Pain in the hip
Childhood
A child with hip disease may not present with pain or a history of trauma but with an unexplained limp. Unexplained knee pain should raise the suspicion of hip abnormality.
Congenital dislocation of the hip—Ultrasound screening should detect children at risk, but missed cases may present with a delay in walking, limp, or discrepancy in leg length. Children usually present before the age of 5 years. Missed diagnosis can lead to a non-congruent joint and early osteoarthritic degeneration in adulthood.
Perthes' disease—Disintegration of the femoral head, with subsequent healing and deformity of the hip, usually occurs in boys aged 5-10 years. The precise cause is unclear, but segmental avascular necrosis of the femoral head is probably responsible. A limp, hip pain, or knee pain may result. Treatment aims to contain the femoral head in the acetabulum to reduce the risks of future osteoarthritis.
Figure 1.
Anteroposterior radiograph of child with dislocated right hip. Note the lateral displacement of the femur and the poorly developed ossific nucleus of the hip
Slipped upper femoral epiphysis is typically seen in overweight, hypogonadal boys, who often present with pain referred to the knee, although girls can also be affected. Diagnosis can be difficult, but a “frog lateral” radiograph will show the deformity. Surgical stabilisation is needed urgently to prevent further slippage of the epiphysis. The contralateral hip is at high risk of slippage, and patients and parents should be warned to return if any knee or hip pain occurs.
Septic arthritis is relatively uncommon, but it should be suspected in a child who is ill, toxic, and unable to walk. Pain prevents movement of the affected joint. Diagnosis is confirmed by raised white cell count and erythrocyte sedimentation rate and perhaps by effusion on ultrasound images. Urgent surgical drainage is vital to reduce the risk of late osteoarthritis. Diagnosis can be particularly difficult in neonates. Staphylococcus aureus is the usual infective organism.
Transient synovitis or “irritable hip”—A reactive effusion may occur in the hip in association with a systemic viral illness. Affected children are not acutely unwell and can move the hip, but with some stiffness. Ultrasonography may show an effusion. The condition is usually self limiting. Perthes' disease may also present in the early stages with an effusion without changes visible on radiography.
Other arthritides—Juvenile chronic arthritis may present with hip pain. General management of the arthritic process is important, with physiotherapy to prevent joint contracture.
Figure 2.
Radiograph of child's right hip. Displacement of the epiphysis relative to the femoral neck is easily seen
Adults
Pain from the hip is usually felt in the groin or lateral or anterior thigh. Referred pain to the knee is easily missed. Although buttock pain may originate from the hip, the lumbar spine is the usual source. Hip disorders often produce a limp, a reduced walking distance, and stiffness that prevents activities of daily living, such as getting in and out of baths, putting on shoes, and foot care.
Table 1.
Causes of hip pain in adults
| • Osteoarthritis |
| • Other arthritides: |
| Rheumatoid arthritis |
| Psoriatic arthritis |
| Ankylosing spondylitis |
| • Hip fracture |
| • Paget's disease |
| • Avascular necrosis |
| • Malignancy |
| • Infection |
| • Painful soft tissue conditions around the hip: |
| Trochanteric bursitis |
| Snapping ilio-psoas tendon |
| Torn acetabular labrum |
Osteoarthritis—Osteoarthritis is one of the commonest causes of hip pain in adults; although it usually develops in people over 60, it can occur at any age. Rest, simple analgesia, or a walking stick often relieve the pain. A limp may develop, with associated stiffness. In extreme situations, leg length is lost, and the hip adopts a fixed flexion and adduction deformity. Total hip replacement is effective at relieving pain.
This article is adapted from the third edition of the ABC of Rheumatology, which is published by BMJ Books
Other arthritides—Rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis can also produce hip pain. The last is particularly associated with stiffness. Total hip replacement is often needed.
Hip fracture—Osteoporotic hip fracture in elderly women is epidemic. A fall followed by inability to bear weight and a short externally rotated leg are diagnostic. An undisplaced fracture may not stop the patient bearing weight, and it may not be visible on initial radiograph. Repeat films are usually required, and a bone scan or magnetic resonance imaging if there is doubt. Treatment is by surgical stabilisation or by replacement of the femoral head (hemiarthroplasty). Considerable comorbidity is often found.
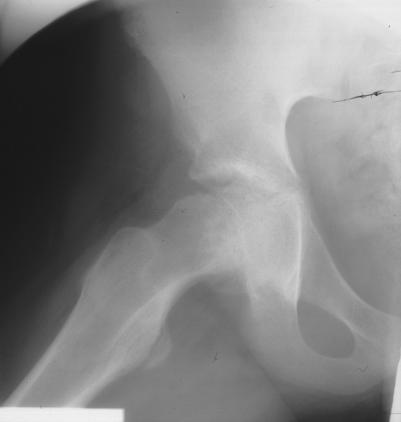
Figure 3.
Osteoarthritis of right hip with loss of joint space, subarticular cysts, peripheral osteophytes, and subchondral sclerosis
Paget's disease—The pelvis is often affected in Paget's disease and can cause hip pain. Treatment of the disease with bisphosphonates can reduce pain, but co-existent osteoarthritis of the hip can also occur.
Table 2.
Causes of avascular necrosis
| • Most cases are idiopathic |
| • Associated conditions include: |
| Excess alcohol |
| Prolonged steroid therapy |
| Working in pressurised environments—for example, deep sea divers |
Avascular necrosis—Segmental avascular necrosis of the weight bearing portion of the femoral head can occur. This produces progressive pain, limp, and late secondary osteoarthritis. Magnetic resonance imaging gives a diagnosis in the early stages, but if radiological evidence is established, surgical treatment to arrest the disease is less successful. Hip replacement may ultimately be required.
Malignancy—Metastases in the pelvis or proximal femur will produce hip pain. Treatment with local radiotherapy or bisphosphonates, or both, may slow progression. Surgical stabilisation of impending fractures may be required. Primary bone tumours as a cause of hip pain are extremely rare.
Infection—Primary septic arthritis is rare in adults, but it may present insidiously in immunocompromised patients. Plain radiography and ultrasonography may be needed to show the presence of an effusion. Surgical drainage is usually necessary.
Trochanteric bursitis—This is inflammation of the bursa between the greater trochanter and fascia lata. It is characterised by pain over the trochanter (not in the groin) and is usually self limiting. Local physiotherapy, anti-inflammatory drugs, rest, and occasionally local anaesthetic and steroid injections can help.
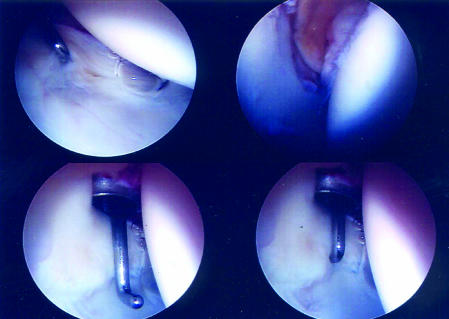
Figure 4.
Arthroscopic images of a hip. Top left shows small acetabular labral tear
Snapping ilio-psoas tendon—This causes a painful “clunk” in the groin when the hip goes from extension to flexion. The hip is otherwise normal. The psoas tendon impinges on the capsule of the hip anteriorally to produce discomfort. Radiography shows abnormal movement of fluoroscopic contrast agent injected into the psoas tendon. Surgical release may be needed.
Torn acetabular labrum—This produces pain in the groin on rotatory movements of the hip, and the hip may feel unstable or give way. Magnetic resonance imaging shows the abnormality, and the torn labrum can be removed arthroscopically.
Knee pain
Knee pain may present spontaneously or after injury. Stiffness or the inability to extend the knee fully indicate effusion within the joint. An effusion can be detected by the disappearance of the dimples either side of the patella, and it may produce a patellar “tap,” in which the patella can be pushed on to the anterior surface of the femur by the examiner's fingers.
Figure 5.
Right knee effusion: note the loss of dimples either side of the patella compared with left knee
Knee pain may be referred from the hip (see slipped upper femoral epiphysis, above). The knee is a more superficial joint than the hip, and so the site of pain and tenderness often indicates the site of an abnormality.
Children
Anterior knee pain is seen in adolescent girls. It is caused by softening of cartilage on the posterior aspect of the patella. Pain usually settles at skeletal maturity.
Patella subluxation is seen in girls with patellar maltracking and is sometimes related to tibial torsional deformities or valgus knees. It usually responds to physiotherapy.
Osgood-Schlatter disease—This is an osteochondritis of the tibial tubercle seen in adolescent boys. Localised pain and tenderness and swelling of the insertion of the patellar tendon are seen. The only treatment required is analgesia as the condition is self limiting.
Table 3.
Sporting injuries to the knee
| Origin | Symptoms | Cause |
|---|---|---|
| Twisting during football | Sudden pain and swelling | Haemarthrosis due to torn cruciate ligament or major meniscal detachment |
| Slowly developing effusion | Smaller meniscal tear | |
| Valgus strain | Medial pain and tenderness, no effusion | Torn medial collateral ligament |
Adults
Injuries
Sporting injuries of the knees often occur. Falls from heights and serious trauma can produce intra-articular fractures that need urgent orthopaedic referral.
Spontaneous knee pain, redness, and swelling
Acute arthritis may produce significant swelling, heat, and pain in the knee. Septic arthritis should be excluded if the patient is systemically unwell, although the signs can be masked by steroid treatment.
The knee should be aspirated under aseptic conditions and the fluid cultured to establish the diagnosis. Examination of the fluid for crystals should also be carried out. Intra-articular steroids should never be given until sepsis has been excluded.
Table 4.
Causes of acute, hot, red knee
| • Gout |
| • Pseudogout |
| • Other types of arthritis such as Reiter's syndrome |
Chronic pain and swelling
Osteoarthritis in the knee usually affects the medial compartment, with the development of a typical varus deformity. An effusion may be present, with medial joint line tenderness. Rheumatoid arthritis produces synovitis and effusions but may lead to a valgus deformity. Both may need total knee arthroplasty if conservative measures fail. Other arthritides, such as ankylosing spondylitis and psoriatic arthritis, may affect the knees.
Chronic pain and instability
Recurrent medial joint line pain, instability, and tenderness may indicate a chronic medial meniscal tear or osteoarthritis. Loose bodies may be produced in osteoarthritis, which can cause instability and intermittent pain; these may be palpable if they lie in the suprapatellar pouch. Osteochondritis dissecans is characterised by separation of areas of articular cartilage from their bony bed, leading to pain, swelling, and the knee “giving way.” The loose bodies may be palpable. Typical sites for such separation include the medial femoral condyle and the patella.
A chronically unstable knee may indicate an old rupture of the anterior cruciate ligament. Surgery is indicated for substantial instability and in professional sportspeople.
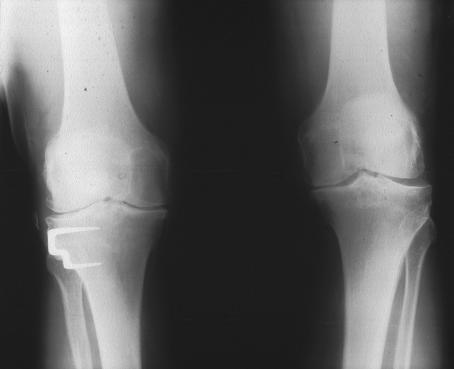
Figure 6.
Osteoarthritis of both knees. The left knee shows typical medial compartment disease; the right shows medial and lateral disease. The patient has had a high tibial osteotomy
Localised pain and swelling
Bursae occur in several sites around the knee. Swelling over the patellar ligament occurs with chronic kneeling; it responds to appropriate knee pads. Popliteal cysts (“Baker's cysts”) usually reflect underlying knee pathology and respond to treatment of the synovitis. Removal is potentially hazardous, and recurrence is common.
Semimembranous bursae are common in children on the posteromedial aspect of the knee. They usually disappear as the child grows
Andrew J Hamer is consultant orthopaedic surgeon at Northern General Hospital, Sheffield
The ABC of Rheumatology is edited by Michael L Snaith, senior lecturer in rheumatology, University of Sheffield.
Competing interests: None declared.
Further reading and resources
- • Solomon L, Nayagam D, Warwick D. Apley's system of orthopaedics and fractures. 8th ed. London: Arnold, 2001
- • McRae R. Clinical orthopaedic examination. Edinburgh: Churchill Livingstone, 1997
- • Miller MD, ed. Review of orthopaedics. Philadelphia: W B Saunders, 2000