Abstract
Acquired bilateral nevus of Ota-like macules (ABNOM) or Hori's nevus, a rare form of acquired dermal melanocytoses, presents as bilateral facial blue-gray macules without ocular or mucosal involvement. This condition is mostly found in women of Asian descent and usually appears in the fourth or fifth decade of life. Pathogenesis is unknown, though few theories have been proposed. Effective treatment has been found to be achieved with pigment-specific lasers. Herein, we report a case of Hori's nevus with mucosal involvement. A 42-year-old male patient, presented to us with blue-gray discoloration on either side of his face, both eyes, and in the mouth since the age of one year. Histopathological examination showed clusters and singly dispersed pigmented melanocytes within the upper and mid-dermis regions. Special staining of melanocytes using Masson-Fontana stain was positive. Diagnosis of Hori's nevus was made by correlating clinical and histopathological findings. Patient was informed of his treatment options, but refused treatment. A similar case of Hori's nevus with mucosal involvement has not been reported so far.
Keywords: Acquired bilateral nevus of Ota-like macules, bilateral nevus of Ota, hori's nevus
Introduction
What was known?
Acquired bilateral nevus of Ota-like macules (ABNOM) or Hori's nevus is an acquired dermal melanocytoses most commonly seen in women of Asian descent after the third decade of life. It presents clinically as multiple speckled blue-brown and/or slate-gray macules occurring bilaterally on malar areas or less commonly forehead, upper eyelids, and nose, without ocular or mucosal pigmentation.
Acquired bilateral nevus of ota-like macules (ABNOM) or Hori's nevus was first described by Hori et al. in 1984. It presents as asymptomatic blue- brown or slate-gray colored macules, located bilaterally on the face, without mucosal involvement. It is a condition usually found in middle-aged women of Asian descent. Pathogenesis is unknown, though a few theories have been suggested. Effective treatment has been found, to be achieved with pigment-specific lasers. Here, we report a case of Hori's nevus with mucosal involvement in a 42 yr. old South- Indian male.
Case Report
A 42-year old male presented to the skin out-patient department with symptoms suggestive of chronic urticaria. On examination, we observed symmetrical blue-gray discoloration on either side of his face [Figure 1]. On asking the patient for further details, he mentioned that his mother noticed the lesions at around one year of age, together with discoloration of his eyes and palate. No history suggestive of change in size, color, distribution of the lesions over the past few years could be elicited. There was no evidence of neurological involvement or visual disturbance. Patient was not on medications for any medical condition. There is no history of smoking or chewing tobacco.
Figure 1.

Blue-gray macules over the face and blue-brown discoloration of the sclera
Clinical examination revealed, multiple, discrete, speckled, blue-gray to slate-gray, hyperpigmented macules, symmetrically distributed on either side of the face, involving the forehead, anterior aspect of the scalp, bilateral temporal, zygomatic, malar areas, upper eyelids, nose, and pinnae [Figure 1]. Blue-brown discoloration of both sclera and a hyperpigmented irregular mottled patch over the hard palate was also noted [Figures 2a, b and Figure 3]. On ophthalmologic examination only scleral discoloration was observed and an otoscopic examination of both ears revealed normal tympanic membrane.
Figure 2a.

Blue-brown discoloration of right sclera
Figure 2b.

Blue-brown discoloration of left sclera
Figure 3.

Blue-gray discoloration of the hard palate
Histopathological examination of the hyperpigmented macules over the right frontal region of the scalp revealed increased melanin in the basal layers of the epidermis, clusters, and singly dispersed pigmented melanocytes within the papillary dermis and upper reticular dermis [Figure 4a]. Special staining for melanocytes with Fontana-Masson stain was positive [Figure 4b]. Mucosal biopsy of the hyperpigmented patch over the hard palate also revealed similar histopathological findings.
Figure 4a.
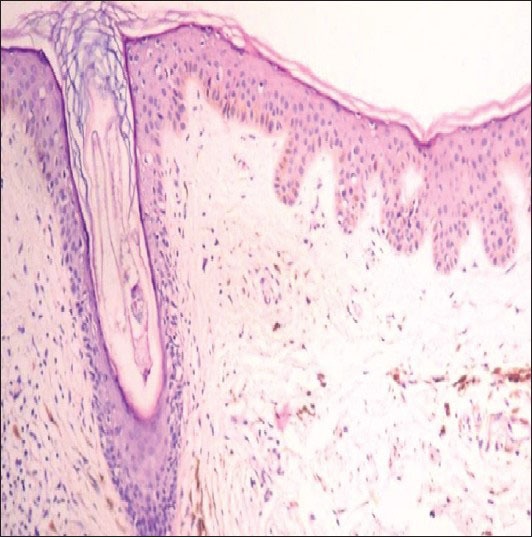
Melanin pigment in the upper and middle dermis (H and E stain, ×10)
Figure 4b.
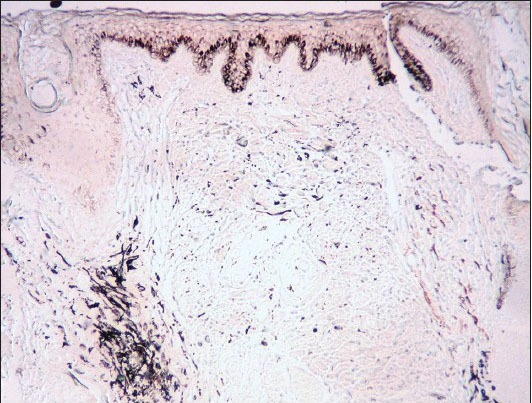
Special stain for melanocytes-Fontana-masson stain positive (×10)
By correlating the clinical and histopathological findings, we arrived at a diagnosis of Hori's nevus. Patient was informed of the available treatment options, but he refused treatment as he was asymptomatic.
Discussion
Hori's nevus, was originally described as acquired bilateral nevus of Ota-like macules (ABNOM), by Hori et al. in 1984.[1] It also goes by the synonyms “Nevus fusco-caeruleus zygomaticus and Acquired circumscribed dermal facial melanocytoses.”[2] It is most commonly seen in women of Asian descent after the third decade of life. It presents clinically as multiple speckled blue-brown and/or slate-gray macules occurring bilaterally on malar regions or less commonly on forehead, upper eyelids, cheeks, and nose, without ocular or mucosal pigmentation. Initially it presents as discrete brown macules, which later, over time progress to form confluent slate-gray macules.[1]
Histopathologically, irregularly shaped bipolar melanocytes that contain many singly dispersed melanosomes in stages II, III, and IV of melanisation in the middle and the upper dermis without disturbance of normal skin architecture are seen.[1] This condition is characterized by prominent epidermal hypermelanosis together with dermal melanophages. Variations in color (brown, gray, blue) are due to the varied proportion of pigmented cells in the epidermis and dermis.[3]
Pathogenesis though unknown, a few theories have been proposed, namely, the dropping-off of epidermal melanocytes.[1] This mechanism is consistent with the fact that the color of the macules varies with the maturity of the lesions. Initially, these macules are usually brown and discrete becoming bluish-gray and diffuse over time. The early-stage brown lesions are thought to be due to the presence of melanocytes at the basal layer of the epidermis and their subsequent migration into the dermis leads to a darker bluish-gray color.[3] Other theories proposed are the migration of hair bulb melanocytes, reactivation of preexisting dermal melanocytes, and manifestation of latent dermal melanocytosis, which is triggered by dermal inflammation, atrophy, or aging-related degeneration of the epidermis and dermis.[1]
Hori's nevus can occur simultaneously with other pigmentary abnormalities such as melasma, freckles, solar lentigenes, and nevus of Ota. It has been misdiagnosed many times in the past as Riehl's melanosis and can be differentiated from the same histologically.[3,4,5] It also mimics the centrofacial type of melasma when confined to the malar area or forehead and can be distinguished from the same histologically.[5] This condition should be clinically and histologically differentiated from bilateral Ota's nevus. Pigmentation of ABNOM is not as intensive as the bilateral nevus of Ota.[1,5]
Hori's nevus is particularly challenging to treat and there are at least two potential reasons for this: First, the melanocytes are located perivascularly leading to a higher likelihood of postinflammatory hyperpigmentation after laser therapy, and second, frequent association with melasma and thus, the associated presence of epidermal pigmentation. However, there are reports of it being successfully treated with pigment-specific lasers, namely the Q-switched Nd: Yag laser (1064 nm), Q-switched alexandrite laser (755 nm), and Q-switched ruby laser (694 nm).[6,7] As such, combination approaches are frequently used. Prior epidermal ablation with carbon dioxide laser has been found to increase the therapeutic efficacy of pigment specific lasers.[8] Dermabrasion using the coarse diamond fraise tip has also been found to be cost effective with good cosmetic results.[9]
Review of literature yielded evidence of only 15 cases of nevus of Ota involving the oral mucosa, to date, of which majority of them were noted on the hard palate. Most of the cases have occurred in females (64%). Appearance of palatal pigmentation usually blends with oral mucosa and is typically irregular, ill-defined, and often mottled patch.[10]
In this rare case of ABNOM or Hori's nevus, there was also presence of mucosal involvement. In this report, a rare case of ABNOM or Hori's nevus, there was also presence of mucosal involvement. We have mentioned the differences between bilateral nevus of Ota, Hori's nevus and the present case in Table 1.
Table 1.
Differences between bilateral of Ota, Hori's nevus and the present case
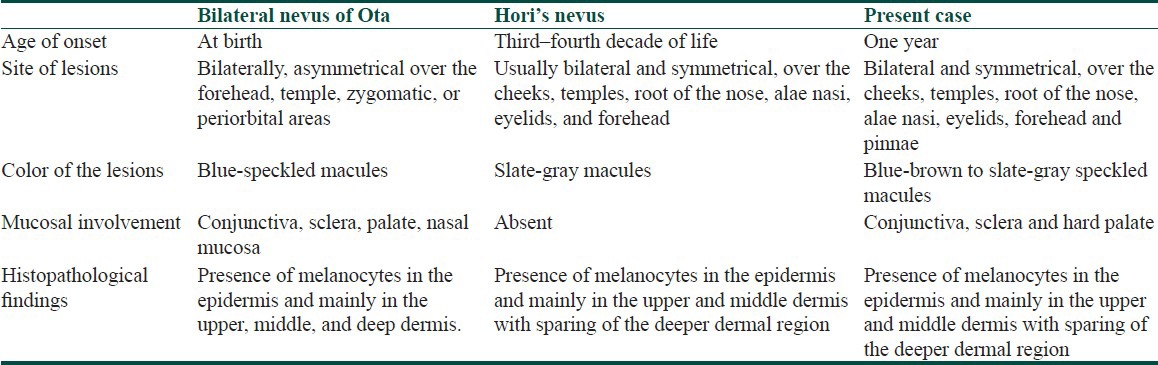
Our case differed from bilateral nevus of Ota in the following aspects: Acquired onset, site of involvement, and histopathological findings. Our case differed from Hori's nevus in the following aspects: Early onset and mucosal involvement.
We preferred to diagnose this case, a variant of Hori's nevus and not bilateral nevus of Ota, in view of the similarities with the former condition. The patient was informed of his treatment options, mainly in the form of pigment-specific lasers, but as he was asymptomatic, he refused any treatment.
What is new?
Hori's nevus in this case presented at one year of age and is associated with conjunctival and oral mucosal involvement that can be differentiated from a bilateral nevus of Ota, which has a similar presentation, by clinico-histopathologic correlation.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Hori Y, Kawashima M, Oohara K, Kukita A. Acquired bilateral nevus of Ota-like macules. J Am Acad Dermatol. 1984;10:961–4. doi: 10.1016/s0190-9622(84)80313-8. [DOI] [PubMed] [Google Scholar]
- 2.Sun CC, Lu YC, Lee EF, Nakagawa H. Naevus fusco-caeruleus zygomaticus. Br J Dermatol. 1987;117:545–53. doi: 10.1111/j.1365-2133.1987.tb07485.x. [DOI] [PubMed] [Google Scholar]
- 3.Hori Y, Takayama O. Circumscribed dermal melanoses: Classification and histologic features. Dermatol Clin. 1988;6:315–26. [PubMed] [Google Scholar]
- 4.Ee HL, Wong HC, Goh CL, Ang P. Characteristics of Hori naevus: A prospective analysis. Br J Dermatol. 2006;154:50–3. doi: 10.1111/j.1365-2133.2005.06689.x. [DOI] [PubMed] [Google Scholar]
- 5.Park JH, Lee MH. Acquired, bilateral nevus of Ota-like macules (ABNOM) associated with Ota's nevus: Case report. J Korean Med Sci. 2004;19:616–8. doi: 10.3346/jkms.2004.19.4.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cho SB, Park SJ, Kim MJ, Bu TS. Treatment of acquired bilateral nevus of Ota-like macules (Hori's nevus) using 1064-nm Q-switched Nd: YAG laser with low fluence. Int J Dermatol. 2009;48:1308–12. doi: 10.1111/j.1365-4632.2008.04061.x. [DOI] [PubMed] [Google Scholar]
- 7.Lam AY, Wong DS, Lam LK, Ho WS, Chan HH. A retrospective study on the efficacy and complications of Q- switched alexandrite laser in the treatment of acquired bilateral nevus of Ota-like macules. Dermatol Surg. 2001;27:937. doi: 10.1046/j.1524-4725.2001.01094.x. [DOI] [PubMed] [Google Scholar]
- 8.Manuskiatti W, Sivayathorn A, Leelaudomlipi P, Fitzpatrick RE. Treatment of acquired bilateral nevus of Ota-like macules (Hori's nevus) using a combination of scanned carbon dioxide laser followed by Q-switched ruby laser. J Am Acad Dermatol. 2003;48:584–91. doi: 10.1067/mjd.2003.193. [DOI] [PubMed] [Google Scholar]
- 9.Kunachak S, Kunachakr S, Sirikulchayanonta V, Leelaudomniti P. Dermabrasion is an effective treatment for acquired bilateral nevus of Ota-like macules. Dermatol Surg. 1996;22:559–62. doi: 10.1111/j.1524-4725.1996.tb00374.x. [DOI] [PubMed] [Google Scholar]
- 10.Guledgud MV, Patil K, Srivathsa SH, Malleshi SN. Report of rare palatal expression of Nevus of Ota with amendment of Tanino's classification. Indian J Dent Res. 2011;22:850–2. doi: 10.4103/0970-9290.94684. [DOI] [PubMed] [Google Scholar]


