Pregnant women who request a caesarean section should not automatically get one if there are no medical reasons to support it, say new guidelines.
Instead they should be properly counselled about the merits and demerits of caesarean section and vaginal birth and how labour can be managed so that they can make a fully informed choice about the best care for themselves and their baby. If a doctor still thinks that a caesarean section is inappropriate then the request can be declined, but the woman should be referred to another doctor.
The new guidelines, published by the National Collaborating Centre for Women's and Children's Health for the National Institute for Clinical Excellence, outline the possible benefits and risks of caesarean section on the basis of available research.
They also suggest how rates of caesarean section can be reduced—for example, by introducing fetal blood sampling alongside more standard tests, such as fetal heart monitoring, or by using external cephalic version at 36 weeks' gestation for women with a breech presentation.
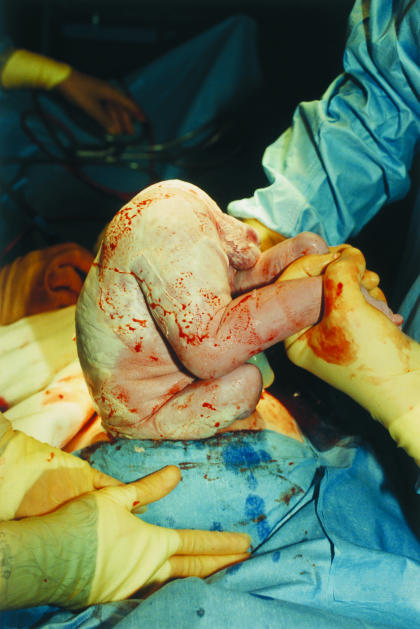
Figure 1.
Seven per cent of caesarean sections in 2001 were the result of the mother's request
Credit: LAWRENCE LAWRY/SPL
The rate of caesarean sections has been climbing for the past 25 years, and many people with an interest in obstetrics feel it is too high.
Figures from the national sentinel caesarean section audit carried out for 2001 show that 21.5% of pregnant women in England and Wales had a caesarean section, although the rates varied—from 18% to 25%—around both countries. Of those women who did have a caesarean section, 7% (representing 1.5% of all births) were the result of the mother's request.
Professor David James, professor of fetomaternal medicine and director of medical education at Queen's Medical Centre in Nottingham, estimates that 10% of indications for caesarean section are invalid. Since 2001, his unit has reduced its rate of caesarean deliveries from 29% to 21-22%. It has done this by reducing the incidence of unnecessary induction of labour, moving from a two hourly to four hourly review of progress during labour, and encouraging women who have had a previous caesarean to opt for a vaginal birth.
“There is no doubt that a smaller number of women having vaginal birth have complications than do those who have a caesarean section, but there are risks associated with both types of birth. If there was clear evidence that one way was better than another we would not need a guideline,” said Professor James.
The guidelines can be accessed at www.rcog.org.uk or www.nice.org.uk