Abstract
Objective To assess the risk of maternal, fetal, and neonatal outcomes associated with the administration of an MF59 adjuvanted A/H1N1 vaccine during pregnancy.
Design Historical cohort study.
Setting Singleton pregnancies of the resident population of the Lombardy region of Italy.
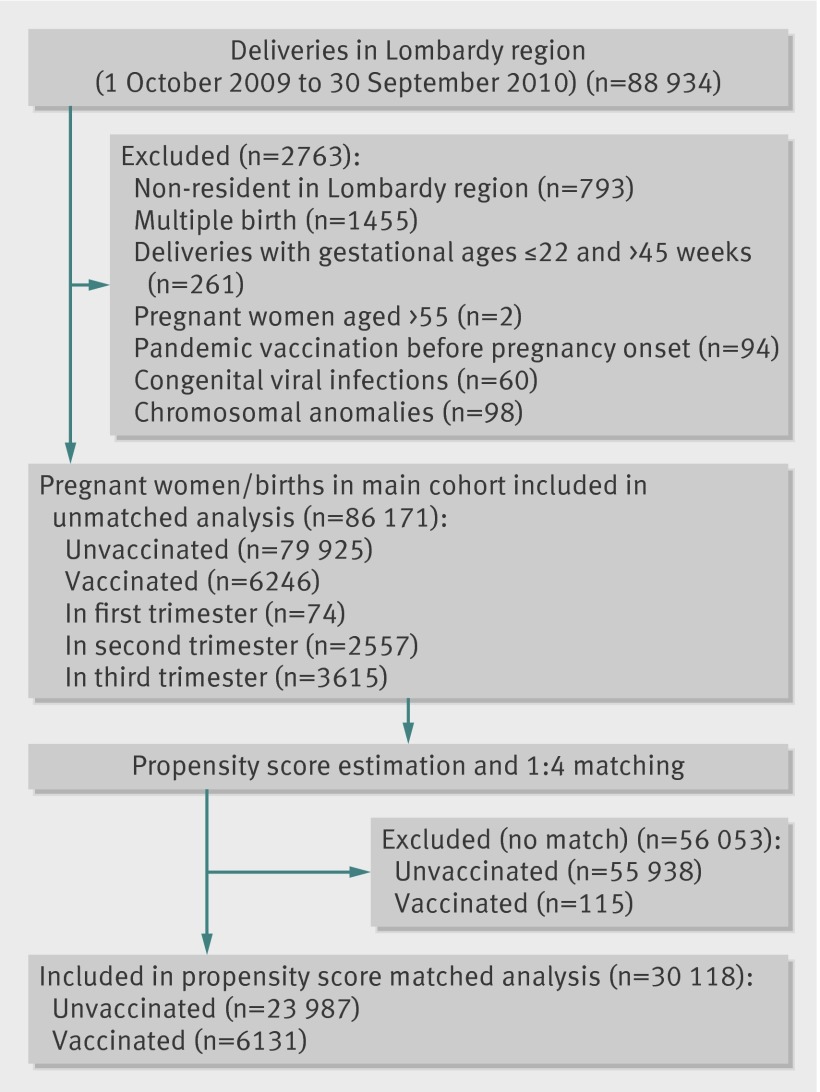
Participants All deliveries between 1 October 2009 and 30 September 2010. Data on exposure to A/H1N1 pandemic vaccine, pregnancy, and birth outcomes were retrieved from regional databases. Vaccinated and non-vaccinated women were compared in a propensity score matched analysis to estimate risks of adverse outcomes.
Main outcome measures Main maternal outcomes included type of delivery, admission to intensive care unit, eclampsia, and gestational diabetes; fetal and neonatal outcomes included perinatal deaths, small for gestational age births, and congenital malformations.
Results Among the 86 171 eligible pregnancies, 6246 women were vaccinated (3615 (57.9%) in the third trimester and 2557 (40.9%) in the second trimester). No difference was observed in terms of spontaneous deliveries (adjusted odds ratio 1.02, 95% confidence interval 0.96 to 1.08) or admissions to intensive care units (0.95, 0.47 to 1.88), whereas a limited increase in the prevalence of gestational diabetes (1.26, 1.04 to 1.53) and eclampsia (1.19, 1.04 to 1.39) was seen in vaccinated women. Rates of fetal and neonatal outcomes were similar in vaccinated and non-vaccinated women. A slight increase in congenital malformations, although not statistically significant, was present in the exposed cohort (1.14, 0.99 to 1.31).
Conclusions Our findings add relevant information about the safety of the MF59 adjuvanted A/H1N1 vaccine in pregnancy. Residual confounding may partly explain the increased risk of some maternal outcomes. Meta-analysis of published studies should be conducted to further clarify the risk of infrequent outcomes, such as specific congenital malformations.
Introduction
In June 2009 the World Health Organization announced that the diffusion of influenza A/H1N1 had reached pandemic status.1 A specific question concerned the effect of the infection during pregnancy. Initial reports highlighted the possibility of severe complications in younger age groups in comparison with previous influenza seasons;2 3 moreover, pregnant women were considered to be at higher risk of admission to hospital or to an intensive care unit and of maternal death.4 5 The influenza infection also had a negative effect on birth outcomes, in terms of an increased risk of prematurity, low birth weight, and perinatal mortality.6 7 8 9 Moreover, a potential role in the development of congenital malformations was suggested.9 10 11
Although not previously recommended on a large scale, vaccination against influenza during the second and third pregnancy trimester was deemed an appropriate intervention to prevent maternal morbidity and mortality and to reduce the risk of adverse fetal outcomes.8 In Italy, all women in the second or third pregnancy trimester were advised to have the pandemic vaccine, which was available free of charge within the national health service.12
Given the paucity of data on the safety of the vaccination during pregnancy, regulatory authorities, such as the European Medicines Agency, the European Centre for Disease Prevention and Control, and the Heads of Medicines Agencies, suggested strengthening the surveillance systems and conducting epidemiological studies on immunised women.13 Thus, several studies, sponsored by companies and public institutions, were planned worldwide.14 15 16 17 18 19 20 21 22 23 24 25
A specific question concerned the potential role of the different adjuvants included in each vaccine.13 26 27 In Italy, only the A/H1N1 MF59 adjuvanted formulation (Focetria, manufactured by Novartis) was administered to the population. With the objective of estimating the risk of adverse outcomes during pregnancy, in both mothers and newborns, in association with the pandemic vaccination, we carried out a cohort study in the largest Italian region (Lombardy), the resident population of which amounts to around 10 million inhabitants.
Methods
Study population and design
We retrieved all deliveries in women resident in the Lombardy region, occurring in public or private institutions as well as at home, through the regional birth registry (we included stillbirths if the gestational age exceeded 180 days). The study population included all singleton pregnancies (live births and stillbirths) between 1 October 2009 and 30 September 2010, in women aged at least 12 and up to 55 years, whose delivery took place between 23 and 45 weeks of gestation. In case of multiplicity during the study period, we included only the first pregnancy.
Pregnant women who were immunised with the A/H1N1 pandemic vaccine were eligible for the vaccinated (exposed) cohort. All other pregnant women were eligible for the non-vaccinated (unexposed) cohort.
We excluded pregnancies from the cohort if either chromosomal aberrations or congenital viral infections were reported in the birth registry (supplementary table A). We also excluded women if the pandemic vaccination was administered before the start of pregnancy. We estimated the onset of pregnancy by subtracting the gestational age (weeks of amenorrhoea) from the date of delivery (both types of data are reported in the birth registry). We did not include voluntary abortions and miscarriages (pregnancy loss before 180 days of amenorrhoea) in the study, as the information on gestational age is not recorded.
Exposure to pandemic vaccination
The pandemic vaccine was available only through the vaccination centres of the local health units, which were also in charge of recording the information on immunised patients and date of administration. As most vaccines were administered before the end of 2009, we restricted the study period for ascertainment of exposure to between the beginning of the vaccination campaign (1 October 2009) and 31 March 2010.
We considered pregnant women to be exposed to the vaccine from the day of vaccination. We calculated the gestational age at vaccination (index date) after having determined the onset of pregnancy.
Outcomes
We identified pregnancy and neonatal outcomes. Complications of pregnancy included pre-eclampsia/eclampsia (called eclampsia hereafter), gestational diabetes, in-hospital maternal death (deaths during labour or delivery occurring in a healthcare institution), admission to intensive care unit, and type of delivery. Perinatal deaths comprised stillbirths and in-hospital death of live newborns. We defined stillbirth, according to the Italian legal definition, as the delivery of a dead fetus after 180 days of amenorrhoea. Neonatal outcomes included small for gestational age neonates (defined as live newborns with birth weight below the 10th centile for their gestational age within the cohort of live births only), admission to neonatal intensive care unit, occurrence of neonatal reanimation, and congenital malformations. We identified newborns as having a congenital malformation if a compatible code, according to ICD-9 (international classification of diseases, 9th revision), was present in either the medical birth registry or the hospital discharge form of the neonate. We retained for the analysis only congenital malformations classified according to EUROCAT (European surveillance of congenital anomalies) guidelines.28 We also developed a composite neonatal morbidity outcome with the aim of identifying potential fetal stress during delivery. The composite outcome was based on the presence of any of the following clinical information/diagnoses: very low five minute Apgar score (≤3), acute respiratory distress syndrome, asphyxia, intraventricular haemorrhage, and acute necrotising enterocolitis. Supplementary table B gives details about outcome definitions.
Source of data and potential confounders
We used only routinely collected information in the study and abstracted the following regional databases: birth registry, pandemic vaccination, hospital discharges, drug prescriptions, and clinical investigations. All databases were linkable through a unique, anonymised, personal identifier.
We used the birth registry of the Lombardy region, which is filled in for each delivery, to identify the cohort of pregnant women and to abstract information on parents (for example, education and occupational status), pregnancy (for example, gestational age and parity), and deliveries (for example, weight and Apgar score). The registry also includes a section dedicated to stillbirths and congenital malformations.
The hospital discharge database includes all hospital discharge forms for both mothers and newborns. We used the following information: age, dates of admission and discharge, diagnoses and procedures according to the ICD-9, internal transfer (such as admission to intensive care unit), mother/newborn discharge status (that is, dead/alive).
The drug prescription database contains the information on prescriptions issued to outpatients within the regional health service, and we obtained information on date of prescription, drug, and number of packages. The vaccination database contains information on patients who received the pandemic vaccine and the date of vaccination. We used the clinical investigation database to obtain information on women who were exempted from copayments (disease allowances) because of low income or presenting chronic diseases (such as, diabetes, hypertension, or epilepsy).
We took five main categories of potential confounders into account: demographic characteristics of the mothers, socioeconomic status, history of previous pregnancy(ies), history of selected comorbidities and drugs at pregnancy onset, and healthcare use. Supplementary table C gives details on the specific confounders included in the study. No data were available on alcohol use, smoking status, body mass index, over the counter drugs, and multivitamin supplementation.
Statistical analysis
We reported patients’ characteristics by vaccine exposure status. We compared the two groups by using a t test for continuous variables and a χ2 test for categorical ones. Given the large number of potential confounders, we used a propensity score model for multivariate analysis. We applied logistic regression to estimate the probability of each pregnant woman receiving A/H1N1 vaccination versus remaining unvaccinated. We tested all variables previously mentioned as potential confounders and included in the propensity score those with P≤0.05: age, nationality, education, mother’s occupational status, mother’s civil status, previous deliveries, previous live births, previous caesarean deliveries, comorbidities and drugs at pregnancy onset (pulmonary disease, cardiovascular disease, diabetes, antidepressants, antibacterials, autoimmune disease, immunodeficiency condition), total number of different drugs used in the six months before pregnancy onset, and number of deliveries occurring in the hospital. As missing data for the variables included in the propensity score affected 1.3% of the study population, we included in the matched analysis only women with a complete dataset.
We matched women exposed and unexposed to vaccination by propensity score (at the fourth decimal digit) and by gestational age (that is, unexposed women must have had a gestational age at least equal to the gestational age at vaccination of the corresponding exposed woman). We matched up to four unexposed women to each exposed one, and we excluded exposed women with no match from the matched analyses.
We took the decision to conduct the study in the overall population of the Lombardy region as part of the surveillance on the safety of the pandemic vaccine. We identified no predefined hypothesis and did no formal estimate of the sample size.
We did both matched and unmatched analyses. In the unmatched analysis, we considered all outcomes occurring from pregnancy onset to delivery. In the matched analysis, we counted only outcomes from the vaccination date to delivery and from the corresponding index date in the non-vaccinated cohort. We used a conditional logistic regression model to estimate crude and adjusted odds ratios, with 95% confidence intervals. We used Stata software (version 11.2) for the statistical analyses.
We also did a pre-planned sensitivity analysis on the matched cohort to investigate the potential protective role of the “healthy vaccinee effect.” In this analysis, we excluded all outcomes occurring in the two weeks after the index date. The risk estimates of the sensitivity analysis were expected to move towards the null in case of a confounding role of the “healthy vaccinee effect.”
Results
Study cohort
Between 1 October 2009 and 30 September 2010, 88 934 deliveries occurred in the Lombardy region; we excluded 2763 of these, mainly because of multiple births and residency outside the region, leaving a study cohort of 86 171 women (figure). About 7% of the cohort (6246 women) received the A/H1N1 vaccine, mostly in the month of November 2009 (supplementary figure). The vaccination was administered either in the third (3615 women; 57.9%) or second trimester of pregnancy (2557 women; 40.9%), and the median gestational age at vaccination was 27 weeks. Only 74 (1.2%) women were vaccinated in the first trimester.
Flow chart of women included in study cohort
Immunised women were more frequently of Italian nationality, with a higher socioeconomic status, a greater prevalence of concomitant diseases (such as cardiovascular diseases, pulmonary diseases, or diabetes), and more drug prescriptions before the onset of pregnancy (tables 1 and 2). After matching by propensity score and gestational age, we included 6131 exposed and 23 987 unexposed women in the analysis; the two groups were well balanced with respect to baseline characteristics (tables 1 and 2).
Table 1.
Demographics and socioeconomic status. Values are numbers (percentages) unless stated otherwise
| Characteristics | Unmatched cohort | Matched cohort | |||||
|---|---|---|---|---|---|---|---|
| Unvaccinated (n=79 925) | Vaccinated (n=6246) | P value | Unvaccinated (n=23 987) | Vaccinated (n=6131) | P value | ||
| No of deliveries in 2009 in hospital: | |||||||
| <500 | 3425 (4.3) | 208 (3.3) | <0.001 | 815 (3.4) | 208 (3.4) | 0.77 | |
| 500-999 | 15 259 (19.1) | 965 (15.5) | 3872 (16.1) | 956 (15.6) | |||
| 1000-1499 | 18 328 (22.9) | 1217 (19.5) | 4736 (19.7) | 1213 (19.8) | |||
| ≥1500 | 42 913 (53.7) | 3856 (61.7) | 14 564 (60.7) | 3754 (61.2) | |||
| Mean (SD) age at delivery, years | 31.7 (5.3) | 32.6 (5.0) | <0.001 | 32.5 (5.0) | 32.6 (5.0) | 0.35 | |
| Age group at delivery: | |||||||
| <20 | 1059 (1.3) | 58 (0.9) | <0.001 | 205 (0.9) | 57 (0.9) | 0.84 | |
| 20-24 | 7385 (9.2) | 354 (5.7) | 1440 (6.0) | 352 (5.7) | |||
| 25-29 | 17 557 (22.0) | 1168 (18.7) | 4588 (19.1) | 1147 (18.7) | |||
| 30-34 | 28 091 (35.2) | 2331 (37.3) | 8829 (36.8) | 2298 (37.5) | |||
| 35-39 | 21 011 (26.3) | 1892 (30.3) | 7274 (30.3) | 1847 (30.1) | |||
| 40-44 | 4632 (5.8) | 422 (6.8) | 1588 (6.6) | 410 (6.7) | |||
| ≥45 | 190 (0.2) | 21 (0.3) | 63 (0.3) | 20 (0.3) | |||
| Italian nationality | 56 605 (70.8) | 4951 (79.3) | <0.001 | 18 996 (79.2) | 4853 (79.2) | 0.95 | |
| Education (mother and/or father): | |||||||
| University degree | 24 576 (30.8) | 2398 (38.4) | <0.001 | 8989 (37.5) | 2342 (38.2) | 0.49 | |
| Secondary school | 54 130 (67.7) | 3790 (60.7) | 14 836 (61.9) | 3744 (61.1) | |||
| Primary school/none | 939 (1.2) | 45 (0.7) | 162 (0.7) | 45 (0.7) | |||
| Mother’s occupational status: | |||||||
| Employed | 54 889 (68.7) | 4668 (74.7) | <0.001 | 18 058 (75.3) | 4592 (74.9) | 0.93 | |
| Unemployed/seeking first occupation | 3551 (4.4) | 245 (3.9) | 922 (3.8) | 241 (3.9) | |||
| Housewife | 20 520 (25.7) | 1269 (20.3) | 4816 (20.1) | 1250 (20.4) | |||
| Student/other | 773 (1.0) | 48 (0.8) | 191 (0.8) | 48 (0.8) | |||
| Mother’s civil status at delivery: | |||||||
| Single | 18 216 (22.8) | 1259 (20.2) | <0.001 | 4961 (20.7) | 1249 (20.4) | 0.94 | |
| Married | 57 555 (72.0) | 4668 (74.7) | 18 028 (75.2) | 4620 (75.4) | |||
| Separated/divorced/widowed | 2475 (3.1) | 200 (3.2) | 751 (3.1) | 198 (3.2) | |||
| Not declared | 936 (1.2) | 66 (1.1) | 247 (1.0) | 64 (1.0) | |||
| Father’s occupational status: | |||||||
| Employed | 74 167 (92.8) | 5847 (93.6) | <0.01 | 22 509 (93.8) | 5748 (93.8) | 0.28 | |
| Unemployed/seeking first occupation | 2142 (2.7) | 135 (2.2) | 492 (2.1) | 133 (2.2) | |||
| Student/other | 281 (0.4) | 14 (0.2) | 79 (0.3) | 13 (0.2) | |||
| Low income allowance | 1840 (2.3) | 154 (2.5) | 0.40 | 505 (2.1) | 149 (2.4) | 0.12 | |
| Consanguinity between mother and father (relationship of fourth, fifth, or sixth degree) | 888 (1.1) | 46 (0.7) | 0.006 | 270 (1.1) | 46 (0.8) | 0.01 | |
Table 2.
Pregnancy history and risk factors. Values are numbers (percentages) unless stated otherwise
| Characteristics | Unmatched cohort | Matched cohort | |||||
|---|---|---|---|---|---|---|---|
| Unvaccinated (n=79 925) | Vaccinated (n=6246) | P value | Unvaccinated (n=23 987) | Vaccinated (n=6131) | P value | ||
| Previous conceptions | 46 455 (58.1) | 3878 (62.1) | <0.001 | 14 721 (61.4) | 3797 (61.9) | 0.42 | |
| Previous delivery(ies) (parity): | |||||||
| 0 | 43 933 (55.0) | 3159 (50.6) | <0.001 | 12 267 (51.1) | 3115 (50.8) | 0.90 | |
| 1 | 26 904 (33.7) | 2339 (37.5) | 8891 (37.1) | 2286 (37.3) | |||
| 2 | 6841 (8.6) | 578 (9.3) | 2218 (9.2) | 565 (9.2) | |||
| ≥3 | 2247 (2.8) | 170 (2.7) | 611 (2.6) | 165 (2.7) | |||
| Live births: | |||||||
| 1 | 27 039 (33.8) | 2358 (37.8) | <0.001 | 8967 (37.4) | 2302 (37.6) | 0.94 | |
| ≥2 | 8985 (11.2) | 747 (12.0) | 2832 (11.8) | 729 (11.9) | |||
| Stillbirths: | |||||||
| 0 | 79 410 (99.4) | 6202 (99.3) | 0.57 | 23 828 (99.3) | 6089 (99.3) | 0.85 | |
| ≥1 | 515 (0.6) | 44 (0.7) | 159 (0.7) | 42 (0.7) | |||
| Spontaneous abortions: | |||||||
| 0 | 67 057 (83.9) | 5118 (81.9) | <0.001 | 19 829 (82.7) | 5020 (81.9) | 0.35 | |
| 1 | 10 104 (12.6) | 870 (13.9) | 3224 (13.4) | 861 (14.0) | |||
| ≥2 | 2764 (3.5) | 258 (4.1) | 934 (3.9) | 250 (4.1) | |||
| Voluntary abortions: | |||||||
| 0 | 75 636 (94.6) | 5934 (95.0) | 0.20 | 22 774 (94.9) | 5822 (95.0) | 0.96 | |
| ≥1 | 4289 (5.4) | 312 (5.0) | 1213 (5.1) | 309 (5.0) | |||
| Previous caesarean deliveries: | |||||||
| 0 | 71 548 (89.5) | 5472 (87.6) | <0.001 | 21 103 (88.0) | 5387 (87.9) | 0.94 | |
| 1 | 7127 (8.9) | 679 (10.9) | 2533 (10.6) | 651 (10.6) | |||
| ≥2 | 1250 (1.6) | 95 (1.5) | 351 (1.5) | 93 (1.5) | |||
| Comorbidities and drugs at pregnancy onset: | |||||||
| Pulmonary diseases | 3055 (3.8) | 379 (6.1) | <0.001 | 1197 (5.0) | 361 (5.9) | 0.01 | |
| Cardiovascular disease | 1788 (2.2) | 218 (3.5) | <0.001 | 696 (2.9) | 197 (3.2) | 0.20 | |
| Haematological disease | 105 (0.1) | 12 (0.2) | 0.2 | 36 (0.2) | 11 (0.2) | 0.60 | |
| Diabetes | 258 (0.3) | 38 (0.6) | <0.001 | 94 (0.4) | 28 (0.5) | 0.48 | |
| Neurological and psychiatric diseases | 560 (0.7) | 65 (1.0) | 0.1 | 207 (0.9) | 63 (1.0) | 0.22 | |
| Inflammatory bowel disease/intestinal anti-inflammatory agents | 242 (0.3) | 25 (0.4) | 0.2 | 84 (0.4) | 24 (0.4) | 0.63 | |
| Immunosuppressive drugs | 53 (0.1) | 11 (0.2) | 0.002 | 15 (0.1) | 10 (0.2) | 0.02 | |
| Antidepressants | 1273 (1.6) | 155 (2.5) | <0.001 | 518 (2.2) | 138 (2.3) | 0.66 | |
| Antiepileptics | 317 (0.4) | 29 (0.5) | 0.4 | 126 (0.5) | 27 (0.4) | 0.40 | |
| Drugs for gastrointestinal reflux disease | 2339 (2.9) | 246 (3.9) | <0.001 | 854 (3.6) | 239 (3.9) | 0.21 | |
| Contraceptive drugs | 1847 (2.3) | 155 (2.5) | 0.4 | 604 (2.5) | 150 (2.5) | 0.75 | |
| Drugs for human fertilisation | 3134 (3.9) | 345 (5.5) | <0.001 | 1180 (4.9) | 333 (5.4) | 0.10 | |
| Non-steroidal anti-inflammatory drugs | 2146 (2.7) | 219 (3.5) | <0.001 | 748 (3.1) | 211 (3.4) | 0.20 | |
| Antibacterial for systemic use | 16 794 (21.0) | 1712 (27.4) | <0.001 | 6305 (26.3) | 1669 (27.2) | 0.14 | |
| Thyroid disease | 1646 (2.1) | 172 (2.8) | <0.001 | 603 (2.5) | 161 (2.6) | 0.62 | |
| Folic acid before pregnancy onset | 2540 (3.2) | 268 (4.3) | <0.001 | 933 (3.9) | 260 (4.2) | 0.21 | |
| Folic acid during first trimester | 1589 (2.0) | 418 (6.7) | <0.001 | 543 (2.3) | 406 (6.6) | <0.001 | |
| Iron supplementation | 1110 (1.4) | 118 (1.9) | 0.001 | 364 (1.5) | 116 (1.9) | 0.04 | |
| Autoimmune disease | 740 (0.9) | 99 (1.6) | <0.001 | 298 (1.2) | 89 (1.5) | 0.19 | |
| Immunodeficiency conditions | 537 (0.7) | 69 (1.1) | <0.001 | 207 (0.9) | 62 (1.0) | 0.27 | |
| Rare diseases | 293 (0.4) | 29 (0.5) | 0.2 | 98 (0.4) | 29 (0.5) | 0.49 | |
| Use of medically assisted reproduction: | 901 (1.1) | 103 (1.6) | <0.001 | 345 (1.4) | 100 (1.6) | 0.26 | |
| Type of medically assisted reproduction technique: | |||||||
| Drug treatment to induce ovulation | 70 (0.1) | 16 (0.3) | <0.001 | 34 (0.1) | 14 (0.2) | 0.29 | |
| Intrauterine insemination | 114 (0.1) | 7 (0.1) | 45 (0.2) | 7 (0.1) | |||
| Gamete intrafallopian transfer | 7 (0.01) | 0 | 1 (0.00) | 0 | |||
| Fertilisation in vitro and embryo transfer | 263 (0.3) | 28 (0.5) | 89 (0.4) | 27 (0.4) | |||
| Intracytoplasmatic sperm injection | 406 (0.5) | 46 (0.7) | 165 (0.7) | 46 (0.8) | |||
| Other techniques | 41 (0.1) | 6 (0.1) | 11 (0.1) | 6 (0.1) | |||
| Previous hospital admission: | |||||||
| 0 | 65 970 (82.5) | 5024 (80.4) | <0.001 | 19 520 (81.4) | 4940 (80.6) | 0.25 | |
| 1 | 11 700 (14.6) | 996 (16.0) | 3657 (15.2) | 974 (15.9) | |||
| 2 | 1645 (2.1) | 168 (2.7) | 565 (2.4) | 162 (2.6) | |||
| ≥3 | 610 (0.8) | 58 (0.9) | 245 (1.0) | 55 (0.9) | |||
| Drugs used in previous six months: | |||||||
| 0 | 48 921 (61.2) | 3217 (51.5) | <0.001 | 12 816 (53.4) | 3179 (51.9) | 0.01 | |
| 1 | 17 082 (21.4) | 1496 (24.0) | 5833 (24.3) | 1480 (24.1) | |||
| 2 | 7514 (9.4) | 734 (11.8) | 2760 (11.5) | 722 (11.8) | |||
| 3 | 3375 (4.2) | 385 (6.2) | 1336 (5.6) | 374 (6.1) | |||
| ≥4 | 3033 (3.8) | 414 (6.6) | 1242 (5.2) | 376 (6.1) | |||
Pregnancy complications
Vaccinated and non-vaccinated women were similar in terms of proportion of spontaneous deliveries (adjusted odds ratio 1.02, 95% confidence interval 0.96 to 1.08) and post-partum admissions to the intensive care unit (0.95, 0.47 to 1.88). Vaccinated women had a slightly higher risk of eclampsia (adjusted odds ratio 1.19, 1.02 to 1.39) and gestational diabetes (1.26, 1.04 to 1.53) (table 3). We observed only minor differences between matched and unmatched analyses. The risk estimates did not change when we excluded the two weeks following the vaccination from the analysis (table 4).
Table 3.
Pregnancy, fetal, and neonatal outcomes
| Unmatched cohort analysis | Propensity score matched analysis | ||||||
|---|---|---|---|---|---|---|---|
| No (%) of cases | Unadjusted odds ratio (95% CI) | No (%) of cases | Adjusted odds ratio (95% CI) | ||||
| Unvaccinated (n=79 925) | Vaccinated (n-6246) | Unvaccinated (n=23 987) | Vaccinated (n=6131) | ||||
| Pregnancy outcomes | |||||||
| Pre-eclampsia/eclampsia | 2679 (3.4) | 248 (4.0) | 1.19 (1.04 to 1.36) | 715 (3.0) | 219 (3.6) | 1.19 (1.02 to 1.39) | |
| Gestational diabetes | 1738 (2.2) | 183 (2.9) | 1.36 (1.16 to 1.59) | 444 (1.9) | 144 (2.3) | 1.26 (1.04 to 1.53) | |
| In-hospital maternal death | 2 (0.0) | 0 | — | 0 | 0 | — | |
| Admission to ICU | 164 (0.2) | 10 (0.2) | 0.78 (0.41 to 1.48) | 42 (0.2) | 10 (0.2) | 0.95 (0.47 to 1.88) | |
| Type of delivery: spontaneous v others | 53 940 (67.5) | 4173 (66.8) | 0.96 (0.92 to 1.02) | 16 003 (66.7) | 4107 (67.0) | 1.02 (0.96 to 1.08) | |
| Fetal and perinatal outcomes | |||||||
| Stillbirths | 207 (0.3) | 16 (0.3) | 0.99 (0.57 to 1.68) | 58 (0.2) | 16 (0.3) | 1.06 (0.61 to 1.85) | |
| In-hospital neonatal death | 74 (0.1) | 5 (0.1) | 0.86 (0.35 to 2.14) | 19 (0.1) | 5 (0.1) | 1.04 (0.39 to 2.78) | |
| Perinatal death | 281 (0.4) | 21 (0.3) | 0.96 (0.60 to 1.52) | 77 (0.3) | 21 (0.3) | 1.06 (0.65 to 1.71) | |
| Neonatal outcomes | |||||||
| Small for gestational age | 7947 (9.9) | 570 (9.1) | 0.91 (0.83 to 0.99) | 2307 (9.6) | 562 (9.2) | 0.95 (0.86 to 1.04) | |
| Admission to neonatal ICU | 1639 (2.1) | 148 (2.4) | 1.16 (0.97 to 1.38) | 492 (2.1) | 146 (2.4) | 1.14 (0.95 to 1.37) | |
| Neonatal reanimation | 724 (0.9) | 59 (0.9) | 1.04 (0.80 to 1.36) | 203 (0.8) | 58 (0.9) | 1.12 (0.83 to 1.50) | |
| Composite outcome | 2415 (3.0) | 180 (2.9) | 0.95 (0.82 to 1.11) | 710 (3.0) | 176 (2.9) | 0.96 (0.81 to 1.13) | |
| Congenital malformations:* | 3246 (4.1) | 284 (4.5) | 1.13 (0.99 to 1.28) | 945 (3.9) | 276 (4.5) | 1.14 (0.99 to 1.31) | |
| Nervous system | 148 (0.2) | 14 (0.2) | 1.21 (0.67 to 2.15) | 45 (0.2) | 13 (0.2) | 1.09 (0.58 to 2.02) | |
| Eye | 28 (0.04) | 3 (0.05) | 1.37 (0.42 to 4.51) | 8 (0.03) | 3 (0.05) | 1.50 (0.40 to 5.65) | |
| Ear, face, and neck | 71 (0.1) | 10 (0.2) | 1.80 (0.88 to 3.61) | 27 (0.1) | 10 (0.2) | 1.42 (0.69 to 2.94) | |
| Congenital heart defects | 1269 (1.6) | 113 (1.8) | 1.14 (0.94 to 1.39) | 351 (1.5) | 110 (1.8) | 1.22 (0.98 to 1.51) | |
| Respiratory | 52 (0.1) | 7 (0.1) | 1.72 (0.72 to 3.94) | 13 (0.1) | 7 (0.1) | 2.00 (0.79 to 5.07) | |
| Orofacial clefts | 86 (0.1) | 4 (0.1) | 0.59 (0.19 to 1.68) | 20 (0.1) | 3 (0.05) | 0.54 (0.16 to 1.84) | |
| Digestive system | 262 (0.3) | 23 (0.4) | 1.12 (0.72 to 1.75) | 74 (0.3) | 23 (0.4) | 1.18 (0.73 to 1.89) | |
| Abdominal wall defects | 15 (0.02) | 2 (0.03) | 1.71 (0.39 to 7.46) | 2 (0.01) | 2 (0.03) | 4.00 (0.56 to 28.40) | |
| Urinary | 423 (0.5) | 34 (0.5) | 1.03 (0.71 to 1.48) | 128 (0.5) | 32 (0.5) | 0.98 (0.67 to 1.45) | |
| Genital | 20 (0.03) | 0 | — | 6 (0.03) | 0 | — | |
| Limb | 972 (1.2) | 82 (1.3) | 1.08 (0.86 to 1.35) | 288 (1.2) | 80 (1.3) | 1.09 (0.85 to 1.40) | |
| Other anomalies | 78 (0.1) | 8 (0.1) | 1.31 (0.63 to 2.72) | 24 (0.1) | 8 (0.1) | 1.33 (0.60 to 2.97) | |
ICU=intensive care unit.
*At least one.
Table 4.
Sensitivity analysis on pregnancy, fetal, and neonatal outcomes: propensity score matched analysis
| No (%) of cases | Adjusted odds ratio (95% CI) | ||
|---|---|---|---|
| Unvaccinated (n=22 145) | Vaccinated (n=5776) | ||
| Pregnancy outcomes | |||
| Pre-eclampsia/eclampsia | 675 (3.0) | 210 (3.6) | 1.19 (1.01 to 1.39) |
| Gestational diabetes | 422 (1.9) | 139 (2.4) | 1.25 (1.03 to 1.52) |
| In-hospital maternal death | 0 | 0 | — |
| Admission to ICU | 39 (0.2) | 10 (0.2) | 1.04 (0.52 to 2.09) |
| Type of delivery: spontaneous v others | 14 841 (67.0) | 3875 (67.1) | 1.00 (0.94 to 1.07) |
| Fetal and perinatal outcomes | |||
| Stillbirths | 49 (0.2) | 14 (0.2) | 1.10 (0.60 to 2.01) |
| In-hospital neonatal death | 16 (0.1) | 4 (0.1) | 0.98 (0.33 to 2.95) |
| Perinatal death | 65 (0.3) | 18 (0.3) | 1.07 (0.63 to 1.82) |
| Neonatal outcomes | |||
| Small for gestational age | 2134 (9.6) | 523 (9.1) | 0.93 (0.84 to 1.03) |
| Admission to neonatal ICU | 416 (1.9) | 128 (2.2) | 1.16 (0.95 to 1.42) |
| Neonatal reanimation | 174 (0.8) | 56 (1.0) | 1.24 (0.92 to 1.68) |
| Composite outcome | 646 (2.9) | 158 (2.7) | 0.92 (0.77 to 1.02) |
| Congenital malformations:* | 873 (3.9) | 260 (4.5) | 1.14 (0.99 to 1.31) |
| Nervous system | 40 (0.2) | 12 (0.2) | 1.15 (0.60 to 2.19) |
| Eye | 8 (0.04) | 3 (0.1) | 1.46 (0.39 to 5.50) |
| Ear, face, and neck | 26 (0.1) | 10 (0.2) | 1.36 (0.65 to 2.84) |
| Congenital heart defects | 319 (1.4) | 105 (1.8) | 1.25 (1.00 to 1.57) |
| Respiratory | 13 (0.1) | 6 (0.1) | 2.00 (0.79 to 5.01) |
| Orofacial clefts | 17 (0.1) | 3 (0.1) | 0.64 (0.18 to 2.22) |
| Digestive system | 69 (0.3) | 22 (0.4) | 1.17 (0.72 to 1.89) |
| Abdominal wall defects | 2 (0.00) | 2 (0.03) | 4.00 (0.61 to 28.39) |
| Urinary | 121 (0.5) | 28 (0.5) | 0.92 (0.61 to 1.39) |
| Genital | 6 (0.03) | 0 | — |
| Limb | 266 (1.2) | 75 (1.3) | 1.06 (0.82 to 1.38) |
| Other anomalies | 23 (0.1) | 6 (0.1) | 1.03 (0.42 to 2.54) |
ICU=intensive care unit.
*At least one.
Fetal and neonatal outcomes
The rates of fetal and perinatal outcomes were very similar between vaccinated and non-vaccinated women in both unmatched and matched cohorts (table 3). The adjusted odds ratio of perinatal deaths (stillbirths and in-hospital deaths) was 1.06 (0.65 to 1.71). The likelihood of a newborn being small for gestational age was not affected by vaccination during pregnancy (adjusted odds ratio 0.95, 0.86 to 1.04). We found no differences between vaccinated and non-vaccinated women with regards to the risk estimates of admissions to neonatal intensive care units, need for reanimation procedures, or the composite outcome suggestive of fetal stress at delivery.
A diagnosis of congenital malformation was present in 3246 (4.1%) newborns in the unexposed cohort and 284 (4.5%) in the vaccinated one. The slight increase in the risk estimate was on the margin of statistical significance (adjusted odds ratio 1.14, 0.99 to 1.31). We observed similar rates of congenital malformation regardless of the trimester of vaccination. When classifying congenital malformations according to the organ system subgroups of EUROCAT, we observed a slight, non-significant, increase in congenital malformations in the vaccinated cohort in most subgroups. The sensitivity analysis did not alter the risk estimates: for instance, the odds ratio for heart defects was 1.22 (0.98 to 1.51) in the matched analysis and 1.25 (1.00 to 1.57) in the sensitivity analysis (tables 3 and 4).
Discussion
This was a large population based cohort study that investigated the association between the MF59 adjuvanted pandemic A/H1N1 vaccination in pregnancy and multiple adverse outcomes. We did not find an increased risk of either fetal or birth outcomes following vaccination, whereas a limited increase in the prevalence of gestational diabetes and eclampsia was observed.
Comparison with other studies
Only a few studies have been conducted on the association between pandemic vaccination and maternal or birth outcomes. Three papers focused on the risk of pre-eclampsia/eclampsia after vaccination.14 17 20 Our findings are in line with the risk estimates provided by two of these studies: adjusted odds ratio 1.12 (0.81 to 1.55) and adjusted hazard ratio 1.10 (0.97 to 1.26).14 17 In the second study, the comparison was made between women vaccinated during pregnancy with the pandemic A/H1N1 vaccine and those who received the seasonal influenza vaccine.17 The third study, which compared 18 612 women who received the AS03 adjuvanted vaccine and 136 914 non-vaccinated women in Sweden, did not suggest any increased risk (0.99, 0.92 to 1.07).20
With regard to gestational diabetes, Heikkinen and colleagues found a protective effect of the MF59 adjuvanted vaccine (0.48, 0.29 to 0.80).14 However, the study was based on a relatively limited cohort of vaccinated women (n=2295) and the authors recognise that “the significantly decreased odds for gestational diabetes is most likely related to the differential follow-up times, as illustrated by the absence of any effect in the proportional hazard model.” A study carried out in Sweden found no effect for gestational diabetes (0.94, 0.81 to 1.09).20
With regard to congenital malformations, which are considered the most severe birth outcomes, the overall risk estimates seen in our study were comparable to those reported by five other published studies.14 16 17 20 24 In particular, the estimate was consistent with the one provided by Heikkinen and colleagues, who were testing the same vaccine composition used in our study. The distribution pattern of congenital malformations was comparable to those already published14 20; the slight imbalance in the prevalence of heart defects in the vaccinated cohort, which is on the margin of statistical significance, is coherent with the findings of Heikkinen.14 However, our study was not intended to highlight differences in risk within subgroups of congenital malformations and, in this respect, the results should be considered as hypothesis generating. To avoid over-interpretation of our findings, a meta-analysis of the studies that investigated heart defects is needed.
Overall, our findings are consistent with those reported by other studies that tested different vaccine formulations (both adjuvanted and not adjuvanted ones) when considering most of the outcomes tested.
Strengths and limitations of study
We considered many potential confounders (including socioeconomic status), which we identified from multiple databases, allowing increased quality and completeness of data. Moreover, the study design was based on information collected from registries, which allowed an independent selection of confounding factors, exposures, and outcomes.
Many outcomes depend on gestational age. We thus matched exposed and non-exposed women by timing of vaccination during pregnancy, aligning the gestational age (in days) of unexposed women with the gestational age (in days) at vaccination, eliminating this relevant confounder.
To take into account the potential confounding factor attributable to the healthy vaccinee effect (that is, the relative good health of patients at the moment of vaccine administration), we did a sensitivity analysis excluding outcomes occurring in the two week period after vaccination. Overall, the sensitivity analysis shifted the risk estimates toward the null, indicating the presence of such residual confounding.
Unlike other studies, we were not able to control our estimates for some confounding factors such as smoking history, alcohol consumption, and body mass index, which could play a role in the aetiology of different outcomes and may be associated with the decision to be vaccinated. For instance, we found a higher prevalence of underlying risk factors among women undergoing vaccination, which is not surprising as the immunisation was primarily recommended in women with comorbidities. The vaccination rate of 7.2% is similar to the coverage reported by other EU countries29; the relatively low proportion of vaccinated women could be due to the fact that this was the first time that pregnant women without comorbidities were prioritised for vaccination. Pregnant women underwent vaccination at a late stage of pregnancy in the Lombardy region, and only 74 (1.2%) were vaccinated during the first trimester. This very limited cohort makes unfeasible any evaluation of outcomes, and our data can be useful if added to similar ones in a meta-analysis.
Conclusions
Our findings add to the available body of evidence on the safety of the MF59 adjuvanted pandemic A/H1N1 vaccine in pregnancy. Meta-analysis of published studies should be carried out to better define the risk of less frequent outcomes, such as specific congenital malformations. In comparison with the past, future vaccination campaigns targeted at pregnant women will rely on more sound evidence on the safety of vaccine. Clearly, two other factors—maternal and fetal risks associated with the influenza infection during pregnancy, together with the evidence on the effectiveness of the vaccination—should also be taken into account in decision making.
What is already known on this topic
Pregnant women were prioritised as target group for the 2009-10 pandemic influenza vaccination campaign
The effect of MF59 adjuvanted A/H1N1 vaccine on “hard” pregnancy outcomes, such as gestational diabetes, eclampsia, and congenital malformations, has rarely been explored
Only one industry sponsored study, including 2295 vaccinated women, investigated maternal outcomes and congenital malformations in association with MF59 adjuvanted vaccine
What this study adds
No increased risk of either fetal or birth outcomes was seen following vaccination, whereas a limited increase in the prevalence of gestational diabetes and eclampsia was observed
These findings add to the available body of evidence on the safety of the MF59 adjuvanted pandemic vaccine in pregnancy
In comparison with the past, future vaccination campaigns targeted at pregnant women will rely on more sound evidence on the safety of vaccine
Contributors: GT, MG, MV, and CZ conceived the study. FT, RDC, SSA, and GT designed the study. FT, RDC, SSA, and GT analysed the data. FT and GT wrote the manuscript. FT, GT, RDC, SSA, MG, MV, and CZ contributed to the discussion and reviewed the manuscript. All authors saw, commented on, and approved the final version of the paper. GT is the guarantor.
Funding: Only public employees of the national or regional health authorities were involved in conceiving, planning, and conducting the study; no additional funding was received.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: The study was approved by the ethics committee of the Italian National Institute of Health. Only anonymised data were used.
Transparency: GT affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Data sharing: The authors are willing to collaborate in answering further research questions and to participate in systematic reviews or meta-analyses.
Cite this as: BMJ 2014;348:g3361
Web Extra. Extra material supplied by the author
References
- 1.Chan M. World now at the start of 2009 influenza pandemic. 2009. www.who.int/mediacentre/news/statements/2009/h1n1_pandemic_phase6_20090611/en/index.html.
- 2.Chowell G, Bertozzi SM, Colchero MA, Lopez-Gatell H, Alpuche-Aranda C, Hernandez M, et al. Severe respiratory disease concurrent with the circulation of H1N1 influenza. N Engl J Med 2009;361:674-9. [DOI] [PubMed] [Google Scholar]
- 3.Vaillant L, La Ruche G, Tarantola A, Barboza P. Epidemiology of fatal cases associated with pandemic H1N1 influenza 2009. Euro Surveill 2009;14(33):pii=9309. [DOI] [PubMed] [Google Scholar]
- 4.Jamieson DJ, Honein MA, Rasmussen SA, Williams JL, Swerdlow DL, Biggerstaff MS, et al, for the Novel Influenza A (H1N1) Pregnancy Working Group. H1N1 2009 influenza virus infection during pregnancy in the USA. Lancet 2009;374:451-8. [DOI] [PubMed] [Google Scholar]
- 5.ANZIC Influenza Investigators and Australasian Maternity Outcomes Surveillance System. Critical illness due to 2009 A/H1N1 influenza in pregnant and postpartum women: population based cohort study. BMJ 2010;340:c1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Griffith GW, Adelstein AM, Lambert PM, Weatherall JA. Influenza and infant mortality. BMJ 1972;3:553-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nishiura H. Excess risk of stillbirth during the 1918-1920 influenza pandemic in Japan. Eur J Obstet Gynecol Reprod Biol 2009;147:115. [DOI] [PubMed] [Google Scholar]
- 8.Mak TK, Mangtani P, Leese J, Watson JM, Pfeifer D. Influenza vaccination in pregnancy: current evidence and selected national policies. Lancet Infect Dis 2008;8:44-52. [DOI] [PubMed] [Google Scholar]
- 9.Laibl VR, Sheffield JS. Influenza and pneumonia in pregnancy. Clin Perinatol 2005;32:727-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Acs N, Bánhidy F, Puhó E, Czeizel AE. Maternal influenza during pregnancy and risk of congenital abnormalities in offspring. Birth Defects Res A Clin Mol Teratol 2005;73:989-96. [DOI] [PubMed] [Google Scholar]
- 11.Czeizel AE, Puhó EH, Acs N, Bánhidy F. Use of specified critical periods of different congenital abnormalities instead of the first trimester concept. Birth Defects Res A Clin Mol Teratol 2008;82:139-46. [DOI] [PubMed] [Google Scholar]
- 12.Ministero del Lavoro, della Salute e delle Politiche Sociali. Misure urgenti in materia di protezione dal virus influenzale A(H1N1). 2009. www.trovanorme.salute.gov.it/dettaglioAtto?completo=si&id=30406.
- 13.European Medicines Agency, European Centre for Disease Prevention and Control, Heads of Medicines Agencies. European strategy for influenza A/H1N1 vaccine benefit-risk monitoring. 2009. www.ema.europa.eu/docs/en_GB/document_library/Report/2010/01/WC500044933.pdf.
- 14.Heikkinen T, Young J, van Beek E, Franke H, Verstraeten T, Weil JG, et al. Safety of MF59-adjuvanted A/H1N1 influenza vaccine in pregnancy: a comparative cohort study. Am J Obstet Gynecol 2012;207:177.e1-8. [DOI] [PubMed] [Google Scholar]
- 15.Pasternak B, Svanström H, Mølgaard-Nielsen D, Krause TG, Emborg HD, Melbye M, et al. Vaccination against pandemic A/H1N1 2009 influenza in pregnancy and risk of fetal death: cohort study in Denmark. BMJ 2012;344:e2794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pasternak B, Svanström H, Mølgaard-Nielsen D, Krause TG, Emborg HD, Melbye M, et al. Risk of adverse fetal outcomes following administration of a pandemic influenza A(H1N1) vaccine during pregnancy. JAMA 2012;308:165-74. [DOI] [PubMed] [Google Scholar]
- 17.Conlin AM, Bukowinski AT, Sevick CJ, De Scisciolo C, Crum-Cianflone NF. Safety of the pandemic H1N1 influenza vaccine among pregnant U.S. military women and their newborns. Obstet Gynecol 2013;12:511-8. [DOI] [PubMed] [Google Scholar]
- 18.Fell DB, Sprague AE, Liu N, Yasseen AS 3rd, Wen SW, Smith G, et al, for the Better Outcomes Registry & Network (BORN) Ontario. H1N1 influenza vaccination during pregnancy and fetal and neonatal outcomes. Am J Public Health 2012;102:e33-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Håberg SE, Trogstad L, Gunnes N, Wilcox AJ, Gjessing HK, Samuelsen SO, et al. Risk of fetal death after pandemic influenza virus infection or vaccination. N Engl J Med 2013;368:333-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Källén B, Olausson PO. Vaccination against H1N1 influenza with Pandemrix(®) during pregnancy and delivery outcome: a Swedish register study. BJOG 2012;119:1583-90. [DOI] [PubMed] [Google Scholar]
- 21.Ludvigsson JF, Zugna D, Cnattingius S, Richiardi L, Ekbom A, Örtqvist Å, et al. Influenza H1N1 vaccination and adverse pregnancy outcome. Eur J Epidemiol 2013;28:579-88. [DOI] [PubMed] [Google Scholar]
- 22.Richards JL, Hansen C, Bredfeldt C, Bednarczyk RA, Steinhoff MC, Adjaye-Gbewonyo D, et al. Neonatal outcomes after antenatal influenza immunization during the 2009 H1N1 influenza pandemic: impact on preterm birth, birth weight, and small for gestational age birth. Clin Infect Dis 2013;56:1216-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rubinstein F, Micone P, Bonotti A, Wainer V, Schwarcz A, Augustovski F, et al, for the EVA Study Research Group Estudio Embarazo y Vacuna Antigripal. Influenza A/H1N1 MF59 adjuvanted vaccine in pregnant women and adverse perinatal outcomes: multicentre study. BMJ 2013;346:f393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oppermann M, Fritzsche J, Weber-Schoendorfer C, Keller-Stanislawski B, Allignol A, Meister R, et al. A(H1N1)v2009: a controlled observational prospective cohort study on vaccine safety in pregnancy. Vaccine 2012;30:4445-52. [DOI] [PubMed] [Google Scholar]
- 25.Sammon CJ, Snowball J, McGrogan A, de Vries CS. Evaluating the hazard of foetal death following H1N1 influenza vaccination; a population based cohort study in the UK GPRD. PLoS One 2012;7:e51734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jamieson DJ, Rasmussen SA. The safety of adjuvants in influenza vaccines during pregnancy: what do we know and why do we need them? Am J Obstet Gynecol 2012;207:145-6. [DOI] [PubMed] [Google Scholar]
- 27.Steinhoff MC, MacDonald NE. Influenza pandemics—pregnancy, pathogenesis, and perinatal outcomes. JAMA 2012;308:184-5. [DOI] [PubMed] [Google Scholar]
- 28.European surveillance of congenital anomalies (EUROCAT). Malformation coding guides. www.eurocat-network.eu/aboutus/datacollection/guidelinesforregistration/malformationcodingguides.
- 29.Mereckiene J, Cotter S, Weber JT, Nicoll A, D’Ancona F, Lopalco PL, et al. Influenza A(H1N1)pdm09 vaccination policies and coverage in Europe. Euro Surveill 2012;17(4):pii=20064. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.