Abstract
Background: Although telehealth is a promising solution for healthcare professionals who work in remote and rural regions, the influence of specific telehealth applications on the nursing workforce remains unknown. This case study aimed to explore the potential influence of a teleassistance service in wound care (the acronym in French is TASP) on nursing practices and on nurse retention in peripheral areas. Materials and Methods: We carried out an exploratory single case study based on 16 semistructured interviews with two promoters of TASP, five nursing managers, and nine nurses from three levels of expertise associated with this service. Results: According to participants, the main positive influences of TASP were observed in quality of care, professional autonomy, professional development, and decrease of professional isolation. Participants mentioned increased workload associated with global patient data collection at first consultation as a negative effect of TASP. Finally, three possible effects of TASP on nurse retention were identified: none or minimal, imprecise, or mostly positive. Conclusions: This case study highlights the positive influence of TASP on several dimensions of nursing practice, in addition to its essential role in improving the quality of care. However, it is important to consider that the service cannot be considered as a solution to or replacement for the shortage of nurses.
Key words: : information and communication technologies, nursing practice, nurse retention, wound care, home health monitoring, telemedicine
Introduction
In view of the predicted nursing shortage and its effects on healthcare,1 recruitment and retention of nurses remain serious challenges for Canadian decision makers.2 Indeed, 22,000 nurses are lacking, and a shortfall of 60,000 full-time equivalent nurses is expected by 2022.3 Other barriers to retention of nurses are factors associated with workload such as overtime, understaffing, turnover, or absenteeism.4
The situation is more acute in remote and rural communities. In developing and developed countries, equitable access to appropriate healthcare in these areas is undermined by shortage and misdistribution of nurses and the health workforce.5–7 Rural and remote Canada is not an exception. Dissatisfaction with work schedules,8,9 lower community satisfaction,8 lack of opportunity to maintain skills,9 and an aging workforce closer to retirement10 are some issues that exert downward pressure on the working conditions of nurses.
Telehealth has been proposed as a strategy to support clinical practice and improve knowledge and skills of healthcare professionals in rural and remote areas.7,11 Some studies have analyzed the influence of telehealth on workforce recruitment and retention factors,12–16 but few studies have addressed the influence of telehealth on nursing practice, particularly with respect to nurse recruitment and retention factors.17–21
Thus, we initiated a project, in collaboration with decision makers, entitled “Supporting Work Practices Through Telehealth: Impact on Nurses in Outlying Regions.”22 Our objective was to document nurses' perceptions regarding the influence of information and communication technologies (ICT), including telehealth, on their practice and, eventually, on their recruitment and retention in remote or outlying regions. In the first phase of the project, we achieved an overall picture of ICT influences on clinical practice and retention of nursing staff from a nursing management viewpoint.23 In the second phase of the project, we used case studies to determine the main effects of the introduction of specific ICT applications on factors associated with retention of nurses in remote and outlying regions.
The purpose of this article is to share the results of our case study of a telehealth application in the province of Quebec, Canada, known as “wound care teleassistance” (the acronym in French is TASP), especially regarding its influences on nursing professional practice, recruitment, and retention. TASP is one of the few telehealth projects that have entered current healthcare services in Quebec. It offers an opportunity to better understand the challenges for nurses to integrate this service into their clinical practice and its potential influence on their recruitment and retention.
TASP Service
Telemedicine in wound care has been reviewed and documented in various countries.24 Most of these studies focused on physicians. A study in the United States measured their attitudes toward telemedicine and their satisfaction with using this application in wound care.25 In The Netherlands, a study focused on the integration and routine use of telemedicine in wound care by general practitioners.26 In other studies conducted in Switzerland27 and Mexico,28 the issue was on physician evaluation of chronic wound images taken using a mobile telephone. Other studies have examined the influence of this telemedicine application on nurse practices in homecare29 or in various healthcare facilities.30,31 All highlighted the lack of wound care specialists in rural or remote areas, which might force patients to travel long distances to obtain treatment. Some issues raised in these studies were related to acceptance29 and implementation30,31 of telemedicine in wound care.
The application studied here, TASP, is distinct from those covered in previous studies. It is an operational service made by and for the nurses in wound care, a field under the responsibility of nurses in Quebec, according to Section 36 of the Nurses Act.32 Established as a project in 2008, TASP was offered to patients in remote or rural areas lacking nurse expertise in wound care. Now this service, free of charge for all Quebec residents within the Health Insurance Plan of Quebec (the acronym in French is RAMQ), is deployed in 65 healthcare centers of the Integrated University Healthcare Network (the acronym in French is RUIS) of the University of Sherbrooke, mainly in local community service centers (the acronym in French is CLSC) and residential and long-term care centers (the acronym in French is CHSLD). No homecare services were implemented at the time of this study.
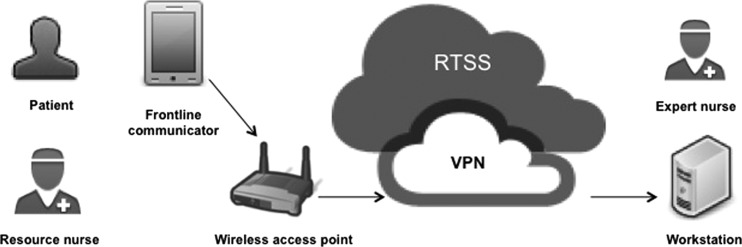
TASP uses a wireless technology, which is an audiovisual communication system that has the capacity for asynchronous or synchronous electronic voice and image transfer. In a facility, a nurse records a patient's wound with a mobile video developed by Audisoft, a commercial provider of mobile communication systems. At the same time, in another facility, an expert nurse observes the wound on his or her computer screen. All data are transmitted via a secure connection. The legend in Figure 1 provides more details on the telemedicine wound care system.
Fig. 1.
The wound care teleassistance system. The resource nurse processes the virtual clinic with the “Frontline Communicator,” the mobile telecommunication device of the wound care teleassistance system. It includes two software applications: (1) “Frontline PDA,” which ensures real-time transmission of data from the mobile device to distant workstations; and (2) “Efon VCN,” which allows connection of the mobile device to a secure network for remote support. Audiovisual communication between the resource nurse and his or her patient can only be seen by the expert nurse with the virtual private network (VPN) of the wound care teleassistance service. This VPN is part of a secure network of the Ministry of Health and Social Services known as the Health Services Telecommunications Network (the acronym in French is RTSS). The expert nurse assesses the resource nurse with his or her computer workstation, which includes two software applications: (1) “Frontline PC,” which allows the reception of audiovisual communication from the frontline personal digital assistant (PDA); and (2) “Real VCN,” which allows the workstation to provide remote support via the RTSS network.
This service relies on the involvement of approximately 4,000 nurses in the RUIS territory. These nurses are distributed among three levels of expertise. Twelve are expert nurses, approximately 80 are resource nurses, and the rest are bedside nurses. The expert nurse is an enterostomal therapy nurse or a nurse with strong knowledge and experience in complex wound care. From a hub healthcare organization, he or she brings management support and ongoing training to a resource nurse and his or her patient in a remote location. The resource nurse, a full-time bedside nurse interested in improving his or her skill in wound care, initially evaluates the global health of the patient and contacts the expert nurse for a virtual session. Both nurses can initiate live or deferred clinical exchanges. The number of sessions varies depending on the extent of the wound. The bedside nurse is a nurse who provides direct care to his or her patient and can assist the resource nurse in virtual clinic sessions.
Materials and Methods
The researchers of the team (M.-P.G., E.B., F.C., G.P., and J.C.) used a participatory approach involving the Telehealth Coordination Center (TCC) of the RUIS of the University of Sherbrooke and five Nursing Departments of healthcare organizations involved in TASP. This collaboration aimed to promote cooperation and mutual respect between researchers and nurses involved in TASP. As this study was descriptive and exploratory in nature, we were mainly interested in documenting the effects of TASP on factors related to clinical practice and retention of nursing staff.
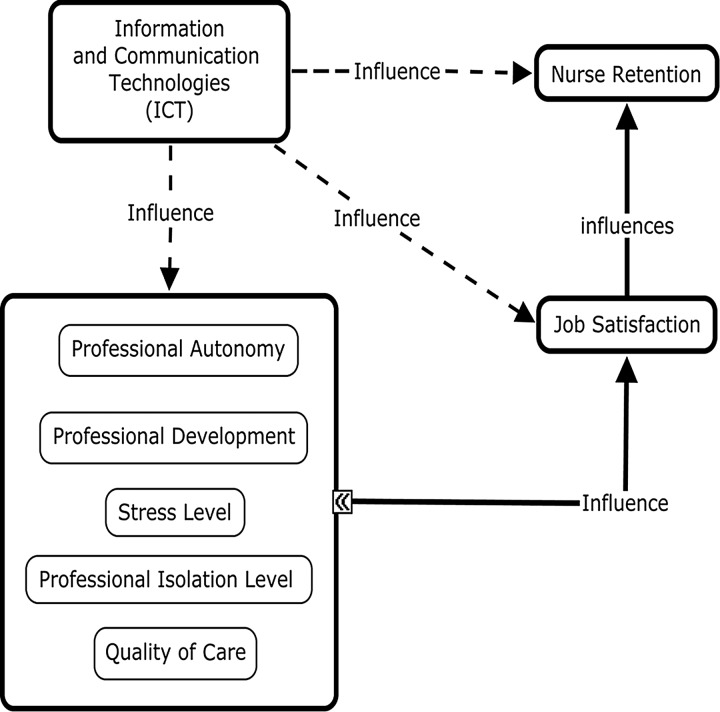
We used a conceptual map developed during the first phase of our research by four members of our team (M.-P.G., F.C., G.P., and J.C.), illustrating the influence of ICT on the retention of healthcare professionals. This influence constitutes our research proposal, adapted for the nursing community. It is inspired by local12–14 and international16 studies, as well as a systematic review on the impact of ICT on the recruitment and retention of the healthcare workforce.15
Based on the premise that job satisfaction is an important dimension in nurse retention,33–35 we propose in this conceptual map (Fig. 2) a set of factors affecting nurse job satisfaction, including professional autonomy,36 professional development,37,38 feeling of professional isolation,35 level of stress,33 and quality of care.35 These factors were chosen because they could potentially be influenced by ICT and thus act as key levers on nurse retention through their mediation effect on job satisfaction.
Fig. 2.
Conceptual map illustrating the influence of information and communication technologies (ICT) on nurse retention. Dotted lines signify the research proposal about potential influence of ICT on retention of nurses. Continuous lines indicate factors of nurse retention based on literature review.
Six healthcare organizations with operational TASP from two regions with different areas (rural or urban) were initially invited. This selection allowed us to explore the influence of this service in nursing practices from various settings.
We favored a purpose-based sampling in the final selection of participants, based on the role of the nurses in the service (Table 1). The Principal Investigator (M.-P.G.) made an initial contact with each TCC to obtain the center's point of view as the promoter of TASP. Then, a member of the TCC (S.Q.) made contacts with Nursing Departments of four healthcare organizations using TASP. One of them declined because of recent changes at the head of its Nursing Department. Later a member of the research team (E.B.) contacted two other Nursing Departments in rural areas. In all case, information leaflets were sent to the managers of each Nursing Department, inviting them to participate in the study. They consulted the nurses working in the service and provided a list of those interested in participating in the interviews.
Table 1.
Roles of Participants
| ROLE | PARTICIPANTS | N |
|---|---|---|
| Expert nurse | P6*, P9* | 2 |
| Resource nurse | P7*, P12*, P14*, P15*, P16* | 5 |
| Bedside nurse | P8, P13 | 2 |
| Director of nursing | P4, P10 | 2 |
| Director of nursing and local responsible | P2 | 1 |
| Local responsible | P5, P11 | 2 |
| Promoters | P1, P3 | 2 |
| Total | 16 | |
An asterisk indicates a first-hand participation in wound care teleassistance to the patient.
The study was approved by the ethics committees of the participating organizations. A consent form was presented and explained to each participant, as well as his or her opportunity to withdraw at any time, without prejudice. All participants previously gave their free and informed consent.
In total, 16 semistructured interviews (12 face-to-face and 4 by telephone) were conducted between April 23 and October 2, 2012. All participants were interviewed individually. Four researchers (M.-P.G., E.B., F.C., and G.P.), who were not involved in the tele–wound care service, conducted the interviews. The interview questions focused on the influence of the telemedicine wound care service on nurse practices and on the retention of nurses. The average length of each interview was 44 min, producing a total of 254 pages of transcripts. All participants received transcripts of their interviews in verbatim form for validation purposes.
We carried out data analysis with the support of NVivo 9 software (QSR International, Warrington, United Kingdom), according to the method described by Miles and Huberman,39 which enabled us to identify themes and relationships between themes in the interviews through the construction of matrices. Once the interviews transcribed in verbatim form, a member of the team research (E.B.) performed an initial codification and proposed a code tree to the research teams. Two members of the research team (M.-P.G. and E.B.) independently carried out the final process of codification. The research team established a consensus when thematic codes required adjustments. The codification was based on our conceptual map and from the emerging themes from the interviews and the vision of the participants. We sent a preliminary report to the TCC, which diffused it to the healthcare organizations in order to validate the content of this research.
Results
Description of Participants
Sixteen nurses participated in the study: two TASP promoters (both nurses) who collaborated to implement this service on the RUIS territory and members of the TCC, five members of three Nursing Departments (of which three were responsible of the service in their facilities), and nine nurses representing the three levels of expertise associated with this service (Table 1).
Among these participants, seven were providing a first-hand service at the time of the study (all the expert and resource nurses). One bedside nurse had some experience in assisting the resource nurse at her facility. Other bedside nurses had not assisted in a virtual session but had observed significant changes in their workplace after the implementation of the service.
Influences of TASP on Nursing Practice
During the interviews, participants drew a picture of the influence of the TASP service on six dimensions of nursing practice (Table 2). We present these dimensions and their most significant aspects.
Table 2.
Influences of the Wound Care Teleassistance System on Nursing Practice
| DIMENSION AND THEMES | PARTICIPANTS | N |
|---|---|---|
| Quality of care | ||
| Interdisciplinary work (+) | P1, P2, P3, P5, P6*, P7*, P9*, P11, P13, P14*, P15*, P16* | 12 |
| Accessibility (+) | P2, P3, P5, P6*, P9*, P10, P11, P13, P14*, P15*, P16* | 11 |
| Development of nursing expertise in wound care (+) | P3, P4, P5, P6,* P7*, P9*, P10, P11, P13, P14*, P15* | 11 |
| Overall improvement of quality of care (+) | P3, P6*, P9*, P10, P12*, P13, P14*, P15*, P16* | 9 |
| Standardization (+) | P1, P2, P4, P5, P7*, P9, P11, P12*, P13 | 9 |
| Patient monitoring (+) | P6*, P9*, P10, P11, P13, P14*, P15*, P16* | 8 |
| Quality of communication with patients (+) | P3, P6*, P9*, P13 | 4 |
| Patient involvement in healing process (+) | P3, P6*, P7* | 3 |
| Professional development | ||
| Promotion of knowledge transfer (+) | P2, P3, P5, P6*, P7*, P8, P9*, P11, P12*, P13, P14*, P15*, P16* | 13 |
| Promotion of knowledge sharing (+) | P5, P6*, P7*, P9*, P12*, P14* | 6 |
| Professional isolation | ||
| Mutual aid (+) | P2, P3, P5, P7*, P8, P9*, P10, P12*, P13, P14*, P15*, P16* | 12 |
| Job satisfaction | ||
| Appreciation by nurses of their role (+) | P5, P6*, P7, P10, P11 | 5 |
| External recognition of wound care expertise (+) | P5, P7, P8 | 3 |
| Overall satisfaction with the service (+) | P14*, P16* | 2 |
| Stress level | ||
| The service secures nurses' work (+) | P6*, P9*, P15* | 3 |
| Stress is temporary and confined to specific situations (+) | P7*, P8, P9* | 3 |
| No stress (+) | P9* | 1 |
| Workload | ||
| Substantial time spent by resource nurses on the global data collection of patients (–) | P3, P6*, P7*, P8, P14*, P15*, P16* | 7 |
| Reducing calls and travels (+) | P1, P3, P5, P9* | 4 |
| Substantial time spent by expert nurses on digitized and written reports on virtual clinic sessions (–) | P9*, P15* | 2 |
The plus and minus signs indicate positive and negative influences of the wound care teleassistance system, respectively. An asterisk indicates a first-hand participation in wound care teleassistance to the patient.
A positive influence on the quality of care
The majority of participants highlighted a positive influence of TASP on many aspects of quality of care. We outline the following: accessibility, standardization of clinical practice, interdisciplinary work, and patient–nurse relations. This service offered a greater accessibility, both geographically (proximity of the service in the patient's community, simultaneous access to specialized resources) and temporally (reduced wait times, prompt access to medical products). Some participants specifically pointed out the reduction of travel for nurses and patients, especially to the hospitals. A resource nurse from a small community illustrated it as follows: “I think it is a good technology. This is a new and wonderful service for our patients…It even reduces congestion in the emergency room. That's for sure. If someone comes here with a wound, there's no need to go to the emergency room.”
Another significant contribution of TASP to the quality of care is the standardization of clinical practice. Its benefits were the use of a clear and common language among participants, which reassured the patient, and a potential source of savings in the management of wound care products. A majority of participants also recognized a shared nursing expertise in wound care that was not limited to expert nurses. In particular, the resource nurse—through her ability to do an overall assessment of the patient—updated her knowledge in wound care. Indirectly, the bedside nurse could benefit from new skills by consulting notes or receiving instructions from the resource nurse.
The interdisciplinary work between nurses and other specialists was positive but still in its early stages. According to the situation and the level of expertise, nurses had the opportunity to work with the patient's physician or other healthcare professionals. Although some participants mentioned an improved general collaboration between nurses and physicians, others qualified the scope of this interdisciplinary work: according to the setting, some physicians worked more easily with the expert nurse than with nurses with lesser levels of expertise.
The patient–nurse relation is another dimension of quality of care that emerged from interviews. Although the resource nurse and the patient cannot see the expert nurse on a screen, it is not considered as an obstacle to human and professional communication during virtual clinics. As a nurse expert stated: “The dynamic is often the same and also cordial. We try to be sensitive, like a family who is working for the patient. Yes, a team. It isn't cold. It's never cold…because it's not obvious for the patient to be in front of a camera and not seeing the interlocutor on the other side. We need a warm hearted session.” Other significant positive effects of TASP on quality of care are indicated in Table 2.
Professional development oriented toward knowledge transfer
Professional development was an important objective of the TASP service. This theme is reflected in participants' comments under the themes of knowledge transfer and sharing.
Knowledge transfer took place with resource nurses and, to a lesser extent, bedside nurses during virtual clinical sessions with the expert nurse. Resource nurses had the opportunity to update their knowledge of the types of wound dressings and other products (e.g., ointments, gels) for treatment, to better describe their evolution, and to develop new techniques of treatment. Bedside nurses were unable to attend the virtual clinic meetings because of their daily workload and staff shortages. However, they had the opportunity to consult resource nurses directly or indirectly, through their sharing of working notes, outside these meetings.
On the other hand, knowledge transfer was closely linked to the rise of professional autonomy. As summarized by a Nursing Department representative: “Currently, the expert nurse helps to guide nurses. She asks: ‘Why did you do it that way?’ They must be more and more autonomous.” Expert nurses promoted autonomy of their colleagues with a nondirective approach stimulating their clinical judgement. Resource nurses perceived more autonomy with the gradual reduction of the need to validate their treatment plan with expert nurses. For bedside nurses, this autonomy was manifest by having access to information regarding the prevention of wounds.
Finally, TASP was seen as a lever for nurses to share knowledge by joining committees, communities of practice, conferences, and discussion groups. As an expert nurse narrated: “We have a solid network between expert nurses. We meet at least two or three times a year, because nursing and medical practices may differ from one region to another even if we have a common framework. So we share a lot of information.”
Decreased professional isolation through mutual aid
During the interviews, several participants mentioned a reduction of the feeling of professional isolation among nurses. Virtual clinics have encouraged mutual support between levels of expertise: between the expert nurse and the resource nurse, between the resource nurse and the bedside nurse, between the three levels of expertise, and among resource nurses. Additionally, the service helped to break the isolation of resource nurses working in rural areas. As an expert nurse highlighted: “Nursing staff in remote areas felt alone, helpless…and isolated in terms of clinical support and expertise. Teleassistance solved this.”
Influence on job satisfaction
Several participants commented the influence of TASP on job satisfaction. Most of them observed an enhancement of nurses' role in their practice. As explained by a Nursing Department representative: “It's positive because [TASP] enhances nurses. It enhances them in their role.” A resource nurse added: “For me, I think it's rewarding. And when we're valued, we want to go on.” An expert nurse also highlighted patients' recognition of their work: “There is a gentleman who wrote in our local newspaper about our good care!”
Perceived stress and workload
In general, the TASP service secured the work of resource nurses in terms of clinical support. When resource nurses talked about stress, it was restricted to specific times or particular activities, especially during the initial familiarization period with the service or with related technologies or during the development of a training session.
However, several participants mentioned work overload among resource nurses, especially during the initial patient data collection. This activity was considered laborious because of the difficult access to patient records, the requirement to obtain the consent of relatives, and some constraints to reconcile this role with ongoing tasks. Moreover, the perception of work overload among expert nurses remains an open question. On one hand, the service allowed them to reduce travel time through the territory and to remain at their workplace. On the other hand, an expert nurse spent more time writing reports of virtual clinical sessions: “Me, even if it's only assistance, l must write a report in the computer…And this is lengthy…So, I must write a full consultation, a request for service in the computer. So, it's an average of one hour per patient.”
Potential influence on recruitment and retention
During the interviews, we explored the influence of TASP on nurse recruitment and retention. Few participants commented about recruitment, and their opinions remained divided and diverse. An expert nurse evaluated this complex situation of recruitment: “We are…in a time of nurse shortage. And we would like a resource nurse dedicated to teleassistance and wound care in her workplace. Unfortunately, they can't and the Administration can't provide that.…”
On the other hand, the potential influence of TASP on nurse retention was commented on more by participants. Their comments reflected three types of perceived effects of the TASP service on nurse retention (Table 3).
Table 3.
Influences of the Wound Care Teleassistance System on Nurses' Recruitment and Retention
| RESPONSE | RECRUITMENT | RETENTION |
|---|---|---|
| Little or no influence | P9*, P10 | P10, P11, P12*, P13, P14*, P15* |
| Undecided | P9*, P11 | P6* |
| Positive influence | P9*, P6* | P3, P5, P7*, P8, P9*, P12, P16* |
An asterisk indicates a first-hand participation in wound care teleassistance to the patient.
The first is the lack or little effect of TASP on nurse retention. The main reasons are the following: the recent implementation of the service; the insufficient number of nurses, particularly bedside nurses, working in the service, and the fact that it is not an incentive to remain in a particular organization. As a resource nurse from a small community pointed out: “Retention, I think is a big word. Of course, if you're more satisfied, if you have more answers to your questions, it's beneficial. But it would be wrong to say that it will keep nurses here.”
The second type of effect is the imprecise direction of TASP's influence. In one organization, a participant was reluctant to affirm that the service directly influenced retention of nurses despite clear benefits such as the acquisition and transfer of knowledge, greater autonomy, and an increased feeling of security.
Finally, the third type of perceived effect is positive. Some participants believed that the TASP service contributed to retention by being associated with one of the following aspects of nursing practice: learning, development of expertise, enhancement of the resource nurse's role, quality of care, and the new generation of nurses familiarized with ICT.
Discussion
In this study, we sought to explore and document the influence of a teleassistance service in wound care on nursing practice, as well as on the recruitment and retention of nurses in a regional health university network in the Province of Quebec. Using a conceptual map derived from the literature and the first phase of our research, we conducted a series of interviews with participants from five healthcare organizations.
Wound care through telehealth can be included as a particular modality of teledermatology,24,29 which is one of the most studied speciality areas in telemedicine.40 Although studies in teledermatology analyzed wound care from the perspective of the enhancement of quality of care24,31,41 or patient satisfaction,42 few noted their influence on nursing practice.29–31 Although the results of this case study cannot be generalized outside or even inside the Canadian health system, they can be used as a comparative basis to explore and reffine our conceptual map about the influence of telehealth on factors associated with nurse satisfaction and, eventually, their retention.
In general, the influence of the TASP service on nursing practice is perceived positively and remains consistent with the original objectives of the project. We also observe the importance given to the influence of telehealth on professional development, thus being in agreement with a systematic review of the use of telehealth (in this case videoconferencing) for educational purposes with physicians and nurses in remote areas.43 A study of an application similar to TASP also stresses this type of benefits.31 At first glance, resource nurses can benefit from knowledge transfer realized by expert nurses.
On the other hand, unlike previous research,23 the theme of professional autonomy was subsumed within professional development. Resource nurses could raise their autonomy through knowledge transfer from expert nurses. This association between transfer of knowledge and professional autonomy demonstrated a form of acceptance of the service by nurses. Technologies that might limit professional autonomy can provoke resistance among users.44
Participants also pointed out several benefits of the TASP service associated with quality of care. One of the benefits identified in studies of similar applications is the reduced travel of patients to hospitals, which promotes time and cost savings.24,28,29,31 Another benefit highlighted in this case study is the ability to establish a good audio and visual communication between nurse and patient, which is also documented in a study evaluating an application for remote wound care consultation.31 This last point illustrates that this technology does not constitute a barrier to the presence of dynamic interactions between the expert nurse, her colleagues, and patients. Similarly, expert nurses have developed communicative skills through the TASP, thereby constituting a core competency to telehealth.45 Finally, the perception that this service contributes to a significant improvement in wound healing is consistent with other studies.24,29
Additionally, this case study helps to highlight some dimensions unexplored in the literature regarding this kind of telehealth application. This is particularly the case with the impact of TASP on reducing professional isolation, which is manifested by an increased mutual assistance among nurses of different levels of expertise, and even for those who cannot directly attend the virtual clinics.
To a lesser extent, the TASP service is perceived as influencing job satisfaction, stress level, and workload. The influence of TASP on job satisfaction is manifested through the pride of having developed an expertise in wound care in nursing, as reported by some participants. Although stress is time-limited and circumscribed by familiarization with the technology, there are indications that some activities, particularly in connection with the preliminary phase of data collection, could result in work overload among resource nurses.
The TASP service helps to support clinical nurses. However, participants remain cautious about the impact of this service on the recruitment and retention of nurses. Few mentioned the theme of recruitment, illustrating that the service, although gradually deployed since 2009, does not play a major influence in the decision of a nurse to work in a given organization. With respect to retention, we observed different perceptions of participants, similar to those observed in the first phase of our research. Indeed, in a study conducted among nursing managers from 16 healthcare organizations in the Province of Quebec,23 we found limited support for a direct influence of ICT on nurse recruitment and retention. However, unlike previous research, we observed a greater enthusiasm among participants who emphasized positive effects of the service on retention. Although there is a common and widespread acceptance of TASP as a tool to support nursing practice in wound care, opinions were divided about its potential to promote retention of nursing staff.
This study has some limitations that must be considered. First, we have not addressed the factors facilitating or impeding the use of TASP in this study, which would deserve particular attention and could provide further information about this service. In addition, by focusing on the current use of the TASP service, we did not elaborate on its earlier operational phases (promotion and implantation). The fact that a manager of the TCC invited Nursing Departments to select nurses for participating in this study could introduce a source of bias. They could have suggested participants with a more positive opinion of the service. Meanwhile, the diversity of participants (managers and nurses from the three levels of expertise) and healthcare organizations involved provides us with instructive, diversified, and complex narratives of TASP. The best example is the lack of consensus about the influence of TASP in nurse retention. Finally, in spite of the previous identification of key groups of participants involved in TASP, it appeared in the coding and analysis of data that a group of stakeholders was omitted. These are head nurses, who directly supervise and coordinate the work of nursing staff. It would be appropriate to explore in a subsequent study their perceptions on the present issues and other implications of TASP on their management responsibilities, such as the time allocated by head nurses to exercise their supervisory role within this service.
Conclusions
This case study has contributed to point out the positive influence of a teleassistance service in wound care on several dimensions of nursing practice, in addition to its essential role in improving the quality of care. However, it is important to consider some adverse effects, especially a possible work overload associated with the deployment of this service. Although its influence on nurse recruitment and retention appears limited, a service based on information and communication technologies such as TASP could be an important tool to support nursing practice.
Acknowledgments
This research is funded by the Canadian Institutes of Health Research, in collaboration with the Ministry of Health and Social Services of Quebec through the program Partnerships for Health System Improvement (grant 200911PHE-CFBA-217005-PHE-11114). The authors wish to thank the participants who contributed to this research. They also would like to thank Anne Bernard Desrosiers who participated in data collection, as well as Geneviève Schoeb and Martin Larrivée for verbatim transcription of the interviews.
Disclosure Statement
No competing financial interests exist.
References
- 1.Murphy GT, Birch S, Alder R, et al. . Tested solutions for eliminating Canada's registered nurse shortage. Available at www.nursesunions.ca/sites/default/files/rn_shortage_report_e.pdf (last accessed July17, 2013)
- 2.Law S, Flood C, Gagnon D. Listening for direction III: National consultation on health services and policy issues 2007–2010: Final report. Available at www.cfhi-fcass.ca/Libraries/Listening_for_Direction/LfDIII-FINAL_ENG.sflb.ashx (last accessed July17, 2013)
- 3.Canadian Federation of Nurses Unions. Nursing workforce backgrounder. Available at www.nursesunions.ca/sites/default/files/2013.backgrounder.nursing_workforce.e.pdf (last accessed July17, 2013)
- 4.O'Brien-Pallas L, Hayes L. Challenges in getting workforce research in nursing used for decision-making in policy and practice: A Canadian perspective. J Clin Nurs 2008;17:3338–3346 [DOI] [PubMed] [Google Scholar]
- 5.Humphreys JS. Key considerations in delivering appropriate and accessible health care for rural and remote populations: Discussant overview. Aust J Rural Health 2009;17:34–38 [DOI] [PubMed] [Google Scholar]
- 6.Dolea C, Stormont L, Braichet JM. Evaluated strategies to increase attraction and retention of health workers in remote and rural areas. Bull World Health Organ 2010;88:379–385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. Increasing access to health workers in remote and rural areas through improved retention. 2010. Available at http://whqlibdoc.who.int/publications/2010/9789241564014_eng.pdf (last accessed July17, 2013) [PubMed]
- 8.Stewart NJ, D'Arcy C, Kosteniuk J, et al. . Moving on? Predictors of intent to leave among rural and remote RNs in Canada. J Rural Health 2011;27:103–113 [DOI] [PubMed] [Google Scholar]
- 9.Hunsberger M, Baumann A, Blythe J, Crea M. Sustaining the rural workforce: Nursing perspectives on worklife challenges. J Rural Health 2009;25:17–25 [DOI] [PubMed] [Google Scholar]
- 10.Montour A, Baumann A, Blythe J, Hunsberger M. The changing nature of nursing work in rural and small community hospitals. Rural Remote Health 2009;9:1089. [PubMed] [Google Scholar]
- 11.De Roodenbeke E, Lucas S, Rouzaut E, Bana F. Outreach services as a strategy to increase access to health workers in remote and rural areas. 2011. Available at http://whqlibdoc.who.int/publications/2011/9789241501514_eng.pdf (last accessed July17, 2013) [PubMed]
- 12.Duplantie J, Gagnon MP, Fortin JP, Landry R. Telehealth and the recruitment and retention of physicians in rural and remote regions: A Delphi study. Can J Rural Med 2007;12:30–36 [PubMed] [Google Scholar]
- 13.Fortin JP, Landry R, Gagnon MP, et al. . La télésanté: Une stratégie pour soutenir la pratique des médecins en régions éloignées. Ottawa: Fondation Canadienne de la Recherche sur les Services de Santé, 2006 [Google Scholar]
- 14.Gagnon MP, Duplantie J, Fortin JP, Landry R. Exploring the effects of telehealth on medical human resources supply: A qualitative case study in remote regions. BMC Health Serv Res 2007;7:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gagnon MP, Pollender H, Trepanier A, et al. . Supporting health professionals through information and communication technologies: A systematic review of the effects of information and communication technologies on recruitment and retention. Telemed J E Health 2011;17:269–274 [DOI] [PubMed] [Google Scholar]
- 16.Moffatt JJ, Eley DS. The reported benefits of telehealth for rural Australians. Aust Health Rev 2010;34:276–281 [DOI] [PubMed] [Google Scholar]
- 17.Sanner T. Using telehealth to address the nursing shortage. Home Healthc Nurse 2004;22:695–699 [DOI] [PubMed] [Google Scholar]
- 18.Sharman Z. Nursing technologies? Gender, care, and skill in the use of patient care information systems. In: Balka E, Green E, Henwood F, eds. Gender, health and information technology in context. Hampshire, United Kingdom: Palgrave Macmillan, 2009:88–103 [Google Scholar]
- 19.Simpson RL. From tele-ed to telehealth: The need for IT ubiquity in nursing. Nurs Adm Q 2005;29:344–348 [DOI] [PubMed] [Google Scholar]
- 20.Trepanier A, Gagnon MP, Mbemba GI, et al. . Factors associated with intended and effective settlement of nursing students and newly graduated nurses in a rural setting after graduation: A mixed-methods review. Int J Nurs Stud 2013;50:314–325 [DOI] [PubMed] [Google Scholar]
- 21.Williams M. Rural professional isolation: An integrative review. Online J Rural Nurs Health Care 2012;12:3–10 [Google Scholar]
- 22.Gagnon MP, Paré G, Pollender H, et al. . Supporting work practices through telehealth: Impact on nurses in peripheral regions. BMC Health Serv Res 2011;11:27–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gagnon MP, Breton E, Paré G, et al. . L'influence des technologies de l'information et des communications sur le maintien en poste des infirmières. Sante Publique 2013;25:305–313 [PubMed] [Google Scholar]
- 24.Chanussot-Deprez C, Contreras-Ruiz J. Telemedicine in wound care: A review. Adv Skin Wound Care 2013;26:78–82 [DOI] [PubMed] [Google Scholar]
- 25.Dobke MK, Bhavsar D, Herrera F. Do telemedicine wound care specialist consults meet the needs of the referring physician? A survey of primary care providers. Int J Telemed Appl 2011;2011:321376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van der Heijden JP, de Keizer NF, Bos JD, et al. . Teledermatology applied following patient selection by general practitioners in daily practice improves efficiency and quality of care at lower cost. Br J Dermatol 2011;165:1058–1065 [DOI] [PubMed] [Google Scholar]
- 27.Braun RP, Vecchietti JL, Thomas L, et al. . Telemedical wound care using a new generation of mobile telephones: A feasibility study. Arch Dermatol 2005;141:254–258 [DOI] [PubMed] [Google Scholar]
- 28.Chanussot-Deprez C, Contreras-Ruiz J. Telemedicine in wound care. Int Wound J 2008;5:651–654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hofmann-Wellenhof R, Salmhofer W, Binder B, et al. . Feasibility and acceptance of telemedicine for wound care in patients with chronic leg ulcers. J Telemed Telecare 2006;12(Suppl 1):15–17 [DOI] [PubMed] [Google Scholar]
- 30.Barrett M, Larson A, Carville K, Ellis I. Challenges faced in implementation of a telehealth enabled chronic wound care system. Rural Remote Health 2009;9:1154. [PubMed] [Google Scholar]
- 31.Clegg A, Brown T, Engels D, et al. . Telemedicine in a rural community hospital for remote wound care consultations. J Wound Ostomy Continence Nurs 2011;38:301–304 [DOI] [PubMed] [Google Scholar]
- 32.Gouvernement du Québec. Nurses Act. Available at http://www2.publicationsduquebec.gouv.qc.ca/dynamicSearch/telecharge.php?type=2&file=/I_8/I8_A.html (last accessed September19, 2013)
- 33.Coomber B, Barriball KL. Impact of job satisfaction components on intent to leave and turnover for hospital-based nurses: A review of the research literature. Int J Nurs Stud 2007;44:297–314 [DOI] [PubMed] [Google Scholar]
- 34.Molinari DL, Monserud MA. Rural nurse job satisfaction. Rural Remote Health 2008;8:1055. [PubMed] [Google Scholar]
- 35.Hayes B, Bonner A, Pryor J. Factors contributing to nurse job satisfaction in the acute hospital setting: A review of recent literature. J Nurs Manag 2010;18:804–814 [DOI] [PubMed] [Google Scholar]
- 36.Krebs JP, Madigan EA, Tullai-McGuinness S. The rural nurse work environment and structural empowerment. Policy Polit Nurs Pract 2008;9:28–39 [DOI] [PubMed] [Google Scholar]
- 37.MacLeod ML, Kulig JC, Stewart NJ, et al. . The nature of nursing practice in rural and remote Canada. Can Nurse 2004;100:27–31 [PubMed] [Google Scholar]
- 38.Hayes LJ, O'Brien-Pallas L, Duffield C, et al. . Nurse turnover: A literature review—An update. Int J Nurs Stud 2012;49:887–905 [DOI] [PubMed] [Google Scholar]
- 39.Miles MB, Huberman AM. Analyse des données qualitatives, 2nd ed. Brussels: De Boeck, 2003 [Google Scholar]
- 40.Nami N, Giannini E, Burroni M, et al. . Teledermatology: State-of-the-art and future perspectives. Expert Rev Dermatol 2012;7:1–3 [Google Scholar]
- 41.van der Heijden JP, de Keizer NF, Bos JD, et al. . Teledermatology applied following patient selection by general practitioners in daily practice improves efficiency and quality of care at lower cost. Br J Dermatol 2011;165:1058–1065 [DOI] [PubMed] [Google Scholar]
- 42.Dobke MK, Bhavsar D, Gosman A, et al. . Pilot trial of telemedicine as a decision aid for patients with chronic wounds. Telemed J E Health 2008;14:245–249 [DOI] [PubMed] [Google Scholar]
- 43.Chipps J, Brysiewicz P, Mars M. A systematic review of the effectiveness of videoconference-based tele-education for medical and nursing education. Worldviews Evid Based Nurs 2012;9:78–87 [DOI] [PubMed] [Google Scholar]
- 44.Cresswell K, Sheikh A. Organizational issues in the implementation and adoption of health information technology innovations: An interpretative review. Int J Med Inform 2013;82:e73–e86 [DOI] [PubMed] [Google Scholar]
- 45.Arnaert A, Macfarlane F. 4. Telehealth nursing in Canada: Opportunities for nurses to shape the future. In: Kumar S, Snooks H, eds. Telenursing. London: Springer, 2011:29–45 [Google Scholar]