Abstract
Reactive perforating collagenosis (RPC) is a rare form of transepithelial elimination, in which genetically altered collagen is extruded through the epidermis. Of the acquired and inherited form, inherited form is extremely rare. Here, we present two cases of inherited form of RPC in a family.
Keywords: Familial reactive perforating collagenosis, inherited, transepidermal elimination
Introduction
What was known?
Reactive perforating collagenosis (RPC) is a type of transepithelial elimination disorder characterized by elimination of altered collagen through the epidermis.
The classical four transepithelial elimination (TEE) disorders include reactive perforating collagenosis (RPC), elastosis perforans serpiginosa (EPS), perforating folliculitis (PF), and Kyrle's diseases (KD). These four classical entities have some specific differentiating features. RPC and EPS have an inherited as well as an acquired form while PF and KD are in most cases, acquired.[1]
RPC is a rare form of TEE in which genetically altered collagen is extruded through the epidermis.[2] Here, we present two cases of inherited form of RPC in a family.
Case Report
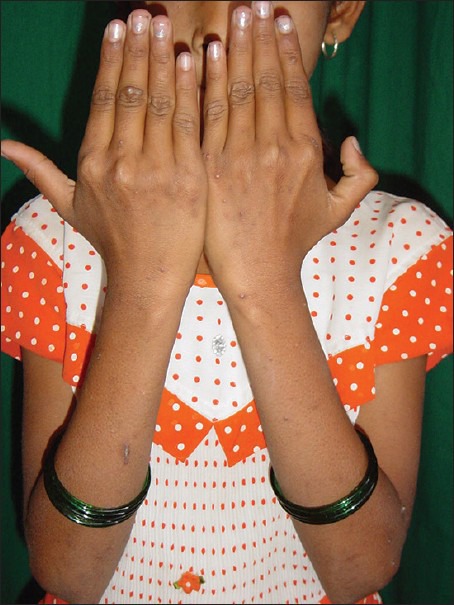
A 30-year-old woman presented to the out-patient department with minimally itchy papules over the extremities since childhood. History of spontaneous remission and exacerbation was present. There was no history of oozing, vesiculation, or crusting. There were no specific aggravating or relieving factors. Among her two daughters, the eldest aged 10 years had similar lesions since one year of age. Similar history of minimal itch and spontaneous resolution and exacerbation was seen. Cutaneous examination revealed multiple pigmented well-defined keratotic papules with central adherent keratotic plugs on the forearms and legs. Koebners phenomenon was present in the child. Scarring was seen over the resolved lesions [Figures 1–3]. Nails, hair, teeth, and mucosa were normal. Systemic examination was unremarkable. Complete hemogram, blood sugar, liver function tests, and renal function tests were normal. Urine analysis for albumin and microscopy was normal.
Figure 1.

Mother and child showing multiple keratotic papules over the extremities
Figure 3.
Keratotic papules with koebnerization over the forearm in the child
Figure 2.

Keratotic papules over the extremities
Biopsy of the lesion from the forearm of the mother revealed the epidermis showing cup- shaped depression containing parakeratotic cells intermingled with basophilic material and degenerated collagen bundles. At the base, the epidermis is thinned out with fragmented fibrous tissue. Hair shaft is seen in the crater. Papillary dermis showed proliferating capillaries and sparse lymphocytic infiltration and collagen bundles suggesting a diagnosis of RPC [Figure 4]. Both mother and child were started on topical corticosteroids (fluticasone) to be applied once in the morning, along with retinoic acid and moisturizers with minimal improvement after two months of treatment.
Figure 4.
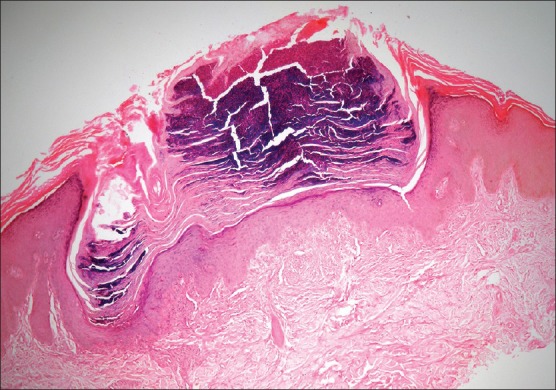
Epidermis shows cup shaped depression containing parakeratotic cells intermingled with basophilic material and degenerated collagen bundles. At the base the epidermis is thinned out with fragmented fibrous tissue. Hair shaft is seen in the crater. Papillary dermis showed proliferating capillaries and sparse lymphocytic infiltration and collagen bundles. H and E, ×40
Discussion
RPC is a rare skin disorder characterized by transepidermal elimination of altered collagen through the epidermis.[3] Two patterns of RPC exist; the rare inherited form seen in children and the common acquired form seen in adults.[2] Classic RPC is a genodermatosis that is inherited as an autosomal dominant or recessive trait.[4] Fewer than 50 case reports of the inherited form of RPC exist in the world literature.[5] The acquired form is more common and is often referred to as acquired perforating dermatosis mostly associated with diabetes, hemodialysis, and internal neoplasia.[1] Overexpression of TGF-ß3 and extracellular matrix proteins may be seen in these patients.[6]
Though the exact cause is not known, the basic defect seems to be a genetic abnormality of the collagen leading to its focal damage, which is then extruded as a result of necrolysis of the overlying epidermis. Also, elevated serum and tissue concentration of fibronectin may be responsible for inciting increased epithelial migration and proliferation culminating in perforation.[7] It is also believed that transepidermal elimination of collagen is simply a reaction to chronic scratching or rubbing in pruritic patients.[8]
Trauma and cold induce the degeneration of collagen with thinning of epidermis in familial RPC. Lesions of acquired form of RPC may follow trauma, folliculitis, cold, and various systemic disorders like diabetes mellitus, renal failure, hyperparathyroidism, liver diseases, neurodermatitis, Immunoglobin A nephropathy, periampullary carcinoma with jaundice, adenocarcinoma, and liver neoplasms.[9]
The inherited form usually starts in infancy or early childhood as small papules on the extensor surface of the hands, the elbows, and the knees following superficial trauma. The lesion increases in size to form an umblicated papule with central adherent keratotic plugs which regresses spontaneously in 6-8 weeks to leave a hypopigmented area or slight scar. Pruritus is common and Koebner's phenomenon may be present.[9] In some cases, recurrences were seen a little more frequently in summer than in winter owing to the longer duration of the former.[5] Our patient gave no history of any aggravating or relieving factors.
The condition may be mistaken clinically for molluscum contagiosum, papular urticaria, perforating serpiginous elastoma, PF, perforating granuloma annulare, and Kyrle's disease, but the histology is characteristic. Histopathologically, the classic lesion shows a vertically oriented, shallow, cup-shaped invagination of the epidermis, forming a short channel which is lined by acanthotic epithelium along the sides. At the base of the invagination, there is an attenuated layer of keratinocytes. Within the channel, there are densely packed degenerated basophilic staining material and basophilically altered collagen bundles. Vertically oriented perforating bundles of collagen are present interposed between the keratinocytes of the attenuated bases of the invagination. Masson's trichrome stain can be done to confirm that the fibers are collagen.[4]
Lesions are usually self-healing without any treatment, but often recur. Treatment is mainly aimed at controlling the pruritus. Topical corticosteroids under occlusion, emollients, keratolytics, retinoids, systemic antihistaminics, photochemotherapy, ultraviolet B phototherapy, liquid nitrogen cryotherapy, allopurinol, oral isotretinoin, methotrexate, and electrical nerve stimulation have been tried with varying success.[3,8]
What is new?
The inherited form of reactive perforating collagenosis is very rarely reported.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Rapini RP, Herbert AA, Drucker CR. Acquired perforating dermatosis. Evidence for combined transepidermal elimination of both collagen and elastic fibers. Arch Dermatol. 1989;125:1074–8. doi: 10.1001/archderm.125.8.1074. [DOI] [PubMed] [Google Scholar]
- 2.Faver IR, Daoud MS, Su WP. Acquired reactive perforating collagenosis. Report of six cases and review of the literature. J Am Acad Dermatol. 1994;30:575–80. doi: 10.1016/s0190-9622(94)70065-6. [DOI] [PubMed] [Google Scholar]
- 3.Bhat YJ, Manzoor S, Qayoom S, Wani R, Baba AN, Bhat AH. Familial reactive perforating collagenosis. Indian J Dermatol. 2009;54:334–7. doi: 10.4103/0019-5154.57608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Naik NS, Nousari CH, Heilman ER, Friedman RJ. Degenerative diseases and perforating disorders. In: Elder DE, Elenitsas R, Johnson BL, Murphy GF, Xu X, editors. Lever's Histopathology of the Skin. 10th ed. Philadelphia: Lippincott Williams and Wilkins; 2009. pp. 395–6. [Google Scholar]
- 5.Ramesh V, Sood N, Kubba A, Singh B, Makkar R. Familial reactive perforating collagenosis: A clinical, histopathological study of 10 cases. J Eur Acad Dermatol Venereol. 2007;21:766–70. doi: 10.1111/j.1468-3083.2006.02085.x. [DOI] [PubMed] [Google Scholar]
- 6.Gambichler T, Birkner L, Stücker M, Othlinghaus N, Altmeyer P, Kreuter A. Up-regulation of transforming growth factor-beta3 and extracellular matrix proteins in acquired reactive perforating collagenosis. J Am Acad Dermatol. 2009;60:463–9. doi: 10.1016/j.jaad.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 7.Morgan MB, Truitt CA, Taira J, Somach S, Pitha JV, Everett MA. Fibronectin and the extracellular matrix in the perforating disorders of the skin. Am J Dermatopathol. 1998;20:147–54. doi: 10.1097/00000372-199804000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Schmults CA. Acquired reactive perforating collagenosis. Dermatol Online J. 2002;8:8. [PubMed] [Google Scholar]
- 9.Cerio R, Calnan CD, Wilson-Jones E. A clinico-pathological study of reactive perforating collagenosis: Report of 10 cases. Br J Dermatol. 1987;117:16–7. [Google Scholar]


