Abstract
Background: The prevalence of obesity and overweight persists in the preschool population, despite some prevention and treatment advances, particularly in minorities. Investigating the prevalence of dyslipidemia and the effect of family health may also guide the focus of intervention efforts.
Methods: Anthropometric data were collected from urban minority preschool children (n=161; 42% female) enrolled in USDA Head Start. Blood was collected by finger prick and analyzed with the Cholestech LDX Analyzer (Cholestech Corporation, Hayward, CA). Caregivers provided a self-reported family health history for cardiovascular diseases (CVDs).
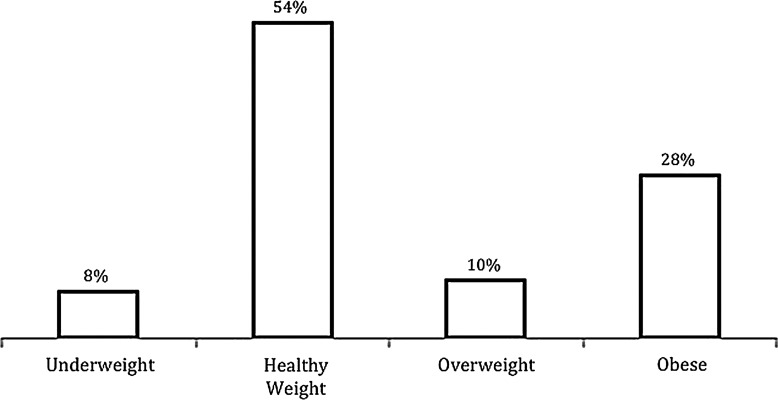
Results: By BMI percentile, 8% of the children were underweight (UW), 54% healthy weight (HW), 10% overweight (OW), and 28% obese (OB). One of every 5 children had borderline or high-risk levels for total cholesterol (TC), high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, and triglycerides based on the National Cholesterol Education Program categories. In OW/OB children only, BMI was positively correlated with TC (r(61)=0.428; p=0.001) and LDL (r(58)=0.395; p=0.005). Child BMI was also associated with family comorbid diseases (r(159)=0.177; p=0.025). UW/HW children with a family history of CVD had significantly higher LDL than UW/HW children without a family history of CVD (p=0.001). Step-wise regression analysis revealed that BMI (p=0.005) plus family history of heart attack (p=0.018) were significant predictors of blood TC levels.
Conclusion: Continued efforts to treat and prevent elevated weight are urgently needed for minority preschoolers. Attention to CVD screening may be an important target in school, community, and healthcare arenas for minority populations regardless of weight status.
Introduction
Cardiovascular disease (CVD) is the leading cause of death in the United States,1 a concern that needs to be addressed early in life. The detrimental relationship between body weight, blood lipids, and CVD risk is well established in adults and youth as young as 5 years.2,3 Although there has been a significant decrease in obesity trends among 2- to 5-year-old children in the last 9 years, there has been no change in infants, toddlers, older youth, and adolescents.4 This age group remains vulnerable because overweight preschool-age children are five times as likely to be overweight during adolescence than are their normal-weight counterparts,5 and this trend continues into adulthood.6,7 Annual medical care costs associated with obesity in childhood have reached $2.9 billion, including the additional prescription drugs, emergency room visits, and outpatient visits,8 indicating an increase in the severity of weight-related health consequences. This is of particular importance in African American preschool children, among whom the rate of obesity is double that of white preschool children,9 and marked disparities exist around access and use of medical care.10
CVD risk factors in children include elevated blood pressure, family health history, and dyslipidemia. Researchers have observed positive associations between CVD risk factors, blood pressure, and measures of weight in preschool-aged children.11–13 A strong link has been found between family CVD health history and a child's risk for CVD.14 Few studies, however, have examined the relationship between weight and blood lipids, and the data vary among ethnic groups. In a study with New York Head Start schools involving a 73% minority sample, obese preschoolers had twice the risk of low high-density lipoprotein (HDL) cholesterol levels, compared to nonobese children.15 Messiah and colleagues have reported racial differences in blood lipid levels and risk factors for CVD in preschoolers. They observed that non-Hispanic black preschoolers showed a correlation between BMI as well as waist circumferences and C-reactive protein; however, total cholesterol (TC) and low-density lipoprotein (LDL) cholesterol were not significantly associated with weight regardless of race in the ethnically diverse sample of 3600 children ages 3–6 years.16 Further research is needed to elucidate the weight and blood lipid relationship in this age group with attention to ethnicity. Overall, advancements in the field prompted the 2008 American Academy of Pediatrics policy update regarding lipid screening in children.17 The policy update states that screening should be completed at least once between the ages of 2 and 10 years for children with a positive family history, including CVD risk factors such as existing CVD, diabetes, and hypertension (HTN).
Low income is associated with lower health status in children,18,19 including iron deficiency anemia20 and obesity.21 Newacheck and colleagues22 found that near-poor or poor children are three times as likely as nonpoor children to experience unmet medical needs. Head Start is a federal program that promotes school readiness and comprehensive services to children ages 3–5 years from low-income families up to 130% of the US poverty guidelines in an effort to overcome educational and economic disadvantage. Therefore, Head Start sites servicing a minority population are an ideal setting to examine CVD risk in preschool-aged, minority, near-poor, or poor children.
Accordingly, this study explored the association between blood lipid levels, family health, and weight in a sample of urban minority children enrolled in Head Start. The aims of this study were to (1) determine the prevalence of obesity and dyslipidemia and (2) investigate the CVD risk through the correlations of weight, dyslipidemia, and family health in a sample of urban minority children enrolled in Head Start in the City of Detroit.
Methods
Setting and Sample
This study presents an analysis of baseline data from the intervention study Healthy Kids Healthy Lives23 with USDA Head Start preschool-age children throughout the 2008–2009 academic year. The study was conducted through a Head Start system with 15 sites in the City of Detroit. A convenience sample of 208 children ages 3–5 years were recruited from six of the Head Start sites. These six sites were chosen because they are all located within close proximity to one another, and therefore it was presumed that they had a similar socioeconomic status. To be eligible for the Head Start program, federal poverty guidelines were used to evaluate the family income. In 2008, the poverty level was $14,000 for a household size of two and $17,600 for a household size of three.24 Other criteria for Head Start include children between 6 weeks and 5 years of age, children with special needs, and foster children with high risk factors. In the present study, no child had special needs. The institutional review board of Wayne State University (Detroit, MI) approved the protocol, permission to conduct the study was received from the Head Start programs, and informed consent was obtained from children's caregivers.
Measurements
Anthropometrics
Weight and height measurements were gathered from preschool-aged children before beginning the Healthy Kids Healthy Lives intervention. Trained graduate student data collectors weighed children without coats and shoes using a portable digital scale (Tanita Model BC551; Tanita Corp of America, Arlington Heights, IL). Two measures were obtained from each child. If the two readings were within 0.1 kg, an average was taken and used as the body weight. If the two readings differed by more than 0.1 kg, a third reading was taken and readings were averaged. Heights were obtained using a portable stadiometer (Seca 214; Seca North America East, Hanover, MD). Two measurements without shoes were recorded. If the two readings were within 0.2 cm of each other, then the readings were averaged and recorded. If the difference was more than 0.2 cm, a third measure was taken before averaging. Weight and height measurements were used to calculate BMI and BMI-for-age percentiles were calculated based on CDC guidelines by using the online calculator.25 All children were categorized as underweight (UW; <5th percentile), healthy weight (HW; 5th to <85th percentile), overweight (OW; 85th–94th percentile), and obese (OB; ≥95th percentile).
Blood Lipids
A registered pediatric nurse obtained a nonfasting blood sample (35 μL) from each enrolled child by finger prick. Blood samples were analyzed immediately using the Cholestech LDX Analyzer (Cholestech Corporation). Every machine was calibrated each day before its use. Output from the machine after a 5-minute processing time included TC, HDL, LDL, and triglycerides (TGs). The results obtained using this machine correlated well with measures obtained by other means.26 Caregivers were notified of the day designated for the procedure for each classroom by letters sent home as well as in-person reminders by research assistants during the previous day's pickup and dropoff. Caregivers were encouraged, but not required, to be present to support the child and receive the incentive of $20 for participation. A Head Start staff member was present during all blood samplings and provided the caregivers, who were unable to attend, with the incentive at the time of pickup.
Family Health
To collect information about family health history, caregivers completed a self-report questionnaire during the orientation session at each school before the commencement of this study. Two investigators were present when the caregivers completed these questionnaires to answer any questions. The caregivers were given sufficient time to complete the questionnaire without feeling rushed. This measure included inquiry about the instance of comorbid diseases, such as diabetes, stroke, heart attack, and high blood pressure in the child's parents or grandparents. The items were summed to create a family health status score ranging from 0 (no comorbid diseases reported) to 4 (four comorbid diseases reported) for scale analysis and a presence of family health risk score dichotomized to yes or no for categorical analysis.
Statistical Analysis
Descriptive statistics were used to present the demographic and lipid data. Comparative values for plasma lipid and lipoprotein risk levels are from the National Cholesterol Education Program (NCEP) Expert Panel on Blood Cholesterol Levels in Children and Adolescents (provided in Table 1).27 Child BMI percentile was categorized into UW/HW and OW/OB, and group correlations were performed with lipid levels. Chi-square tests were used to examine relationships between family health status (defined as presence of a comorbid disease), child weight status, and child blood-lipid risk. Interactions among child weight status and family health history on blood lipid levels were analyzed by general linear models. All statistical analyses were conducted with IBM SPSS Statistics 20.0 (IBM Corp., Armonk, NY), and the significance level was set at p<0.05.
Table 1.
Blood Lipid Risk of Preschool-Age Children
| Acceptable level n, (%) | Borderline risk n, (%) | High risk n, (%) | Blood lipid rangesa | |
|---|---|---|---|---|
| Total cholesterol (n=161) | 125 (78) | 28 (17) | 8 (5) | Acceptable <170 Borderline 170–199 High ≥200 |
| Low-density lipoprotein (n=119) | 91 (77) | 20 (17) | 8 (7) | Acceptable <110 Borderline 110–129 High ≥130 |
| High-density lipoprotein (n=157) | 95 (61) | 34 (22) | 28 (18) | Acceptable >45 Borderline 40–45 High ≤40 |
| Triglycerides (n=147) | 77 (52) | 32 (22) | 38 (26) | Acceptable <75 Borderline 75–99 High ≥100 |
National Cholesterol Education Program Expert Panel on Blood Cholesterol Levels in Children and Adolescents.27
Results
The final sample of 161 children included only those with complete total cholesterol and family health data. There were no differences in body weight and BMI percentile between those who participated and those who declined to participate in this study. The racial distribution is as follows: 149 (92.5%) African Americans; 3 (1.9%) Hispanic; 1 Asian/Pacific Islander (0.6%); 1 Caucasian (0.6%), and 7 (4.3%) other. Instances of missing data resulted when caregivers were not available to complete the questionnaire (n=31; 15%) or refused to participate in the blood sampling (n=16; 7%). Of those caregivers who provided the household income data (n=100), 80 (80.0%) were below the federal poverty guidelines set for 2008, 11 (11.0%) were between 101% and 130% of poverty guidelines, 3 (3.0%) were between 131% and 150% of the poverty guidelines, and 6 (6.0%) were 150% above the poverty guideline levels. Machine-reading error also resulted in the decreased sample size for HDL, LDL, and TGs. Mean age of the children was 3 years and 7 months (±7 months). Body weight distribution, according to BMI percentile, is shown in Figure 1.
Figure 1.
Body weight distribution according to BMI percentile for the minority preschoolers in the current study.
Blood Lipid Levels
At least 1 of every 5 children in this preschool-age sample presented with borderline or high-risk level for TC, HDL, LDL, and TGs based on the NCEP risk categories. Regardless of weight status 40% or more of the children had borderline or high-risk levels of HDL and TGs. The 85th and 95th percentiles for TC are 182 and 201 mg/dL; for LDL, 121 and 132 mg/dL; and for TG, 123 and 174 mg/dL, respectively. For HDL, the 15th and 5th percentiles are 36.5 and 28 mg/dL, respectively. In the OW/OB children only, BMI was positively correlated with total cholesterol (r(61)=0.428; p=0.001) and LDL (r(58)=0.395; p=0.005). Blood-lipid risk levels are presented in Table 1.
Family Health History
Over half of the caregivers reported a family health history of one or more comorbid diseases (Table 2). High blood pressure was the most frequent comorbidity (40%), followed by diabetes (21%), heart attack (14%), and stroke (12%). Child BMI was positively associated with the number of comorbid diseases reported (r(159)=0.177; p=0.025). However, no relationship was found between family comorbid diseases and child BMI category (chi-square) (χ2; [1; N=159]=0.82; p=0.37) or blood-lipid risk (TC, χ2 [1; N=182]=0.81; p=0.37; LDL, χ2 [1; N=133]=1.72; p=0.19; TGs, χ2 [1; N=167]=0.30; p=0.59; and HDL, χ2 [1; N=179]=0.73, p=0.39).
Table 2.
Caregiver-Reported Family Health Status
| Number of diseases reported | Number of caregivers | Percent of caregivers |
|---|---|---|
| 0 | 76 | 47 |
| 1 | 48 | 30 |
| 2 | 22 | 14 |
| 3 | 12 | 7.5 |
| 4 | 3 | 1.9 |
TC levels were significantly higher in children with a family history of CVD (with: 163.2±5.8 vs. without: 149.9±2.4 mg/dL; p=0.046), but were not affected by the weight categories. Blood LDL levels tended to be higher in children with a family history of CVD than those without (99.9±7.5 vs. 85.0±2.9 mg/dL; p=0.067). However, an interaction between a family history of CVD and children's weight category was observed for blood LDL levels (Table 3). UW/HW children with a family history of CVD had significantly higher LDL than UW/HW children without a family history of CVD. This difference in LDL levels based on family history of CVD was not observed in OW/OB children.
Table 3.
Blood Lipid Levels Based on Body Weight Category and Family CVD History
| With family CVD history | Without family CVD history | |||
|---|---|---|---|---|
| UW/HW | OW/OB | UW/HW | OW/OB | |
| TCa (mg/dL) | 167.5±10.8 | 159±3.9 | 145.4±2.7 | 154±4.1 |
| LDL* (mg/dL) | 111.8±15.4 | 88.2±10.5 | 79.5±2.8 | 90.6±5.2 |
| HDL (mg/dL) | 49.5±2.9 | 52.4±3.9 | 48.8±1.5 | 48.4±1.5 |
| TG (mg/dL) | 73.8±6.8 | 113.6±37.6 | 82.8±4.4 | 90.2±8.7 |
| With family HTN history | Without family HTN history | |||
|---|---|---|---|---|
| UW/HW | OW/OB | UW/HW | OW/OB | |
| TC (mg/dL) | 148±4.9 | 156±4.4 | 148±3.6 | 155±5.5 |
| LDL (mg/dL) | 87.5±5.7 | 88.9±6.3 | 82.1±4.3 | 91.5±6.7 |
| HDL (mg/dL) | 47.3±2.4 | 46.3±2.0 | 50.1±1.6 | 50.6±2.1 |
| TGb,** (mg/dL) | 83.6±5.3 | 112.4±13.2 | 79.7±5.3 | 78.3±9.2 |
TC levels were significantly higher in children with a family history of CVD than in children without a family history of CVD (p=0.046).
TG levels were significantly higher in children with a family history of HTN than in children without a family history of HTN (p=0.027).
Family CVD history×BMI category interaction, p=0.034.
Family history×BMI category interaction, p=0.068.
CVD, cardiovascular disease; UW, underweight; HW, healthy weight; OW, overweight; OB, obese; TC, total cholesterol; LDL, low-density lipoprotein; HDL, high-density lipoprotein; TG, triglyceride; HTN, hypertension.
A family history of HTN and body weight categories did not affect TC or LDL levels. Children with a family history of HTN tended to have lower HDL, as compared to children without a family history of HTN (46.8±1.6 vs. 50.3±1.4 mg/dL; p=0.088). Body weight did not affect HDL status. A family history of HTN was associated with significantly elevated blood TG levels (with: 98.0±6.1, without: 79.0±5.4 mg/dL; p=0.027). OW/OB children from families with a history of HTN tended to have higher TG levels than those without (112.4±13.2 vs. 78.3±9.2 mg/dL; p=0.055). No such difference was observed in children without a family history of HTN. No other interaction between family health history and BMI categories was observed for other blood lipid data. Step-wise regression analysis revealed that BMI (p=0.005) plus family history of heart attack (p=0.018) are significant predictors of blood TC levels. No other factors, such as family income, caregivers' education levels, and child's gender, played a role in determining blood lipid levels.
There was a significant interaction between BMI category and family CVD history in LDL level.
Discussion
This study examined the prevalence of obesity and dyslipidemia in a sample of urban minority children enrolled in Head Start in the City of Detroit. It also aimed to investigate the children's CVD risk through the interaction of weight, dyslipidemia, and family health. The prevalence of having a BMI ≥95th percentile was more than 1 in 4 in this specific sample and reached almost 40% when the OW and OB BMI categories were combined. These rates are higher than both the non-Hispanic black National Health and Nutrition Examination Survey sample (24%)9 and a sample of over 300 non-Hispanic black Head Start preschoolers in the south (18%).28 The data suggest that environment, such as high unemployment (approximately 19% in 200829) and crime rates (938 per 100,000 in 200830), in the local economy may have an effect on weight in these young African American children. The high crime rate in this city may have made the environment unsafe for young children to engage in outdoor activities, thus reducing physical activity levels. The high unemployment rate creates a financial burden in the family that may force caregivers to purchase low-quality and inexpensive foods, which are usually high in fat and salt,31 for the family. Family eligibility to enroll in the USDA Head Start program also demonstrates that these children are at a higher socioeconomic disadvantage. Thus, community-specific interventions with a focus on weight loss and weight maintenance in this age group are needed to curb the proven progression of weight into later childhood, adolescence, and adulthood.32 A recent review by Kuhl and colleagues33 suggests that preschool is an optimal time for shaping healthy weight habits through family-based behavioral weight interventions.
Rates of dyslipidemia were elevated in our preschool participants regardless of weight status. In particular, unhealthy HDL and TG levels affected 40% or more of the minority children. Interestingly, the literature has shown that African Americans are less likely than non-Hispanic whites to have unhealthy levels of these two blood parameters,34 which subsequently may mask the risk of CVD in this minority group. Positive relationships between BMI and TC as well as between BMI and LDL were also found among the children classified as overweight and obese, a finding not consistent with existing literature with Head Start minority youth.15 Additional research is needed to understand the risk of weight and blood lipids in preschool-aged children.
Because of the lack of definitive evidence, the US Preventive Services Task Force35 has not made any recommendation for or against lipid screening among children and adolescents. In contrast, the Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents Summary Report36 suggests that medical providers obtain a fasting lipid profile in children ages 1–4 years if a family history is positive for early CVD, a parent presents with dyslipidemia, and in the presence of any other risk factors, such as elevated BMI. The current study did find an association between child BMI and endorsement of a family health history positive for CVD. Family history of CVD was also related to increased lipid levels in the children without excess weight. Thus, it is prudent that pediatricians recommend blood lipid level measures early for children with family history of CVD, even though they are not overweight or obese. Overall, the inconsistent national recommendations paired with studies indicating interventions are needed in medical settings around the implementation of screening recommendations,37 and disparities in the follow-up care of minority children38 suggest that a gap may exist in current health services for minority preschoolers at risk for CVD.
There are limitations to address within this study, including the small, convenience sample. The preschool children also provided nonfasted blood for the lipid profiling, which may affect TG levels in particular. No waist circumference or blood pressure were measured, thus no inference about metabolic syndrome can be made for this group of young children. Because this sample is a homogeneous sample in terms of family income, education levels, and neighborhood surroundings, the relationships between BMI, BMI percentile, and blood lipid parameters may have been masked as a result of small variances.
Conclusion
This study found high levels of dyslipidemia and family history for CVDs in addition to elevated weight in this specific sample of minority preschool children. Relationships were also found between child weight and (1) lipid levels, specifically total cholesterol and LDL, and (2) reported family health history of CVDs. Continued efforts to treat and prevent elevated weight are urgently needed for minority preschoolers. Providing regular healthcare and screening in this population may be beneficial for the prevention and care of future cardiovascular complications.
Acknowledgments
This research was supported by Wayne State University Research Enhancement Funds (to K.-L.C.J.). The authors greatly thank the families for their participation.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Hoyert D, Xu J. Deaths: Preliminary data for 2011. Natl Vital Stat Rep 2012;61:1–64 [PubMed] [Google Scholar]
- 2.Friedemann C, Heneghan C, Mahtani K, et al. Cardiovascular disease risk in healthy children and its association with body mass index: Systematic review and meta-analysis. BMJ 2012;345:e4759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nadeau KJ, Maahs DM, Daniels SR, et al. Childhood obesity and cardiovascular disease: Links and prevention strategies. Nat Rev Cardiol 2011;8:513–525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nader PR, O'Brien M, Houts R, et al. Identifying risk for obesity in early childhood. Pediatrics 2006;118:e594–e601 [DOI] [PubMed] [Google Scholar]
- 6.Field AE, Cook NR, Gillman MW. Weight status in childhood as a predictor of becoming overweight or hypertensive in early adulthood. Obes Res 2005;13:163–169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stettler N, Iotova V. Early growth patterns and long-term obesity risk. Curr Opin Clin Nutr Metab Care 2010;13:294–299 [DOI] [PubMed] [Google Scholar]
- 8.Trasande L, Chatterjee S. The impact of obesity on health service utilization and costs in childhood. Obesity 2009;17:1749–1754 [DOI] [PubMed] [Google Scholar]
- 9.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012;307:483–490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flores G, Tomany-Korman SC. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics 2008;121:e286–e298 [DOI] [PubMed] [Google Scholar]
- 11.Jones A, Charakida M, Falaschetti E, et al. Adipose and height growth through childhood and blood pressure status in a large prospective cohort study. Hypertension 2012;59:919–925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Voors AW, Webber LS, Berenson GS. Blood pressure of children, ages 2 1/2–5 1/2 years, in a total community—the Bogalusa heart study. Am J Epidemiol 1978;107:403–411 [DOI] [PubMed] [Google Scholar]
- 13.Hernandez B, Uphold CR, Graham MV, et al. Prevalence and correlates of obesity in preschool children. J Pediatr Nurs 1998;13:68–76 [DOI] [PubMed] [Google Scholar]
- 14.Imes CC, Lewis FM. Family history of cardiovascular disease, perceived cardiovascular disease risk, and health-related behavior: A review of the literature. J Cardiovasc Nurs 2014;29:108–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams CL, Strobino B, Bollella M, et al. Body size and cardiovascular risk factors in a preschool population. Prev Cardiol 2004;7:116–121 [DOI] [PubMed] [Google Scholar]
- 16.Messiah SE, Arheart KL, Natale RA, et al. BMI, waist circumference, and selected cardiovascular disease risk factors among preschool-age children. Obesity (Silver Spring) 2012;20:1942–1949 [DOI] [PubMed] [Google Scholar]
- 17.Daniels SR, Greer FR; Committee on Nutrition. Lipid screening and cardiovascular health in childhood. Pediatrics 2008;122:198–208 [DOI] [PubMed] [Google Scholar]
- 18.Yoo J, Slack K, Holl J. Material hardship and the physical health of school-aged children in low-income households. Am J Public Health 2009;99:829–836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ashiabi GS, O'Neal KK. Children's health status: Examining the associations among income poverty, material hardship, and parental factors. PLoS One 2007;2:e940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alaimo K, Olson C, Frongillo E Jr, et al. Food insufficiency, family income, and health in US preschool and school-aged children. Am J Public Health 2001;91:781–786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maher EJ, Li G, Carter L, et al. Preschool child care participation and obesity at the start of kindergarten. Pediatrics 2008;122:322–330 [DOI] [PubMed] [Google Scholar]
- 22.Newacheck PW, Hughes DC, Hung YY, et al. The unmet health needs of America's children. Pediatrics 2000;105:989–997 [PubMed] [Google Scholar]
- 23.Shen B, Reinhart-Lee T, Janisse H, et al. African American preschool children's physical activity levels in Head Start. Res Q Exerc Sport 2012;83:168–174 [DOI] [PubMed] [Google Scholar]
- 24.US Department of Health and Human Services. Head Start. Poverty guidelines and determining eligibility for participation in Head Start programs. Available at http://eclkc.ohs.acf.hhs.gov/hslc/tta-system/operations/mgmt-admin/eligibility-enroll/income/PovertyGuideline.htm Last accessed March12, 2014
- 25.Centers for Disease Control and Prevention. BMI percentile calculator for child and teen—English version. Available at http://apps.nccd.cdc.gov/dnpabmi Last accessed March4, 2014
- 26.Shepard M, Mazzachi B, Shepard A. Comparative performance of two point-of-care analysers for lipid testing. Clin Lab 2007;53:561–566 [PubMed] [Google Scholar]
- 27.National Cholesterol Education Program Expert Panel on Blood Cholesterol Levels in Children and Adolescents. National Cholesterol Education Program (NCEP): Highlights of the report of the expert panel on blood cholesterol levels in children and adolescents. Pediatrics 1992;89:495–501 [PubMed] [Google Scholar]
- 28.Acharya K, Feese M, Franklin F, et al. Body mass index and dietary intake among Head Start children and caregivers. J Am Diet Assoc 2011;111:1314–1321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Homefacts. Detroit, MI unemployment rate report. Available at www.homefacts.com/unemployment/Michigan/Wayne-County/Detroit.html Last accessed March12, 2014
- 30.Crime rate in Detroit, Michigan (MI): Murders, rapes, robberies, assaults, burglaries, thefts, auto thefts, arson, law enforcement employees, police officers, crime map; Available at www.city-data.com/crime/crime-Detroit-Michigan.html Last accessed March12, 2014 [Google Scholar]
- 31.Appelhans BM, Milliron BJ, Woolf K, et al. Socioeconomic status, energy cost, and nutrient content of supermarket food purchases. Am J Prev Med 2012;42:398–402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cunningham SA, Kramer MR, Narayan KM. Incidence of childhood obesity in the United States. N Engl J Med 2014;370:403–411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kuhl ES, Clifford LM, Stark LJ. Obesity in preschoolers: Behavioral correlates and directions for treatment. Obesity 2012;20:3–29 [DOI] [PubMed] [Google Scholar]
- 34.Sumner AE. Ethnic differences in triglyceride levels and high-density lipoprotein lead to underdiagnosis of the metabolic syndrome in black children and adults. J Pediatr 2009;155:S7.e7–e11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.US Preventive Services Task Force. Screening for lipid disorders in children: Recommendation statement. Available at www.uspreventiveservicestaskforce.org/uspstf07/chlipid/chlipidrs.htm Last accessed March12, 2014
- 36.National Heart, Lung, and Blood Institute. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents: Summary report. NIH publication no. 12-7486A. US Department of Health and Human Services, National Institues of Health, National Heart, Lung, and Blood institute: Bethesda, MD, 2012 [Google Scholar]
- 37.Van Cleave J, Kuhlthau KA, Bloom S, et al. Interventions to improve screening and follow-up in primary care: A systematic review of the evidence. Acad Pediatr 2012;12:269–282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weinick R, Krauss N. Racial/ethnic differences in children's access to care. Am J Public Health 2000;90:1771–1774 [DOI] [PMC free article] [PubMed] [Google Scholar]