Abstract
Objectives.
To examine the association of orthostatic hypotension with incident heart failure (HF) in older adults.
Methods.
Of the 5,273 community-dwelling adults aged 65 years and older free of baseline prevalent HF in the Cardiovascular Health Study, 937 (18%) had orthostatic hypotension, defined as ≥20 mmHg drop in systolic or ≥10 mmHg drop in diastolic blood pressure from supine to standing position at 3 minutes. Of the 937, 184 (20%) had symptoms of dizziness upon standing and were considered to have symptomatic orthostatic hypotension. Propensity scores for orthostatic hypotension were estimated for each of the 5,273 participants and were used to assemble a cohort of 3,510 participants (883 participants with and 2,627 participants without orthostatic hypotension) who were balanced on 40 baseline characteristics. Cox regression models were used to estimate the association of orthostatic hypotension with centrally adjudicated incident HF and other outcomes during 13 years of follow-up.
Results.
Participants (n = 3,510) had a mean (±standard deviation) age of 74 (±6) years, 58% were women, and 15% nonwhite. Incident HF occurred in 25% and 21% of matched participants with and without orthostatic hypotension, respectively (hazard ratio, 1.24; 95% confidence interval, 1.06–1.45; p = .007). Among matched participants, hazard ratios for incident HF associated with symptomatic (n = 173) and asymptomatic (n = 710) orthostatic hypotension were 1.57 (95% confidence interval, 1.16–2.11; p = .003) and 1.17 (95% confidence interval, 0.99–1.39; p = .069), respectively.
Conclusions.
Community-dwelling older adults with orthostatic hypotension have higher independent risk of developing new-onset HF, which appeared to be more pronounced in those with symptomatic orthostatic hypotension.
Key Words: Orthostatic hypotension, Heart failure, Mortality.
Orthostatic hypotension, a blood pressure dysregu- lation, has been shown to be a risk factor for incident heart failure (HF) in middle-aged adults (1,2). Although orthostatic hypotension is common in older adults (3–5) and other blood pressure disorders such as isolated systolic hypertension (6) and isolated diastolic hypotension (7) are common risk factors for incident HF, little is known about the association of orthostatic hypotension with incident HF in older adults. In the Rotterdam Study, among an all-white cohort of adults, aged 55 years or older, orthostatic hypotension was associated with higher risk of coronary heart disease and all-cause mortality but had no significant association with incident HF (8). Because orthostatic hypotension is often associated with other HF risk factors such as prior acute myocardial infarction and isolated systolic hypertension and diabetes (2,9), to what extent its association with outcomes are intrinsic in nature remains unclear. Regression-based risk adjustments may not ensure that baseline confounders are properly balanced between the two study groups, in which case, the adjusted association may not be reflective of the true association (10). Therefore, in the current study, we examined the independence of association of orthostatic hypotension with incident HF in a propensity-matched cohort of older adults in the Cardiovascular Health Study.
Methods
Study Design and Participants
The Cardiovascular Health Study is an ongoing epidemiological study of risk factors for cardiovascular morbidity and mortality in community-dwelling adults aged 65 and older (N = 5,888 [11–14]). Participants from four U.S. communities were recruited during the period 1989–1990 (n = 5,201) and a second cohort of African Americans were recruited in 1992–1993 (n = 687). We used a public-use copy of the Cardiovascular Health Study data (N = 5,795; 93 did not consent to be part of the public-use data) obtained from the National Heart, Lung, and Blood Institute, which also sponsored the study. Of the 5,795 participants, 267 had no data on baseline orthostatic hypotension. Of the remaining 5,528 participants, 255 patients with centrally adjudicated prevalent HF at baseline were excluded (6,7,15), resulting in a final sample size of 5,273 older adults free of baseline HF. Missing values for covariates were imputed based on values predicted by age, sex, and race.
Baseline Orthostatic Hypotension
Baseline blood pressure was measured using a mercury sphygmomanometer after 20 minutes of rest in the supine position, as well as after 3 minutes of standing. Orthostatic hypotension was defined as a systolic blood pressure drop of ≥20 mmHg or a diastolic blood pressure drop of ≥10 mmHg after 3 minutes of standing, or dizziness, lightheadedness, or faintness upon standing (9). Participants in this latter category were considered to have symptomatic orthostatic hypotension. Of the 5,273 older adults without HF, 937 (18%) had baseline orthostatic hypotension, of whom 184 (20%) were symptomatic.
Incident Heart Failure and Other Outcomes
The primary outcome of the current study was new-onset HF during 13 years of follow-up. The Cardiovascular Health Study Events Committee centrally adjudicated incident HF. The process of adjudication has been previously described (6,7,16) and has been described as comparable to the Framingham criteria for the diagnosis of HF (17). Briefly, self-reports of physician-diagnosed HF during semiannual visits were validated by medical record review for symptoms, signs, and other supporting findings suggestive of HF, use of medications commonly used for HF, and follow-up surveillance assessments. Secondary outcomes included all-cause mortality and incident cardiovascular events, namely, acute myocardial infarction, angina pectoris, stroke, and peripheral arterial disease.
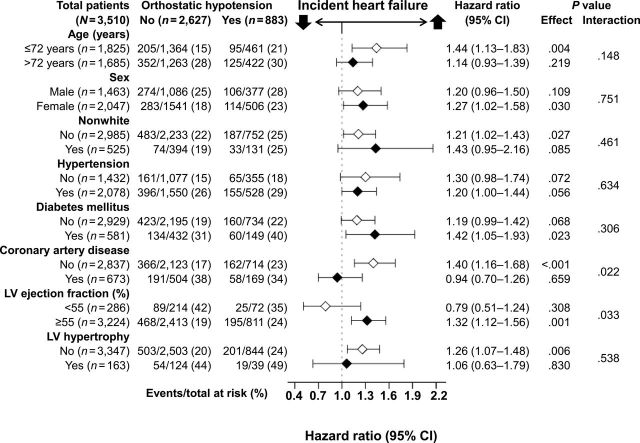
Assembly of a Balanced Study Cohort
To attenuate the confounding effect of other HF risk factors, the prevalence of which were likely to be higher in those with orthostatic hypotension (2,9), we used propensity score matching to assemble a cohort in which those with and without orthostatic hypotension would be well balanced in all measured baseline characteristics (18–20). Propensity scores or probabilities of orthostatic hypotension were estimated for each of the 5,273 participants using a nonparsimonious multivariable logistic regression model (21–23). In the model, orthostatic hypotension was used as the dependent variable and the 40 baseline characteristics displayed in Figure 1 were entered as covariates. A greedy matching protocol was used to match each participant with orthostatic hypotension with up to three participants without orthostatic hypotension who had similar propensity scores (24,25). Thus, we matched 883 orthostatic hypotension participants with another 2,627 nonorthostatic hypotension participants. Absolute standardized differences for all 40 covariates were estimated and presented as Love plots (26,27). Of the 883 matched participants with orthostatic hypotension, 173 (20%) had symptomatic orthostatic hypotension.
Figure 1.
Love plots displaying absolute standardized differences comparing 40 baseline characteristics between patients with and those without baseline orthostatic hypotension in the Cardiovascular Health Study, before and after propensity score matching.
Statistical Analysis
Pearson chi-square test, Student t test, Wilcoxon rank-sum test, and paired-sample t test were used to compare between-group baseline characteristics, before and after propensity matching, as appropriate. We used Kaplan–Meier and Cox proportional hazard analyses to estimate the associations of orthostatic hypotension with incident HF and other outcomes. Subgroup analyses were conducted to examine homogeneity of association with incident HF. To understand the impact of symptoms of dizziness associated with orthostatic hypotension, we separately examined the associations of symptomatic (n = 173) and asymptomatic (n = 710) orthostatic hypotension (versus those without; n = 2,627) with incident HF. A formal sensitivity analysis was conducted to quantify the degree of a hidden bias that would need to be present to invalidate our conclusions based on the propensity-matched cohort (28). We then repeated our analysis in all 5,273 prematch participants using three different Cox regression models: (a) unadjusted; (b) multivariable-adjusted, using all covariates used in the propensity score model; and (c) propensity score–adjusted models. All statistical tests were two-tailed with 95% confidence levels and a p value < .05 was considered significant. SPSS for Windows, version 20 (IBM Corp., Armonk, NY) was used for all data analysis.
Results
Baseline Characteristics
Participants (n = 3,510) had a mean (±standard deviation) age of 74 (±6) years, 58% were women, and 15% were nonwhite. Imbalances in baseline characteristics before matching and balances achieved after matching between patients with and without orthostatic hypotension are displayed in Table 1. Among those with orthostatic hypotension, mean drops in systolic and diastolic blood pressures were 20 and 7 mmHg, respectively. There was no significant difference in drop of either blood pressure between participants with symptomatic and those with asymptomatic orthostatic hypotension (p = .913 and .302, respectively). After matching, standardized differences for all measured covariates were <10%, suggesting substantial covariate balance across the groups (Figure 1).
Table 1.
Baseline Characteristics of Participants With and Without Orthostatic Hypotension, Before and After Propensity Score Matching
| Variable, n (%) or Mean (± SD) | Before Matching (n = 5,273) | After Matching (n = 3,510) | ||||
|---|---|---|---|---|---|---|
| Orthostatic Hypotension | p Value | Orthostatic Hypotension | p Value | |||
| No (n = 4,336) | Yes (n = 937) | No (n = 2,627) | Yes (n = 883) | |||
| Age, years | 73 (6) | 74 (6) | <.001 | 74 (6) | 74 (6) | .705 |
| Female | 2,495 (58) | 540 (58) | .960 | 1,541 (59) | 506 (57) | .480 |
| Nonwhite | 711 (16) | 142 (15) | .349 | 394(15) | 131(15) | .907 |
| Married | 2,884 (67) | 616 (66) | .650 | 1,738 (66) | 584 (66) | .991 |
| Education, college or higher | 1,912 (44) | 363 (39) | .003 | 1,024 (39) | 348 (39) | .820 |
| Income, ≥25,000 | 1,591 (37) | 326 (35) | .273 | 907 (35) | 315 (36) | .536 |
| Smoking, pack years | 17 (27) | 17 (26) | .825 | 18 (28) | 17 (25) | .487 |
| Alcohol per week, units | 2.6 (6.6) | 2.1 (5.8) | .015 | 2.1 (5.2) | 2.2 (6.0) | .766 |
| Body mass index, kg/m2 | 27 (4) | 26 (4) | <.001 | 26 (4) | 26 (4) | .644 |
| General health fair to poor | 961 (22) | 257(27) | .001 | 693 (26) | 226 (26) | .646 |
| Pulse rate, beats per minute | 68 (11) | 68 (12) | .577 | 68 (11) | 68 (11) | .971 |
| Systolic blood pressure, mmHg | 136 (21) | 138 (23) | .029 | 137 (22) | 138 (23) | .512 |
| Diastolic blood pressure, mmHg | 71 (11) | 69 (12) | <.001 | 70 (11) | 70 (12) | .664 |
| Ankle arm index ratio | 1.07 (0.17) | 1.04 (0.18) | <.001 | 1.06 (0.17) | 1.05 (0.17) | .179 |
| Morbidities | ||||||
| Coronary artery disease | 741 (17) | 188 (20) | .030 | 504 (19) | 169 (19) | .976 |
| Hypertension | 2,513 (58) | 571 (61) | .093 | 1,550 (59) | 528 (60) | .678 |
| Diabetes | 666 (15) | 167 (18) | .061 | 432 (16) | 149 (17) | .766 |
| Stroke | 149 (3) | 52 (6) | .002 | 117 (5) | 43 (5) | .608 |
| COPD | 530 (12) | 121 (13) | .560 | 345 (13) | 117 (13) | .929 |
| Cancer | 626 (14) | 142 (15) | .572 | 411 (16) | 134 (15) | .739 |
| Arthritis | 2,206 (51) | 465 (50) | .488 | 1,320 (50) | 438 (50) | .741 |
| Atrial fibrillation, by ECG | 91 (2) | 21 (2) | .784 | 63 (2) | 19 (2) | .675 |
| LV hypertrophy, by ECG | 180 (4) | 50 (5) | .107 | 124 (5) | 39 (4) | .711 |
| LV ejection fraction, <55% | 309 (7) | 83 (9) | .067 | 214 (8) | 72 (8) | .994 |
| Antihypertensive drug use | 1,962 (45) | 449 (48) | .137 | 1,204 (46) | 413 (47) | .608 |
| ACE inhibitors | 291 (7) | 54 (6) | .287 | 168 (6) | 49 (6) | .367 |
| Beta-blockers | 542 (13) | 129 (14) | .291 | 330 (13) | 118 (13) | .537 |
| Calcium channel blockers | 537 (12) | 128 (14) | .286 | 344 (13) | 116 (13) | .974 |
| Diuretics | 1,164 (27) | 270 (29) | .219 | 708 (27) | 252 (29) | .360 |
| Geriatric parameters | ||||||
| ADL score | 0.11 (0.45) | 0.13 (0.49) | .190 | 0.12 (0.50) | 0.12 (0.46) | .862 |
| IADL score | 0.31 (0.68) | 0.35 (0.71) | .126 | 0.34 (0.72) | 0.34 (0.70) | .929 |
| Walk block last week | 40 (55) | 37 (54) | .141 | 37 (52) | 38 (54) | .844 |
| Time to walk 15 feet, seconds | 5.7 (2.1) | 5.8 (2.2) | .198 | 5.8 (2.2) | 5.8 (2.1) | .799 |
| Loss balance | 940 (22) | 239 (26) | .011 | 629 (24) | 213 (24) | .914 |
| Orthostatic dizziness | 855 (20) | 184 (20) | .955 | 508 (19) | 173 (20) | .869 |
| Fall frequency | 125 (3) | 43 (5) | .007 | 104 (4) | 35 (4) | .995 |
| Laboratory data | ||||||
| Serum glucose, mg/dL | 111 (36) | 112 (37) | .362 | 111 (35) | 112 (37) | .583 |
| Serum creatinine, mg/dL | 0.95 (0.35) | 0.99 (0.51) | .009 | 0.95 (0.35) | 0.96 (0.31) | .537 |
| Hemoglobin, g/dL | 14.0 (1.3) | 14.0 (1.4) | .894 | 14.0 (1.4) | 14.0 (1.4) | .558 |
| Serum uric acid, mg/dL | 5.7 (1.5) | 5.5 (1.5) | .005 | 5.6 (1.5) | 5.6 (1.5) | .818 |
| Serum total cholesterol, mg/dL | 212 (39) | 212 (40) | .784 | 213 (39) | 212 (40) | .947 |
| Serum triglyceride, mg/dL | 138 (75) | 143 (79) | .072 | 140 (74) | 142 (76) | .619 |
| Serum albumin, g/dL | 4.00 (0.29) | 4.01 (0.30) | .021 | 4.01 (0.29) | 4.01 (0.30) | .671 |
| Serum C-reactive protein, mg/dL | 4.7 (8.2) | 4.5 (8.0) | .518 | 4.6 (8.0) | 4.5 (8.1) | .807 |
| Serum insulin, μU/mL | 16.6 (23.9) | 16.8 (23.9) | .760 | 16.4 (22.5) | 16.7 (24.1) | .761 |
Notes: ACE = angiotensin-converting enzyme; ADL = activities of daily living; COPD = chronic obstructive pulmonary diseases; ECG = electrocardiography; IADL = instrumental activities of daily living; LV = left ventricular; LVH = left ventricular hypertrophy, SD = standard deviation.
Association of Orthostatic Hypotension With Incident Heart Failure
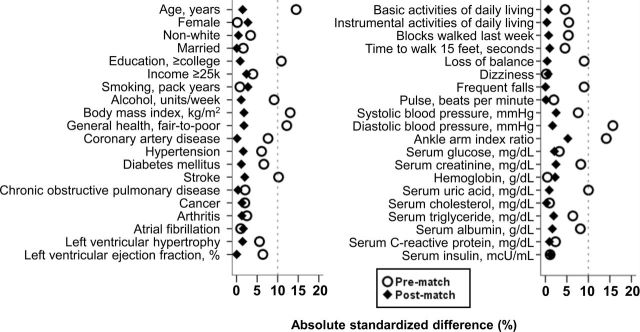
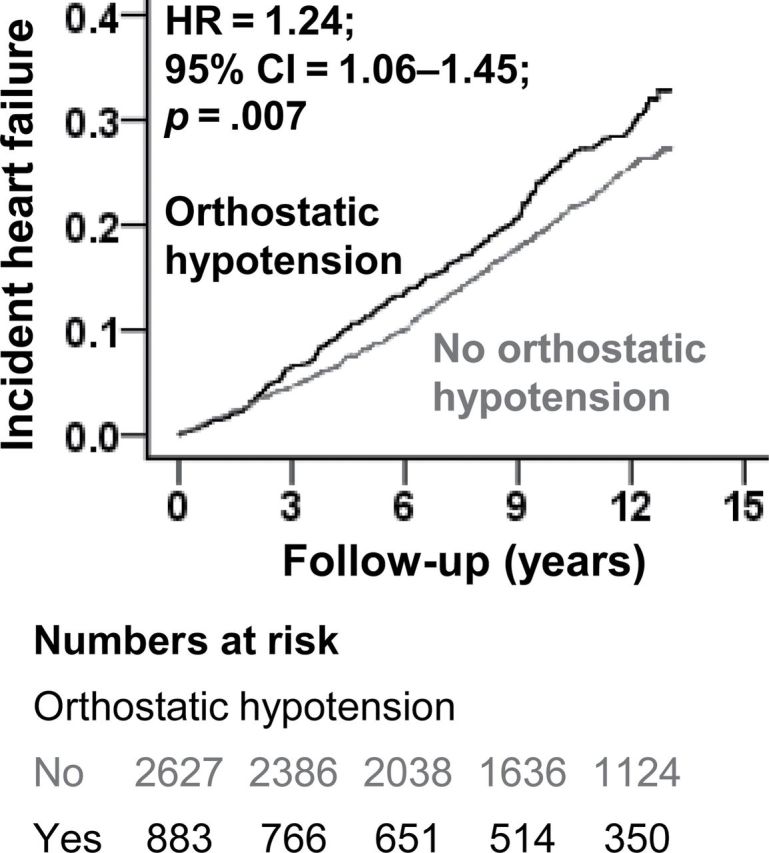
Incident HF occurred in 25% and 21% of matched participants with and those without orthostatic hypotension, respectively, during 13 years of follow-up (hazard ratio [HR] associated with orthostatic hypotension, 1.24; 95% confidence interval [CI], 1.06–1.45; p = .007, Table 2, Figure 2). This association was rather homogeneous across various clinically relevant subgroups, except for subgroups with and without coronary artery disease and asymptomatic left ventricular systolic dysfunction (Figure 3). Compared with older adults without orthostatic hypotension, HRs associated with symptomatic (n = 173) and asymptomatic (n = 710) orthostatic hypotension were 1.57 (95% CI, 1.16–2.11; p = .003) and 1.17 (95% CI, 0.99–1.39; p = .069), respectively. Among the 5,273 prematched participants, unadjusted, multivariable-adjusted, and propensity score–adjusted HRs for incident HF associated with orthostatic hypotension were 1.42 (95% CI, 1.23–1.64; p < .001), 1.29 (95% CI, 1.11–1.50; p = .001), and 1.24 (95% CI, 1.07–1.43; p = .005), respectively (Table 2).
Table 2.
Associations of Baseline Orthostatic Hypotension With Incident Heart Failure
| Outcomes | % (events/total) | Hazard Ratio, (95% CI); p Value | |
|---|---|---|---|
| No Orthostatic Hypotension | Orthostatic Hypotension | ||
| Prematched | |||
| Unadjusted | 20% (850/4,336) | 25% (237/937) | 1.42 (1.23–1.64); p < .001 |
| Multivariable-adjusted* | — | — | 1.29 (1.11–1.50); p = .001 |
| Propensity score–adjusted | — | — | 1.24 (1.07–1.43); p = .005 |
| Matched | 21% (557/2,627) | 25% (220/883) | 1.24 (1.06–1.45); p = .007 |
*Adjusted for all variables in Figure 1.
Figure 2.
Kaplan–Meier plot for incident heart failure by baseline orthostatic hypotension (CI = confidence interval; HR = hazard ratio).
Figure 3.
Association of baseline orthostatic hypotension with incident heart failure in subgroups of propensity-matched cohort of older adults in the Cardiovascular Health Study. CI = confidence interval; LV = left ventricular.
Association of Orthostatic Hypotension With Other Outcomes
Baseline orthostatic hypotension had no significant association with all-cause mortality or other incident cardiovascular events (Table 3). However, compared with those without orthostatic hypotension, matched participants with symptomatic orthostatic hypotension had higher risk of all-cause mortality (HR, 1.45; 95% CI, 1.18–1.77; p < .001), incident acute myocardial infarction (HR, 1.22; 95% CI, 0.75–1.96; p = .423), angina pectoris (HR, 1.74; 95% CI, 1.24–2.47; p < .001), and stroke (HR, 1.69; 95% CI, 1.19–2.42; p = .004). Orthostatic hypotension associated with unadjusted, multivariable-adjusted, and propensity-adjusted HRs for all-cause mortality and other cardiovascular events in the prematch cohort are displayed in Table 3.
Table 3.
Associations of Baseline Orthostatic Hypotension With Other Outcomes
| Outcomes | % (events/total) | Hazard Ratio, (95% CI); p Value | |
|---|---|---|---|
| No Orthostatic Hypotension | Orthostatic Hypotension | ||
| All-cause mortality | |||
| Prematch (unadjusted) | 42% (1,826/4,336) | 51% (474/937) | 1.30 (1.17–1.43); p < .001 |
| Postmatch (adjusted) | 47% (1,221/2,627) | 50% (437/883) | 1.10 (0.99–1.23); p = .084 |
| Incident acute myocardial infarction* | |||
| Prematch (unadjusted) | 11% (451/3,992) | 14% (117/848) | 1.31 (1.07–1.61); p = .009 |
| Postmatch (adjusted) | 12% (278/2,380) | 13% (108/804) | 1.20 (0.96–1.50); p = .112 |
| Incident angina pectoris* | |||
| Prematch (unadjusted) | 19% (693/3,721) | 21% (166/784) | 1.22 (1.03–1.45); p = .021 |
| Postmatch (adjusted) | 19% (413/2,207) | 21% (156/746) | 1.17 (0.97–1.40); p = .100 |
| Incident stroke* | |||
| Prematch (unadjusted) | 13% (549/4,187) | 16% (141/885) | 1.30 (1.08–1.57); p = .005 |
| Postmatch (adjusted) | 14% (345/2,510) | 16% (132/840) | 1.18 (0.97–1.44); p = .106 |
| Incident peripheral artery disease | |||
| Prematch (unadjusted) | 4% (162/4,336) | 4% (36/937) | 1.09 (0.76–1.56); p = .640 |
| Postmatch (adjusted) | 4% (113/2,627) | 4% (31/883) | 0.84 (0.56–1.25); p = .381 |
*Baseline-prevalent cases were excluded from the at-risk populations.
Discussion
Findings from our study demonstrate that among community-dwelling older adults, baseline orthostatic hypotension has independent association with higher risk for incident HF but not with other incident cardiovascular events or mortality. The association with incident HF was mostly mediated by symptomatic orthostatic hypotension. Further, symptomatic orthostatic hypotension also had independent associations with total mortality, incident stroke, and incident angina pectoris. These findings suggest that in older adults, orthostatic hypotension may not be an independent risk factor for mortality and cardiovascular morbidity unless associated with symptoms of dizziness.
Older adults with orthostatic hypotension had higher prevalence of many HF risk factors such as coronary artery disease and stroke, which may in part explain the unadjusted association with higher risk of incident HF. Adjustment for these and other confounders attenuated this association but did not render it to nonsignificance. The persistent association of orthostatic hypotension and incident HF among matched older adults is unlikely to be explained by any of the measured baseline risk factors that were balanced between the groups. This leaves the potential for confounding by unmeasured confounders. However, findings from our sensitivity analysis suggest that a hidden binary covariate that is a near-perfect predictor of incident HF would need to increase the odds of orthostatic hypotension by 14% to explain away this association, suggesting that the association observed in our study was rather insensitive to bias due to unmeasured confounders (28).
Another potential explanation is that although our matching allowed a balance in the prevalence of risk factors such as coronary artery disease, it is possible that those with orthostatic hypotension hadmore severe disease, which progressed at a faster rate during follow-up, leading to more new HF cases. Our observation of lack of an association of asymptomatic orthostatic hypotension and the similarity in drop of blood pressure in those with symptomatic and asymptomatic orthostatic hypotension is intriguing and suggests that blood pressure dysregulation per se may not be prognostically important. Although orthostatic hypotension has been shown to be associated with left ventricular hypertrophy, vascular stiffness, and impaired ventricular filling in older adults (29–31), these cross-sectional observations are likely due to shared pathophysiology and may not imply causal associations.
Several studies have examined the association of orthostatic hypotension with incident HF in middle-aged adults (1,2). In contrast, the current study is based on community-dwelling older adults in whom both orthostatic hypotension and HF are common. Further, in contrast to previous studies in which incident HF was primarily based on hospitalized HF patients, HF was centrally adjudicated in our study based on both inpatient and outpatient diagnoses (16). Findings from our study also demonstrated, for the first time, the association of orthostatic hypotension with incident HF and other adverse outcomes were more pronounced in the presence of orthostatic dizziness. Finally, propensity matching allowed us to assemble a balanced cohort and conclude that the association of orthostatic hypotension with incident HF is unlikely to be explained by baseline imbalances in other measured risk factors.
Risk factors for HF in older adults may vary from those in younger adults. Nontraditional risk factors such as isolated diastolic hypotension, impairment of activities of daily living, and hypoalbuminemia may be risk factors for incident HF in older adults (7,32,33). Findings from the current study suggest that orthostatic hypotension, especially when associated with dizziness, maybe a new nontraditional risk factor for HF in old age. Orthostatic hypotension is easily measured in clinical practice and should be routinely assessed in older adults. Although primary orthostatic hypotension has no effective therapy, iatrogenic orthostatic hypotension may be avoided by avoiding culprit drugs and aggressive initiation of antihypertensive drugs (34).
Our study has several limitations that are typical for an observational study. Despite the displayed balance in all measured baseline covariates, bias due to imbalances in unmeasured covariates is possible. It is possible that participants without baseline orthostatic hypotension developed orthostatic hypotension during follow-up and vice versa. This regression dilution may have attenuated the association observed in our study (35). Future studies need to develop interventions that may reduce the risk of orthostatic hypotension in older adults. The A allele of the single-nucleotide polymorphism rs4149601, located in the NEDD4L gene and associated with blood pressure variations, has been shown to be protective against orthostatic hypotension in those with hypertension (36). However, the investigators of the Genetics of Postural Hemodynamics Consortium have recently examined 31 recently discovered blood pressure–associated single-nucleotide polymorphisms and observed weak associations between these gene variants and orthostatic hypotension (37).
In conclusion, among community-dwelling older adults, baseline orthostatic hypotension is associated with higher risk of incident HF, which appears to be more pronounced in those with associated dizziness. Future studies need to develop and test interventions to treat orthostatic hypotension.
Funding
R.M.A. is supported by the National Institutes of Health through grant 5UL1 RR025777.
Acknowledgment
The Cardiovascular Health Study (CHS) was conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with the CHS Investigators. This manuscript was prepared using a limited access data set obtained by the NHLBI and does not necessarily reflect the opinions or views of the CHS Study or the NHLBI.
References
- 1. Jones CD, Loehr L, Franceschini N, et al. Orthostatic hypotension as a risk factor for incident heart failure: the atherosclerosis risk in communities study. Hypertension. 2012;59:913–918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fedorowski A, Engström G, Hedblad B, Melander O. Orthostatic hypotension predicts incidence of heart failure: the Malmö preventive project. Am J Hypertens. 2010;23:1209–1215 [DOI] [PubMed] [Google Scholar]
- 3. Kawaguchi T, Uyama O, Konishi M, Nishiyama T, Iida T. Orthostatic hypotension in elderly persons during passive standing: a comparison with young persons. J Gerontol A Biol Sci Med Sci. 2001;56:M273–M280 [DOI] [PubMed] [Google Scholar]
- 4. Belmin J, Abderrhamane M, Medjahed S, et al. Variability of blood pressure response to orthostatism and reproducibility of the diagnosis of orthostatic hypotension in elderly subjects. J Gerontol A Biol Sci Med Sci. 2000;55:M667–M671 [DOI] [PubMed] [Google Scholar]
- 5. Ooi WL, Hossain M, Lipsitz LA. The association between orthostatic hypotension and recurrent falls in nursing home residents. Am J Med. 2000;108:106–111 [DOI] [PubMed] [Google Scholar]
- 6. Ekundayo OJ, Allman RM, Sanders PW, et al. Isolated systolic hypertension and incident heart failure in older adults: a propensity-matched study. Hypertension. 2009;53:458–465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Guichard JL, Desai RV, Ahmed MI, et al. Isolated diastolic hypotension and incident heart failure in older adults. Hypertension. 2011;58:895–901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Verwoert GC, Mattace-Raso FU, Hofman A, et al. Orthostatic hypotension and risk of cardiovascular disease in elderly people: the Rotterdam study. J Am Geriatr Soc. 2008;56:1816–1820 [DOI] [PubMed] [Google Scholar]
- 9. Rutan GH, Hermanson B, Bild DE, Kittner SJ, LaBaw F, Tell GS. Orthostatic hypotension in older adults. The Cardiovascular Health Study. CHS Collaborative Research Group. Hypertension. 1992;19(6 Pt 1):508–519 [DOI] [PubMed] [Google Scholar]
- 10. Fitzmaurice G. Confounding: regression adjustment. Nutrition. 2006;22:581–583 [DOI] [PubMed] [Google Scholar]
- 11. Hirsch CH, Fried LP, Harris T, Fitzpatrick A, Enright P, Schulz R. Correlates of performance-based measures of muscle function in the elderly: the Cardiovascular Health Study. J Gerontol A Biol Sci Med Sci. 1997;52:M192–M200 [DOI] [PubMed] [Google Scholar]
- 12. Newman AB, Haggerty CL, Kritchevsky SB, Nevitt MC, Simonsick EM; Health ABC Collaborative Research Group. Walking performance and cardiovascular response: associations with age and morbidity–the Health, Aging and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2003;58:715–720 [DOI] [PubMed] [Google Scholar]
- 13. Fried LF, Shlipak MG, Stehman-Breen C, et al. Kidney function predicts the rate of bone loss in older individuals: the Cardiovascular Health Study. J Gerontol A Biol Sci Med Sci. 2006;61:743–748 [DOI] [PubMed] [Google Scholar]
- 14. Inzitari M, Naydeck BL, Newman AB. Coronary artery calcium and physical function in older adults: the Cardiovascular Health Study. J Gerontol A Biol Sci Med Sci. 2008;63:1112–1118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Psaty BM, Kuller LH, Bild D, et al. Methods of assessing prevalent cardiovascular disease in the Cardiovascular Health Study. Ann Epidemiol. 1995;5:270–277 [DOI] [PubMed] [Google Scholar]
- 16. Ives DG, Fitzpatrick AL, Bild DE, et al. Surveillance and ascertainment of cardiovascular events. The Cardiovascular Health Study. Ann Epidemiol. 1995;5:278–285 [DOI] [PubMed] [Google Scholar]
- 17. Schellenbaum GD, Rea TD, Heckbert SR, et al. Survival associated with two sets of diagnostic criteria for congestive heart failure. Am J Epidemiol. 2004;160:628–635 [DOI] [PubMed] [Google Scholar]
- 18. Rosenbaum PR, Rubin DB. The central role of propensity score in observational studies for causal effects. Biometrika. 1983;70: 41–55 [Google Scholar]
- 19. Rubin DB. Using propensity score to help design observational studies: Application to the tobacco litigation. Health Serv Outcome Res Methodol. 2001;2:169–188 [Google Scholar]
- 20. Ahmed A, Husain A, Love TE, et al. Heart failure, chronic diuretic use, and increase in mortality and hospitalization: an observational study using propensity score methods. Eur Heart J. 2006;27: 1431–1439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Williams BR, Zhang Y, Sawyer P, et al. Intrinsic association of widowhood with mortality in community-dwelling older women and men: findings from a prospective propensity-matched population study. J Gerontol A Biol Sci Med Sci. 2011;66:1360–1368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Du XL, Jones DV, Zhang D. Effectiveness of adjuvant chemotherapy for node-positive operable breast cancer in older women. J Gerontol A Biol Sci Med Sci. 2005;60:1137–1144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Juliebø V, Krogseth M, Skovlund E, Engedal K, Wyller TB. Medical treatment predicts mortality after hip fracture. J Gerontol A Biol Sci Med Sci. 2010;65:442–449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ahmed A, Fonarow GC, Zhang Y, et al. Renin-angiotensin inhibition in systolic heart failure and chronic kidney disease. Am J Med. 2012;125:399–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ahmed A, Rich MW, Zile M, et al. Renin-angiotensin inhibition in diastolic heart failure and chronic kidney disease. Am J Med. 2013;126:150–161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Patel K, Fonarow GC, Kitzman DW, et al. Angiotensin receptor blockers and outcomes in real-world older patients with heart failure and preserved ejection fraction: a propensity-matched inception cohort clinical effectiveness study. Eur J Heart Fail. 2012;14 1179–1188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mujib M, Patel K, Fonarow GC, et al. Angiotensin-converting enzyme inhibitors and outcomes in heart failure and preserved ejection fraction. Am J Med. 2013;126:401–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rosenbaum PR. Sensitivity to hidden bias.In: Rosenbaum PR, ed. Observational Studies. Vol. 1 New York, NY: Springer; 2002: 105–170 [Google Scholar]
- 29. Boddaert J, Tamim H, Verny M, Belmin J. Arterial stiffness is associated with orthostatic hypotension in elderly subjects with history of falls. J Am Geriatr Soc. 2004;52:568–572 [DOI] [PubMed] [Google Scholar]
- 30. Gottdiener JS, Yanez D, Rautaharju P, et al. Orthostatic Hypotension in the Elderly: Contributions of Impaired LV Filling and Altered Sympathovagal Balance. Am J Geriatr Cardiol. 2000;9:273–280 [DOI] [PubMed] [Google Scholar]
- 31. Fan XH, Wang Y, Sun K, et al. Disorders of orthostatic blood pressure response are associated with cardiovascular disease and target organ damage in hypertensive patients. Am J Hypertens. 2010;23:829–837 [DOI] [PubMed] [Google Scholar]
- 32. Bowling CB, Fonarow GC, Patel K, et al. Impairment of activities of daily living and incident heart failure in community-dwelling older adults. Eur J Heart Fail. 2012;14:581–587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Filippatos GS, Desai RV, Ahmed MI, et al. Hypoalbuminaemia and incident heart failure in older adults. Eur J Heart Fail. 2011;13:1078–1086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gupta V, Lipsitz LA. Orthostatic hypotension in the elderly: diagnosis and treatment. Am J Med. 2007;120:841–847 [DOI] [PubMed] [Google Scholar]
- 35. Clarke R, Shipley M, Lewington S, et al. Underestimation of risk associations due to regression dilution in long-term follow-up of prospective studies. Am J Epidemiol. 1999;150:341–353 [DOI] [PubMed] [Google Scholar]
- 36. Luo F, Wang Y, Wang X, Sun K, Zhou X, Hui R. A functional variant of NEDD4L is associated with hypertension, antihypertensive response, and orthostatic hypotension. Hypertension. 2009;54:796–801 [DOI] [PubMed] [Google Scholar]
- 37. Fedorowski A, Franceschini N, Brody J, et al. Orthostatic hypotension and novel blood pressure-associated gene variants: Genetics of Postural Hemodynamics (GPH) Consortium. Eur Heart J. 2012;33: 2331–2341 [DOI] [PMC free article] [PubMed] [Google Scholar]