions with Incarceration and Unstable Housing Predicting Number of Sex Partners and Number of Unprotected Sex Acts.
|
Number Sex Partners
N = 293 |
Number Unprotected Sex Acts
N = 292 |
|||||
|---|---|---|---|---|---|---|
|
| ||||||
| Wald χ2 | Exp(B) | (95% CI) | Wald χ2 | Exp(B) | (95% CI) | |
| Main Effects Models | ||||||
| Incarceration | 5.02* | 1.05 | (1.01,1.10) | 265.97*** | 1.25 | (1.21,1.28) |
| Unstable Housing | 0.74 | 0.97 | (0.89,1.05) | 16.96*** | 1.11 | (1.05,1.16) |
| Interaction Models | ||||||
| Incarceration | 6.10* | 1.06 | (1.01,1.11) | 268.23*** | 1.25 | (1.22,1.29) |
| Unstable Housing | 0.29 | 0.98 | (0.90,1.06) | 20.74*** | 1.12 | (1.07,1.18) |
| IncarcXUnstHous | 6.13** | 0.94 | (0.89,0.99) | 3.80* | 0.97 | (0.94,1.00) |
Note: gender, age, education, partner status, binge drinking, marijuana use, and cocaine use were included as control variables in all analyses (not shown here). IncarcXUnstHous = incarceration by unstable housing interaction. All main effects and control variables were mean centered.
p < .05;
p < .01;
p < .001
Figure 1. Pattern of Interactions between Incarceration and Unstable Housing Predicting Number of Sex Partners and Number of Unprotected Sex Acts.
Note: The interaction between incarceration and housing was plotted at one standard deviation above the mean of housing and incarceration for “high” groups and one standard deviation below the mean of housing and incarceration for “low” groups.
We conducted follow-up analyses to determine if these effects differed by gender. Controlling for age, education, substance abuse, and partner type we found that gender did not interact with incarceration or unstable housing to predict number of sex partners. However, gender interacted with both incarceration (Wald χ2=16.32, Exp(B)=0.90, 95% CI [0.86, 0.95], p<0.001) and unstable housing (Wald χ2=7.62, Exp(B)=1.15, 95% CI [1.04, 1.26], p<0.01) to predict the number of unprotected sex acts. Results indicated that the associations between incarceration and unprotected sex and between unstable housing and unprotected sex were both stronger for men than women.
Similarly, we conducted follow-up analyses to determine if the relationship between incarceration, unstable housing, and risky sexual behaviors differed depending on whether participants were in sexual relationships with primary partners or casual partners. Partner type did not interact with incarceration history to predict the number of unprotected sex acts; however, partner type did interact with unstable housing (Wald χ2=4.23, Exp(B)=1.11, 95% CI [1.01, 1.22], p<0.05), such that the relationship between unstable housing and unprotected sex was stronger for individuals with casual sex partners compared to those with primary sex partners. Additionally, we ran separate poisson regression models divided by partner status to determine if the interaction between unstable housing and incarceration would be associated with more unprotected sex regardless of whether an individual had primary or casual sex partners in the past 3 months. We found the interaction between incarceration and unstable housing remained significant in each group (primary partner group: Wald χ2=32.46, Exp(B)=0.85, 95% CI [0.80, 0.90], p<0.001; casual partner group: Wald χ2=5.05, Exp(B)=1.04, 95% CI [1.01, 1.08], p<0.05), demonstrating that the association holds for both primary and casual partners.
Discussion
The current research significantly extends previous studies that demonstrate an association between incarceration history or unstable housing and risky sexual behaviors8,10 by showing that these factors interact to predict risky sexual behaviors among African American STD clinic patients. Importantly, this interaction is evident regardless of whether individuals are in primary or casual sexual relationships and while accounting for important individual risk factors such as age, substance use, and education. To our knowledge, this is the first study to test the joint role of these structural factors and their impact on HIV risk behaviors. These findings have important implications for understanding risk behaviors and their contribution to the STD and HIV epidemics among African Americans. Incarceration is itself at epidemic levels in the US, in particular among African American males, who have the highest rates of incarceration of all racial/ethnic groups.11,12 Also, with the “great recession” of 2008, housing instability has increased significantly among low-income populations, including African Americans. These structural factors thus have the potential to increasingly fuel already glaring STD/HIV disparities among African Americans in the US, and they deserve significant attention. Such attention should come not only in the form of increased research to understand this phenomenon and interventions to change structures, but also through efforts to change policies that would increase vulnerable populations’ access to resources such as low cost housing and incarceration re-entry programs.
Considering that previous research has shown both incarceration and unstable housing to disrupt sexual networks and relationship functioning,2,4 it is in some ways not surprising that the confluence of these structural barriers leads to the most dramatic influences on risk behavior. Such risk behavior is troubling as the role of concurrency in facilitating HIV transmission, particularly in African American populations, has become increasingly apparent.10 This evidence provides clear support for the further development and testing of structural-level interventions, particularly those interventions that consider multiple structural barriers. These barriers may include incarceration and unstable housing as well as factors such as unemployment, poverty, racism and discrimination, poor access to health care, inadequate comprehensive sex education, and condom inaccessibility. In fact, this study adds even more urgency to other recent calls for the increased testing of structural intervention strategies in the United States.4,16
An important direction for future research will be to tease apart the mechanisms by which these factors act synergistically to increase risky behavior. The disruption in one’s life caused by incarceration (and/or factors that led to incarceration) may put one on a trajectory that includes unstable housing, relationship problems or dissolution, and risky sexual behaviors. Thus, it is possible that a history of incarceration serves as a causal agent that leads to housing instability and riskier sexual behaviors upon release for some individuals. This explanation is particularly relevant to the current study given that we assessed lifetime incarceration (of individuals who were no longer incarcerated), but we assessed housing instability in the past 6 months. On the other hand, it is possible that the factors that lead to unstable housing (e.g., financial problems, substance abuse) may also increase risk of behaviors that could lead to incarceration (e.g., theft, drug possession) and simultaneously impact sexual risk behaviors. Because this was a cross-sectional study, we were not able to determine causality or directionality in the associations between incarceration, housing, and risky sex practices. There are likely important mechanisms to be further understood, such as relationship dissolution, financial instability, and lack of social support, which may mediate the association between structural factors and risky sexual behaviors. Longitudinal research is needed to begin teasing apart the sequencing of these risk factors.
Although this study contributes to the mounting evidence that structural factors can increase vulnerability to HIV/STDs,2,5 a few limitations are worth considering. First, all data were collected via a self-report assessment. Because the number of sexual partners and frequency of unprotected intercourse may be perceived as undesirable, these behaviors may have been underreported. We used ACASI procedures to increase honest reporting;17 however, it remains possible that memory lapses or intentional misreporting could have biased study results. Additionally, although this study investigated structural risk factors, only individual-level data were analyzed. Subsequent research should also collect additional non self-report data on contextual factors (e.g., incarceration rates, poverty, homelessness, presence/absence of policies that impact these factors) for use in hierarchal models that examine respective contributions to HIV/STD risk at various levels within an ecological framework.
Conclusion
We found that the confluence of unstable housing and more frequent incarceration was associated with more engagement of sexual behaviors that place individuals at risk for HIV and STDs. Prevention approaches should increasingly address these structural-level factors as they can both increase risk for HIV transmission and impede effective access to treatment for individuals already infected. Previous work has suggested that participants in interventions who are unstably housed are less likely to change risky behavior than individuals with more secure housing.18,19 Housing status could be addressed in comprehensive intervention work, through laws and subsidies that provide guaranteed housing, for example,16 or through prevention approaches that offer employment and housing case management.20 Indeed, the current study supports the recent focus on structural intervention approaches to HIV prevention, particularly among African Americans.21 Overall, interventions that go beyond the individual level to change the structural factors affecting low-income African Americans’ risk behaviors should be given high priority in future prevention efforts.22
Acknowledgements
This work was supported by a Research Support Grant from the Office of the Vice President for Research and funds from the College of Communications and Information Studies at the University of Kentucky. This work was also supported in part by funding from NIH/NIAID 5 T32 AI07001-34: Training in Sexually Transmitted Diseases and HIV, support from the National Center for Research Resources and the National Center for Advancing Translational Sciences (NIH grant UL1TR000083), and support from the UNC Center for AIDS Research (NIH grant P30AI50410). The authors thank Greg Snow for his work on this project and Deborah Washburn and the clinic staff for their support of the project.
Contributor Information
Laura Widman, University of North Carolina, Chapel Hill.
Seth M. Noar, University of North Carolina, Chapel Hill
Carol E. Golin, University of North Carolina, Chapel Hill
Jessica Fitts Willoughby, University of North Carolina, Chapel Hill.
Richard Crosby, University of Kentucky.
References
- 1.CDC Sexually Transmitted Disease Surveillance - 2009. CDC. 2010 [Google Scholar]
- 2.Aidala AA, Sumartojo E. Why housing? AIDS and Behavior. 2007;11:1–6. doi: 10.1007/s10461-007-9302-z. [DOI] [PubMed] [Google Scholar]
- 3.Millett GA, Peterson JL, Flores SA, et al. Comparisons of disparities and risks of HIV infection in Black and other men who have sex with men in Canada, UK, and USA: A meta-analysis. Lancet. 2012;380:341–348. doi: 10.1016/S0140-6736(12)60899-X. [DOI] [PubMed] [Google Scholar]
- 4.National AIDS Minority Council . Mass incarceration, housing instability and HIV/AIDS: Research findings and policy recommendations. 2013. [Google Scholar]
- 5.Sumartojo E. Structural factors in HIV prevention: Concepts, examples, and implications for research. AIDS. 2000;14:S3–S10. doi: 10.1097/00002030-200006001-00002. [DOI] [PubMed] [Google Scholar]
- 6.Auerbach JD, Coates TJ. HIV prevention research: Accomplishments and challenges for the third decade of AIDS. American Journal of Public Health. 2000;90:1029–1032. doi: 10.2105/ajph.90.7.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta GR, Parkhurst JO, Ogden JA, Aggleton P, Mahal A. Structural approaches to HIV prevention. Lancet. 2008;372:764–775. doi: 10.1016/S0140-6736(08)60887-9. [DOI] [PubMed] [Google Scholar]
- 8.Aidala A, Cross JE, Stall R, Harre D, Sumartojo E. Housing status and HIV risk behaviors: Implications for prevention and policy. AIDS and Behavior. 2005;9:251–265. doi: 10.1007/s10461-005-9000-7. [DOI] [PubMed] [Google Scholar]
- 9.Browning CR, Olinger-Wilbon M. Neighborhood structure, social organization, and number of short-term sexual partnerships. Journal of Marriage and Family. 2003;65:730–745. [Google Scholar]
- 10.Adimora AA, Schoenbach VJ, Doherty IA. Concurrent sexual partnerships among men in the United States. American Journal of Public Health. 2007;97:2230–2237. doi: 10.2105/AJPH.2006.099069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hartney C, Vuong L. Created equal: Racial and ethnic disparities in the U.S. criminal justice system. National Council on Crime & Delinquency; Oakland, CA: 2009. Available at: http://nicic.gov/Library/023643. [Google Scholar]
- 12.Carson EA, Sabol WJ. Prisoners in 2011. U.S. Bureau of Justice Statistics. 2012 Available at: http://www.bjs.gov/content/pub/pdf/p11.pdf.
- 13.DeNavas-Walt C, Proctor BD, Smith JC. Income, Poverty, and Health Insurance Coverage in the United States: 2010, U.S. Census Bureau, Current Population Reports: 60-239. U.S. Government Printing Office; Washington, D.C.: 2011. [Google Scholar]
- 14.Noar SM, Crosby R, Benac C, Snow G, Troutman A. Application of the attitude-social influence-efficacy model to condom use among African-American STD clinic patients: implications for tailored health communication. AIDS and Behavior. 2011;15:1045–57. doi: 10.1007/s10461-009-9599-x. [DOI] [PubMed] [Google Scholar]
- 15.Tabachnick BG, Fidell LS. Using multivariate statistics. 5th ed. Allyn & Bacon; Boston: 2006. [Google Scholar]
- 16.Adimora AA, Auerbach JD. Structural interventions for HIV prevention in the United States. JAIDS. 2010;55:S132–S135. doi: 10.1097/QAI.0b013e3181fbcb38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Des Jarlais DC, et al. Audio-computer interviewing to measure risk behaviour for HIV among injecting drug users: A quasi-randomised trial. Lancet. 1999;353:1657–61. doi: 10.1016/s0140-6736(98)07026-3. [DOI] [PubMed] [Google Scholar]
- 18.Des Jarlais DC, Braine N, Friedmann P. Unstable housing as a factor for increased injection risk behavior at US syringe exchange programs. AIDS and Behavior. 2007;11:78–84. doi: 10.1007/s10461-007-9227-6. [DOI] [PubMed] [Google Scholar]
- 19.Elifson KW, Sterk CE, Theall KP. Safe living: The impact of unstable housing conditions on HIV risk reduction among female drug users. AIDS and Behavior. 2007;11:45–55. doi: 10.1007/s10461-007-9306-8. [DOI] [PubMed] [Google Scholar]
- 20.Raj A, Dasgupta A, Goldson I, Lafontant D, Freeman E, Silverman JG. Pilot evaluation of the Making Employment Needs [MEN] Count intervention: Addressing behavioral and structural HIV risks in heterosexual Black men. AIDS Care. 2013 doi: 10.1080/09540121.2013.804901. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bowleg L, Raj A. Shared communities, structural contexts, and HIV risk: prioritizing the HIV risk and prevention needs of Black heterosexual men. American Journal of Public Health. 2012;102(Suppl 2):S173–177. doi: 10.2105/AJPH.2011.300342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Auerbach J. Transforming social structures and environments to help in HIV prevention. Health Affairs. 2009;28:1655–1665. doi: 10.1377/hlthaff.28.6.1655. [DOI] [PubMed] [Google Scholar]