Abstract
Background: Cellular phones enable communication between healthcare providers and patients for prevention, diagnosis, and treatment of diseases. However, few studies have examined the user-friendliness or effectiveness of cellular phone-based medical informatics (CPBMI) for healthcare. Materials and Methods: This study investigated the use of CPBMI to identify its current status within the medical field, advantages and disadvantages, practicability, clinical effectiveness, costs, and cost-saving potential. Results: CPBMI was validated in terms of practicality and provision of medical benefits. It is critical to use CPBMI in accordance with the different features of each disease and condition. Use of CPBMI is expected to be especially useful for patients with chronic disease. Conclusions: We discussed the current status of the clinical use, benefits, and risks of CPBMI. CPBMI and information technology–based health management tools are anticipated to become useful and effective components of healthcare management in the future.
Key words: : cellular phone, mobile health, healthcare, telemedicine
Introduction
Various types of chronic diseases such as diabetes mellitus (DM), hypertension, hyperlipidemia, and cardiovascular disease have been the focus of intense research in recent years.1,2 Attention to these diseases has increased in tandem with the rapid increase in the elderly population due to improvements in living standards and the development of medical technologies.3–6 Despite new developments in various pharmaceutical treatments and health management methods, continued population aging will ultimately result in the increase in public health expenditures, threatening national welfare and medical systems. Therefore, development of solutions by thorough analysis of the problems that must be faced is essential.
Recently, telemedicine and ubiquitous healthcare, which have been extensively studied for several years, have received additional attention with the development of biosensors and information technology (IT)–based devices and systems that enable patients to receive healthcare information and services without any restrictions of time and place. Because of these advantages, use of IT-based devices and systems has been proposed as means of reducing medical costs while improving the quality of medical services. In the past, IT-based medical services were only provided temporarily or restricted to use for health management by existing health providers. As the convergence of IT and medical services has increasingly enabled patients to access medical services in the course of their daily lives without time or space limitations, use of biosensors and related forms of medical technology has become a preferred means of delivering healthcare services.
The rapid increase in use of cellular phones in recent years has encouraged the development of significantly advanced health applications. In what has become known as cellular phone-based medical informatics (CPBMI) for healthcare, cellular phone-based personal healthcare tools aimed at prevention, diagnosis, and treatment of diseases are used to enable communication between healthcare providers and patients. Despite their proliferation, few studies have examined the user-friendliness or effectiveness of CPBMI tools or their commercialization potential. It is particularly essential to investigate patient and provider experiences with CPBMI to assist in the effective linking of mobile health and health management services. Before applying a newly developed system to medical practice, evidence-based examination of the practicality and clinical effectiveness of the system and cost–benefit analysis of its potential for commercialization should be conducted. To contribute to the fulfillment of these research needs, this study systematically reviewed the results of previous studies that had investigated the use of CPBMI to identify its current status within the medical field, advantages and disadvantages, practicality, clinical effectiveness, costs, and cost-saving potential.
Clinical Evidence of CPBMI
Current Clinical Use
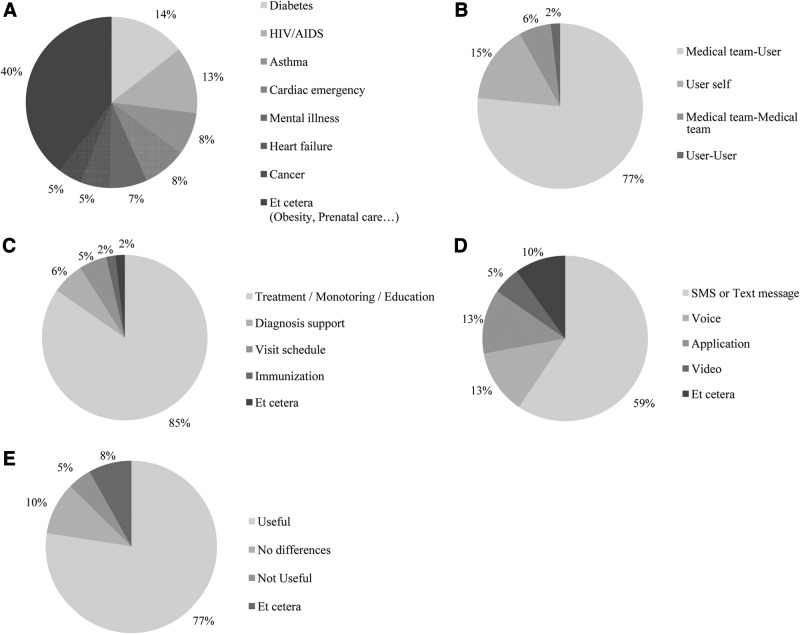
A search of Medline for scientific articles published between January 2003 and December 2012 using the search MeSH terms “cellular phone” and “delivery of health care” was conducted. MeSH terms were used for further detailed description of the search strategy. Among the 136 retrieved articles, 25 were excluded (14 articles did not focus on cellular phone health, 4 were case studies, 3 were not provided with full text, and the remaining 4 were ongoing studies), leaving a total of 111 articles for further analysis. Review of the 111 articles indicated that clinical research into disease management using CPBMI began increasing in 2003 and dramatically increased in 2007, the year in which the smartphone was released, as reflected in the large increase in the number of research articles published since that year. Among all diseases, DM (16 of 111 [14.4%]) was the most frequently examined disease in the articles, followed by human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) (14 of 111 [12.6%]) and asthma (9 of 111 [8.1%]) (Fig. 1A). From the simple use of short message service (SMS) by medical professionals for providing recommendations to the use of complex smartphone applications, increased access to cellular phones has introduced many options for providing medical feedback to patients. In terms of the relationship between providers and receivers of medical information, the most common issues examined by the articles were the active involvement of medical teams while communicating with patients (85 of 111 [76.6%]), patient self-management (17 of 111 [15.3%]), communication among medical team members (7 of 111 [6.3%]), and communication among patients (2 of 111 [1.8%]) (Fig. 1B). The most commonly studied research topics were the use of CPBMI in disease management, education, and monitoring (94 of 111 [84.7%]), disease diagnosis (7 of 111 [6.3%]), and confirmation of appointments (6 of 111 [5.4%]), all of which have been explored in previous studies (Fig. 1C). Use of SMS or text messaging (66 of 111 [59.5%]), applications (14 of 111 [12.6%]), direct phone calls (14 of 111 [12.6%]), and videoconferencing (6 of 111 [5.4%]) were the most frequently used methods for transferring information between patients and doctors (Fig. 1D). The results revealed that 77.5% (86 of 111) of those using CPBMI found it useful, whereas 4.5% (5 of 111) did not find it to be beneficial (Fig. 1E). Other CPBMI uses examined included transmission of photographs of injuries by patients to doctors for review and treatment recommendations7 and reminders regarding appointments by hospitals to patients.8,9
Fig. 1.
Areas of focus in the 111 articles examined: (A) type of disease, (B) types of users, (C) type of feedback, (D) type of communication, and (E) usefulness of cellular phone-based medical informatics for healthcare. COPD, chronic obstructive pulmonary disease; HIV/AIDS, human immunodeficiency virus/acquired immunodeficiency syndrome; SMS, short message service.
Among the services and outcomes examined for various diseases, improvement in medication adherence, keeping hospital appointments, and lifestyle management were the focus of articles investigating the use of CPBMI by HIV/AIDS patients and healthcare providers.10–13 Medication adherence and provision of education to enable self-regulation were the focus of articles investigating the use of CPBMI by asthma patients and healthcare providers.14–17 Active participation in lifestyle management and the feedback regarding blood glucose levels were mainly discussed in studies of CPBMI in diabetes patients and healthcare providers.18–24 Notably, many articles reported the use of CPBMI in enabling lifestyle modification in the treatment of all three diseases, but they described the use of different services in accordance with the characteristics of each disease. Articles that examined the use of CPBMI by diabetes patients and healthcare providers reported that programs with IT infrastructure showed increased effectiveness of management, even with a minimal number of hospital visits.
Diabetes Mellitus
CPBMI is considered particularly effective in the treatment of DM, one of the most studied diseases, whose management requires adherence to appropriate pharmacotherapy with concurrent management of lifestyle factors, including diet and exercise. In the 16 articles that focused DM, 3 articles had the same design and different study periods18,25,26; therefore we selected the latest study.18 Of the 14 articles that focused on DM, 11 reported the results of clinical trials (Table 1),18–24,27–30 2 suggested systems,31,32 and 1 explored other issues.33 Most previous clinical trials of the use of CPBMI in DM management investigated a medical team's use of CPBMI to provide medical information to patients and assess patients' glycated hemoglobin level, an indicator of the average plasma glucose concentration for the previous 3 months.34 The overall results of these studies indicated that use of CPBMI is an effective means of managing blood glucose levels. Studies suggesting a system evaluated the methods of improving health conditions with lifestyle modifications, such as diet and exercise, by enabling access to patient medical records by medical team members and obtaining medical feedback from patients living in remote areas. The practicality of various DM-related applications has already been demonstrated. In particular, previous studies have confirmed that the active involvement of medical teams improves the glucose-lowering effects of traditional DM treatments. However, active involvement of medical teams is directly related to increased medical costs; hence, cost–benefit analysis using valid methods should be conducted, along with an analysis of the use of artificial intelligence or clinical decision support systems (CDSSs) for reducing personnel expenses.35,36
Table 1.
Results of Clinical Trials Investigating Cellular Phone-Based Medical Informatics for Healthcare Use in the Management of Diabetes Mellitus
| REFERENCE (YEAR) | RELATIONSHIP | AGE (YEARS) | STUDY DURATION | INTERVENTION (N) | FEEDBACK | HBA1C REDUCTION FROM BASELINE (%) | P VALUE |
|---|---|---|---|---|---|---|---|
| Bell et al.19 (2012) | M-U | 55±10 | 52 weeks | Video message group (32) | Video message | −1.3 | 0.002a |
| 60±11 | Control group (33) | Usual care | −0.9 | <0.002a | |||
| Zolfaghari et al.20 (2012) | M-U | 51.07 | 12 weeks | SMS group (38) | SMS | −1.01 | <0.01a |
| 53.71 | Telephone group (39) | Phone | −0.93 | <0.01a | |||
| Shetty et al.21 (2011)b | M-U | 50.1±9.9 | 52 weeks | SMS and Internet group (110) | SMS | — | <0.007a |
| 50.5±8.3 | Control group (105) | Usual care | — | NSa | |||
| Schiel et al.27 (2011)c | U-self | 14.5±2.2 | 1–3 days | Physical activity application (16) | Self-monitor | ||
| Carroll et al.28 (2011) | M-U | 14–18 | 12 weeks | Phone group (10) | Voice+SMS | −0.5 | 0.04a |
| Curran et al.29 (2010)c | U-self | — | 2 weeks | 6 patients | Suggestion of AI insulin dose | ||
| Istepanian et al.30 (2009) | M-U | 60±12 | 9 months | Telemonitoring group (72) | Message letter | −0.14 | 0.06d |
| 57±13 | Control group (65) | Usual care | +0.30 | ||||
| Cho et al.22 (2009) | M-U | 45.2±11.3 | 12 weeks | Internet group (34) | Internet-based | −0.7 | <0.01a |
| 51.1±13.2 | Phone group (35) | SMS feedback | −1.2 | <0.01a | |||
| Kim et al.23 (2008) | M-U | 45.5±9.1 | 52 weeks | SMS and Internet group (18) | SMS feedback | −1.49 | <0.05a |
| 48.5±8.0 | Control group (16) | Usual care | +0.53 | NSa | |||
| Kim et al.18 (2006) | M-U | 46.8±8.8 | 52 weeks | SMS and Internet group (25) | SMS feedback | −1.05 | <0.05a |
| 47.5±9.1 | Control group (26) | Usual care | +0.11 | NSa | |||
| Kim et al.24 (2006)e | M-U | 41.5±12.3 | 12 weeks | SMS and Internet group (25) | SMS feedback | Not checked | |
| No control group |
Data are mean±standard deviation values unless otherwise indicated.
p value from baseline to the end of the study within the same group, dp value at the end of the study between the two groups.
Results of Shetty et al.21: the percentage of those with glycated hemoglobin (HbA1c)<8% went from 30.8% to 55.1% in the short message service (SMS) group (p<0.007) and from 31.8% to 48.5% in the control group.
Results of Schiel et al.27 and Curran et al.29 indicated that use of cellular phone-based medical informatics is an acceptable means of managing blood glucose levels.
Results of Kim et al.24: mean decrease of 28.6 mg/dL (p=0.006) in fasting plasma glucose levels and 78.4 mg/dL (p=0.003) in 2-h postprandial blood sugar levels.
AI, artificial intelligence; M-U, interaction between medical providers and users; NS, not significant; U-self, users' self-management without interaction with medical providers.
Among the articles exploring management of blood glucose levels, a greater number examined Web-based tools, compared with those using CPBMI-based tools. One study suggested that use of Web-based tools provides both short- and long-term benefits and that use of a CDSS reduces personnel expenses.35 As the length of messages using SMS is limited, use of Web-based tools is beneficial in the delivery of large amounts of information. Above all, use of either Web-based or CPBMI-based tools motivates DM patients, particularly those living in rural regions with few specialized hospitals or with limited access due to physical impairment, to participate in DM management and lifestyle modification. Further evidence-based clinical investigation of the effectiveness of CPBMI in DM management needs to be conducted in this direction.
ASTHMA
Of the nine articles that examined the use of CPBMI by asthma patients and healthcare providers, eight were original research articles14–17,37–40 examining asthma management programs using SMS, and the last was a qualitative study.41 Of the eight original articles (Table 2), six investigated the effectiveness of using CPBMI in terms of convenience and self-management, focusing primarily on the use of CPBMI for self-management rather than for the control of asthma and its related adverse effects. Previous studies found that simple use of SMS increased medication compliance, early detection of adverse effects, and management during the course of daily life without the need to visit a hospital. Although the articles reported that use of CPBMI improved the practicability of and ability to engage in self-management, additional research is needed to confirm these findings while considering the economic aspects of CPBMI use. For chronic disease patients, the ability to engage in self-regulation is a critical indicator of successful outcomes. Thus, it is ideal that personnel in the health system take responsibility for monitoring medical outcomes while taking advantage of CPBMI to improve patient self-management of diseases and risk factors.
Table 2.
Results of Clinical Trials Investigating Cellular Phone-Based Medical Informatics for Healthcare Use in the Management of Asthma
| REFERENCE (YEAR) | RELATIONSHIP | AGE (YEARS) | STUDY DURATION | INTERVENTION (N) | FEEDBACK | RESULTS |
|---|---|---|---|---|---|---|
| Seid et al.14 (2012) | M-U | 15.1±1.67 | 12 weeks | Phone and text messaging group (12) | Text messages | Acceptable and feasible |
| Control group (14) | ||||||
| Petrie et al.15 (2012) | M-U | 16–45 | 18 weeks | Text message group | Text messages | Increases adherence to inhaler |
| Control group | ||||||
| Britto et al.16 (2012) | M-U | 15.2±1.4 | 12 weeks | Teenagers with asthma (12) | Text messages | May support self-management |
| Strandbygaard et al.17 (2010) | M-U | 34.4 | 12 weeks | SMS group (12) | Text messages | Increased adherence to medication |
| 30.7 | Control group (14) | |||||
| Ryan et al.37 (2012) | M-U | 46.6±18.0 | 26 weeks | Mobile phone monitoring (145) | Text messages | Did not improve asthma controlNot cost-effective |
| 51.5±17.7 | Paper-based monitoring (143) | |||||
| Prabhakaran et al.38 (2010) | U-self | 50.4±1.9 | 26 weeks | Mobile telephone group (43) | Self-care program | ConvenientImproves asthma self-control |
| 54.0±2.4 | Control group (46) | |||||
| Liu et al.39 (2011) | M-U | 37±12 | 44 weeks | SMS group (60) | Text messages | No significant differences No reduction in admission rates (p=0.5) |
| 40±13 | Control group (60) | |||||
| Anhøj et al.40 (2004) | M-U | 38.5 | 12 weeks | SMS group (12) | Text messages | May be a tool for supporting self-management |
Data are mean±standard deviation values unless otherwise indicated.
M-U, interaction between medical providers and users; SMS, short message service; U-self, users' self-management without interaction with medical providers.
Because CPBMI use is targeted at patients with chronic diseases, most users tend to be of advanced age, with the exception of asthma patients, who tend to be much younger than patients with other chronic diseases. Although younger patients tend to be less averse to using cellular phones and new devices and as a group tend to use cellular phones more actively, their level of interest in and their understanding of their disease and motivation to engage in treatment tend to be significantly higher than those of older patients. Such differences between older and younger patients call for additional large-scale research to identify the proper approach to using CPBMI with each patient age group.
Among the many asthma-related smartphone applications that have emerged in recent years, several are for use during emergency events, such as the sudden occurrence of asthma, whereas others allow mobile measuring devices to be connected to the smartphone to check the patient's condition and transmit the data that will be useful for subsequent procedures. Global positioning systems have also been installed in inhalers to collect geographic data useful to healthcare providers for identifying the areas in which inhalers are most widely used. Overall, the findings reported in the articles focusing on asthma patients and healthcare providers indicate the great potential of smartphone applications in the management of asthma.
HIV/AIDS
Since the introduction of antiretroviral therapy (ART), HIV-infected patients have experienced greatly improved prognosis.42 Maintaining the effects of ART over long periods requires strict adherence to ART; while irregular adherence is associated with decreased effectiveness, increased drug resistance, and consequential failure of therapy, high adherence is associated with improved virologic outcomes, reduced virologic failure, and shorter term of hospitalization.43 Adherence to ART is affected by the interaction between healthcare providers and patients as well as the psychosocial condition of the patient. Hence, increasing the motivation of patients to participate in therapy and adhere to ART are primary concerns of healthcare providers. Therefore, it needs to focus on the majority of CPBMI-based health management programs for HIV patients.
Besides promoting adherence to ART, CPBMI-based tools can be used for providing information to and counseling patients living in remote regions or who have limited access to medical services. Successful use of systems alerting patients of the importance of medication adherence and determining intake status via SMS has been reported in many countries, including Kenya36,37 and Cameron.38 In the case of Kenya, one study found that adherence to ART was significantly higher (p=0.006) and suppression of viral load was significantly increased (p=0.04) in the group with access to SMS use (61.5% and 57.1%, respectively) compared with values in those without access (49.8% and 48.3%, respectively).11 In addition, counseling via cellular phone was found to increase the level of adherence from 87% to 94% and improve self-efficacy (p<0.05).13
Several studies have demonstrated the practicality of CPBMI use in various aspects of HIV treatment.44–46 As a consequence, many investigators have attempted to develop management systems for better outcomes of HIV patients, and scientific evidence of the clinical effects of mobile applications has been reported.
Future Prospects of CPBMI
Based on the results, CPBMI was validated in terms of practicality and provision of medical benefits. Therefore, it is critical to use CPBMI in accordance with the different features of each disease and condition. Lifestyle management appears to be the priority in the use of CPBMI by patients with chronic diseases and their healthcare providers. Use of CPBMI is expected to be especially useful for patients with not only chronic diseases related to unhealthy lifestyles, such as obesity, high blood pressure, and DM, but also for patients from whom biometric data must be consistently collected, such as those who have undergone cardiac surgery or have congestive heart failure or asthma. Use of CPBMI by such patients is anticipated to contribute to the prevention of secondary complications and reduction of medical costs.
Technological Improvements
Accuracy of monitoring devices and networks for communication
Close and constant cooperation between patients and healthcare providers is key to chronic disease management.47 Comprehensive biometric information collected during the course of a patient's daily life needs to be reliably transferred to healthcare providers to enable ongoing monitoring of the patient's condition and prompt identification of a worsening prognostic condition that requires early intervention and secondary prevention. To accomplish these outcomes, sensing devices and networks must be able to collect accurate data in a reliable manner.
Comfort and convenience of using devices
As patients with chronic diseases tend to be of advanced age, many are likely to experience difficulty adapting to a new device. This fact presents a major challenge, as the patient level of satisfaction in using devices directly determines patient compliance with their use.48 Hence, cellular phones that are simple and convenient for use by older patients must be designed. Fortunately, most studies have found that the study participants adapted well to the devices investigated.22,23,30 Recent developments in smartphones and networks for communication are expected to contribute to the increased use of CPBMI, which in turn is expected to increase the release of mobile medical applications. To promote the stability and reliability of mobile medical applications, assessment criteria should be defined, and official guidelines should be provided for smartphone applications.
Medical Improvement
Need for clinical evidence
Although previous studies have proved the practicality of CPBMI use, its actual medical effectiveness has not yet been established, and clinical evidence of its effectiveness is limited. Appropriate application of CPBMI to medical fields requires collection of large-scale, research-based evidence of its clinical effectiveness. Substantial reviews need to be focused on investigating the effectiveness of CPBMI. A potential confounding factor in this finding is that due to the nature of chronic diseases, simply providing encouragement to patients with these diseases may itself provide beneficial effects for CPBMI users. In other words, the beneficial effects of CPBMI may be attributable to its use to provide reminders to patients, rather than the actual use of CPBMI by these patients. However, using CPBMI for providing reminders and motivating patients was found to have similar beneficial effects, a finding that will assist in the formulation of public health strategies for improving chronic disease management and healthcare services.
Need for economic analysis
Commercialization of CPBMI requires analysis of its cost-effectiveness and assessment of its practicability and clinical benefits. The pricing of devices and applications, which will be one of the most important factors in user motivation, is anticipated to increase with the inclusion of personalized medical feedback systems within CPBMI programs. Because increased costs are a burden to not only patients but also medical teams, a compromise between CPBMI use and other alternative strategies must be sought. If saving time for doctors' feedback and providing guidelines properly inferred through a CDSS or artificial intelligence program35 can be utilized, it will consequently reduce medical costs, which are a significant factor in CPBMI.
Need for research on CDSS
The development of labor-saving autoregulation programs adaptable to each situation is also expected to prevent increases in medical expenses.35,36 After various data such as medical and family history, physical and clinical characteristics, and blood test results have been entered into them, autofeedback programs can be used to analyze the data and show diagnostic results, recommend additional tests, validate decisions, and automatically refine artificial intelligence models. To address cases in which additional information is entered or required, the means of providing feedback should be developed. Such systems could be a vital part of prevention-oriented healthcare systems aimed at identifying those at risk of developing diabetes, hypertension, and cardiovascular diseases.
Need for research into health-coordinating centers
In current healthcare systems, medical teams lack experience regarding the use of IT-based tools other than the automated prescription systems available in many hospitals. These teams must learn to use CPBMI, medical devices, and networks as part of a supportive system, as well as to provide medical feedback. The participation of medical professionals in specialized health-coordinating centers is essential to provide medical feedback effectively without discomfort to users.49 Such professionals would be responsible for responding in real time to users' requests in a specialized center that can meet their needs even when they are away from the hospital setting. To obtain successful outcomes, medical teams must collaborate with various professionals in the use of CPBMI, telecommunication devices, and other IT tools.
User Improvements
Although familiar with in-hospital medical care, patients are relatively less experienced and confident with using CPBMI. Hence, promoting patients' active and voluntary participation is very important. Besides interaction between medical providers and patients, communication among chronic disease patients is also important. Building a community among patients with the same chronic diseases and symptoms who visit the same hospital by allowing them to connect easily will yield good medical outcomes, which is the ultimate goal of CPBMI.
Conclusions
The goal of health management has transitioned from providing effective diagnosis and treatment of diseases to preventing diseases via lifestyle modifications. Meeting this new goal requires management of health and disease not only while patients are visiting the hospital but also while they are proceeding through their daily routines and are away from the hospital. Such lifestyle management will require the introduction of new medical tools, among which CPBMI-based tools appear particularly promising and important. As discussed in this article, lifestyle management is an essential component in the management of patients with chronic diseases, including HIV infection, DM, and asthma, which are either very difficult or impossible to cure. Although their potential has only begun to be investigated and much more research must be conducted into device development and use, CPBMI and IT-based health management tools are anticipated to become useful and effective components of healthcare management in the future.
Acknowledgment
This research was supported by a grant of the Korean Health Technology R&D Project, Ministry of Health and Welfare (HI13C2164), and by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIP) (2010-0028631).
Disclosure Statement
No competing financial interests exist.
References
- 1.Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, Zimmet P, Son HY. Epidemic obesity and type 2 diabetes in Asia. Lancet 2006;368:1681–1688 [DOI] [PubMed] [Google Scholar]
- 2.Chan JC, Malik V, Jia W, Kadowaki T, Yajnik CS, Yoon KH, Hu FB. Diabetes in Asia: Epidemiology, risk factors, and pathophysiology. JAMA 2009;301:2129–2140 [DOI] [PubMed] [Google Scholar]
- 3.Lawler SP, Winkler E, Reeves MM, Owen N, Graves N, Eakin EG. Multiple health behavior changes and co-variation in a telephone counseling trial. Ann Behav Med 2010;39:250–257 [DOI] [PubMed] [Google Scholar]
- 4.Reynolds NR, Testa MA, Su M, Chesney MA, Neidig JL, Frank I, Smith S, Ickovics J, Robbins GK; AIDS Clinical Trials Group 731 and 384 Teams. Telephone support to improve antiretroviral medication adherence: A multisite, randomized controlled trial. J Acquir Immune Defic Syndr 2008;47:62–68 [DOI] [PubMed] [Google Scholar]
- 5.Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academies Press, 2001 [PubMed] [Google Scholar]
- 6.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: The Chronic Care Model, part 2. JAMA 2002;288:1909–1914 [DOI] [PubMed] [Google Scholar]
- 7.Barghouthi T, Glynn F, Speaker RB, Walsh M. The use of a camera-enabled mobile phone to triage patients with nasal bone injuries. Telemed J E Health 2012;18:150–152 [DOI] [PubMed] [Google Scholar]
- 8.Perron NJ, Dao MD, Kossovsky MP, Miserez V, Chuard C, Calmy A, Gaspoz JM. Reduction of missed appointments at an urban primary care clinic: A randomised controlled study. BMC Fam Pract 2010;11:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koshy E, Car J, Majeed A Effectiveness of mobile-phone short message service (SMS) reminders for ophthalmology outpatient appointments: Observational study. BMC Ophthalmol 2008;8:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pop-Eleches C, Thirumurthy H, Habyarimana JP, Zivin JG, Goldstein MP, de Walque D, MacKeen L, Haberer J, Kimaiyo S, Sidle J, Ngare D, Bangsberg DR. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: A randomized controlled trial of text message reminders. AIDS 2011;25:825–834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lester RT, Ritvo P, Mills EJ, Kariri A, Karanja S, Chung MH, Jack W, Habyarimana J, Sadatsafavi M, Najafzadeh M, Marra CA, Estambale B, Ngugi E, Ball TB, Thabane L, Gelmon LJ, Kimani J, Ackers M, Plummer FA. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): A randomised trial. Lancet 2010;376:1838–1845 [DOI] [PubMed] [Google Scholar]
- 12.Mbuagbaw L, Thabane L, Ongolo-Zogo P, Lester RT, Mills E, Volmink J, Yondo D, Essi MJ, Bonono-Momnougui RC, Mba R, Ndongo JS, Nkoa FC, Ondoa HA. The Cameroon Mobile Phone SMS (CAMPS) trial: A protocol for a randomized controlled trial of mobile phone text messaging versus usual care for improving adherence to highly active anti-retroviral therapy. Trials 2011;12:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kalichman SC, Kalichman MO, Cherry C, Swetzes C, Amaral CM, White D, Jones M, Grebler T, Eaton L. Brief behavioral self-regulation counseling for HIV treatment adherence delivered by cell phone: An initial test of concept trial. AIDS Patient Care STDS 2011;25:303–310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seid M, D'Amico EJ, Varni JW, Munafo JK, Britto MT, Kercsmar CM, Drotar D, King EC, Darbie L. The in vivo adherence intervention for at risk adolescents with asthma: Report of a randomized pilot trial. J Pediatr Psychol 2012;37:390–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Petrie KJ, Perry K, Broadbent E, Weinman J. A text message programme designed to modify patients' illness and treatment beliefs improves self-reported adherence to asthma preventer medication. Br J Health Psychol 2012;17:74–84 [DOI] [PubMed] [Google Scholar]
- 16.Britto MT, Munafo JK, Schoettker PJ, Vockell AL, Wimberg JA, Yi MS. Pilot and feasibility test of adolescent-controlled text messaging reminders. Clin Pediatr (Phila) 2012;51:114–121 [DOI] [PubMed] [Google Scholar]
- 17.Strandbygaard U, Thomsen SF, Backer V. A daily SMS reminder increases adherence to asthma treatment: A three-month follow-up study. Respir Med 2010;104:166–171 [DOI] [PubMed] [Google Scholar]
- 18.Kim HS, Jeong HS. A nurse short message service by cellular phone in type-2 diabetic patients for six months. J Clin Nurs 2006;16:1082–1087 [DOI] [PubMed] [Google Scholar]
- 19.Bell AM, Fonda SJ, Walker MS, Schmidt V, Vigersky RA. Mobile phone-based video messages for diabetes self-care support. J Diabetes Sci Technol 2012;6:310–319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zolfaghari M, Mousavifar SA, Pedram S, Haghani H. The impact of nurse short message services and telephone follow-ups on diabetic adherence: Which one is more effective? J Clin Nurs 2012;21:1922–1931 [DOI] [PubMed] [Google Scholar]
- 21.Shetty AS, Chamukuttan S, Nanditha A, Raj RK, Ramachandran A. Reinforcement of adherence to prescription recommendations in Asian Indian diabetes patients using short message service (SMS)—A pilot study. J Assoc Physicians India 2011;59:711–714 [PubMed] [Google Scholar]
- 22.Cho JH, Lee HC, Lim DJ, Kwon HS, Yoon KH. Mobile communication using a mobile phone with a glucometer for glucose control in Type 2 patients with diabetes: As effective as an Internet-based glucose monitoring system. J Telemed Telecare 2009;15:77–82 [DOI] [PubMed] [Google Scholar]
- 23.Kim SI, Kim HS. Effectiveness of mobile and internet intervention in patients with obese type 2 diabetes. Int J Med Inform 2008;77:399–404 [DOI] [PubMed] [Google Scholar]
- 24.Kim HS, Yoo YS, Shim HS. Effects of an internet-based intervention on plasma glucose levels in patients with type 2 diabetes. J Nurs Care Qual 2006;20:335–340 [DOI] [PubMed] [Google Scholar]
- 25.Kim HS. A randomized controlled trial of a nurse short-message service by cellular phone for people with diabetes. Int J Nurs Stud 2007;44:687–692 [DOI] [PubMed] [Google Scholar]
- 26.Kim HS. Impact of Web-based nurse's education on glycosylated haemoglobin in type 2 diabetic patients. J Clin Nurs 2007;16:1361–1366 [DOI] [PubMed] [Google Scholar]
- 27.Schiel R, Thomas A, Kaps A, Bieber G. An innovative telemedical support system to measure physical activity in children and adolescents with type 1 diabetes mellitus. Exp Clin Endocrinol Diabetes 2011;119:565–568 [DOI] [PubMed] [Google Scholar]
- 28.Carroll AE, DiMeglio LA, Stein S, Marrero DG. Contracting and monitoring relationships for adolescents with type 1 diabetes: A pilot study. Diabetes Technol Ther 2011;13:543–549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Curran K, Nichols E, Xie E, Harper R. An intensive insulinotherapy mobile phone application built on artificial intelligence techniques. J Diabetes Sci Technol 2010;4:209–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Istepanian RS, Zitouni K, Harry D, Moutosammy N, Sungoor A, Tang B, Earle KA. Evaluation of a mobile phone telemonitoring system for glycaemic control in patients with diabetes. J Telemed Telecare 2009;15:125–128 [DOI] [PubMed] [Google Scholar]
- 31.Skrøvseth SO, Arsand E, Godtliebsen F, Joakimsen RM. Model driven mobile care for patients with type 1 diabetes. Stud Health Technol Inform 2012;180:1045–1049 [PubMed] [Google Scholar]
- 32.Lyles CR, Harris LT, Le T, Flowers J, Tufano J, Britt D, Hoath J, Hirsch IB, Goldberg HI, Ralston JD. Qualitative evaluation of a mobile phone and web-based collaborative care intervention for patients with type 2 diabetes. Diabetes Technol Ther 2011;13:563–569 [DOI] [PubMed] [Google Scholar]
- 33.Quinn CC, Gruber-Baldini AL, Shardell M, Weed K, Clough SS, Peeples M, Terrin M, Bronich-Hall L, Barr E, Lender D. Mobile diabetes intervention study: Testing a personalized treatment/behavioral communication intervention for blood glucose control. Contemp Clin Trials 2009;30:334–346 [DOI] [PubMed] [Google Scholar]
- 34.Nathan DM, Singer DE, Hurxthal K, Goodson JD. The clinical information value of the glycosylated hemoglobin assay. N Engl J Med 1984;310:341–346 [DOI] [PubMed] [Google Scholar]
- 35.Cho JH, Choi YH, Kim HS, Lee JH, Yoon KH. Effectiveness and safety of a glucose data-filtering system with automatic response software to reduce the physician workload in managing type 2 diabetes. J Telemed Telecare 2011;17:257–262 [DOI] [PubMed] [Google Scholar]
- 36.Mohammed KA, Seema S, Nikhil T. Review of electronic decision-support tools for diabetes care: A viable option for low- and middle-income countries? J Diabetes Sci Technol 2011;5:553–570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ryan D, Price D, Musgrave SD, Malhotra S, Lee AJ, Ayansina D, Sheikh A, Tarassenko L, Pagliari C, Pinnock H. Clinical and cost effectiveness of mobile phone supported self monitoring of asthma: Multicentre randomised controlled trial. BMJ 2012;344:e1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Prabhakaran L, Chee WY, Chua KC, Abisheganaden J, Wong WM. The use of text messaging to improve asthma control: A pilot study using the mobile phone short messaging service (SMS). J Telemed Telecare 2010;16:286–290 [DOI] [PubMed] [Google Scholar]
- 39.Liu WT, Huang CD, Wang CH, Lee KY, Lin SM, Kuo HP. A mobile telephone-based interactive self-care system improves asthma control. Eur Respir J 2011;37:310–317 [DOI] [PubMed] [Google Scholar]
- 40.Anhøj J, Møldrup C. Feasibility of collecting diary data from asthma patients through mobile phones and SMS (short message service): Response rate analysis and focus group evaluation from a pilot study. J Med Internet Res 2004;6:e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pinnock H, Slack R, Pagliari C, Price D, Sheikh A. Understanding the potential role of mobile phone-based monitoring on asthma self-management: Qualitative study. Clin Exp Allergy 2007;37:794–802 [DOI] [PubMed] [Google Scholar]
- 42.Murphy EL, Collier AC, Kalish LA, Assmann SF, Para MF, Flanigan TP, Kumar PN, Mintz L, Wallach FR, Nemo GJ. Highly active antiretroviral therapy decreases mortality and morbidity in patients with advanced HIV disease. Ann Intern Med 2001;135:17–26 [DOI] [PubMed] [Google Scholar]
- 43.Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, Wagener MM, Singh N. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med 2000;133:21–30 [DOI] [PubMed] [Google Scholar]
- 44.da Costa TM, Barbosa BJ, Gomes e Costa DA, Sigulem D, de Fátima Marin H, Filho AC, Pisa IT. Results of a randomized controlled trial to assess the effects of a mobile SMS-based intervention on treatment adherence in HIV/AIDS-infected Brazilian women and impressions and satisfaction with respect to incoming messages. Int J Med Inform 2012;81:257–269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bradley J, Ramesh BM, Rajaram S, Lobo A, Gurav K, Isac S, Chandra Shekhar Gowda G, Pushpalatha R, Moses S, Sunil KD, Alary M. The feasibility of using mobile phone technology for sexual behaviour research in a population vulnerable to HIV: A prospective survey with female sex workers in South India. AIDS Care 2012;24:695–703 [DOI] [PubMed] [Google Scholar]
- 46.Hardy H, Kumar V, Doros G, Farmer E, Drainoni ML, Rybin D, Myung D, Jackson J, Backman E, Stanic A, Skolnik PR. Randomized controlled trial of a personalized cellular phone reminder system to enhance adherence to antiretroviral therapy. AIDS Patient Care STDS 2011;25:153–161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cho JH, Kim HS, Han JH, Lee JH, Oh JA, Choi YH, Yoon KH. Ubiquitous diabetes management system via interactive communication based on information technologies: Clinical effects and perspectives. Korean Diabetes J 2010;34:267–274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lim S, Kim SY, Kim JI, Kwon MK, Min SJ, Yoo SY, Kang SM, Kim HI, Jung HS, Park KS, Ryu JO, Shin H, Jang HC. A survey on ubiquitous healthcare service demand among diabetic patients. Diabetes Metab J 2011;35:50–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kim HS, Shin JA, Chang JS, Cho JH, Son HY, Yoon KH. Continuous glucose monitoring: Current clinical use. Diabetes Metab Res Rev 2012;28(Suppl 2):73–78 [DOI] [PubMed] [Google Scholar]