Abstract
This study explores the manifestation and measurement of anxiety symptoms in 415 children with ASDs on a 20-item, parent-rated, DSM-IV referenced anxiety scale. In both high and low-functioning children (IQ above vs below 70), commonly endorsed items assessed restlessness, tension and sleep difficulties. Items requiring verbal expression of worry by the child were rarely endorsed. Higher anxiety was associated with functional language, IQ above 70 and higher scores on several other behavioral measures. Four underlying factors emerged: Generalized Anxiety, Separation Anxiety, Social Anxiety and Over-arousal. Our findings extend our understanding of anxiety across IQ in ASD and provide guidance for improving anxiety outcome measurement.
Keywords: Autism Spectrum Disorders, anxiety, measurement, comorbidity
Autism spectrum disorders (ASDs), including Autistic Disorder, Asperger’s Disorder and Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS), are characterized by impairments in social reciprocity and communication, together with repetitive and restricted behaviors and interests. In addition to these core symptoms, an estimated 40% of children with ASDs fulfill diagnostic criteria for an anxiety disorder (van Steensel et al. 2011) and as many as 84% have impairing, subclinical anxiety symptoms (White et al. 2009). Co-occurring anxiety can cause acute distress, amplify the core symptoms of ASD and trigger behavioral difficulties including tantrums, aggression and self-injury (Canitano 2006). Despite the prevalence of anxiety in ASDs, it remains unclear whether anxiety difficulties constitute a separate condition or align more closely with core ASD features. For example, social avoidance in Social Anxiety Disorder may appear similar to social withdrawal in ASDs. Furthermore, the appearance of anxiety symptoms may differ in children across the range of intellectual functioning and verbal abilities, presenting a key challenge for anxiety measurement in this group.
In early descriptions of autism, Kanner (1943) observed children with an ‘anxiously obsessive desire for the maintenance of sameness’. The third edition of the Diagnostic and Statistical Manual (DSM-III; American Psychiatric Association 1980) integrated anxiety symptoms within the core ASD criteria, including ‘intense and unusual anxieties’, ‘sudden, excessive anxiety’ and ‘unexplained panic attacks’. In the DSM-IV (and the proposed criteria of DSM-V) however, anxiety is not essential for an ASD diagnosis (American Psychiatric Association 2000). The DSM-IV also advises that Separation Anxiety Disorder, Social Anxiety Disorder and Generalized Anxiety Disorder can only be diagnosed if the symptoms are not better accounted for by the ASD itself (Witwer and Lecavalier 2010). A more thorough understanding of the nature of anxiety in ASDs would facilitate assessment and detection of change with treatment.
The common co-occurrence of anxiety in ASDs has been confirmed in over forty studies to date, using both dimensional (Lecavalier 2006; Kim et al. 2000) and categorical (Weisbrot et al. 2005; Gadow et al. 2004, 2005) approaches to measurement. In a comprehensive review, White and colleagues (White et al. 2009) reported that 11 to 84% of children with ASDs exhibit impairing anxiety symptoms. This variation likely stems from differences in sample size and ascertainment, as well as the anxiety measure employed. A meta-analysis of 31 studies showed that the most common anxiety diagnoses were specific phobia (30%), Obsessive Compulsive Disorder (OCD) (17%), social anxiety (17%) and generalized anxiety (15%) (van Steensel et al. 2011). Children with ASDs were over twice as likely as typically developing children to reach diagnostic cut-off for each anxiety disorder (Costello et al. 2005)..
The impact of cognitive ability requires particular attention when considering anxiety in ASDs. Subjects in previous samples have differed in their intellectual functioning and many reports have focused exclusively on children with ‘high-functioning’ autism or Asperger’s Disorder (White et al. 2009). Three studies, with sample sizes ranging from 172 to 1202, reported greater parent-rated anxiety symptoms in higher-functioning children with ASDs compared to children with IQ below 70 (Sukhodolsky et al. 2008; Weisbrot et al. 2005; Mazurek and Kanne 2010). In contrast, according to the meta-analysis by van Steensel and colleagues (2011), anxiety disorders were more common in participants with lower IQ scores across ASD subtypes. These inconsistent findings regarding anxiety and IQ may be attributable to the challenges of assessing anxiety in lower-functioning children–resulting in false positives or false negatives.
A previous study by Sukhodolsky and colleagues (2008) investigated anxiety symptoms in a sample of 5–17 year-olds with ASDs (N=172). Their measure was the parent-reported 20-item anxiety scale of the Child and Adolescent Symptom Inventory (Gadow and Sprafkin 1998, 2002), which showed good internal consistency across IQ. These investigators examined the association between anxiety in ASD and behavioral difficulties and observed low correlations between anxiety and measures of irritability, hyperactivity and adaptive behavior. Finally, higher levels of anxiety were associated with functional language, higher IQ and higher levels of stereotyped behaviors.
The current study represents a timely extension of the findings by Sukhodolsky et al (2008), using the same CASI-Anxiety scale in a related but expanded sample (N=415). First, we aimed to explore the frequency and distribution of anxiety symptoms in children with ASDs and the relationship between anxiety and other measures of problem behavior and adaptive functioning. We then aimed to broaden investigation to the item level, exploring the factor analytic structure of the CASI-Anxiety and the applicability of items across IQ. Finally we compared the clinical characteristics of children with the highest levels and lowest levels of anxiety in this sample in order to profile children with the most severe anxiety difficulties.
Methods
Participants
445 participants (aged 4–17 years) took part in one of four federally-funded, multisite treatment trials for ASDs (Research Units on Pediatric Psychopharmacology (RUPP) Autism Network 2002, 2005; King et al. 2009; Aman et al. 2009; Scahill et al. 2012). The studies were approved by each institutional review board and written informed consent was obtained from parents or legal guardians prior to data collection. Developmentally able minors also provided assent.
Samples from two of these studies were included in a previous paper (Sukhodolsky et al. 2008). The first (RUPP 1, Research Units on Pediatric Psychopharmacology (RUPP) Autism Network 2002) was a double-blind placebo-controlled trial of risperidone in children with Autistic Disorder (N=101) and serious behavioral problems. RUPP 2 targeted hyperactivity and compared methylphenidate versus placebo in children with ASDs (N=66) (Research Units on Pediatric Psychopharmacology (RUPP) Autism Network 2005).
The current study included participants from two additional trials. RUPP 3 (Aman et al. 2009) compared risperidone only with risperidone and parent management training in 124 children with an ASD diagnosis and severe behavioral problems. The final study randomized 149 children with ASDs to citalopram or placebo for moderate or greater repetitive behaviors (King et al. 2009; Scahill et al. 2012).
CASI-Anxiety data were available for 415 children (353 boys, 62 girls). Children with incomplete or missing data (N=30; 6.7%) were significantly younger (mean 7.0, sd 1.74 years versus 8.47, sd 2.87), had lower Vineland Communication scores (mean 43.34, sd 13.29 versus 57.16, sd 22.50) and lower ABC-Irritability scores (mean 16.90, sd 9.55 versus 21.39, sd 10.87) compared to the remaining sample.
The majority (n=336, 81%) of children were diagnosed with Autistic Disorder, 200 (51%) had an IQ greater than or equal to 70, and 94 (23%) were classified as non-verbal. All participants were healthy, medication-free for at least two weeks (one month for fluoxetine or antipsychotic medications) prior to baseline and judged free of another psychiatric condition in need of treatment. Based on parent-report, the sample was 70% Caucasian, 11% African-American, 8% Hispanic, 7% Asian and 4% ‘other’.
Procedure
The current study uses datapretreatment assessment for each trial. incorporated tests of IQ and adaptive behavior, along with medical and psychiatric histories, a physical examination and parent-rated questionnaires. The diagnostic assessment was conducted by an experienced team at each site and corroborated by the Autism Diagnostic Interview-Revised (ADI-R, Le Couteur 2003). Diagnosis of Asperger’s Disorder or PDD-NOS was based on DSM-IV criteria using all available clinical information.
Measures
Child and Adolescent Symptom Inventory (CASI)
This 132-item, parent-rated scale is a reliable and valid screening instrument for DSM-IV psychiatric disorders (Gadow and Sprafkin 1998, 2002; Sprafkin et al. 2002). Items are scored on a scale from 0 (never) to 3 (very often); with scores of 2 and 3 indicating clinical significance.
CASI-Anxiety scale
The CASI includes 26 items across several DSM-IV anxiety disorders: generalized anxiety (8 items), separation anxiety (8 items), Post Traumatic Stress Disorder (PTSD, 2 items), somatization (2 items), social phobia (2 items), OCD (2 items), simple phobia (1 item) and panic disorder (1 item). The Symptom Severity score (the sum of all CASI anxiety items) has demonstrated satisfactory internal consistency, reliability and validity in typically developing, clinic-referred and ASD samples (Sprafkin et al. 2002).
In a previous investigation, 6 items were excluded prior to analysis (Sukhodolsky et al. 2008). The two PTSD items were removed due to low occurrence in ASDs. Four items were excluded to reduce overlap with oppositional defiant disorder (ODD), ADHD and OCD. For these analyses, we included subjects with at least 18 of 20 items completed (the total score was calculated using a mean scale replacement).
CASI-PDD scale
The current study also used the 12-item CASI-PDD scale, which assesses social deficits, communication problems and repetitive and unusual behaviors.
The Aberrant Behavior Checklist (ABC)
This 58-item, parent-rated scale of childhood behavior, assesses i) Irritability (aggression, tantrums, self-injury; 15 items; α in this sample = 0.88); ii) Social Withdrawal / Lethargy (social interest, response to others; 16 items); iii) Stereotypic Behavior (7 items); iv) Hyperactivity (16 items) and v) Inappropriate Speech (excessive talking, repeating phrases; 4 items) (Aman et al. 1985). Items are scored from 0 (not a problem) to 3 (severe problem). The ABC has solid validity and reliability from previous studies and has normative data in developmentally disabled populations (Brown et al. 2002; Marshburn and Aman 1992).
Vineland Adaptive Behavior Scales
The Vineland is a reliable and valid semi-structured parent interview designed to assess adaptive competencies in childhood (Sparrow et al. 1984). The current analyses included three domains i) Communication ii) Daily living iii) Socialization. Raw scores are converted to standard scores (mean 100; SD 15), with higher scores representing greater adaptive functioning.
Children’s Yale-Brown Obsessive Compulsive Scale modified for Pervasive Developmental Disorders (CYBOCS-PDD)
This is a 5-item, clinician-rated scale adapted from the 10-item CYBOCS designed to quantify symptom severity in children with OCD (Goodman et al. 1989; Scahill et al. 1997). Given the difficulty of assessing obsessions in children with ASDs, the five obsession items of the original CYBOCS were dropped. Thus, the CYBOCS-PDD retains the five compulsion items and uses the parent as the primary informant. Several repetitive behaviors relevant to ASD were added to the symptom checklist and the probes were adjusted to make them developmentally appropriate for children with ASDs. The CYBOCS-PDD has demonstrated reliability, validity and sensitivity to change (McDougle et al. 2005; Scahill et al. 2006).
Intellectual Functioning
Several IQ tests were used based on the participants’ age and ability. These included the Wechsler Intelligence Scale for Children-III (Wechsler 1991), the Wechsler Preschool and Primary Scale of Intelligence-Revised (Wechsler 1989), the Mullen Scales of Early learning (Mullen 1995), the Leiter International Performance Scale-Revised (Roid and Miller 1997) and the Slosson Intelligence Test (Jensen and Armstrong 1985). IQ scores were available for 392 children (23 could not be tested). Given the range of assessment employed, children were classified with IQ below 70 or IQ greater than or equal to 70.
Analyses
We conducted descriptive analyses of the heterogeneous sample. The internal consistency of the CASI-Anxiety scale was assessed with the Cronbach alpha statistic. The distributions of CASI-Anxiety scores were examined for the full sample and for children with IQ above and below 70. T-tests were used to explore differences in CASI-Anxiety scores according to ethnicity, ASD diagnosis, IQ and age (above and below the median). A Pearson’s correlation was also calculated between the CASI-Anxiety and age to further investigate th relationship between age and anxiety.
Correlations (Pearson’s or Spearman’s Rank) were used to examine associations between the CASI-Anxiety and the ABC subscales, the Vineland and the CYBOCS-PDD, for the full sample and children with IQ above and below 70. Differences in these correlations were assessed using Fisher’s r-to-z transformations.
Chi-square and t-tests were used to compare the highest and lowest quartile of CASI-Anxiety scorers on IQ (above and below 70), the presence of language (verbal or non-verbal) and clinical indices (ABC, CYBOCS-PDD, CASI-PDD and Vineland Adaptive Behavior Scales). Logistic regression was used to test associations with membership of the high anxiety group. First, individual categorical variables were assessed, such as: language (verbal vs. nonverbal); ethnicity (Caucasian vs. all other ethnicities); diagnosis (Autistic Disorder versus PDD-NOS/Asperger’s Disorder), age (above vs. below the median) and IQ (above or below 70). Univariate analyses were also conducted using the upper quartile as a cut off for each of the ABC, Vineland, CYBOCS-PDD and CASI-PDD scales. Variables showing a significant association with high anxiety were included within a multivariate forward logistic regression model, controlling for age and gender.
To evaluate scale items, we examined the per-item mean and the number of children scoring at a clinically significant level (score of two (often) or three (very often)). T-tests were used to compare the endorsement of items between children with an IQ above and below 70.
Exploratory factor analysis (EFA) was employed to identify factor loadings underlying the items. Confirmatory factor analysis (CFA) compared the fit of different models to the observed data. Acknowledging the potential drawbacks of using the same sample for CFA and EFA, we conducted the EFA with the full sample and the CFA with half the sample selected at random.
EFA was conducted with the Comprehensive Exploratory Factor Analysis (CEFA) software. Ordinary least squares was selected as the discrepancy function because it requires fewer assumptions than maximum likelihood estimation or generalized least squares estimation. CASI items are scored on an ordinal scale. Therefore, we conducted factor analysis with polychoric correlations matrices rather than Pearson correlations, which could have underestimated inter-item associations.
CFA, using Lisrel,(Jöreskog and Sörbom 2004) compared the factor structure derived from the EFA to a one-factor solution. Root Mean Square Error Approximation (RMSEA) and Root Mean Square Residuals (RMR) were used as fit statistics. Lower RMSEA and RMR scores (ideally <0.05) indicate a better model fit.
Results
Sample Characteristics
The demographic and clinical characteristics of the study sample (N=415) are provided in Table 1. The proportion of children with an IQ of 70 or greater in the RUPP 2 (49%), RUPP 3 (56%) and STAART studies (54%) was higher than RUPP 1 (19%) (χ2 (3) = 38.79; p<0.01). ABC Irritability subscale scores differed between groups (F(3,106)=111.53, p<0.01), being highest in RUPP 3 (mean 29.48 sd 6.62) and lowest in the STAART study (mean 12.19, sd 8.67). ABC Hyperactivity subscale scores were also highest for RUPP 3 (mean 35.64, sd 8.40) and lowest for the STAART study (mean 19.90, sd 11.67) (F(3,408)=64.28, p<0.01). Mean CASI-Anxiety scores differed between groups (F(3,411)=3.09, p<0.01), being highest in RUPP 3 (16.19, sd 10.05) and lowest in the STAART study (12.84, sd 9.27). Although there are some differences in the characteristics of the four samples, these variations increase the heterogeneity of the combined dataset and fit with the exploratory nature of this study..
Table 1.
Demographic and clinical characteristics of the participants (separated by IQ level)
| Full Sample | IQ <70 | IQ ≥70 | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| Number of participants | 415 | 200 (51%) | 192 (49%) | |||
| Male (%) | 353 (85%) | 165 (83%) | 168 (88%) | |||
| Verbal (%) | 316 (77%) | 131 (66%) | 177 (100%) | |||
| Mean age in years (sd) | 8.47 (2.87) | 8.68 (2.89) | 8.35 (2.89) | |||
|
|
||||||
| ASD Diagnosis (%) | Autistic Disorder | 336 (81%) | 183 (92%) | 130 (68%) | ||
| Asperger’s Disorder | 20 (5%) | 2 (1%) | 18 (9%) | |||
| PDD-NOS | 59 (14%) | 15 (8%) | 44 (23%) | |||
|
| ||||||
| Means for continuous measures (sd) | t statistic | p value | ||||
|
| ||||||
| CASI | Anxiety Scale | 14.17 (9.37) | 12.24 (7.94) | 16.47 (10.26) | 4.58 | <0.01** |
| PDD scale | 21.70 (7.85) | 24.06 (7.72) | 19.05 (7.19) | 6.59 | <0.01** | |
|
|
||||||
| CYBOCS-PDD | 14.75 (3.09) | 14.89 (3.38) | 14.49 (2.79) | 1.27 | 0.20 | |
|
|
||||||
| Vineland Adaptive Behavior Scale | Communication | 57.16 (22.50) | 43.86 (16.14) | 72.03 (19.15) | 15.68 | <0.01** |
| Daily Living | 46.52 (21.06) | 36.78 (17.10) | 57.57 (19.75) | 11.08 | <0.01** | |
| Socialization | 55.38 (16.09) | 48.67 (15.27) | 62.77 (14.31) | 9.36 | <0.01** | |
|
|
||||||
| Aberrant Behavior Scales | Irritability | 21.39 (10.87) | 23.09 (10.75) | 19.84 (10.92) | 2.94 | <0.01** |
| Social Withdrawal | 14.24 (8.76) | 15.71 (9.20) | 12.80 (8.32) | 3.24 | <0.01** | |
| Stereotypy | 8.40 (5.12) | 9.58 (5.18) | 7.04 (4.78) | 5.03 | <0.01** | |
| Hyperactivity | 29.61 (11.70) | 30.77 (10.57) | 28.06 (12.89) | 2.26 | 0.02* | |
| Inappropriate Speech | 5.78 (3.73) | 5.97 (3.95) | 5.84 (3.33) | 0.33 | 0.75 | |
p<0.01;
p<0.05
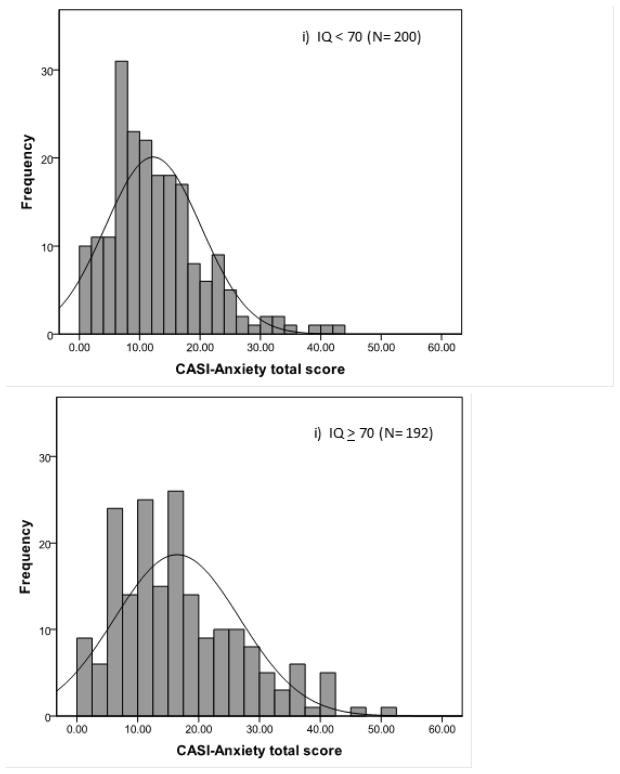
CASI-Anxiety scores ranged from 0 to 50 (mean 14.17, sd 9.4) and were slightly positively skewed (skew 1.03, kurtosis 0.94). The internal consistency of the items was high (α=0.87). Figure 1 shows the distribution of scores in children with IQ above and below 70. Children with an IQ of 70 or above were significantly more anxious (mean 16.47, sd 10.26) than those with IQ below 70 (mean 12.24, sd 7.94) (t(390)=4.58, p<0.01). Nonverbal children with IQ below 70 had even lower scores (mean 10.33, sd 6.73). When adjusting for IQ, there were no significant differences in anxiety across ASD diagnoses (F(2,388)=2.47; p=0.08). There were no significant differences in anxiety between younger and older (below and above median age) children (t(415)=1.13; p=0.26), between Caucasian children and children of other ethnicities (t(415)=1.25; p=0.24), or between males and females (t(415)=1.24; p=0.22).
Figure 1.
Frequency distributions of CASI-Anxiety scores for children with IQ i) below 70 ii) 70 or above
Pearson correlations (or Spearman for ABC Inappropriate Speech subscale and the CYBOCS-PDD scales, which were not normally distributed) between the CASI-Anxiety and behavioral scales are shown in Table 2. In the sample as a whole, correlations were often significant - but small to medium. There were slightly higher correlations between the CASI-Anxiety and these behavioral scales in children with an IQ below 70 compared to those with an IQ of 70 or above, although this difference only reached significance (p<0.05) for the ABC Inappropriate Speech subscale (z=2.3; p=0.02). The pattern of mean comparisons and correlations was unchanged when performed with transformed CASI-Anxiety scores to correct for the slightly positive skew.
Table 2.
Correlationsa between CASI-Anxiety and other behavior measures
| Measure | Total Sample (n=415) | IQ<70 (n =200)b | IQ≥70 (n=192)b | |
|---|---|---|---|---|
| Aberrant Behavior Checklist | Irritability | 0.31** | 0.40** | 0.31** |
| Social Withdrawal | 0.22** | 0.35** | 0.20** | |
| Stereotypy | 0.13** | 0.25** | 0.19* | |
| Hyperactivity | 0.23** | 0.35** | 0.20** | |
| Inappropriate Speecha | 0.31** | 0.42** | 0.21** | |
|
| ||||
| Vineland Adaptive Behavior | Communication | 017** | 0.15* | −0.05 |
| Daily Living | 0.13** | 0.21** | −0.13 | |
| Socialization | 0.18** | 0.14 | 0.07 | |
|
|
||||
| CYBOCS-PDDa | 0.08 | 0.08 | 0.18* | |
|
|
||||
| CASI | PDD scale | 0.17** | 0.29** | 0.24** |
p<0.05;
p<0.01
Pearson’s correlations were used for the majority of the subscales. Spearman’s rank correlations were used for the Inappropriate Speech and CYBOCS-PDD subscales owing to non-normal distributions.
IQ was unavailable for 23 subjects
Fisher’s r-to-z transformation was used to compare correlations in the lower vs higher IQ groups. Shaded cells indicate a significant group difference.
Children with high levels of anxiety
Children in the upper and lower quartile on the CASI-Anxiety scale were comparable in age (t (217)=0.56, p=0.58). A greater proportion of children with high anxiety had IQ scores of 70 or above (63%) compared to the low anxiety group (36%) (χ2 (1)=14.28, p=0.01) and a larger proportion were verbal (high anxiety: 90%; low anxiety: 64%; χ2 (1)= 19.74, p<0.01).
Table 3 shows that children in the high anxiety group scored significantly higher than children in the low anxiety group for all the ABC subscales (p<0.05). Consistent with the greater percentage of children with IQ of 70 or above, Vineland scales were also higher in the high anxiety group (p<0.05). CASI-PDD scores were also significantly higher in the high anxiety compared to the low anxiety group, suggesting greater ASD severity (p<0.01), but there no group difference on the CYBOCS-PDD scale (p=0.18).
Table 3.
Descriptive statistics for children in the highest and lowest quartiles on the CASI-Anxiety scale
| Frequency (%) | High anxiety (N=107) | Low anxiety (N=110) | |||
|---|---|---|---|---|---|
| IQ <70 (%) | 36 (35%) | 62 (61%) | |||
| Verbal (%) | 96 (90%) | 70 (64%) | |||
| Male (%) | 95 (89%) | 91 (83%) | |||
|
| |||||
| Scale | Mean (sd) | t statistic | p value | ||
|
| |||||
| Aberrant Behavior Checklist | Irritability | 25.42 (10.75) | 16.26 (10.04) | 6.40 | <0.01** |
| Social Withdrawal | 16.63 (9.25) | 11.17 (7.27) | 4.77 | <0.01** | |
| Stereotypy | 9.22 (5.35) | 7.61 (4.97) | 2.29 | 0.02* | |
| Hyperactivity | 33.30 (12.19) | 25.75 (11.62) | 4.60 | <0.01** | |
| Inappropriate Speech | 7.73 (3.27) | 4.25 (3.69) | 7.24 | <0.01** | |
|
| |||||
| Vineland Adaptive Behavior Scores | Communication | 61.97 (21.61) | 52.46 (22.15) | 3.19 | <0.01** |
| Daily Living | 50.39 (21.04) | 43.50 (20.78) | 2.41 | 0.02* | |
| Socialization | 59.87 (15.96) | 53.91 (15.19) | 2.80 | <0.01** | |
|
| |||||
| CYBOCS-PDD | 15.11 (2.60) | 14.61 (2.78) | 1.36 | 0.18 | |
|
| |||||
| CASI | PDD scale | 23.48 (7.63) | 19.61 (8.09) | 3.58 | <0.01** |
p<0.01;
p<0.05
Univariate logistic regressions revealed six significant associations with membership of the highest quartile on the CASI Anxiety scale: IQ of 70 or above (p<0.01), diagnosis of PDD-NOS or Asperger’s Disorder (versus Autistic Disorder) (p=0.02), being verbal (p<0.01) and scoring in the top quartile on the ABC Irritability, Social Withdrawal, Hyperactivity or Inappropriate Speech subscales (p<0.01). These variables were then included within a forward multivariate logistic regression, controlling for age and gender. The model provided a good fit to the data according to the Hosmer and Lemeshow test (χ2=2.53, df=7, p=0.93). Membership in the high anxiety group was most strongly associated with verbal ability (OR: 3.96 CI 1.37–11.41; p<0.01) and top quartile scores on the ABC Irritability (OR: 3.56 CI 1.37–9.25; p<0.01), Inappropriate Speech (OR: OR 4.19 CI 1.79–9.80; p<0.01) and Hyperactivity (OR: 2.52 CI 1.04–6.10; p<0.01) subscales. Children with IQ of 70 or above were nearly three times as likely to be in the high anxiety group compared to intellectually disabled children (OR: 2.92 CI 1.35–6.30; p<0.01).
Item-endorsement
Table 4 presents per-item means and the percentages of subjects scoring at the clinically significant level (rating of 2 or 3) for children with IQ 70 or above 0 (N=192) and those below 70 (N=200). Across the full sample, the three most commonly endorsed items were: i) ‘acts restless or edgy’ ii) ‘has difficulty falling asleep’ iii) ‘is more anxious in social situations than other children’. The three least endorsed items were: i) ‘worries about physical health’ ii) ‘has nightmares about being separated from parents’ iii) ‘complains about feeling sick when separation is expected.’
Table 4.
Item endorsement statistics for children with IQ above and below 70
| Item (number refers to the number in the full CASI measure) | IQ <70 (N=200) | IQ ≥ 70 (N=192) | ||
|---|---|---|---|---|
|
| ||||
| Mean (SD) | N at clinical cut-off (%)a | Mean (SD) | N at clinical cut-off (%)a | |
|
| ||||
| 47 is over concerned about abilities | 0.20 (0.55) | 10 (4.5) | 0.73 (0.90) | 41 (20.8) |
| 48 has difficulty controlling worries | 0.46 (0.77) | 23 (10.4) | 1.16 (1.11) | 73 (37.0) |
| 49 acts restless or edgyb | 1.53 (1.02) | 109(49.1) | 1.53 (1.00) | 103 (52.3) |
| 51 is extremely tense or unable to relaxb | 1.13 (0.99) | 70 (31.5) | 1.08 (0.92) | 59 (29.9) |
| 52 has difficulty falling asleepb | 1.37 (1.10) | 87 (39.2) | 1.36 (1.18) | 80 (40.6) |
| 53 is overly fearful of specific objects | 1.12 (1.01) | 66 (29.7) | 1.32 (1.13) | 83 (42.1) |
| 54 complains about heart poundingc | 0.11 (0.45) | 7 (3.2) | 0.41 (0.77) | 21 (10.6) |
| 55 cannot get distressing thoughts out of mind | 0.26 (0.62) | 13 (5.9) | 0.88 (1.01) | 55 (27.9) |
| 61 complains about physical health problemsc | 0.27 (0.63) | 11 (5) | 0.62 (0.85) | 31 (15.8) |
| 62 worries about physical health | 0.09 (0.40) | 4 (1.8) | 0.28 (0.63) | 11 (5.6) |
| 63 more anxious in social situations than most children | 1.54 (1.10) | 111 (50) | 1.73 (1.18) | 111 (56.4) |
| 64 is excessively shy with peers | 0.89 (0.95) | 56 (25.3) | 1.14 (1.09) | 66 (33.5) |
| 65 gets very upset when expects to be separated | 1.11 (0.97) | 55 (24.8) | 1.09 (0.98) | 47 (23.8) |
| 66 worries that parents will be hurt/leave | 0.40 (0.82) | 21 (9.5) | 0.49 (0.83) | 25 (12.7) |
| 67 worries that some disaster will separate from parents | 0.18 (0.55) | 9 (4.1) | 0.32 (0.77) | 16 (8.1) |
| 68 tries to avoid going to school to stay with parents | 0.40 (0.77) | 21 (9.5) | 0.57 (0.90) | 29 (14.7) |
| 69 worries about being left home alone or with sitter | 0.25 (0.59) | 8 (3.6) | 0.40 (0.71) | 15 (7.6) |
| 70 afraid to go to sleep unless near parents | 0.69 (1.01) | 40 (18.1) | 0.82 (0.10) | 43 (21.8) |
| 71 has nightmares about being separated from parentsc | 0.11 (0.45) | 6 (2.7) | 0.22 (0.59) | 9 (4.5) |
| 72 complains about feeling sick when expects separation | 0.12 (0.43) | 6 (2.8) | 0.26 (0.69) | 12 (6.1) |
Values in bold were significantly higher in children with IQ above 70 compared to below 70
Shaded items were excluded from the non-verbal anxiety total
Clinical significance is indicated by a score of 2 or 3 for a particular item
most endorsed items in both the high and low IQ groups
least endorsed items in both the high and low IQ groups
Children with IQ above 70 showed significantly higher per-item means (p<0.05) than children with IQ below 70 for 12 of the 20 items. The item ‘has difficulty controlling worries’ showed the greatest disparity in per-item means across the low IQ (0.46) and high IQ (1.16) groups. This difference in per-item mean score was even greater when compared to the subgroup of non-verbal children in the low IQ group (N=92).
Factor Analysis
Factor solutions with two, three, four and five factors were considered. Of these, the four factor solution was chosen for empirical reasons (e.g. high average factor loadings) and ease of interpretation. Table 5 presents the loadings of each item on all four factors, which corresponded with i) Generalized Anxiety ii) Separation Anxiety iii) Over-arousal (restlessness, tension, sleep difficulties) and iv) Social Anxiety. Correlations between these factors were modest, ranging from 0.12 (between Separation Anxiety and Social Anxiety) and 0.44 (between Generalized Anxiety and Separation Anxiety) (see Table 5). Items tended to load strongly on one factor, with relatively weak loadings on the other three factors. The one fear-rated item (‘is overly fearful of specific objects’), loaded moderately (0.41) onto the Separation Anxiety factor. The five factor solution divided Separation Anxiety into two factors and was discarded. The three factor solution, in contrast, did not distinguish between social anxiety and over-arousal, perhaps due to the low number of social anxiety items.
Table 5.
Factor loadings from the exploratory factor analysis (four factor solution), presented for the full sample
| Item (number refers to the number in the full CASI measure) | Factor 1 | Factor 2 | Factor 3 | Factor 4 |
|---|---|---|---|---|
|
| ||||
| Generalized Anxiety | Separation Anxiety | Over-arousal | Social anxiety | |
| 47 is over concerned about abilities | 0.84 | −0.14 | 0.00 | 0.03 |
| 48 has difficulty controlling worries | 0.84 | −0.07 | 0.07 | 0.15 |
| 49 acts restless or edgy | 0.03 | 0.03 | 0.72 | 0.03 |
| 51 is extremely tense or unable to relax | 0.03 | −0.04 | 0.88 | 0.02 |
| 52 has difficulty falling asleep | −0.08 | 0.10 | 0.57 | 0.00 |
| 53 is overly fearful of specific objects | 0.29 | 0.41 | −0.05 | 0.22 |
| 54 complains about heart pounding | 0.74 | 0.19 | −0.01 | −0.01 |
| 55 cannot get distressing thoughts out of mind | 0.81 | 0.04 | 0.05 | 0.07 |
| 61 complains about physical health problems | 0.71 | 0.04 | 0.09 | −0.02 |
| 62 worries about physical health | 0.85 | 0.09 | 0.01 | −0.03 |
| 63 more anxious in social situations than most children | 0.14 | 0.03 | 0.34 | 0.63 |
| 64 is excessively shy with peers | 0.21 | 0.06 | −0.05 | 0.65 |
| 65 gets very upset when expects to be separated | −0.25 | 0.81 | 0.06 | 0.29 |
| 66 worries that parents will be hurt/leave | 0.25 | 0.67 | 0.01 | 0.12 |
| 67 worries that some disaster will separate from parents | 0.51 | 0.55 | −0.04 | −0.04 |
| 68 tries to avoid going to school to stay with parents | 0.21 | 0.56 | 0.05 | −0.11 |
| 69 worries about being left home alone or with sitter | 0.00 | 0.80 | −0.08 | 0.03 |
| 70 afraid to go to sleep unless near parents | −0.17 | 0.66 | 0.23 | −0.08 |
| 71 has nightmares about being separated from parents | 0.26 | 0.68 | 0.16 | −0.23 |
| 72 complains about feeling sick when expects separation | 0.23 | 0.66 | 0.12 | −0.11 |
|
| ||||
| Correlations between Factors | ||||
|
| ||||
| Factor 1: Generalized Anxiety | 1.00 | |||
| Factor 2: Separation Anxiety | 0.44 | 1.00 | ||
| Factor 3: Over-arousal | 0.32 | 0.37 | 1.00 | |
| Factor 4: Social Anxiety | 0.13 | 0.12 | 0.25 | 1.00 |
Note: Shaded cells illustrate the highest factor loading (>0.50) for each item.
Using half of the full sample selected at random, CFA showed that the four factor solution fit the data significantly better (RMSEA = 0.04 90% CI: 0.02–0.05; RMR =0.08) than the one factor solution (RMSEA = 0.12 90% CI: 0.105–0.124; RMR=0.13) (EFA and CFA solutions are available on request).
Discussion
The current study examined anxiety symptoms in a large well-characterized sample of subjects with ASDs using the 20-item CASI-Anxiety scale. The study replicates and extends a previous study by Sukhodolsky and colleagues (2008), which used the same measure in a related (although smaller) sample. The relatively large and heterogenous sample permitted us to examine the anxiety rating at the item level, to explore the factor structure of the CASI-Anxiety and the endorsement of individual items across IQ. To our knowledge, this is the first study to examine the profile of youth with ASDs and high levels of anxiety on a dimensional measure.
The distribution and psychometric properties of the CASI-Anxiety scale in this sample were consistent with those of Sukhodolsky and colleagues (2008). The mean CASI anxiety score for intellectually disabled children was significantly lower compared to those with an IQ of 70 or above. Nonetheless, both IQ groups showed an approximately normal distribution of CASI Anxiety scores. The high internal consistency of the CASI-Anxiety items suggests that these items are measuring a similar construct. Furthermore, the low correlations between the CASI-Anxiety and the other behavioral scales suggest that this DSM-IV-based anxiety symptom list is measuring something distinct from hyperactivity, irritability, repetitive behavior, or adaptive functioning. The association with parent-rated ASD symptoms was also modest, suggesting that anxiety symptoms do not align closely with manifestations of ASD as measured on the CASI PDD scale. Compared to the children in the lowest quartile on the CASI Anxiety scale, however, those in the highest quartile showed a higher mean score on the CASI-PDD scale. Reports of increased ASD-like traits in typically-developing children with anxiety disorders suggest a possible bidirectional association of anxiety disorders and ASDs (Pine et al. 2008; Ivarsson and Melin 2008). This association seems especially relevant to social anxiety disorder and ASD. However, the current 20-item CASI Anxiety scale includes only 2 items of social anxiety. Given the limited coverage of social anxiety, fuller exploration of the social impairments and social anxiety in children with ASD awaits further study.
We observed that high scores on the CASI-Anxiety scale were associated with being verbal, having an IQ of 70 or above and showing high levels of inappropriate speech, irritability and hyperactivity. Children with the highest levels of anxiety also had higher parent-rated ASD severity scores than those who were less anxious. These associations could reflect the overall behavioral disturbance of children in this sample or suggest that anxiety may amplify other behavioral problems. It may also indicate that a combination of higher IQ, coupled with a more severe behavioral impairment poses a greater risk for anxiety difficulties. This is particularly interesting as irritability, ASD severity and hyperactivity are often associated with lower IQ rather than higher IQ – a paradox that warrants further investigation. The observation that children in the upper quartile on the CASI Anxiety scale had higher Vineland scores is consistent with previous findings showing positive associations between IQ and anxiety in ASDs (Gadow et al. 2005; Sukhodolsky et al. 2008; Weisbrot et al. 2005). Children with higher IQ (particularly coupled with high ASD severity) may have greater awareness of their social differences, but may remain unable to compensate effectively for their difficulties. Given the limited coverage of social anxiety on the current 20-item CASI, however, fuller exploration of the social impairments and social anxiety in children with ASD awaits further study.
Considering the individual items of the CASI-Anxiety, the most and least endorsed statements were the same in the high and low IQ groups. Items such as: ‘acts restless or edgy’, ‘has difficulty falling asleep’ and ‘is extremely tense and unable to relax’ are directly observable and were most commonly endorsed by parents. This result is consistent with previous findings (Witwer and Lecavalier 2010). Some aspects of social anxiety (e.g. ‘is more anxious in social situations than most children’) and separation anxiety (e.g. ‘is easily upset when separation is expected’) were also highly endorsed across IQ groups.
Items such as ‘worries about physical health’, ‘has nightmares about being separated from parents’ and ‘complains about feeling sick when separation is expected’ require inference by the parent or direct expression by the child. Given the difficulties that children with ASDs often have with communication, it is not surprising that these items were rarely endorsed at the clinical level (a score of 2 or 3) (by 3.6% and 4.3% of the full sample respectively). Other items relying on language (e.g. ‘complains about heart pounding’ and ‘worries that disaster will cause separation from parents’) were rarely endorsed by parents of children with intellectual disability. This observation is consistent with a previous study showing that intellectually disabled children with ASDs are less likely to express excessive worry (Witwer and Lecavalier 2010). The high language demand for items starting with ‘worries’ or ‘complains’ apparently limited the rate of endorsement in the lower IQ group, which, in turn, contributed to the lower CASI Anxiety mean score for the intellectually disabled group. Nonetheless, subjects with IQ of 70 or greater had significantly higher mean scores than the intellectually disabled group on the 10 scale items with low verbal demand. This suggests that, even when considering the more observable aspects of anxiety, higher functioning children were rated as exhibiting more anxiety than children with lower IQ.”
The factor structure in this sample suggests that anxiety may be multifactorial in children with ASDs. Although three factors corresponded to DSM-IV categories (Generalized Anxiety, Separation Anxiety and Social Anxiety), the fourth factor was less anxiety specific, encompassing ‘over-arousal’ symptoms such as restlessness and sleep difficulties. This factor analysis relied on a predetermined set of DSM-derived items. These current items are weighted toward separation anxiety (8 of 20 items) with inadequate coverage of social anxiety (2 of 20 items). Future adjustments may involve removal of rarely endorsed items (e.g. the 3 items endorsed by less than 5% of this sample) and addition of items capturing ASD-specific aspects of anxiety and emotional reactivity. Qualitative inquiry with parents may contribute to improved understanding on the manifestations of anxiety in children with ASDs across the IQ range.
There are several limitations of this study. First, this was a convenient sample of pediatric participants in clinical trials selected for specific behavioral difficulties. Therefore, although this was a relatively large and broad sample, the findings may not apply to the wider ASD population. Our findings on divergent validity suggest that the CASI-Anxiety scale is measuring a unique construct. However, we did not have another measure of anxiety (either from parents or additional informants) and consequently we do not have evidence of convergent validity. The small proportion of girls (15%) in the sample also hindered comparisons by gender.
In conclusion, our findings contribute to a growing literature regarding the manifestation and measurement of anxiety in children with ASDs. We observed that anxiety occurs across the full range of IQ. Children with an IQ below 70 have lower scores, in part because the items that rely on language are rarely endorsed and do not contribute to the total score. However, our findings suggest that the CASI-Anxiety scale represents a promising starting point for quantifying anxiety symptoms in this population. Further investigation is needed to determine whether an adapted version of this scale may be useful as an outcome measure for clinical trials.
Acknowledgments
The authors acknowledge Ann Wagner, Ph.D. and Louise Ritz, MBA at NIMH; James Robinson, MED, at NKI; Mark Davies, MPH at NY State Psychiatric Institute, Stacey Grinnon, MA at KAI Research, Inc; Deborah Hirtz PhD at the National Institute of Neurological Disorders and Stroke, Bethesda, Lisa Sullivan, PhD at Boston University; Fay Robinson, MPH at DMSTAT and James Dziura, PhD, Sunkyung Yu, MS, Yanhong Deng, MPH and Allison Gavaletz, BS at Yale University. The RUPP studies were funded by the following NIMH grants and contracts: N01MH70009 and U10MH66764 (Yale); N01MH70001 and U10MH66766 (Indiana University); N01MH80011 and U10MH66768 (Ohio State University); N01MH70010 (UCLA). This publication was also supported by the Yale Clinical and Translational Science Award (CTSA) UL1RR024139, Indiana University CTSA UL1 RR025761, and Ohio State University CTSA UL1 RR025755 from the National Center for Research Resources (NCRR). The STAART citalopram study was funded by NIH via the following center contracts: Mount Sinai School of Medicine: U54-MH066673; University of North Carolina at ChapelHill:U54-MH066418; University of California at Los Angeles: U54-MH068172; Yale University: U54-MH066494. Dartmouth Medical School and Boston University:U54- MH066398; and DM-STAT, Inc, Boston: U01-HD045023.
Abbreviations
- ASDs
Autism Spectrum Disorder
- PDD
Pervasive Developmental Disorder
- RRBI
Repetitive and restricted behaviors and interest
- RUPP
Research Units On Pediatric Psychopharmcology
- STAART
Studies to Advance Autism Research and Treatment
- CYBOCS-PDD
Children’s Yale-Brown Obsessive Compulsive Scale modified for Pervasive Developmental Disorders
Footnotes
Affiliations at time of study:
Drs Hallett, Scahill, Sukhodolsky, Ms Katsovich and Ms Cipriano are with the Child Study Center and School of Nursing, Yale University, New Haven, CT
Drs Aman and Lecavalier are with the Department of Psychology, Ohio State University, Columbus, OH
Dr. McCracken is with the Division of Child & Adolescent Psychiatry, Semel Institute for Neurosciences, UCLA School of Medicine, Los Angeles, CA
Dr. McDougle is with the Lurie Center for Autism, Massachusetts General Hospital for Children and Harvard Medical School, Boston, MA
Dr. Tierney is with the Department of Psychiatry, Kennedy Krieger Institute, Baltimore, MD;
Dr. King is with the Department of Psychiatry, Seattle Children’s Hospital, University of Washington, WA
Dr. Hollander is with the Albert Einstein College of Medicine and Montefiore Medical Center
Dr. Anagnostou is with the Bloorview Research Institute and the Department of Pediatrics, University of Toronto, Toronto, Ontario, Canada
Dr. Sikich is with the Department of Psychiatry, University of North Carolina at Chapel Hill, NC
Dr. Bregman is with the Department of Psychiatry, North Shore–Long Island Jewish Health System, Great Neck, NY
Dr. Donnelly is with the Department of Psychiatry, Dartmouth Medical School, Hanover, NH
Dr. Dukes is with DM-STAT, Inc, Malden and Department of Biostatistics, Boston University, Boston, MA
Dr. Vitiello is with the National Institute of Mental Health, Bethesda, MD
Dr. Gadow is with the Department of Psychiatry and Behavioral Science, State University of New York at Stony Brook, NY
Changes in author affiliation subsequent to the time of study
Dr Hallett is now at the Department of Psychology, Institute of Psychiatry, Kings College London, London.
Dr Scahill is now at the Marcus Autism Center, Emory University, GA
Disclosures: Dr. Scahill: Roche, consultant; Pfizer, consultant; Brachet, consultatnt, BioMarin, consultant. Shire, research support; Roche, research support; Pfizer, research support. Dr. Aman: Roche, consultant; Bristol-Meyers Squibb, consultant, research grant; Forest, consultant; Pfizer, consultant; Supernus, consultant; Johnson & Johnson, research grant. Dr. Gadow: Checkmate Plus, publisher of the Child and Adolescent Symptom Invetory-4; Dr. McDougle: Bristol-Myers Squibb, research grant, speaker’s bureau. Dr. McCracken: salary from UCLA, research support from NIH, Seaside Therapeutics, Roche, and Otsuka; consultant income from Novartis, BioMarin, PharmaNet, and Noven; speaker’s honoraria from the Tourette Syndrome Association; and research study drug supply from Shire; Dr. Arnold: AstraZeneca, advisory board; Biomarin, advisory board; CureMark, research funding; Lilly, research funding; Noven, advisory board; Seaside therapeutics, advisory board; Shire, research funding. Dr. Tierney: BioMarin, consultant. Dr. Donnelly: consultant for Eli Lilly Pharmaceutical Company, Abbott Pharmaceutical Company and Shire Pharmaceuticals. He has served on the Speaker’s Bureau for Eli Lilly, and Shire. He has received research funding from Eli Lilly. Dr. Hollander reports serving as a consultant to Neuropharm. Dr. King reports serving as a consultant to Biomarin and Neuropharm and as an unpaid consultant to Forest, Nastech, and Seaside Therapeutics. He has received or has pending research grant support from Neuropharm and Seaside Therapeutics. Dr. Sikich has received support from Bristol Myers Squibb and Pfizer, participated in clinical trials sponsored by Neuropharm, Curemark, Seaside Pharmaceuticals, and recieved medications or software Janssen Pharmaceutica, Eli Lilly, Pfizer, Bristol Myers Squibb and Positscience. Dr. Hallett, Dr. Lecavalier, Dr. Sukhodolsky, Dr. Vitiello, Ms Katsovich Dr. Anagnostou, Dr. Bregman, and Dr. Dukes report no financial relationships with commercial interests.
Contributor Information
Dr. Victoria Hallett, Child Study Center and School of Nursing, Yale University, New Haven, CT.
Dr. Luc Lecavalier, Department of Psychology, Ohio State University, Columbus, OH.
Dr. Denis G. Sukhodolsky, Child Study Center and School of Nursing, Yale University, New Haven, CT.
Ms. Noreen Cipriano, Child Study Center and School of Nursing, Yale University, New Haven, CT.
Dr. Michael G. Aman, Department of Psychology, Ohio State University, Columbus, OH.
Dr. James T. McCracken, Division of Child & Adolescent Psychiatry, Semel Institute for Neurosciences, UCLA School of Medicine, Los Angeles, CA.
Dr. Christopher J. McDougle, Lurie Center for Autism, Massachusetts General Hospital for Children and Harvard Medical School, Boston, MA.
Dr. Elaine Tierney, Department of Psychiatry, Kennedy Krieger Institute, Baltimore, MD.
Dr. Bryan H. King, Department of Psychiatry, Seattle Children’s Hospital, University of Washington, WA.
Dr. Eric Hollander, Albert Einstein College of Medicine and Montefiore Medical Center.
Dr. Linmarie Sikich, Department of Psychiatry, University of North Carolina at Chapel Hill, NC.
Dr. Joel Bregman, Department of Psychiatry, North Shore–Long Island Jewish Health System, Great Neck, NY.
Dr. Evdokia Anagnostou, Bloorview Research Institute and the Department of Pediatrics, University of Toronto, Toronto, Ontario, Canada.
Dr. Craig Donnelly, Department of Psychiatry, Dartmouth Medical School, Hanover, NH.
Ms. Lily Katsovich, Child Study Center and School of Nursing, Yale University, New Haven, CT.
Dr. Kimberly Dukes, DM-STAT, Inc, Malden and Department of Biostatistics, Boston University, Boston, MA.
Dr. Benedetto Vitiello, National Institute of Mental Health, Bethesda, MD.
Dr. Kenneth Gadow, Department of Psychiatry and Behavioral Science, State University of New York at Stony Brook, NY.
Dr. Lawrence Scahill, Marcus Center, Emory University.
References
- Aman MG, McDougle CJ, Scahill L, Handen B, Arnold LE, Johnson C, et al. Medication and Parent Training in Children With Pervasive Developmental Disorders and Serious Behavior Problems: Results From a Randomized Clinical Trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2009 doi: 10.1097/CHI.0b013e3181bfd669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aman MG, Singh NN, Stewart AW, Field CJ. The aberrant behavior checklist: a behavior rating scale for the assessment of treatment effects. American journal of mental deficiency. 1985;89(5):485–491. [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3. Washington, DC: American Psychiatric Association; 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Brown EC, Aman MG, Havercamp SM. Factor analysis and norms for parent ratings on the Aberrant Behavior Checklist-Community for young people in special education. Research in developmental disabilities. 2002;23(1):45–60. doi: 10.1016/s0891-4222(01)00091-9. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R, Tateneni K, Mels G. CEFA: Comprehensive Exploratory Factor Analysis, Version 3.04. 2009. Computer Software and Manual. [Google Scholar]
- Canitano R. Self injurious behavior in autism: clinical aspects and treatment with risperidone. Journal of neural transmission. 2006;113(3):425–431. doi: 10.1007/s00702-005-0337-x. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Egger HL, Angold A. The developmental epidemiology of anxiety disorders: Phenomenology, prevalence, and comorbidity. Child and adolescent psychiatric clinics of North America. 2005;14(4):631. doi: 10.1016/j.chc.2005.06.003. [DOI] [PubMed] [Google Scholar]
- Gadow KD, DeVincent CJ, Pomeroy J, Azizian A. Psychiatric symptoms in preschool children with PDD and clinic and comparison samples. Journal of autism and developmental disorders. 2004;34(4):379–393. doi: 10.1023/b:jadd.0000037415.21458.93. [DOI] [PubMed] [Google Scholar]
- Gadow KD, Devincent CJ, Pomeroy J, Azizian A. Comparison of DSM-IV symptoms in elementary school-age children with PDD versus clinic and community samples. Autism : the international journal of research and practice. 2005;9(4):392–415. doi: 10.1177/1362361305056079. [DOI] [PubMed] [Google Scholar]
- Gadow KD, Sprafkin J. Adolescent symptom inventory-4 norms manual. Stony Brook, NY: Checkmate Plus; 1998. Stony Brook, NY: Checkmate Plus. [Google Scholar]
- Gadow KD, Sprafkin J. Child symptom inventory-4 screening and norms manual. Stony Brook, NY: Checkmate Plus; 2002. [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale-Brown Obsessive Compulsive Scale.1. Development, Use, and Reliability. Archives of General Psychiatry. 1989;46(11):1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Ivarsson T, Melin K. Autism spectrum traits in children and adolescents with obsessive-compulsive disorder (OCD) Journal of anxiety disorders. 2008;22(6):969–978. doi: 10.1016/j.janxdis.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Jensen JA, Armstrong RJ. Slosson intelligence test for children and adults. East Aurora, NY: Slosson Educational Publications; 1985. [Google Scholar]
- Jöreskog KG, Sörbom D. LISREL 8.7 for Windows [Computer Software] Lincolnwood, IL: Scientific Software International, Inc; 2004. [Google Scholar]
- Kanner L. Autistic Disturbances of Affective Contact. Nervous Child. 1943;2(3):217–250. [PubMed] [Google Scholar]
- Kim JA, Szatmari P, Bryson SE, Streiner DL, Wilson FJ. The Prevalence of Anxiety and Mood Problems among Children with Autism and Asperger Syndrome. Autism : the international journal of research and practice. 2000;4(2):117–132. [Google Scholar]
- King BH, Hollander E, Sikich L, McCracken JT, Scahill L, Bregman JD, et al. Lack of efficacy of citalopram in children with autism spectrum disorders and high levels of repetitive behavior: citalopram ineffective in children with autism. Archives of General Psychiatry. 2009;66(6):583–590. doi: 10.1001/archgenpsychiatry.2009.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Couteur A, Lord C, Rutter M. Autism Diagnostic Interview-Revised. Los Angeles: Western Psychological Services; 2003. [Google Scholar]
- Lecavalier L. Behavioral and emotional problems in young people with pervasive developmental disorders: relative prevalence, effects of subject characteristics, and empirical classification. Journal of autism and developmental disorders. 2006;36(8):1101–1114. doi: 10.1007/s10803-006-0147-5. [DOI] [PubMed] [Google Scholar]
- Marshburn EC, Aman MG. Factor Validity and Norms for the Aberrant Behavior Checklist in a Community Sample of Children with Mental-Retardation. Journal of autism and developmental disorders. 1992;22(3):357–373. doi: 10.1007/BF01048240. [DOI] [PubMed] [Google Scholar]
- Mazurek MO, Kanne SM. Friendship and internalizing symptoms among children and adolescents with ASD. Journal of autism and developmental disorders. 2010;40(12):1512–1520. doi: 10.1007/s10803-010-1014-y. [DOI] [PubMed] [Google Scholar]
- McDougle CJ, Scahill L, Aman MG, McCracken JT, Tierney E, Davies M, et al. Risperidone for the core symptom domains of autism: results from the study by the autism network of the research units on pediatric psychopharmacology. The American journal of psychiatry. 2005;162(6):1142–1148. doi: 10.1176/appi.ajp.162.6.1142. [DOI] [PubMed] [Google Scholar]
- Mullen E. Mullen scales of early learning. Circle Pines, MN: American Guidance Service; 1995. [Google Scholar]
- Pine DS, Guyer AE, Goldwin M, Towbin KA, Leibenluft E. Autism spectrum disorder scale scores in pediatric mood and anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(6):652–661. doi: 10.1097/CHI.0b013e31816bffa5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Research Units on Pediatric Psychopharmacology (RUPP) Autism Network. Risperidone in children with autism and serious behavioral problems. New England Journal of Medicine. 2002;347(5):314–321. doi: 10.1056/NEJMoa013171. [DOI] [PubMed] [Google Scholar]
- Research Units on Pediatric Psychopharmacology (RUPP) Autism Network. Randomized, controlled, crossover trial of methylphenidate in pervasive developmental disorders with hyperactivity. Archives of General Psychiatry. 2005;62(11):1266–1274. doi: 10.1001/archpsyc.62.11.1266. [DOI] [PubMed] [Google Scholar]
- Roid GH, Miller LJ. Leiter international performance scale-revised. Wood Dale, IL: Stoelting; 1997. [Google Scholar]
- Scahill L, McCracken JT, Bearss K, Robinson F, Hollander E, King B, et al. Design and subject characteristics in the federally-funded citalopram trial in children with pervasive developmental disorders. Journal of autism and developmental disorders. 2012;42(3):432–440. doi: 10.1007/s10803-011-1251-8. [DOI] [PubMed] [Google Scholar]
- Scahill L, McDougle CJ, Williams SK, Dimitropoulos A, Aman MG, McCracken JT, et al. Children’s Yale-Brown Obsessive Compulsive Scale modified for pervasive developmental disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(9):1114–1123. doi: 10.1097/01.chi.0000220854.79144.e7. [DOI] [PubMed] [Google Scholar]
- Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI, King RA, Goodman WK, et al. Children’s Yale-Brown Obsessive Compulsive Scale: reliability and validity. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(6):844–852. doi: 10.1097/00004583-199706000-00023. [DOI] [PubMed] [Google Scholar]
- Sparrow SS, Balla DA, Cicchetti DV. Vineland adaptive behavior scales. Circle Pines, MN: American Guidance Service; 1984. [Google Scholar]
- Sprafkin J, Gadow KD, Salisbury H, Schneider J, Loney J. Further evidence of reliability and validity of the Child Symptom Inventory-4: Parent checklist in clinically referred boys. Journal of Clinical Child and Adolescent Psychology. 2002;31(4):513–524. doi: 10.1207/S15374424JCCP3104_10. [DOI] [PubMed] [Google Scholar]
- Sukhodolsky DG, Scahill L, Gadow KD, Arnold LE, Aman MG, McDougle CJ, et al. Parent-rated anxiety symptoms in children with pervasive developmental disorders: Frequency and association with core autism symptoms and cognitive functioning. Journal of abnormal child psychology. 2008;36(1):117–128. doi: 10.1007/s10802-007-9165-9. [DOI] [PubMed] [Google Scholar]
- van Steensel FJ, Bogels SM, Perrin S. Anxiety Disorders in Children and Adolescents with Autistic Spectrum Disorders: A Meta-Analysis. Clinical child and family psychology review. 2011 doi: 10.1007/s10567-011-0097-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Wechsler preschool and primary scale of intelligence-revised. San Antonio, TX: The Psychological Corporation; 1989. [Google Scholar]
- Wechsler D. Wechsler intelligence scale for children. 3. San Antonio, TX: The Psychological Corporation; 1991. [Google Scholar]
- Weisbrot DM, Gadow KD, DeVincent CJ, Pomeroy J. The presentation of anxiety in children with pervasive developmental disorders. Journal of child and adolescent psychopharmacology. 2005;15(3):477–496. doi: 10.1089/cap.2005.15.477. [DOI] [PubMed] [Google Scholar]
- White SW, Oswald D, Ollendick T, Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clinical psychology review. 2009;29(3):216–229. doi: 10.1016/j.cpr.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witwer AN, Lecavalier L. Validity of Comorbid Psychiatric Disorders in Youngsters with Autism Spectrum Disorders. Journal of Developmental and Physical Disabilities. 2010;22(4):367–380. [Google Scholar]