Abstract
Objective
The purpose of this review was to assess the prevalence of unprotected anal intercourse (UAI) among men who have sex with men (MSM) in China.
Methods
A comprehensive search was conducted including online databases like “Wanfang”, Chinese National Knowledge Infrastructure, PubMed and manual searches. Analyses using random-effects models were performed to estimate the prevalence of UAI among MSM in China.
Results
Sixty-two articles reporting eighty-two studies were selected. The pooled prevalence rates of UAI with any male partner, with regular male partners, with non-regular male partners, with casual male partners, and with commercial male partners among MSM were 53%(95%CI: 51–56%), 45%(95%CI: 39–51%), 34%(95%CI: 24–45%), 33%(95%CI: 30–36%), 12% (95%CI: 5–26%), respectively. A cumulative meta-analysis found that the pooled UAI prevalence decreased over time.
Conclusions
Although the prevalence of UAI with male partners among MSM in China presents a decreasing trend over the past decade, the concomitant rise in HIV prevalence and incidence indicates that current prevention intervention efforts are insufficient to effectively contain the spread of HIV. Therefore, the persistently high prevalence of risky sexual behaviors underscores the need for innovative and effective prevention strategies among MSM.
Introduction
Approximately 7.3%, 11.0%, 14.7% and 17.4% of the estimated number of people living with HIV/AIDS in China were infected through unprotected male-to-male sexual contact in 2005, 2007, 2009 and 2011, respectively, reflecting a rapid expansion of the HIV epidemic among men who have sex with men (MSM) in recent years [1]–[4]. Data from meta-analyses [5]–[8] and sentinel surveillance [8], [9] have consistently demonstrated the rising trend of HIV prevalence and incidence among MSM across the nation. Estimated HIV prevalence and incidence increased to 6.0% (4.4–8.2) and 1.0 (0.7–1.3) per 100 person-years, respectively, in 2010 [8], which highlights the magnitude of the HIV epidemic in this population. Recent studies have consistently revealed the rapid expansion and severity of the epidemics of HIV and other sexually transmitted infections (STIs) among MSM in large metropolitan cities in China [6], [10]–[15].
The disproportionately high prevalence of HIV and STIs among MSM is associated with the prevalence of unprotected anal intercourse (UAI) [16], [17], which has been the leading high-risk behavior for HIV infection [18]–[21]. HIV can spread rapidly in a network with a high proportion of HIV-positive male partners engaging in UAI, or with seminal fluid ejaculated inside the rectum [22]–[24]. Men who report receptive UAI (URAI) are at higher risk of HIV infection, compared to men who report insertive UAI (UIAI) [20], [22], [23]; the risk increased by more than three-fold in an Australian cohort of homosexual men [23]. In addition, anal sex is more likely to be unprotected with regular male partners than with casual or commercial male partners [25]–[28], which is challenging for encouraging behavioral changes between steady male couples because UAI implies a commitment of love, fidelity and intimacy according to their perceptions [29], [30]. It cannot be denied that HIV-negative men in discordant couples have the highest risk of acquiring HIV among MSM [22], [23]. Moreover, increasing UAI may also offset the effects of antiretroviral therapy, even lead to HIV resurgence [32], [34], [35]. Conversely, empirical data and mathematical models have shown that decreasing risk behaviors are accompanied by decreasing reproduction numbers [31], [32]. Here the reproduction number is defined as the average number of secondary cases caused by a typical HIV case during its infectious period [33].
An earlier meta-analysis [36] reported that a decreasing trend was observed at last UAI with commercial partners, but no significant change at last UAI appeared prior to the year 2007 among MSM in China. The Chinese government realized the alarmingly high risk among MSM and scaled up intervention efforts among this group [37], and the first nationwide cross-sectional survey among MSM in 61 large cities was initiated in 2008 [38]. It is imperative to evaluate the prevalence of UAI among MSM in order to further guide intervention and prevention programs. This article systematically reviewed published studies to estimate UAI prevalence and characterize its trend among MSM in China.
Methods
This systematic review followed the guidelines of preferred reporting items for systematic reviews and meta-analyses published in PLoS Medicine (Checklist S1) [39].
Search strategy
Searched online databases included “Wanfang” (including more than 5700 Chinese journals issued since 1998), Chinese National Knowledge Infrastructure (CNKI, including more than 7500 Chinese journals issued since 1994), and PubMed up to September 2013. Searches of “Wanfang” and CNKI as Chinese databases focused on published articles. Searches were filtered by titles, abstracts and keywords in the two Chinese databases: (“gang jiao” or “gang men xing jiao” or “gang men xing xing wei”, meaning “anal sex”) and (“nan tong” or “tong zhi” or “nan nan xing xing wei” or “nan nan xing jie chu” or “tong xing lian” or “MSM”, meaning “male-to-male sex act”). The following terms combined were searched by all fields or by MeSH terms in PubMed database: (“anal sex” or “anal intercourse” or “condom use” or “risk behavior”) and (“homosexual” or “bisexual” or “gay” or “MSM” or “men who have sex with men” or “tongzhi”) and “China”. The relevant published articles were examined by hand for additional studies, but none fulfilled the study selection criteria.
Study selection
In this meta-analysis, UAI was defined as occurring with male partners and included both UIAI and URAI. Studies were included if they met all of the following criteria: conducted in mainland China; reported the prevalence of UAI or UIAI or URAI with male partners in the last six months; and reported the location of the study (names of provinces were provided), data collection time, and sample size. UAI information included the following: UAI or UIAI or URAI with male partners (e.g., any [of the following three types], regular, commercial, and casual; or non-regular including commercial and casual). Additional rules (see below) were applied to help data extraction. If multiple publications covered the same study, the most comprehensive article or the article providing more UAI information or the earliest published article (in order of decreasing priority) was selected. We contacted some authors to verify possible multiple publications of the same study. Only baseline information from cohort studies was used in this study. All UAI data were extracted from a given study if information on UAI prevalence by subgroups was available. Authors were contacted to clarify any questions related to UAI data, study design, and data representativeness.
Data extraction
The information from selected articles was extracted and entered into a Microsoft Excel 2010™ (Microsoft Corporation, Redmond, Washington, USA) by one reviewer and reviewed separately by another independent reviewer according to the selection criteria. A third independent reviewer reconciled the discrepancies. We extracted the following variables: first author, year of publication, data collection period, study location (including cities and provinces), publication language, sampling method, age (mean ± SD and/or median, range), sample source, study type, data collection method, HIV prevalence, recruitment settings (defined as the facilities where data were collected, e.g., entertainment venues, offices of Centers for Disease Control), UAI type, sample size, and the number of UAI events among MSM.
Quality Assessment
Quality assessment of the included studies was conducted based on EBMH guidelines for evaluating prevalence studies [40]. Eight items were scored as either 1 or 0, which corresponded to “yes” or “no”, and the total scores ranged from 0 to 8 (Checklist S2).
Statistical methods
All analyses were conducted using a Meta package of R software version 3.0.1 and 3.0.2 (R Foundation for Statistical Computing, Vienna, Austria). Logit transformation was applied to reduce the variances among UAI prevalence of MSM in individual studies. The inverse variance methods and random-effects models were used to determine the weight of each study. Pooled UAI prevalence with any male partner, with regular male partners, with non-regular male partners, with casual male partners, and with commercial male partners, as well as their 95% confidence intervals (95%CI), were reported. A cumulative meta-analysis was performed to trace the dynamics of annual UAI prevalence [41]. Sub-group analyses were conducted to find any differences between stratified variables, e.g., data collection period, region, sampling method, study type, data collection method, recruitment settings and HIV prevalence. Variables with a P-value ≤0.05 in sub-group analyses entered multivariate meta-regression analysis together, and a mixed-effects model was used. Heterogeneity was tested by Q statistics and quantified by I-square statistics. Publication bias was examined by a linear regression test to assess if funnel plots were symmetric (the threshold of P value is 0.05). In the sensitivity analyses, we compared the estimated UAI prevalence among MSM of k studies and UAI prevalence of k-1 studies to determine the robustness of the pooled prevalence. Here, k is the number of studies included in the meta-analyses.
Results
Characteristics of studies
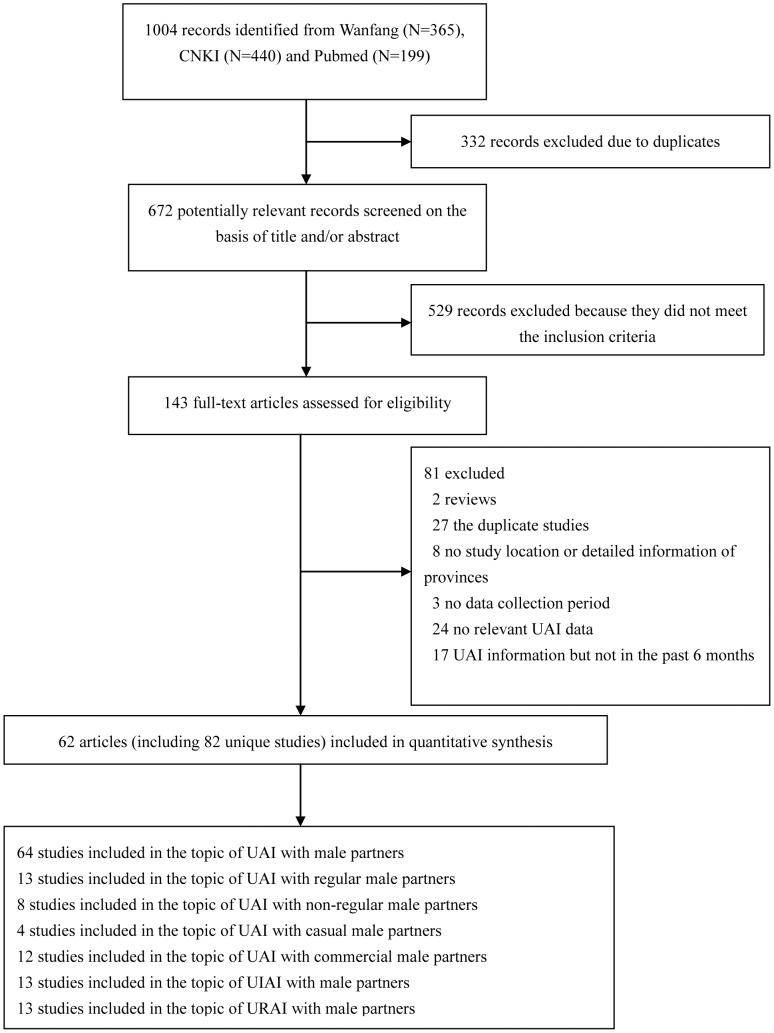
A total of 82 unique studies from 62 publications were selected and included in this meta-analysis (Figure 1). One [42] of the 62 selected publications presented five cross-sectional studies in different years, two publications presented four cross-sectional studies each (one in different cities [43], and one in different years [44]), three publications included three cross-sectional studies each in different years [45]–[47], and four publications included two cross-sectional studies each (one in different HIV infection status [48], two in different cities each [49], [50], and one in different years [51]). Each remaining publication presented one individual study. Table S1 presents a summary description of the 82 studies [42]–[103].
Figure 1. Flow Diagram of the Study Identification and Selection.
A total of 41203 MSM provided information on UAI in the 82 studies (31 studies in English and 51 in Chinese). Among the 82 studies, 23 were conducted from 2001 to 2007, 56 from 2008 to 2012, and another three across from 2007 to 2008 [49], [95]. The participants were recruited from MSM venue-based methods, either in conjunction with or exclusive of other methods, in about half of the studies (42/82). Sampling methods adopted included respondent driven sampling (RDS), snowball sampling, time-location-sampling method, and convenient sampling. The majority of the studies used cross-sectional study designs (72/82) and face-to-face interviews (58/82). These included 82 studies were conducted across 18 of 31 provinces, municipalities, and autonomous regions in China, and nearly three-quarters of the studies were conducted in Beijing, Chongqing, Heilongjiang, Jiangsu and Sichuan. About 80% (27/34) studies collected data in medical facilities among the 34 studies providing information on recruitment settings, while 48 studies failed to provide such information. The ages of participants in 38 studies ranged from 15 to 78 years, and the median mean age of 53 studies was 28.0 years (range: 20.2–36.3). The median HIV prevalence of 64 studies was 6.2% with a range of 0 to 31.6%. The scores of quality assessment ranged from 2 to 6, with a median of 4 in all included studies, and the results were similar to another meta-analysis [104]. The median scores for each item were 1, 0, 1, 0, 1, 0, 1, 0, respectively.
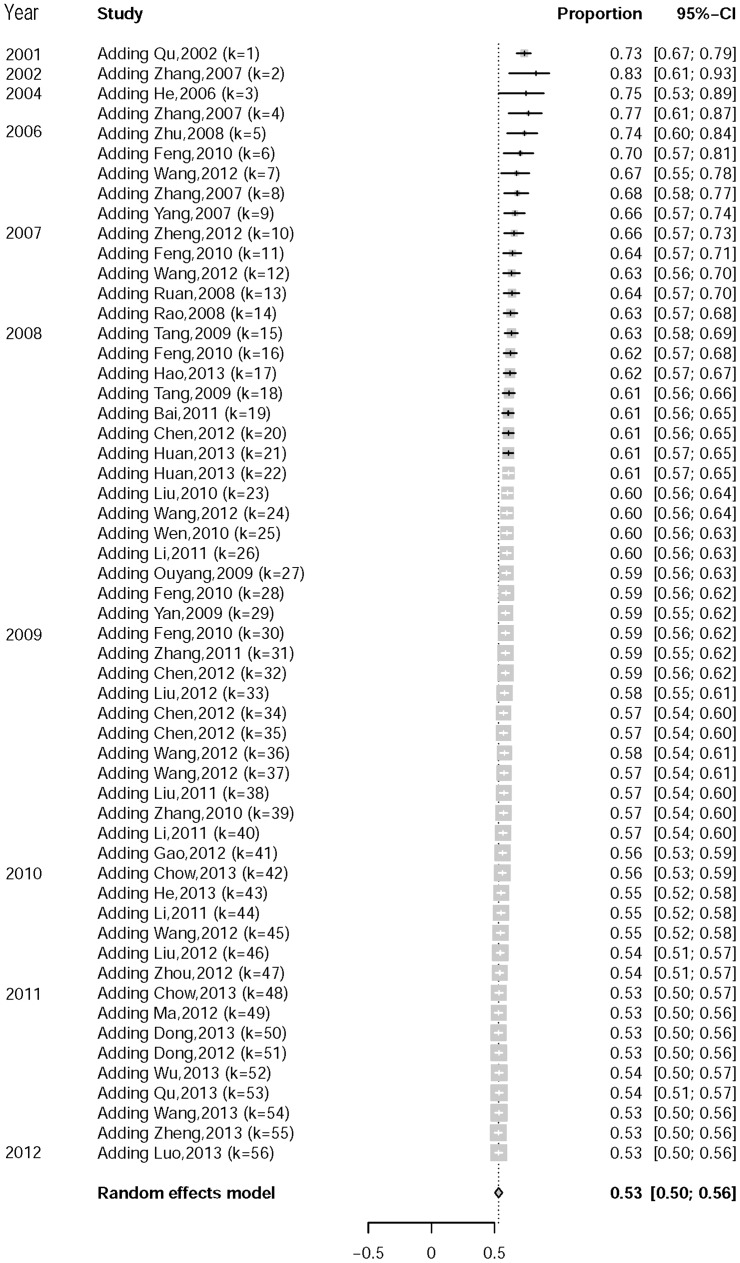
UAI prevalence estimates with male partners
Table 1 and Figures S1-S7 present the UAI prevalence with different types of sexual partners. The pooled UAI prevalence with any male partner (53%, 95%CI: 51–56%) was statistically higher than the UAI prevalence with non-regular (34%, 95%CI: 24–45%), casual (33%, 95%CI: 30–36%), or commercial (12%, 95%CI: 5–26%) male partners, and also higher than the prevalence of UIAI or URAI with any male partner (UIAI: 43%, 95%CI: 36–49%; URAI: 38%, 95%CI: 33–44%). The rates of UAI with different types of male partners ranked in the following descending order: regular male partners (45%, 95%CI: 39–51%), casual male partners, and commercial male partners. A cumulative meta-analysis showed a decreasing trend in prevalence over time (Figure 2). High heterogeneity was found in the overall UAI prevalence with any male partner (Q = 1,308, P<0.0001), with regular male partners (Q = 189, P<0.0001), with non-regular male partners (Q = 198, P<0.0001), with commercial male partners (Q = 634, P<0.0001), UIAI or URAI with any male partner (Q = 269, P<0.0001; Q = 243, P<0.0001). However, no obvious publication bias was observed in all of the above UAI prevalence rates (Table 1). Sensitivity analyses showed no obvious difference between k outcomes from k-1 studies and the outcome from k studies.
Table 1. The Pooled Prevalence of UAI with Male Partners.
| UAI type | No. of studies | Pooled sample size | Number of MSM with UAI | M (IQR) (%) | Pooled UAI prevalence and 95%CI (%) | P value of publication bias |
| UAI with any male partner | 64 | 31362 | 16263 | 53(13) | 53(51–56) | 0.09 |
| UAI with regular male partners | 13 | 4007 | 1665 | 43(10) | 45(39–51) | 0.12 |
| UAI with non-regular male partners | 8 | 2632 | 724 | 33(25) | 34(24–45) | 0.16 |
| UAI with casual male partners | 4 | 1132 | 373 | 32(2) | 33(30–36) | 0.47 |
| UAI with commercial male partners | 12 | 4340 | 389 | 5(40) | 12(5–26) | 0.55 |
| UIAI with any male partner | 13 | 5763 | 2383 | 43(13) | 43(36–49) | 0.31 |
| URAI with any male partner | 13 | 5763 | 2154 | 36(12) | 38(33–44) | 0.45 |
Note: M: median; IQR: inter quartile range.
Figure 2. Cumulative Meta-analysis of UAI with Male Partners among MSM in China.
Sub-group and meta-regression analyses to partially clarify the heterogeneity of UAI prevalence with any male partner
The sub-group analyses (Table 2) showed significant factors for the heterogeneity of UAI prevalence were data collection period, sampling method and HIV prevalence. However, the above variables explained only about 20% of the variance (R2 = 0.20) from the UAI prevalence of individual studies in multivariate meta-regression analysis (Table 3). The variable of data collection period significantly influenced UAI prevalence with any male partner.
Table 2. The Pooled UAI Prevalence with Any Male Partner, by Subgroups.
| Stratified variables | No. of studies | Pooled sample size | Number of MSM with UAI | Pooled UAI prevalence and 95%CI (%) | QB | P value |
| Data collection period | 15.74 | 0 | ||||
| 2001–2007 | 17 | 7909 | 4708 | 61(57–66) | ||
| 2008–2012 | 47 | 23453 | 11555 | 50(48–53) | ||
| Region† | 1.18 | 0.88 | ||||
| Northeast | 12 | 6217 | 3152 | 57(49–65) | ||
| North China | 5 | 3003 | 1592 | 55(47–62) | ||
| East China | 23 | 9567 | 4982 | 53(49–57) | ||
| Southwest | 15 | 7971 | 4365 | 53(48–57) | ||
| South central | 7 | 3604 | 1685 | 51(42–60) | ||
| Sampling method | 8.68 | 0 | ||||
| RDS | 10 | 3593 | 2166 | 61(56–67) | ||
| Other methods | 54 | 27769 | 14097 | 52(49–55) | ||
| Study type | 3.17 | 0.08 | ||||
| Cross-sectional study | 56 | 29053 | 14915 | 52(50–55) | ||
| Other types | 8 | 2309 | 1348 | 60(52–68) | ||
| Data collection method | 0.77 | 0.68 | ||||
| Interviewer | 50 | 25997 | 13496 | 53(50–56) | ||
| Self | 5 | 2418 | 1194 | 51(45–57) | ||
| both | 3 | 1157 | 565 | 50(43–57) | ||
| HIV prevalence | 5.8 | 0.02 | ||||
| ≤5% | 24 | 11776 | 6058 | 57(51–61) | ||
| >5% | 27 | 15898 | 8129 | 49(46–52) | ||
| Recruitment settings | 3.99 | 0.14 | ||||
| Medical facilities | 24 | 9764 | 4939 | 52(49–55) | ||
| MSM venues | 6 | 2909 | 1657 | 60(53–67) | ||
| No report | 34 | 18689 | 9667 | 53(49–57) |
: Region division referred the government website (http://www.xzqh.org.cn/ONEWS_zq.asp?id=6162). Two articles were excluded: one in Ningxia in the northwest region, and one in Guangdong and Sichuan across two regions.
Table 3. Multivariate Meta-regression Analysis of UAI Prevalence with Any Male Partner.
| Variables | β(95% CI) | Standard error | Z | P value |
| Data collection period (reference = 2008–2012) | 0.51(0.26–0.76) | 0.13 | 4.02 | 0 |
| Sampling method (reference = non-RDS) | 0.31(−0.04–0.65) | 0.18 | 1.74 | 0.08 |
| HIV prevalence (reference>5%) | −0.09(−0.32–0.14) | 0.12 | −0.75 | 0.45 |
Discussion
Our meta-analysis estimated UAI prevalence with different types of sexual partners and sexual positions among MSM (including both HIV infected and non-infected individuals) in China. The findings of UAI prevalence from this meta-analysis are robust based on the stable outcomes from the sensitivity analyses. The estimated UAI prevalence with any male partner among MSM in China was 53% (95%CI: 51–56%), which was significantly lower than that (75%; 95%CI: 67–82%) estimated among HIV-infected MSM in a China meta-analysis [105]. The pooled UAI prevalence with any male partner among MSM was 55% (95%CI: 52–58%) in 2008 and 50% (95%CI: 44–57%) in 2009 (data were not shown), which was similar to the 52% reported in the unprecedented nationwide survey targeting MSM in 61 metropolitan cities of China in 2008–2009 [38]. Furthermore, UAI prevalence with any male partner among MSM in China was comparable with that among MSM from the National HIV Behavioral Surveillance System (NHBS) across 21 U.S. cities in 2008 (54%) [25]. Studies [18], [106], [107] evidenced that UAI is an independent predictor associated with HIV and other STIs. The findings of this study reveal the considerable number of MSM practicing UAI with their male partners, which could be a major driving force for the rapid spread of HIV and other STIs among MSM in China.
This study showed a statistically decreasing trend in prevalence rates of UAI with regular male partners, with casual male partners and with commercial male partners. A similar decreasing trend was observed in other studies as well as in the two cycles' surveys of the NHBS System in U.S. [25]–[28]. These all showed that MSM decide upon risky or safe behaviors according to their perception of intimacy levels with male partners. The estimated UAI prevalence rates with regular male partners and with non-regular male partners (43% and 34%) were higher than those reported in NHBS in U.S. (37% and 25%) [25]. Condom use with a regular male partner is a complex topic because it may carry implications about mutual trust and stability in the monogamous relationship [29], [30]. Some factors such as the duration of the monogamous relationship and unprotected sex acts outside of the relationship may increase the potential transmission and spread of HIV and other STIs [30], [108]. The high risk of UAI with regular male partners contributes much to HIV epidemic [29], so encouraging positive social norms about condom use in MSM's mainstream contexts may have a positive intervention impact. This study found that 12% of MSM engaged in UAI with commercial male partners, which might be cautiously explained by the prevalence of sexual dysfunction; the prevalence of erectile dysfunction among MSM in China was about 10% [109]. Additionally, we need to investigate further the syndemic risk factors of the high UAI prevalence with casual male partners from individual, interpersonal and socio-cultural perspectives [110] so that interventions can be prioritized and tailored to the specific subgroups of MSM.
URAI is recognized as carrying a higher risk of acquiring HIV than UIAI [20], [22], [23], which is sometimes referred to as a “strategic position.” It is cautious to apply this strategy to control HIV epidemics despite its lower risk than URAI, since MSM with UIAI are proven to have a higher risk of HIV transmission than MSM without UAI [23]. HIV-negative MSM should protect themselves from HIV by adopting safer sex behaviors, rather than relying on the less risky but still dangerous strategy of UIAI.
A declining UAI prevalence with male partners among MSM in China over time was observed in this study, but the epidemics of HIV and other STIs remained rapidly expanding [5]–[8]. An inverse correlation between UAI prevalence and HIV prevalence has been also reported in five consecutive cross-sectional studies in Harbin, a provincial capital of Heilongjiang, China [42]. However, a previous Chinese meta-analysis [36] did not find the inverse correlation between UAI prevalence and HIV/syphilis prevalence. Our meta-analysis and other HIV/STIs meta-analyses [5]–[8] among MSM in China retrieved and included more studies than the previous meta-analysis [36]. Our meta-analysis included studies conducted over a longer interval from 2001 to 2012, similar to a U.S. meta-analysis [24]. However, the previous meta-analysis [36] showed that the included studies were conducted from 2003 to 2007. Our meta-analysis included studies beyond 2008, which was a critical year when more attention began to be paid to MSM [37], [38]. In addition, we performed more thorough analyses to understand UAI characteristics in China, such as cumulative meta-analysis, meta-regression, and subgroup analyses. In conclusion, the outcomes from our meta-analysis may be more convincing.
The inverse relationship between UAI prevalence and HIV/STIs prevalence may be attributed to several reasons. Outcomes from mathematical model studies [111]–[114] suggest that it requires more than 80 percent coverage in condom use to curb HIV epidemic. HIV transmission probability is a sensitive factor influencing HIV epidemic [115], [116], and higher transmission risk through anal rather than vaginal sex [117], [118] also intensifies HIV transmission among MSM. In addition, high HIV prevalence may be attributed to unprotected group sex [76], [119]; the prevalence of group sex among MSM in China ranged from 11% to 38% [100], [120]. Obviously a higher prevalence of group sex predicts a higher risk of UAI among MSM [121]. The decreasing UAI prevalence over time shows that intervention efforts among MSM in China are effective to some degree. However, the highly prevalent rate of UAI concurrent with a high prevalence of HIV-infected partners in sexual networks fuels the rapid spread of HIV. Therefore, China should develop more effective and better targeted interventions among MSM in a sustainable way to contain HIV spreading. Decreasing UAI exposure is an important goal that can be addressed by providing condoms, behavior change and communication.
Only 20% of the variance from UAI prevalence of individual studies can be explained by data collection period, sampling method and HIV prevalence in this meta-analysis, and more variables are needed to explain the heterogeneity. Though the study did not find a difference in UAI across different regions, UAI prevalence showed high diversity across cities (Q = 12, P = 0.03, Figure S8). HIV status consistent with UAI is also an important factor in explaining the heterogeneity of UAI prevalence among MSM. Future epidemiologic surveys should address the in-depth correlations between interventions and HIV prevalence of MSM and provide intermediate evidence of HIV spread in China. The high heterogeneity across the individual studies incorporated in this meta-analysis was not unique; it was also found in other meta-analyses of MSM in China [5]–[7], [36], [105]. High heterogeneity may result from variations in the study locations, data collection time and sampling methods. Prior China- and U.S.-based UAI meta-analyses showed similar high heterogeneity (P<0.0001) [24], [36], [105]. It seems that heterogeneity is unavoidable in MSM studies based on non-probability sampling and participants' recruitment strategies.
We recognized the limitations of this meta-analysis. First, the research studies were usually reported and conducted in severely endemic areas, which could lead to a potential overestimation of the prevalence of UAI. Second, this study did not differentiate between the rates of UAI among HIV infected and non-infected groups. Serosorting and strategic positioning [23], [30], [122]–[124] were also not explored in this study.
In summary, the findings of this meta-analysis revealed a high prevalence of UAI with male partners and a decreasing trend among MSM in China. The declining rates of UAI among MSM in China suggest that preventive intervention efforts in recent years may slow the increasing rate in HIV prevalence and incidence, but are not enough to control HIV spreading. These interventions include condom promotion, peer education, media-based education and counseling, and HIV testing and counseling [125], [126], which are all independently associated with lower UAI prevalence [97]. In addition, the following factors may lead to a higher risk of UAI: a reluctance to use condoms, multiple partners, and alcohol and/or substance use before sex [107]. However, the continuously high rate of UAI underscores the need for innovative and effective prevention intervention strategies among MSM in China.
Supporting Information
Forest plot of UAI prevalence with any male partner among MSM in China.
(TIF)
Forest plot of UAI prevalence with regular male partners among MSM in China.
(TIF)
Forest plot of UAI prevalence with non-regular male partners among MSM in China.
(TIF)
Forest plot of UAI prevalence with casual male partners among MSM in China.
(TIF)
Forest plot of UAI prevalence with commercial male partners among MSM in China.
(TIF)
Forest plot of UIAI prevalence with any male partner among MSM in China.
(TIF)
Forest plot of URAI prevalence with any male partner among MSM in China.
(TIF)
Subgroups analysis of UAI prevalence with any male partner among MSM in different cities of China.
(TIF)
PRISMA Checklist.
(DOC)
Quality assessment of included individual studies.
(DOC)
Characteristics of studies included in this meta-analysis.
(DOCX)
Acknowledgments
We appreciate the efforts of all the researchers whose articles were included in this study. We also appreciate Jessie Norris's revision work on this manuscript.
Funding Statement
This study is supported by the National Megaprojects of Science Research for the 12th Five-Year Plan (2012ZX10001-001). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Ministry of Health of China, UNAIDS, WHO (2006) 2005 HIV/AIDS Epidemic and work pregress of prevention and control in China. Beijing, China.
- 2.Ministry of Health of China, UNAIDS, WHO (2010) 2009 Estimates for the HIV/AIDS Epidemic in China. Beijing, China.
- 3.Ministry of Health of China, UNAIDS, WHO (2011) 2011 Estimates for the HIV/AIDS Epidemic in China. Beijing, China.
- 4.State council AIDS working committee office, UN theme group on AIDS in China (2007) A joint assessment of HIV/AIDS prevention, treatment and care in China (2007). Beijing, China.
- 5. Chow EP, Wilson DP, Zhang J, Jing J, Zhang L (2011) Human immunodeficiency virus prevalence is increasing among men who have sex with men in China: findings from a review and meta-analysis. Sex Transm Dis 38: 845–857. [DOI] [PubMed] [Google Scholar]
- 6. Chow EP, Wilson DP, Zhang L (2011) HIV and syphilis co-infection increasing among men who have sex with men in China: a systematic review and meta-analysis. PLoS One 6: e22768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Meng X, Zou H, Beck J, Xu Y, Zhang X, et al. (2013) Trends in HIV prevalence among men who have sex with men in China 2003-09: a systematic review and meta-analysis. Sex Health 10: 211–219. [DOI] [PubMed] [Google Scholar]
- 8. Zhang L, Chow EP, Jing J, Zhuang X, Li X, et al. (2013) HIV prevalence in China: integration of surveillance data and a systematic review. The Lancet Infectious Diseases 13: 955–963. [DOI] [PubMed] [Google Scholar]
- 9. Wang L, Wang L, Jessie LN, Li DM, Guo W, et al. (2012) HIV prevalence and influencing factors analysis of sentinel surveillance among men who have sex with men in China. Chinese Medical Journal 125: 1857–1861. [PubMed] [Google Scholar]
- 10. Chow EPF, Wilson DP, Zhang L (2010) The next era of HIV in China: rapidly spreading epidemics among men who have sex with men. Journal of Acquired Immune Deficiency Syndromes 55: e32–e34. [DOI] [PubMed] [Google Scholar]
- 11. Wong FY, Huang ZJ, Wang W, He N, Marzzurco J, et al. (2009) STIs and HIV among men having sex with men in China: a ticking time bomb? AIDS Education & Prevention 21: 430–446. [DOI] [PubMed] [Google Scholar]
- 12. de Lind van Wijngaarden JW, Brown T, Girault P, Sarkar S, van Griensven F (2009) The epidemiology of human immunodeficiency virus infection, sexually transmitted infections, and associated risk behaviors among men who have sex with men in the Mekong Subregion and China: implications for policy and programming. Sex Transm Dis 36: 319–324. [DOI] [PubMed] [Google Scholar]
- 13. Tucker JD, Yin YP, Wang B, Chen XS, Cohen MS (2011) An expanding syphilis epidemic in China: epidemiology, behavioural risk and control strategies with a focus on low-tier female sex workers and men who have sex with men. Sex Transm Infect 87 Suppl 2ii16–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. van Griensven F, van Wijngaarden JWdL (2010) A review of the epidemiology of HIV infection and prevention responses among MSM in Asia. AIDS 24: S30–S40. [DOI] [PubMed] [Google Scholar]
- 15. Baral S, Sifakis F, Cleghorn F, Beyrer C (2007) Elevated risk for HIV infection among men who have sex with men in low-and middle-income countries 2000–2006: a systematic review. PLoS Medicine 4: e339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhong F, Lin P, Xu H, Wang Y, Wang M, et al. (2011) Possible increase in HIV and syphilis prevalence among men who have sex with men in Guangzhou, China: results from a respondent-driven sampling survey. AIDS Behav 15: 1058–1066. [DOI] [PubMed] [Google Scholar]
- 17. Zablotska IB, Prestage G, Middleton M, Wilson D, Grulich AE (2010) Contemporary HIV diagnoses trends in Australia can be predicted by trends in unprotected anal intercourse among gay men. AIDS 24: 1955–1958. [DOI] [PubMed] [Google Scholar]
- 18. Hirshfield S, Remien RH, Walavalkar I, Chiasson MA (2004) Crystal methamphetamine use predicts incident STD infection among men who have sex with men recruited online: a nested case-control study. Journal of Medical Internet Research 6: e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Li HM, Peng RR, Li J, Yin YP, Wang B, et al. (2011) HIV incidence among men who have sex with men in China: a meta-analysis of published studies. PLoS One 6: e23431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Berry M, Wirtz AL, Janayeva A, Ragoza V, Terlikbayeva A, et al. (2012) Risk factors for HIV and unprotected anal intercourse among men who have sex with men (MSM) in Almaty, Kazakhstan. PloS One 7: e43071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Vu L, Andrinopoulos K, Tun W, Adebajo S (2013) High levels of unprotected anal intercourse and never testing for HIV among men who have sex with men in Nigeria: evidence from a cross-sectional survey for the need for innovative approaches to HIV prevention. Sex Transm Infect 89: 659–665. [DOI] [PubMed] [Google Scholar]
- 22. Koblin BA, Husnik MJ, Colfax G, Huang Y, Madison M, et al. (2006) Risk factors for HIV infection among men who have sex with men. AIDS 20: 731–739. [DOI] [PubMed] [Google Scholar]
- 23. Jin F, Crawford J, Prestage GP, Zablotska I, Imrie J, et al. (2009) Unprotected anal intercourse, risk reduction behaviours, and subsequent HIV infection in a cohort of homosexual men. AIDS 23: 243–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Crepaz N, Marks G, Liau A, Mullins MM, Aupont LW, et al. (2009) Prevalence of unprotected anal intercourse among HIV-diagnosed MSM in the United States: a meta-analysis. AIDS 23: 1617–1629. [DOI] [PubMed] [Google Scholar]
- 25. Finlayson TJ, Le B, Smith A, Bowles K, Cribbin M, et al. (2011) HIV risk, prevention, and testing behaviors among men who have sex with men—National HIV Behavioral Surveillance System, 21 US cities, United States, 2008. MMWR 60: 1–34. [PubMed] [Google Scholar]
- 26. Li X, Shi W, Li D, Ruan Y, Jia Y, et al. (2008) Predictors of unprotected sex among men who have sex with men in Beijing, China. Southeast Asian J Trop Med Public Health 39: 99–108. [PMC free article] [PubMed] [Google Scholar]
- 27. Lim SH, Bazazi AR, Sim C, Choo M, Altice FL, et al. (2013) High rates of unprotected anal intercourse with regular and casual partners and associated risk factors in a sample of ethnic Malay men who have sex with men (MSM) in Penang, Malaysia. Sex Transm Infect 89: 642–649. [DOI] [PubMed] [Google Scholar]
- 28. Sanchez T, Finlayson T, Drake A, Behel S, Cribbin M, et al. (2006) Human immunodeficiency virus (HIV) risk, prevention, and testing behaviors—United States, National HIV Behavioral Suveillance System: men who have sex men, November 2003—April 2005. MMWR 55: 1–16. [PubMed] [Google Scholar]
- 29. Blais M (2006) Vulnerability to HIV among regular male partners and the social coding of intimacy in modern societies. Culture, Health & Sexuality 8: 31–44. [DOI] [PubMed] [Google Scholar]
- 30. Suarez T, Miller J (2001) Negotiating risks in context: A perspective on unprotected anal intercourse and barebacking among men who have sex with men—where do we go from here? Archives of Sexual Behavior 30: 287–300. [DOI] [PubMed] [Google Scholar]
- 31. Bezemer D, de Wolf F, Boerlijst MC, van Sighem A, Hollingsworth TD, et al. (2010) 27 years of the HIV epidemic amongst men having sex with men in the Netherlands: an in depth mathematical model-based analysis. Epidemics 2: 66–79. [DOI] [PubMed] [Google Scholar]
- 32. Bezemer D, de Wolf F, Boerlijst MC, van Sighem A, Hollingsworth TD, et al. (2008) A resurgent HIV-1 epidemic among men who have sex with men in the era of potent antiretroviral therapy. AIDS 22: 1071–1077. [DOI] [PubMed] [Google Scholar]
- 33. Amundsen E, Stigum H, Rottingen J, Aalen O (2004) Definition and estimation of an actual reproduction number describing past infectious disease transmission: application to HIV epidemics among homosexual men in Denmark, Norway and Sweden. Epidemiology and Infection 132: 1139–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Clements MS, Prestage G, Grulich A, Van de Ven P, Kippax S, et al. (2004) Modeling trends in HIV incidence among homosexual men in Australia 1995–2006. JAIDS 35: 401–406. [DOI] [PubMed] [Google Scholar]
- 35. van Sighem A, Jansen I, Bezemer D, De Wolf F, Prins M, et al. (2012) Increasing sexual risk behaviour among Dutch men who have sex with men: mathematical models versus prospective cohort data. AIDS 26: 1840–1843. [DOI] [PubMed] [Google Scholar]
- 36. He Q, Xia Y, Raymond HF, Peng R, Yang F, et al. (2011) HIV trends and related risk factors among men having sex with men in mainland China: findings from a systematic literature review. Southeast Asian J Trop Med Public Health 42: 616–633. [PubMed] [Google Scholar]
- 37. Wu ZY, Sullivan SG, Wang Y, Rotheram-Borus MJ, Detels R (2007) Evolution of China's response to HIV/AIDS. The Lancet 369: 679–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wu Z, Xu J, Liu E, Mao Y, Xiao Y, et al. (2013) HIV and syphilis prevalence among men who have sex with men: a cross-sectional survey of 61 cities in China. Clinical Infectious Diseases 57: 298–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Plos Medicine 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Boyle MH (1998) Guidelines for evaluating prevalence studies. Evidence Based Mental Health 1: 37–39. [Google Scholar]
- 41. Jüni P, Nartey L, Reichenbach S, Sterchi R, Dieppe PA, et al. (2004) Risk of cardiovascular events and rofecoxib: cumulative meta-analysis. The Lancet 364: 2021–2029. [DOI] [PubMed] [Google Scholar]
- 42. Wang K, Yan H, Liu Y, Leng Z, Wang B, et al. (2012) Increasing prevalence of HIV and syphilis but decreasing rate of self-reported unprotected anal intercourse among men who had sex with men in Harbin, China: results of five consecutive surveys from 2006 to 2010. Int J Epidemiol 41: 423–432. [DOI] [PubMed] [Google Scholar]
- 43. Xu J, Han DL, Liu Z, Ma XY, Wang LL, et al. (2010) The prevalence of HIV infection and the risk factors among MSM in 4 cities, China. Chin J Prev Med 44: 975–980. [PubMed] [Google Scholar]
- 44. Feng LG, Ding XB, Lu RR, Xu SM, Guo XJ, et al. (2010) Trend on prevalence of HIV and syphilis and estimated HIV incidence among young male students who have sex with men. Acta Academiae Medicinae Militaris Tertiate 32: 2644–2646. [Google Scholar]
- 45. Li JJ, Huan XP, Yan HJ, Zhang M, Tang WM, et al. (2011) Effectiveness of behavioral intervention combined with voluntary counseling and testing on high risk behaviors among MSM. Chin Prev Med 12: 666–669. [Google Scholar]
- 46. Xu J, He J, Feng LG, Ding XB, Xu SM, et al. (2011) Prevalence of HIV and syphilis and its risk behavior among money boys in Chongqing (2006–2008). J Trop Med 11: 1199–1202. [Google Scholar]
- 47. Zhang D, Bi P, Lv F, Zhang J, Hiller JE (2007) Changes in HIV prevalence and sexual behavior among men who have sex with men in a northern Chinese city: 2002–2006. J Infect 55: 456–463. [DOI] [PubMed] [Google Scholar]
- 48. Tang WM, Yan HJ, Liu XY, Wang N, Zhang M, et al. (2009) Factors associated with HIV infection among men who have sex with men in Nanjing, Suzhou and Yangzhou: a 1:4 matched case-control study. Chin J Epidemiol 30: 448–451. [PubMed] [Google Scholar]
- 49. Duan Y, Zhang H, Wang J, Wei S, Yu F, et al. (2013) Community-based peer intervention to reduce HIV risk among men who have sex with men in Sichuan province, China. AIDS Educ Prev 25: 38–48. [DOI] [PubMed] [Google Scholar]
- 50. Chen X, Zhu YY, Huan XP, Wang Q, Zheng H, et al. (2012) Comparison of HIV/AIDS prevalence among men who have sex with men between Suzhou and Yangzhou city. Chin J Public Health 28: 1549–1552. [Google Scholar]
- 51. Chow EP, Chen L, Jing J, Gao L, Zhang J, et al. (2013) HIV disease burden and related risk behaviours among men who have sex with men in Yuxi Prefecture, Yunnan Province, China: 2010-2011. AIDS Behav 17: 2387–2394. [DOI] [PubMed] [Google Scholar]
- 52. Chen AD, Zhong F, Fan LR, Wen F, Cheng WB, et al. (2012) Unprotected anal intercourse and related factors among men who have sex with men in Guangzhou City. South China J Prev Med 38: 1–6. [Google Scholar]
- 53. Cheng WB, Zhong F, Wen F, Gao K, Liu JW, et al. (2010) Investigation of HIV and syphilis infection and AIDS-related behaviors among money boys, in Guangzhou, China. Chin J Prev Med 44: 1027–1031. [PubMed] [Google Scholar]
- 54. Cheng WB, Zhong F, Wen F, Xu HF (2012) Effects on AIDS-related knowledge and attitudes on high risk sexual behavior among men who have sex with men. Chin J Dis Control Prev 16: 1064–1067. [Google Scholar]
- 55. Dong XF, Lei J, Miao ZF, Han X, Yang ZG, et al. (2013) A research of the influencing factors of AIDS high-risky behavior among 400 MSM. Journal of Ningxia Medical University 35: 277–279. [Google Scholar]
- 56. Dong ZQ, Jin MH, Qiu ZH, Yang ZR, Zhang SC, et al. (2012) Survey of AIDS related knowledge awareness and high-risk behavior in 410 men who have sex with men in Huzhou,Zhejiang. Disease Surveillance 27: 623–626. [Google Scholar]
- 57. Feng LG, Ding XB, Xu J, Ouyang L, Xu SM, et al. (2010) Study on HIV syphilis and HCV prevalence and its associated factors among internet MSM comparison to non-internet MSM in Chongqing. J Trop Med 10: 78–82. [Google Scholar]
- 58. Gao YJ, Yu MR, Li SM, Zhang Z, Li DL, et al. (2012) Prevalence and predictors of HIV, syphilis and herpes simplex type 2 virus (HSV-2) infections among the men who have sex with men (MSM) in Beijing. Chin J Public Health 28: 451–453. [Google Scholar]
- 59. He H, Wang M, Zhang HB, Song DD, She M, et al. (2012) The unprotected sexal behaviors and its influencing factors among HIV-infected men who have sex with men in Shanghai, China. Chin J Prev Med 46: 976–981. [PubMed] [Google Scholar]
- 60. Li CM, Jia YJ, Liu JB, Ding XB, Xiao Y (2011) Prevalence and predictors of unprotected anal sex among men who have sex with men in Chongqing municipality, China. Chin J Public Health 27: 351–352. [Google Scholar]
- 61. Liu PL, Yao ZZ, Shi WD, Ding J, Li SL, et al. (2010) Epidemiological study on the status of HIV/STD among MSM in Wuhan City. Chin J Dis Control Prev 14: 917–919. [Google Scholar]
- 62. Liu XX, Zhang MH, Chen X, Zhu YY, Zhu Q, et al. (2012) Analysis on the seroconversion of HIV/syphilis and the predictors of cohort retention among men who have sex with men in Zhenjiang, a prospective cohort study. Chin J Dis Control Prev 16: 1024–1027. [Google Scholar]
- 63. Liu ZY, Wu GH, Xu J, Ding XB, Mi GD, et al. (2011) Factors associated with cohort retention among men who have sex with men. Chin J AIDS STD 17: 646–650. [Google Scholar]
- 64.Luo Y, Bao QG, Zhang XH (2013) Survey on the AIDS-related high risk behaviors and associated factors of men who have sex with men in Huainan city. Anhui J Prev Med 19: : 83–86, 93. [Google Scholar]
- 65. Ma GY, Li KC, Chen HY, Chen J, Xu PP (2012) Investigation of HIV, syphilis and HCV infection and sexual behavioral characteristics among MSM in Ningbo City. Anhui J Prev Med 18: 332–335. [Google Scholar]
- 66. Ma XY, Zhang QY, He X, Zhao JK, Li Y, et al. (2007) Epidemiological study on the status of HIV/STD and relative behaviors among MSM in Beijing. Chin J Epidemiol 28: 851–855. [PubMed] [Google Scholar]
- 67. Ma XY, Zhang QY, Zhao JK, He X, Du H, et al. (2007) Feasibility of using respondent driven sampling in HIV/STD epidemiological survey among MSM. Chin J AIDS STD 13: 311–313. [Google Scholar]
- 68. Ouyang L, Feng LG, Ding XB, Zhao JK, Xu J, et al. (2009) A respondent-driven sampling survey on HIV and risk factors among men who have sex with men in Chongqing. Chin J Epidemiol 30: 1001–1004. [PubMed] [Google Scholar]
- 69. Qu L, Gao YM, Qing H, Yang JY, Tao B (2013) Study on HIV infection and behavior among MSM in different venues. Practical Preventive Medicine 20: 145–149. [Google Scholar]
- 70.Qu SQ, Zhang DP, Wu YH, Zhu H, Cui Y, et al. (2002) A survey of knowledgy, attitude and practice related to HIV/AIDS among men who have sex with men in a northeastern city of China. Chin J AIDS STD 8: 338–340, 370.
- 71. Rao XM, Xiong HY, Ding XB, Feng LG (2008) Study on status of unprotected anal sex and its associated factors among men who have sex with men in Chongqing. Chongqing Medicine 37: 2335–2337. [Google Scholar]
- 72. Wang Y, Li LL, Fan J, Zhao XH, Yang XL, et al. (2013) Analysis on relationship of drug use behavior and HIV infection and related behaviors among men who have sex with men. Chin J Behav Med & Brain Sci 22: 364–366. [Google Scholar]
- 73. Wang Y, Li LL, Zhang GG, Fan J, Zhao XH, et al. (2013) Research on the network activities of MSM and characteristics of the related social behavior of the network sexual partners. Practical Preventive Medicine 20: 260–263. [Google Scholar]
- 74. Wang Y, Xu J, Li ZJ, Zhang GG, Li LL, et al. (2012) Analysis of HIV/syphilis infection among MSM seeking sex partners in different venues and related behavioral features. Chin J AIDS STD 18: 180–183. [Google Scholar]
- 75. Wen F, Zhong F, Cheng WB, Gao K, Luo BL, et al. (2010) HIV and current syphilis prevalence and related factors among men who have sex with men in Guangzhou. South China J Prev Med 36: 19–23. [Google Scholar]
- 76. Wu D, Chen SH, Yang J, Yu MH, Gao YJ, et al. (2013) HIV prevalence and associated factors among gay bathhouse attendees in China. Chin J AIDS STD 19: 127–130. [Google Scholar]
- 77. Yan HJ, Zhang M, Li JJ, Guan WH, Hu HY, et al. (2010) Prevelence of sexually transmitted infections and the behavior characteristics of men who have sex with men in Jiangsu Province. Chin Prev Med 11: 1249–1252. [Google Scholar]
- 78. Yan HM, Wang KL, Zhao DH, Hui S, Luo GL, et al. (2009) An analysis of HIV/AIDS related high-risk behavior, infection status and impact factors among MSM in Heilongjiang Province. Chin J AIDS STD 15: 288–291. [Google Scholar]
- 79. Yang X, Yi D, Ding XB (2007) High risk behaviors of HIV/AIDS in male-to-male sex and its influencing factors in 1000 men in a city. Acad J Sec Mil Med Univ 28: 1223–1228. [Google Scholar]
- 80. Zhang DD, Zhang Y, Li HL, Wang JX, Zhang Z, et al. (2010) Investigation of HIV, syphilis and HCV infection and sexual behavioral characteristics among MSM in Ningbo City. Zhejiang Preventive Medicine 22: 1–3. [Google Scholar]
- 81. Zhang QP, Ding XB, Feng LG, Xu J, Lu RR, et al. (2011) The prevalence of HIV and syphilis and its influencing factors among male sex workers. ACTA Academiae Medicinae Militaris Tertiate 33: 318–321. [Google Scholar]
- 82. Zheng WB, Zhu QY, Lan GH, Zhu JH, Dong BQ (2013) Efficacy of AIDS intervention service among MSM in Guangxi and its influential factors. China Tropical Medicine 13: 175–179. [Google Scholar]
- 83. Zhou JL, Zhang Y, Shi JP, Wang L (2012) Knowledge and behavior about HIV/AIDS and HIV infection among MSM in Liaoning province. Chin J Public Health 28: 806–808. [Google Scholar]
- 84. Zhu JL, Zhang HB, Zheng YZ, Choi KH, Zhu YB (2008) Association between HIV-risk behaviors of young men who have sex with men and characteristics of their core social networks. Chin J Public Health 24: 400–402. [Google Scholar]
- 85. Bai H, Huan X, Tang W, Chen X, Yan H, et al. (2011) A survey of HIV infection and related high-risk factors among men who have sex with men in Suzhou, Jiangsu, China. J Biomed Res 25: 17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Choi KH, Gibson DR, Han L, Guo Y (2004) High levels of unprotected sex with men and women among men who have sex with men: a potential bridge of HIV transmission in Beijing, China. AIDS Educ Prev 16: 19–30. [DOI] [PubMed] [Google Scholar]
- 87. Choi KH, Ning Z, Gregorich SE, Pan QC (2007) The influence of social and sexual networks in the spread of HIV and syphilis among men who have sex with men in Shanghai, China. J Acquir Immune Defic Syndr 45: 77–84. [DOI] [PubMed] [Google Scholar]
- 88. Fan S, Lu H, Ma X, Sun Y, He X, et al. (2012) Behavioral and serologic survey of men who have sex with men in Beijing, China: implication for HIV intervention. AIDS Patient Care STDs 26: 148–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Hao C, Huan X, Yan H, Yang H, Guan W, et al. (2012) A randomized controlled trial to evaluate the relative efficacy of enhanced versus standard voluntary counseling and testing on promoting condom use among men who have sex with men in China. AIDS Behav 16: 1138–1147. [DOI] [PubMed] [Google Scholar]
- 90. Hao C, Lau JT, Zhao X, Yang H, Huan X, et al. (2014) Associations between perceived characteristics of the peer social network involving significant others and risk of HIV transmission among men who have sex with men in China. AIDS Behav 18: 99–110. [DOI] [PubMed] [Google Scholar]
- 91. He Q, Wang Y, Lin P, Liu Y, Yang F, et al. (2006) Potential bridges for HIV infection to men who have sex with men in Guangzhou, China. AIDS Behav 10: S17–23. [DOI] [PubMed] [Google Scholar]
- 92. Hu Y, Qian HZ, Sun J, Gao L, Yin L, et al. (2013) Anal human papillomavirus infection among HIV-infected and uninfected men who have sex with men in Beijing, China. J Acquir Immune Defic Syndr 64: 103–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Huan X, Hao C, Yan H, Guan W, Xu X, et al. (2013) High prevalence of HIV and syphilis among men who have sex with men recruited by respondent-driven Sampling in a city in eastern China. Asia Pac J Public Health [Epub ahead of print]. [DOI] [PubMed]
- 94. Huan X, Tang W, Babu GR, Li J, Zhang M, et al. (2013) HIV risk-reduction counseling and testing on behavior change of MSM. PLoS One 8: e69740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Lau JT, Cai W, Tsui HY, Chen L, Cheng J, et al. (2012) Unprotected anal intercourse behavior and intention among male sex workers in Shenzhen serving cross-boundary male clients coming from Hong Kong, China - prevalence and associated factors. AIDS Care 24: 59–70. [DOI] [PubMed] [Google Scholar]
- 96. Lau JT, Wang M, Wong HN, Tsui HY, Jia M, et al. (2008) Prevalence of bisexual behaviors among men who have sex with men (MSM) in China and associations between condom use in MSM and heterosexual behaviors. Sex Transm Dis 35: 406–413. [DOI] [PubMed] [Google Scholar]
- 97. Liu J, Qu B, Ezeakile MC, Zhang Y (2012) Factors associated with unprotected anal intercourse among men who have sex with men in Liaoning Province, China. PLoS One 7: e50493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Ruan S, Yang H, Zhu Y, Ma Y, Li J, et al. (2008) HIV prevalence and correlates of unprotected anal intercourse among men who have sex with men, Jinan, China. AIDS Behav 12: 469–475. [DOI] [PubMed] [Google Scholar]
- 99. Song D, Zhang H, Wang J, Liu Q, Wang X, et al. (2013) Prevalence and correlates of HIV infection and unrecognized HIV status among men who have sex with men and women in Chengdu and Guangzhou, China. AIDS Behav 17: 2395–2404. [DOI] [PubMed] [Google Scholar]
- 100. Wang Z, Lau JT, Hao C, Yang H, Huan X, et al. (2013) Syphilis-related perceptions not associated with risk behaviors among men who have sex with men having regular male sex partner(s) in Nanjing, China. AIDS Care 25: 1010–1017. [DOI] [PubMed] [Google Scholar]
- 101. Xu JJ, Zhang M, Brown K, Reilly K, Wang H, et al. (2010) Syphilis and HIV seroconversion among a 12-month prospective cohort of men who have sex with men in Shenyang, China. Sex Transm Dis 37: 432–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhao J, Chen L, Cai WD, Tan JG, Tan W, et al. (2013) HIV infection and sexual behaviors among non-commercial men who have sex with men at different venues. Arch Sex Behav [Epub ahead of print]. [DOI] [PubMed]
- 103. Zheng J, Wu Z, Poundstone KE, Pang L, Rou K (2012) HIV, syphilis infection, and risky sexual behaviors among male university students who have sex with men in Beijing, China: a cross-sectional study. AIDS Educ Prev 24: 78–88. [DOI] [PubMed] [Google Scholar]
- 104. Chow EP, Iu KI, Fu X, Wilson DP, Zhang L (2012) HIV and sexually transmissible infections among money boys in China: A data synthesis and mta-analysis. PloS One 7: e48025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. He Q, Peng W-J, Zhang J-Q, Wang B-X, Wang J (2012) Prevalence of unprotected anal intercourse and unprotected vaginal intercourse among HIV-positive men who have sex with men in China: a meta-analysis. Sex Transm Infect 88: 229–233. [DOI] [PubMed] [Google Scholar]
- 106. Ruan Y, Li D, Li X, Qian H-z, Shi W, et al. (2007) Relationship between syphilis and HIV infections among men who have sex with men in Beijing, China. Sex Transm Dis 34: 592–597. [DOI] [PubMed] [Google Scholar]
- 107. Tang W, Huan X, Mahapatra T, Tang S, Li J, et al. (2013) Factors associated with unprotected anal intercourse among men who have sex with men: results from a respondent driven sampling survey in Nanjing, China, 2008. AIDS Behav 17: 1415–1422. [DOI] [PubMed] [Google Scholar]
- 108. Grov C, Rendina HJ, Ventuneac A, Parsons JT (2013) HIV risk in group sexual encounters: an event-level analysis from a National Online Survey of MSM in the U.S.. The Journal of Sexual Medicine 10: 2285–2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Tsui HY, Lau JT, Feng T, Hong F, Cai Y, et al. (2014) Sexual dysfunction and unprotected anal intercourse among men who have sex with men in two Chinese cities. Journal of Sex & Marital Therapy 40: 139–148. [DOI] [PubMed] [Google Scholar]
- 110.Wim VB, Christiana N, Marie L (2013) Syndemic and other risk factors for unprotected anal intercourse among an online sample of Belgian HIV negative men who have sex with men. AIDS and Behavior: 1–9. [DOI] [PubMed]
- 111. Brown T, Peerapatanapokin W (2004) The Asian Epidemic Model: a process model for exploring HIV policy and programme alternatives in Asia. Sex Transm Infect 80: i19–i24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Liu L, Luan R, Yang W, Zhang L, Zhang J, et al. (2009) Projecting dynamic trends for HIV/AIDS in a highly endemic area of China: estimation models for Liangshan Prefecture, Sichuan Province. Current HIV Research 7: 390–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Fang C, Chang Y, Wang J (2005) Higher-than-85% condom use rate in persons with multiple sexual partners is required to control HIV [letter]. Sex Transm Infect [serial on the Internet].
- 114. Lou J, Wu J, Chen L, Ruan Y, Shao Y (2009) A sex-role-preference model for HIV transmission among men who have sex with men in China. BMC Public Health 9 Suppl 1S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Sun X, Xiao Y, Peng Z, Wang N (2013) Modelling HIV/AIDS epidemic among men who have sex with men in China. BioMed Research International [Epub ahead of print].
- 116. Xu X, Xiao Y, Wang N (2012) Modeling sexual transmission of HIV/AIDS in Jiangsu province, China. Mathematical Methods in the Applied Sciences 36: 234–248. [Google Scholar]
- 117. Baggaley RF, White RG, Boily M-C (2010) HIV transmission risk through anal intercourse: systematic review, meta-analysis and implications for HIV prevention. International Journal of Epidemiology 39: 1048–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Powers KA, Poole C, Pettifor AE, Cohen MS (2008) Rethinking the heterosexual infectivity of HIV-1: a systematic review and meta-analysis. The Lancet Infectious Diseases 8: 553–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Pappas G, Jia Y, Khan OA (2011) Three decades of HIV/AIDS. Medscape Public Health.
- 120. Liu H, Yang H, Li X, Wang N, Liu H, et al. (2006) Men who have sex with men and human immunodeficiency virus/sexually transmitted disease control in China. Sex Transm Dis 33: 68–76. [DOI] [PubMed] [Google Scholar]
- 121. Prestage GP, Hudson J, Down I, Bradley J, Corrigan N, et al. (2009) Gay men who engage in group sex are at increased risk of HIV infection and onward transmission. AIDS and Behavior 13: 724–730. [DOI] [PubMed] [Google Scholar]
- 122. Dubois-Arber F, Jeannin A, Lociciro S, Balthasar H (2012) Risk reduction practices in men who have sex with men in Switzerland: serosorting, strategic positioning, and withdrawal before ejaculation. Archives of Sexual Behavior 41: 1263–1272. [DOI] [PubMed] [Google Scholar]
- 123. McDaid LM, Hart GJ (2012) Serosorting and strategic positioning during unprotected anal intercourse: are risk reduction strategies being employed by gay and bisexual men in Scotland? Sex Transm Dis 39: 735–738. [DOI] [PubMed] [Google Scholar]
- 124. Butler DM, Smith DM (2007) Serosorting can potentially increase HIV transmissions. AIDS 21: 1218–1220. [DOI] [PubMed] [Google Scholar]
- 125. Huang Z, Wang M, Fu L, Fang Y, Hao J, et al. (2013) Intervention to increase condom use and HIV testing among men who have sex with men in China: a meta-analysis. AIDS Res Hum Retroviruses 29: 441–448. [DOI] [PubMed] [Google Scholar]
- 126. Shao Y (2006) AIDS epidemic at age 25 and control efforts in China. Retrovirology 3: 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Forest plot of UAI prevalence with any male partner among MSM in China.
(TIF)
Forest plot of UAI prevalence with regular male partners among MSM in China.
(TIF)
Forest plot of UAI prevalence with non-regular male partners among MSM in China.
(TIF)
Forest plot of UAI prevalence with casual male partners among MSM in China.
(TIF)
Forest plot of UAI prevalence with commercial male partners among MSM in China.
(TIF)
Forest plot of UIAI prevalence with any male partner among MSM in China.
(TIF)
Forest plot of URAI prevalence with any male partner among MSM in China.
(TIF)
Subgroups analysis of UAI prevalence with any male partner among MSM in different cities of China.
(TIF)
PRISMA Checklist.
(DOC)
Quality assessment of included individual studies.
(DOC)
Characteristics of studies included in this meta-analysis.
(DOCX)