Abstract
Nikkomycin Z (NikZ) is a chitin synthase inhibitor with activity against Coccidioides species that is being developed as a first-in-class orphan product for treatment of coccidioidomycosis. It has previously been shown to reduce lethal respiratory infections in mice to undetectable levels when treatment is begun 48 hours after infection. The studies described here focus on bracketing NikZ doses for phase 2 and 3 clinical trials, using an established mouse respiratory infection as a model and starting treatment 120 hours after infection. A dose of 80 mg/kg/day, divided into 2 doses, nearly eradicated infection, and larger doses did not improve fungal clearance. Increasing the duration of treatment from 1 week to 3 weeks resulted in a greater percentage of culture-negative mice. Comparative data show that plasma levels of NikZ that nearly eradicate Coccidioides in mice are achievable in patients and provide a plausibly effective dose range for initial phase 2 clinical studies.
Keywords: coccidioidomycosis, anti-fungal drugs, nikkomycin Z, Mouse, experimental infection, pharmacokinetics
Coccidioides posadasii and Coccidioides immitis are soil fungi endemic to the southwestern United States, northern Mexico, and scattered areas throughout South America [1]. Nikkomycin Z (NikZ) is a narrow-spectrum antifungal drug with potent in vitro activity against Coccidioides species [2, 3]. This drug is currently under development as an orphan drug for the treatment of coccidioidomycosis. It has shown efficacy against coccidioidomycosis in naturally infected dogs and experimentally infected mice and has undergone phase 1 studies [4–6].
In previous studies involving 8 mice given 50 mg/kg twice daily for 5 days starting 48 hours after infection, no fungal growth was detected in 7 and only a single colony was detected in the remaining animal when all were euthanized 48 hours after stopping treatment [4]. The purpose of those studies was to provide a highly lethal dose (5000–10 000 spores) and to initiate treatment before the immune system could influence the outcome. One goal of this report was to frame a dose of NikZ for phase 2 and 3 clinical trials by starting treatment after a subacute lethal infection had become established in a murine model of lung infection and after the fungal burden was increased 10–100-fold [7–9]. We also sought to determine whether longer treatment time yielded a greater reduction in fungal burden.
MATERIALS AND METHODS
Mice
Eight-week-old female Swiss-Webster mice were purchased from Harlan Sprague Dawley (Indianapolis, IN) and housed according to National Institutes of Health guidelines. All procedures were approved by the University of Arizona Institutional Animal Care and Use Committee.
Fungal Cultures
C. posadasii strain Silveira was grown to maturity on glucose-yeast extract agar and harvested as previously described [10] Arthroconidia were separated from mycelial fragments, counted on a hemocytometer, and plated to determine the viable-colony count. For infection, arthroconidia were suspended in sterile 0.9% saline for injection to contain the desired inoculum of approximately 500 colony-forming units (CFUs) in 30 µL. The number of arthroconidia given to mice at the time of infection was verified by enumeration on glucose-yeast extract agar plates after incubation for 3 days at 37°C.
Drug Therapies
NikZ HCl powder was provided at >95% purity by the University of Arizona with a certificate of analysis from SRI International (Menlo Park, CA). The powder was weighed with potency correction and dissolved in water to prepare a stock solution. Further dilutions were performed in 0.9% sodium chloride and sterilized by filtration for subcutaneous administration. Saline for injection (0.9% subcutaneously) was used for placebo treatments.
Assay for NikZ in Plasma
Plasma concentrations were analyzed using a validated high-performance liquid chromatography (HPLC) method with ultraviolet detection developed in our laboratory. The assay quantitation range was 0.25–8.00 µg/mL. Samples with concentrations above the upper limit of quantitation were diluted and then reanalyzed. Sample preparation involved mixing 150 µL of sample (standard, quality control, or mouse sample) with 30 µL of 2 mg/mL sodium dodecyl sulfate in water. The sample was mixed and then loaded into an ultrafiltration device (Centrifree YM-30, Millipore, Bilerica, MA), followed by centrifugation at 2000×g for 60 minutes at 4°C. Eighty microliters of the filtrate was then transferred to a HPLC vial and vortex mixed with 20 µL of 6 M acetic acid. The injection volume was 90 µL. Separation was achieved using an octadecylsilane column (Gemini 5 µ C18, 110A, 15 cm × 4.6 mm ID, Phenomenex, Torrance, CA). The mobile phase consisted of 0.05 M acetic acid and 80 mM 1-heptanesulfonic acid in a part ratio of 78 to 22 with acetonitrile. Ultraviolet detection at a wavelength of 263 nm was used. The interday precision was 5.8% at 0.5 µg/mL, 5.7% at 2 µg/mL, and 3.8% at 6 µg/mL.
Murine Infection Studies
Swiss-Webster mice were infected with a lethal target dose of 500 spores (range, 500–550 spores) intranasally, and treatment was initiated 120 hours after infection. For the dose-ranging study, groups of 6 mice were treated twice daily for 7 days and then euthanized 2 days after the last treatment. Lung fungal burdens were quantitated, and whole spleens were cultured to assess dissemination, as previously described [11]. In a second study, performed to determine whether a longer treatment time improved outcome, groups of 20 mice were treated once daily for either 7 days or 21 days, and half of each group was euthanized either 2 days or 3 weeks after treatment to determine whether the fungal burden increased after discontinuing the drug.
Pharmacokinetic Study
Sixteen mice were included in each of 2 groups, which received NikZ 10 mg/kg subcutaneously or NikZ 40 mg/kg subcutaneously. Two mice from each group were euthanized at fixed times after dosing, including 0.25, 0.5, 1.0, 1.5, 2, 4, 6, and 8 hours. A blood specimen was collected under isoflurane anesthesia from the retro-orbital plexus (approximately 200 µL/mouse) into a combination capillary collection/sample container (Microvette CB300, BLQ Braintree Scientific, Braintree, MA) containing heparin. The blood specimen was centrifuged at 3000×g, and plasma was separated, transferred to a cryostorage tube, and frozen on dry ice. After the experiment was completed, the samples were transferred to a −80°C freezer until analyzed.
Statistical Analysis
SAS, version 9.1.3 (SAS Institute, Cary, NC), was used for all analyses unless otherwise stated. Total lung fungal burden counts were log10 transformed before analysis; for lungs without fungal growth, a count of 1 was assigned before log10 transformation, and data were analyzed using a linear model (SAS Proc Mixed).
Dose response was evaluated using nonlinear regression and a sigmoid Emax model implemented with WinNonlin (standard edition, Pharsight, Cary NC). The equation was as follows: log kill = [Emax × doseh]/[ED50h + doseh], where “Emax” is the maximum log10 reduction (kill) in fungal lung burden, “dose” is the daily dose (in milligrams/kilogram/day), “ED50” is the dose that provides 50% of maximum kill (log reduction in organ burden), and “h” is Hill's constant for slope.
WinNonlin, standard edition, was used for the pooled pharmacokinetic analysis by compartmental and noncompartmental methods. In the case of compartmental modeling, all available data points were used. For noncompartmental analysis, the average concentration was used when 2 data points were available for the same postdose time.
RESULTS
Infection Studies
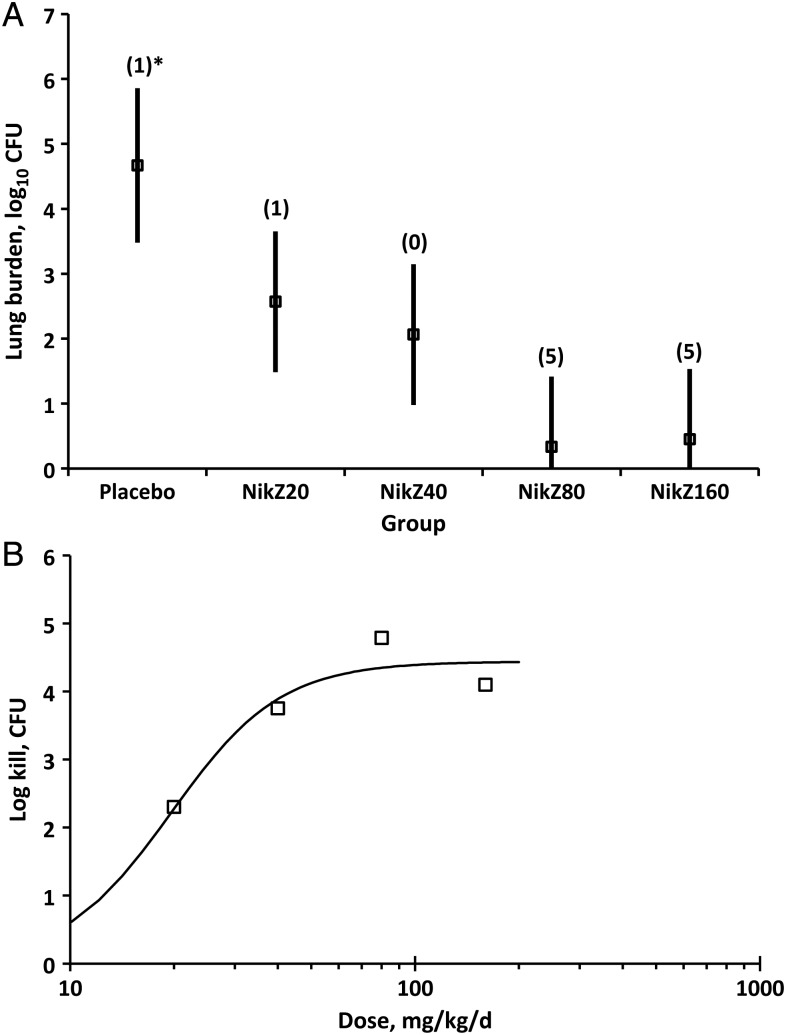
To evaluate dose response, mice were infected with 504 spores of strain Silveira on the basis of postinfection plate counts, and treatment was initiated 120 hours after infection with 20, 40, 80, or 160 mg/kg NikZ daily divided into 2 doses. An equivalent volume of 0.9% saline was given as placebo on the same schedule (ie, twice daily). The mean fungal burden for the placebo group was 4.9 ± 3.0 log10 CFUs. Treatment with NikZ lowered the fungal burden in a dose-dependent manner between 2.6 ± 1.6 and 0.45 ± 1.1 log10 CFUs in total lung (Figure 1A); all dose levels resulted in a statistically lower lung fungal burden than placebo (P = .0036 to < .001). The response (ie, log reduction in fungal burden) is closely approximated using a sigmoid Emax model in which Emax was 4.44, ED50 was 19.6 mg/kg/d, and h was 2.74 (Figure 1B). There was no further increase in efficacy in doses ranging from 80 mg/kg/day to 160 mg/kg/day, making 80 mg/kg/day the optimized dose in this model.
Figure 1.
A, Mean log10 fungal burden (±95% confidence interval) in lungs following treatment with rising oral doses of nikkomycin Z (NikZ) or placebo. Numbers in parentheses are mice with negative test results. The asterisk denotes a culture-negative mouse in the placebo group that was probably uninfected because of technical reasons. NikZ20, 20 mg/kg/d; NikZ40, 40 mg/kg/d; NikZ80, 80 mg/kg/d; NikZ160, 160 mg/kg/d. All daily doses were divided into 2 doses. B, Efficacy of NikZ, showing the log reduction in lung fungal burden in relation to dose.
In previous studies, NikZ has been shown to eradicate infection, based on results of posttreatment quantitative fungal culture [4]. In our studies, in which treatment was started 120 hours after infection, 5 of 6 mice treated with 80 mg/kg/day and 5 of 6 treated with 160 mg/kg/day were negative for fungal growth. With doses of 20 mg/kg/day and 40 mg/kg/day, 1 of 6 and 0 of 6 treated mice, respectively, were negative for fungus on culture. One mouse in the placebo group was uninfected at the time it was euthanized, possibly because it swallowed or sneezed out the infectious suspension. Thus, it is also possible that 1 or more of the test-negative, treated mice were also uninfected.
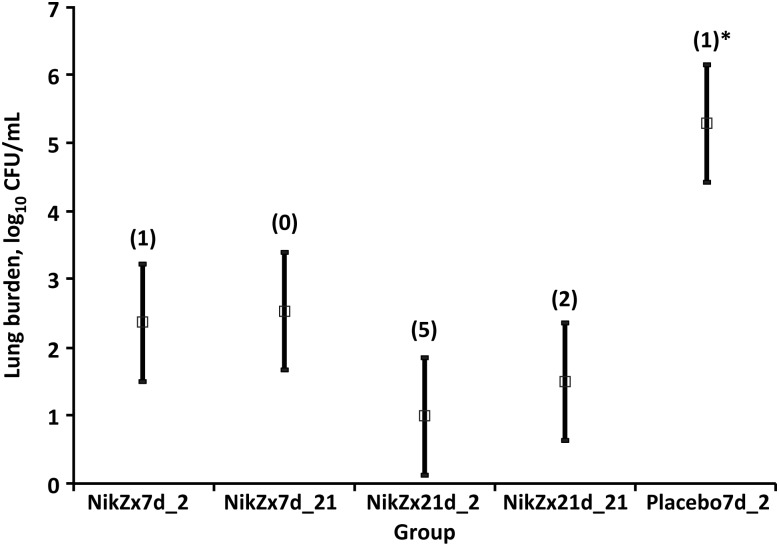
To assess the effect of longer duration of treatment, mice infected with 550 spores were treated with 80 mg/kg NikZ or placebo once daily for 7 days or 21 days and euthanized 2 days after cessation of treatment (Figure 2). Placebo mice were treated for 7 days and euthanized 2 days later and had a mean lung fungal burden of 5.3 ± 2.7 log10 CFUs. This was 2.8–4.1 log10 CFUs higher (P < .001) than that in any of the groups of mice treated with NikZ. In mice treated with NikZ, 3 weeks of treatment significantly reduced the fungal burden, compared with 7 days of treatment, as revealed by evaluation of mice euthanized 2 days after discontinuing treatment (P = .0276), and there were more mice in which fungus was not detected in postmortem lung cultures (5 vs 1).
Figure 2.
Mean lung fungal burden in mice treated for either 7 days or 21 days with 80 mg/kg nikkomycin Z (NikZ) once daily and euthanized 48 hours or 3 weeks after discontinuing drug therapy. All NikZ treatments yielded significantly better results than placebo (P < .001). NikZ administered for 7 days to mice that were euthanized 2 days after cessation of treatment yielded significantly worse results than when administered for 21 days to mice euthanized 2 days after treatment cessation (P = .0276), but results did not differ between the 21-day treatment groups euthanized 2 and 21 days after treatment cessation. Numbers in parentheses are culture-negative animals. The asterisk denotes a culture-negative mouse in the placebo group that was probably uninfected because of technical reasons. Statistical comparisons were performed by analysis of variance.
To assess the durability of treatment after discontinuation of study drug, mice were treated for either 7 days or 21 days with NikZ and euthanized 21 days after stopping treatment, and characteristics were compared to those of the respective groups euthanized 2 days after treatment (Figure 2). In the 7-day treatment group, the mean lung fungal burden was 2.4 ± 1.0 log10 CFUs among mice euthanized 48 hours after treatment and 2.5 ± 0.58 log10 CFUs among mice euthanized 3 weeks after treatment, a difference that was negligible. In mice treated for 7 days, fungal growth was detected in the lungs of all that were assessed 3 weeks after treatment cessation and in the lungs of all but 1 that were euthanized 48 hours after stopping treatment. In mice that were treated with NikZ for 21 days and euthanized 2 days or 21 days after treatment ended, the lung fungal burden was 0.99 ± 1.4 and 1.5 ± 0.94 log10 CFUs, respectively, a difference that was also not significant; fungal growth in the lung was not detected in 5 of 10 and 2 of 10 mice, respectively. Although Figure 2 shows that mice treated for 7 days and euthanized 21 days later had a higher mean fungal burden than those treated for 3 weeks and euthanized 21 days later, the difference was not significant (P = .101).
In all mice treated with NikZ, spleens were negative for fungal growth, whereas 4 of 6 placebo-treated mice (67%) grew fungal colonies on spleen culture (data not shown). One mouse from the placebo group, which was included in the statistical analysis, had no gross or culture evidence of infection in lungs or spleen; the animal may have swallowed or failed to inhale the inoculum.
NikZ Pharmacokinetics in Mice
Twenty of 32 samples were available for pharmacokinetic analysis. Four samples were assayed at a concentration above the upper limit of quantitation, and there was insufficient sample volume available to repeat the assay. Included was 1 sample obtained early (at 0.25 hours) from the 10-mg/kg group and 3 early samples from the 40-mg/kg group. Eight samples had insufficient volume available to perform the assay.
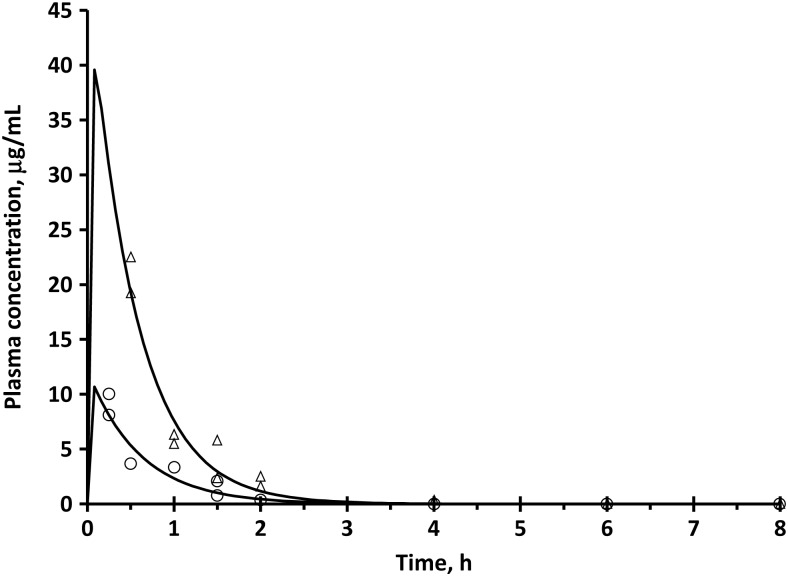
Pooled plasma concentration-time profiles were modeled using a 1-compartment model with first-order input, first-order elimination, and a lag time. The fitted parameter estimates are provided in Table 1. After subcutaneous administration, absorption was very rapid, and there was no apparent lag time. Figure 3 shows the individual and fitted concentration-time profiles. The model explained the concentration-versus-time profiles well; however, there were no early time points with the 40-mg/kg dose. Table 1 provides additional calculated pharmacokinetic parameters for the same experiments. The relative bioavailability for the 10-mg/kg dose, using the 40-mg/kg dose as a reference, was 107%, which indicates that exposure is nearly proportional over the range of 10- to 40-mg/kg doses.
Table 1.
Pharmacokinetic Parameters for Nikkomycin Z (Pooled Data) Administered Subcutaneously, Based on a 1-Compartment Model With First-Order Absorption and Elimination
| Dose Group | Cmax, µg/mL | Tmax, h | AUC0−∞, µg h/mL | CL/F, L/h/kg | V/F, L/kg | Ka, h−1 | Ke, h−1 |
|---|---|---|---|---|---|---|---|
| 10 mg/kg | 11.2 | 0.043 | 7.25 | 1.33 | 0.834 | 96.9 | 1.655 |
| 40 mg/kg | 49.5 | 0.048 | 27.2 | 1.47 | 0.735 | 79.4 | 2.00 |
Precision of the Cmax calculations for the higher dose may be reduced as a result of unavailable measurements at the earliest time point, as detailed in Results.
Abbreviations: AUC, area under the plasma concentration-time curve; CL/F, total clearance divided by fraction absorbed; Cmax, peak plasma concentration; Ka, absorption rate constant; Ke, elimination rate constant; Tmax, time to peak plasma concentration; V/F, volume of distribution divided by fraction absorbed.
Figure 3.
Individual plasma nikkomycin Z (NikZ) concentrations following administration of 10 mg/kg (open circle) and 40 mg/kg (open triangle) subcutaneously. The solid lines represent the fitted concentration versus time profiles, based on a 1-compartment model with first-order absorption and elimination.
Analysis was also performed using pooled data and noncompartmental analysis. Relative bioavailability, determined by noncompartmental analysis, was 135% for the 10-mg/kg dose, which was higher than predicted using the model-based analysis. Much of this difference was due to the limited data that predicted that the peak plasma concentration (Cmax) was higher and occurred earlier than indicated by available data. The Cmax observed was 9.08 µg/mL (time to Cmax [Tmax], 0.25 hours) for 10 mg/kg and 20.8 µg/mL (Tmax, 0.5 hours) for 40 mg/kg. The areas under the plasma concentration-time curve (AUCs0−∞), estimated using the trapezoidal rule with extrapolation, were 6.28 and 18.6 µg h/mL for 10 and 40 mg/kg, respectively.
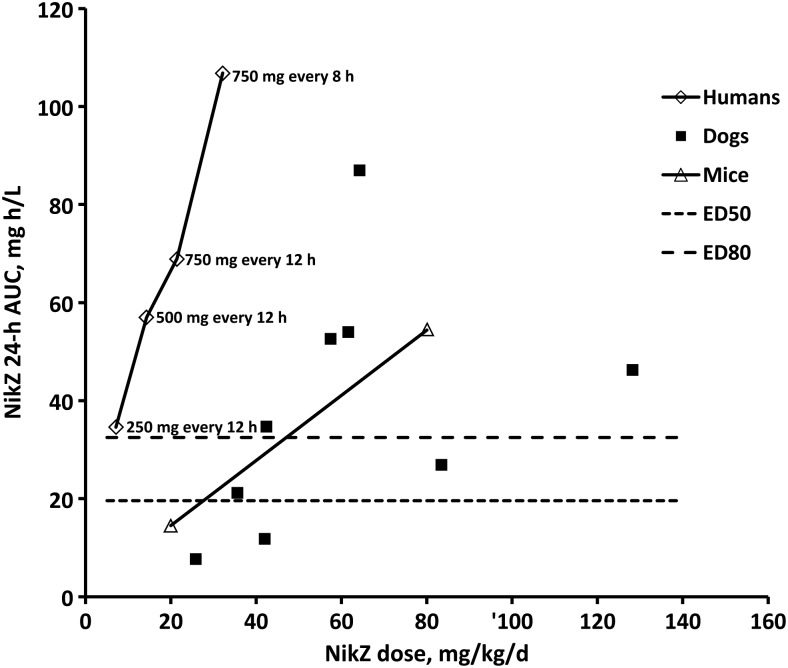
Comparative Pharmacokinetic Data from Dogs, Mice and Humans
Figure 4 shows that twice-daily oral dosing of humans with 250–750 mg NikZ provides 24-hour AUCs within the range of those that were efficacious for treating coccidioidomycosis in experimentally infected mice and naturally infected dogs [5] and therefore suggests a dose range of 250–500mg twice daily for phase 2 clinical trials of coccidioidomycosis. As previously published, the dogs were enrolled with pulmonary coccidioidomycosis and received doses of 250 mg (for those weighing <25 kg) or 500 mg (for those weighing ≥25 kg) twice daily for 60 days, and pharmacokinetic data were collected between the third and fourth week of treatment [5]. The human study included subjects receiving oral doses ranging from 250 mg to 750 mg [12].
Figure 4.
The 24-hour areas under the plasma concentration-time curve (AUCs) for 20 and 80 mg/kg nikkomycin Z (NikZ) daily, divided into 2 doses, in mice, and the 24-hour AUCs associated with 50% and 80% of maximal effect, based on fungal lung burden. Also shown for comparison are the mean 24-hour AUCs associated with 3 different doses in humans and variable doses in 9 dogs [5].
DISCUSSION
These studies were performed to determine the optimal dose of NikZ in a lethal model of coccidioidomycosis in mice for which treatment started 120 hours after infection, by which time granulomas were visible in the lung, the fungal burden had increased 10–100-fold, and inflammation was present [7, 13]. The model was developed to more closely approximate the established disease that humans have when they present with coccidioidomycosis, because sequestration associated with granuloma formation might provide a greater challenge for antifungal therapy. For doses ranging from 20 mg/kg/day to 80 mg/kg/day, significant reductions in fungal burden were attained, but they plateaued and did not improve at a dose of 160 mg/kg/day, resulting in the selection of 80 mg/kg/day as the optimum dose for further studies. The comparative 24-hour AUC graph in Figure 4 shows that the 250–500-mg twice daily doses in humans resulted in blood levels that approximated those in mice that achieved near eradication of fungal burden after receipt of 80 mg/kg/day in divided doses.
In previous studies of highly lethal infectious challenges in which treatment was started 48 hours after infection, the majority of mice had undetectable fungal burdens at euthanization [4]. In the current studies, in which treatment was begun 5 days after infection, we also saw a majority of mice with no fungal burdens in the first study, when mice were treated with 80 mg/kg or 160 mg/kg daily in divided doses and euthanized 48 hours after treatment. However, in a second study, when mice were treated with 80 mg/kg once daily for 7 days, only 1 mouse tested negative for lung fungal growth. Either divided dosing improves eradication of fungus because of the short half-life as shown in a previous publication [4] and/or we experienced biological variation between the 2 studies because the second study did receive a slightly higher infectious dose of spores.
With regard to the duration of treatment study (Figure 2), 3 weeks of NikZ therapy led to a significant reduction in the lung fungal burden and to a greater number of mice with undetectable fungal burdens in the lungs at 48 hours after treatment, compared with 7 days of therapy. Although fungal burdens did not rise significantly during the 3-week observation period for mice treated for either 7 days or 3 weeks, by 3 weeks after treatment, there were slight increases in the mean fungal burden. Possible reasons for this include that the mouse in general is a susceptible host and that the failure of NikZ to completely eradicate infection with either treatment duration once the infection is established in mice leads to a slow increase in the fungal burden once treatment is withdrawn. A possible reason that the difference between the 7-day and 3-week treatment groups euthanized at 3 weeks, although important, was not statistically significant was the small sizes of the groups. Also, our observation at necropsy was that the lungs of more mice treated for 3 weeks appeared grossly normal and had lower fungal burdens than mice treated only 7 days. It would have been interesting to observe the mice longer to determine whether long-term control of disease would have been maintained by the mice treated for 3 weeks, compared with those treated for 1 week.
Finally, the primary objective of the murine dose-ranging and pharmacokinetics studies was to determine a dose range for phase 2 and 3 clinical trials. From the comparative data showing the 24-hour AUC for mice, humans, and dogs (Figure 4), it can be readily seen that humans easily achieve plasma levels that are efficacious in eradicating to nearly eradicating infection in mice with a twice daily dose of 250–500 mg, which is well-tolerated by humans [12]. These blood levels also overlap with what was efficacious in treating naturally infected dogs with coccidioidal pneumonia [5].
In conclusion, NikZ is an orphan drug with the potential treat coccidioidomycosis. It is poised for evaluation in phase 2 studies, and these data provide a rational basis for selecting doses that are likely to be effective in the treatment of human subjects.
Notes
Disclaimer. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Allergy and Infectious Diseases or the National Institutes of Health.
Financial support. This work was supported by the National Institute of Allergy and Infectious Diseases (award R42AI074157 to Valley Fever Solutions).
Potential conflicts of interest. J. N. G. is the chief medical officer of and a significant shareholder in Valley Fever Solutions. All other authors report no potential conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Nguyen C, Barker BM, Hoover S, et al. Recent advances in our understanding of the environmental, epidemiological, immunological, and clinical dimensions of coccidioidomycosis. Clin Microbiol Rev. 2013;26:505–25. doi: 10.1128/CMR.00005-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li RK, Rinaldi MG. In vitro antifungal activity on nikkomycin Z in combination with fluconazole or itraconazole. Antimicrob Agents Chemother. 1999;43:1401–5. doi: 10.1128/aac.43.6.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hector RF, Davidson AP, Johnson SM. Comparison of susceptibility of fungal isolates to lufenuron and nikkomycin Z alone or in combination with itraconazole. Am J Vet Res. 2005;66:1090–3. doi: 10.2460/ajvr.2005.66.1090. [DOI] [PubMed] [Google Scholar]
- 4.Hector RF, Zimmer BL, Pappagianis D. Evaluation of nikkomycins X and Z in murine models of coccidioidomycosis, histoplasmosis, and blastomycosis. Antimicrob Agents Chemother. 1990;34:587–93. doi: 10.1128/aac.34.4.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shubitz LF, Roy ME, Nix DE, Galgiani JN. Efficacy of nikkomycin Z for respiratory coccidioidomycosis in naturally infected dogs. Med Mycol. 2013;51:747–54. doi: 10.3109/13693786.2013.770610. [DOI] [PubMed] [Google Scholar]
- 6.Nix DE, Swezey RR, Hector R, Galgiani JN. Pharmacokinetics of nikkomycin Z after single rising oral doses. Antimicrob Agents Chemother. 2009;53:2517–21. doi: 10.1128/AAC.01609-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shubitz LF, Dial SM, Perrill R, Casement R, Galgiani JN. Vaccine-induced cellular immune responses differ from innate responses in susceptible and resistant strains of mice infected with Coccidioides posadasii. Infect Immun. 2008;76:5553–64. doi: 10.1128/IAI.00885-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kong YM, Levine HB, Madin SH, Smith CE. Fungal multiplication and histopathological changes in vaccinated mice infected with Coccidioides immitis. J Immunol. 1964;92:779–90. [PubMed] [Google Scholar]
- 9.Sun SH, Huppert M. A cytological study of morphogensis in Coccidioides immitis. Sabouraudia. 1976;14:185–98. [PubMed] [Google Scholar]
- 10.Sun SH, Cole GT, Drutz DJ, Harrison JL. Electron-microscopic observations of the Coccidioides immitis parasitic cycle in vivo. J Med Vet Mycol. 1986;24:183–92. [PubMed] [Google Scholar]
- 11.Shubitz LF, Yu J, Hung C, et al. Improved protection of mice against lethal respiratory infection with Coccidioides posadasii using two recombinant antigens expressed as a single protein. Vaccine. 2006;24:5904–11. doi: 10.1016/j.vaccine.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 12.Nix DE, Hoover SE, Thompson CM, Hanan NJ, Chavez SE, Galgiani JN. Pharmacokinetics and safety of nikkomycin Z following multiple rising doses in healthy subjects. Proceedings of the 50th Interscience Conference on Antimicrobial Agents and Chemotherapy, Boston Massachusetts, September 12–15, 2010. Published by American Society for Microbiology, Washington DC.2010. [Google Scholar]
- 13.Shubitz LF, Perrill R, Lewis ML, Dial SM, Galgiani JN. Early post-infection detection of coccidioides in intranasally infected mice. Proceedings of the 55th Annual Coccidioidomycosis Study Group Meeting; Scottsdale Arizona 2 April 2011; Davis, California. 2011. p. 40. [Google Scholar]