Abstract
Background: It is not known whether unmet palliative care needs are associated with an interest in palliative care services among patients with advanced cancer receiving ongoing oncology care.
Objective: To assess the association between unmet palliative care needs and patient interest in subspecialty palliative care services.
Design: Cross-sectional telephone survey.
Subjects and setting: One hundred sixty-nine patients with advanced cancer receiving care from 20 oncologists at two academic cancer centers.
Measurements: Surveys assessed palliative care needs in six domains. Patients were read a description of palliative care and then asked three questions about their current interest in subspecialty palliative care services (perceived need, likelihood of requesting, willingness to see if their oncologist recommended; all outcomes on 0–10 Likert scale).
Results: The vast majority of patients described unmet palliative care needs, most commonly related to psychological/emotional distress (62%) and symptoms (62%). In fully adjusted models accounting for clustering by oncologist, unmet needs in these domains were associated with a higher perceived need for subspecialty palliative care services (psychological/emotional needs odds ratio [OR] 1.30; 95% confidence interval [CI] 1.06–1.58; p=0.01; symptom needs OR 1.27; 95% CI 1.01–1.60; p=0.04). There was no significant association between unmet needs and likelihood of requesting palliative care services. Willingness to see palliative care if oncologist recommended was high (mean 8.6/10, standard deviation [SD] 2).
Conclusion: Patients with advanced cancer and unmet symptom and psychological/emotional needs perceive a high need for subspecialty palliative care services but may not request them. Efforts to increase appropriate use of subspecialty palliative care for cancer may require oncologist-initiated referrals.
Introduction
Recent guidelines recommend expanded use of subspecialty palliative care services for patients with advanced cancer.1,2 Subspecialty palliative care is provided by palliative medicine specialists and grew out of the hospice movement. However, unlike hospice care, which requires that patients have a limited life expectancy and forego many life-prolonging treatments, palliative care may be offered at any stage of a serious illness and can be provided concomitantly with standard oncology care.3 Accumulating evidence that subspecialty palliative care improves patient and caregiver outcomes,4–6 coupled with the recognition that palliative care services are most often offered too late in the cancer care continuum,7 has led the National Comprehensive Cancer Network to recommend that oncologists inform all patients and families earlier about the role and benefits of palliative care.1 Public interest campaigns have focused on increasing patient-driven requests for palliative care services.8,9
However, to date little is known about patient interest in receiving palliative care services or whether this interest reflects unmet palliative care needs. Patients may not recognize which needs would benefit from subspecialty palliative care services or may confuse palliative care with hospice, mistakenly assuming that palliative care is only for people who are at the end of life. In a prior analysis we found that substituting the term supportive care for palliative care was associated with better understanding, more favorable impressions, and higher future perceived need, perhaps because supportive care was less frequently equated with death or dying. However, we found no association between the terminology used and patients' current interest in receiving these services.10 Alternatively, patients may prefer to receive all of their cancer care from a single physician or oncology clinic or be reluctant to request additional services unless recommended by their oncologist. A mismatch between patients' needs and interest in receiving palliative care services could limit the effectiveness of efforts to promote patient requests for palliative care.
Interested in these issues, we conducted this analysis to examine the association between unmet palliative care needs and patient-reported interest in seeing a subspecialty palliative care physician.
Methods
Design
We administered a cross-sectional telephone survey to patients with advanced cancer receiving ongoing oncology care between December 2011 and April 2012. The survey was designed to assess how the language used to describe palliative care services affects patients' understanding and views, utilizing a randomized factorial design. Details of the study design and findings related to the impact of descriptive language have been reported previously.10 We analyzed data from the same initial survey study to answer the current research question. The local university Institutional Review Board approved all study procedures.
Subjects and setting
Study participants were recruited from the offices of 20 medical oncologists practicing at two university-affiliated cancer centers with outpatient palliative care clinics in Pittsburgh, PA. Inclusion criteria were 18 years of age or older, advanced cancer (defined as a stage IV solid tumor or refractory or recurrent hematologic malignancy), ongoing receipt of standard oncology care (defined as a visit with their oncologist within the past 3 months or scheduled in the upcoming 1 month), and access to a telephone. Non-English–speaking patients and patients who were determined by their oncologist to be physically or emotionally unable to complete a 30-minute interview were excluded.
Recruitment and enrollment
Participating oncologists reviewed their clinic schedules to identify up to 30 eligible patients each (range, 6–30). Eligible patients were mailed a letter from their oncologist describing the study that included a toll-free opt out number and a visual response guide. Study staff contacted patients by phone within 3 weeks of mailing the introductory letter. Up to five attempts were made to contact each patient. All participants provided verbal informed consent prior to completing the telephone interview.
Survey content and randomization:
Because many patients with advanced cancer are unfamiliar with the term palliative care,11 we read a brief definition prior to assessing patient interest in subspecialty palliative care services. Pursuant to the initial study question, patients were randomized using a 2×2 factorial design to hear one of four definitions that differed by the name (palliative care versus supportive care) and the description used (a traditional description of palliative care adapted from the cancer center's website versus a patient-centered description using language preferred by the general public in a recent consumer marketing survey).12 Computer-generated block randomization stratified participants by age (>65 or ≤65 years), gender, and interviewer. We found no significant association between language used to describe palliative care and patient-reported current interest in palliative care services (see Appendix A).10 We therefore conducted the current analysis using the entire cohort. Complete descriptions of palliative care and survey content are available in Appendix A (www.liebertpub.com/jpm).
Independent variables
We assessed patients' palliative care needs using an adapted version of a previously validated needs assessment instrument for patients with advanced cancer13 that was subsequently shortened and validated with patients with advanced lung cancer.14 Based on initial expert review and pilot testing, we further shortened the original instrument to reduce participant burden and reworded several questions for clarity. We added 2 questions related to spiritual/existential needs based on the widely used FICA Spiritual Assessment Tool.15 The final survey included 32 questions in 6 domains (symptom, psychological/emotional, medical communication/information, daily living, spiritual/existential, and social). For each item, participants were asked whether this was something that they needed in the last month (yes/no). If the item was identified as a need, they were asked how well this need had been met by health care providers (fully, partially, or not at all).
Dependent variables
After hearing a definition of palliative care, participants were asked to rate the extent to which they agreed or disagreed (0–10 Likert scale) with three statements about their current interest in these services: perceived need (palliative care services would be helpful to me or my family now); likelihood of requesting (I am likely to ask my oncologist if I can see a palliative care doctor); and willingness to see if their oncologist recommended (I would be willing to see a specialized palliative care doctor if my oncologist recommended it).
Other variables
The survey included questions about race, education, income, religion, date of cancer diagnosis, length of time receiving care from current oncologist, and prior use of palliative care services. We collected participant age, gender and cancer type from the medical record.
Analysis
We used summary statistics to analyze demographic/clinical characteristics and distribution of unmet needs. For each domain of palliative care needs, we calculated the percentage of participants who identified at least one unmet need (defined as a need met “partially” or “not at all” by health care providers). We used t tests to assess the relationship between unmet needs in each domain and interest in receiving subspecialty palliative care services. We then dichotomized each dependent outcome variable by distribution, using the median whole number for each outcome to ensure the most balanced groups, and ran univariate logistic regression models to assess the association between demographic/clinical characteristics (age, gender, race, education, income, religion, cancer type, months since cancer diagnosis, months receiving care from current oncologist and prior use of palliative care services) and patient interest. We constructed final multivariate models to examine the association between unmet needs and interest in palliative care adjusting for variables that we hypothesized a priori may be associated with patient interest in receiving palliative care (age, gender, race) and all additional demographic/clinical variables found to be marginally significant (p<0.1) in univariate regression for each outcome. For both univariate and multivariate logistic regression, a random intercept for each oncologist was included in the model using a standard generalized linear mixed model to adjust for clustering effects within each oncologist.
Finally, because prior exposure to palliative care may affect patient needs and interest, we conducted a sensitivity analysis excluding participants who reported previous use of palliative care services.
Results
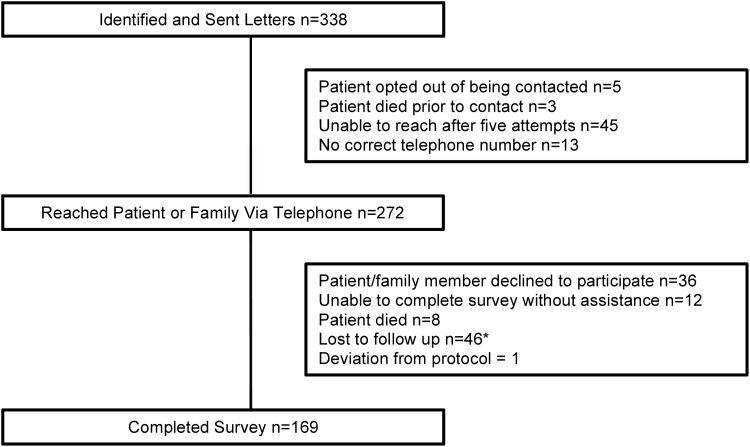
A total of 338 patients were identified as eligible. Of these, 272 were reached by telephone and 169 completed the survey. Patient enrollment is summarized in Figure 1. There were no significant differences in age, gender, or cancer diagnosis between participants and nonparticipants (data not shown). The mean age of participants was 62 years old. The most common cancer diagnoses were breast (32%) and lung (18%). The median number of months since receiving a cancer diagnosis was 46 and the median number of months receiving care from the participating oncologist was 24. Overall, 11% of participants had previously seen a palliative or supportive care provider. Additional demographic and clinical characteristics are shown in Table 1.
FIG. 1.
Enrollment diagram. (*Patient or family reached, requested call-back, and unable to reach on subsequent attempts).
Table 1.
Demographic and Clinical Characteristics of Participants (n=169)a
| Age, mean (SD) | 62.3 (11.6) |
| Female | 107 (63.3) |
| Race | |
| Caucasian | 161 (95.3) |
| Education | |
| ≤High school diploma/GED | 50 (29.6) |
| >High school diploma/GED | 119 (70.4) |
| Ave. Household Income | |
| <$30,000 | 33 (19.5) |
| ≥$30,000 | 97 (57.4) |
| Declined to answer | 39 (23.1) |
| Religion | |
| Catholic/Christian | 150 (88.8) |
| Jewish | 7 (4.1) |
| Other Religion | 6 (3.6) |
| Non/agnostic | 5 (3.0) |
| Cancer diagnosis | |
| Breast | 54 (32) |
| Lung | 31 (18.3) |
| Gastrointestinal | 22 (13.0) |
| Hematologic | 19 (11.2) |
| Genitourinary | 18 (10.7) |
| Sarcoma | 12 (7.1) |
| Skin | 7 (4.7) |
| Gynecologic | 2 (1.2) |
| Brain | 2 (1.2) |
| Other | 2 (1.2) |
| Months since cancer diagnosis, median (MAD) | 46 (54.9) |
| Months receiving care from current oncologist, median (MAD) | 24 (27.4) |
| Seen palliative/supportive care provider | 18 (10.7) |
All numbers are reported as n (%) except where indicated otherwise.
SD, standard deviation; MAD, median absolute deviation.
Of the 169 participants, 139 (82%) identified at least one unmet need. The median number of total unmet needs identified was 3, range, 0–26. Most commonly, participants identified unmet symptom needs (104/169; 62%) and unmet psychological/emotional needs (104/169; 62%). The percentage of participants indentifying unmet needs in each domain is shown in Table 2.
Table 2.
Percentage of One Hundred Sixty-Nine Participants Identifying Unmet Palliative Care Needs in Each of Six Domains
| Domain of needs | Identified unmet need n (%) |
|---|---|
| Symptom | 104 (62) |
| Psychological/emotional | 104 (62) |
| Medical communication/information | 65 (39) |
| Daily living | 46 (27) |
| Spiritual/existential | 39 (23) |
| Social | 33 (20) |
In unadjusted analyses, patients with unmet needs in each of the following four domains reported higher current perceived need for subspecialty palliative care services: symptom, psychological/emotional, medical communication/information and spiritual/existential (Table 3). Only patients with unmet medical/communication needs reported higher likelihood of requesting subspecialty palliative care. Unmet needs were not associated with patient-reported willingness to see a palliative care doctor if their oncologist recommended it, which was overall high (mean, 8.6/10; standard deviation [SD] 2).
Table 3.
Association between Domains of Palliative Care Needs and Interest in Subspecialty Palliative Care Servicesa
| Current perceived need for subspecialty palliative care, mean (SD) | Likelihood of requesting subspecialty palliative care, mean (SD) | Willingness to see subspecialty palliative care if their oncologist recommended it, mean (SD) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| No unmet needs | Any unmet needs | p value | No unmet needs | Any unmet needs | p value | No unmet needs | Any unmet needs | p value | |
| Symptom | 3.9 (3.2) | 5.4 (3.2) | 0.003 | 5.6 (3.5) | 6.2 (3.5) | 0.295 | 8.5 (2.1) | 8.7 (2) | 0.542 |
| Psychological/emotional | 4 (3.3) | 5.4 (3.2) | 0.014 | 5.5 (3.5) | 6.3 (3.4) | 0.187 | 8.5 (2) | 8.6 (2) | 0.705 |
| Medical communication/information | 4.1 (3.1) | 6 (3.3) | 0.001 | 5.6 (3.5) | 6.7 (3.4) | 0.042 | 8.6 (1.9) | 8.6 (2.2) | 0.867 |
| Daily living | 4.7 (3.3) | 5.2 (3.3) | 0.412 | 6 (3.5) | 6 (3.6) | 0.922 | 8.6 (2) | 8.6 (1.9) | 0.939 |
| Spiritual/existential | 4.6 (3.3) | 5.8 (3.2) | 0.04 | 5.7 (3.6) | 6.8 (3.1) | 0.075 | 8.5 (2.1) | 8.8 (1.6) | 0.27 |
| Social | 4.7 (3.3) | 5.3 (3.4) | 0.4 | 6 (3.5) | 5.8 (3.3) | 0.773 | 8.5 (2.1) | 8.8 (1.6) | 0.354 |
All outcomes on 0–10 Likert scale with higher scores indicating higher perceived.
In sensitivity analyses excluding the 11% of participants who reported having previously seen a palliative/supportive care provider, distribution of unmet needs and association between unmet needs and current interest in palliative care was unchanged (results not shown).
In final models adjusted for age, gender, race, clustering by oncologist, and additional clinical/demographic variables with marginal significance in univariate regression, unmet symptom and psychological/emotional needs remained associated with a higher perceived need for subspecialty palliative care services (symptom needs odds ratio [OR] 1.27; 95% confidence interval [CI] 1.01–1.60; p=0.04; psychological/emotional needs OR 1.30; 95% CI 1.06–1.58; p=0.01). However, there was no significant association between unmet needs and likelihood of requesting palliative care services (Table 4).
Table 4.
Odds of Higher Interest in Subspecialty Palliative Care Services among Patients with Unmet Palliative Care Needs
| Odds of higher current perceived need for subspecialty palliative carea (95% CI) | p value | Odds of higher likelihood of requesting subspecialty palliative careb (95% CI) | p value | Odds of greater willingness to see subspecialty palliative care if oncologist- recommendedc (95% CI) | p value | |
|---|---|---|---|---|---|---|
| Symptom | 1.27 (1.01, 1.60) | 0.04 | 0.99 (0.83, 1.18) | 0.88 | 0.98 (0.80, 1.21) | 0.88 |
| Psychological/emotional | 1.30 (1.06, 1.58) | 0.01 | 0.99 (0.86, 1.15) | 0.94 | 1.06 (0.89, 1.27) | 0.49 |
| Medical communication/information | 1.16 (0.87, 1.54) | 0.32 | 1.12 (0.87, 1.44) | 0.39 | 1.02 (0.78, 1.33) | 0.88 |
| Daily living | 1.49 (0.82, 2.70) | 0.19 | 0.93 (0.58, 1.48) | 0.75 | 0.95 (0.56, 1.62) | 0.85 |
| Spiritual/existential | 1.33 (0.76, 2.35) | 0.32 | 1.08 (0.67, 1.74) | 0.74 | 1.33 (0.78, 2.30) | 0.30 |
| Social | 1.19 (0.59, 2.41) | 0.63 | 0.71 (0.40, 1.28) | 0.63 | 1.21 (0.61, 2.40) | 0.58 |
Additionally adjusted for income, month since cancer diagnosis, months receiving care from current oncologist, seen pall/supportive care provider.
Additionally adjusted for seen pall/supportive care provider.
Additionally adjusted for income.
Outcome variables (scale 0–10) were dichotomized by distribution using the median for each (current perceived need≥5 vs.<5; likelihood of requesting>6 vs.≤6; willingness to see if oncologist recommended 10 vs.<10).
All models adjusted for age, gender, race, clustering by oncologist, and additional variables found to be marginally significant (p<0.1) in individual univariate analysis for each outcome, as indicated.
CI, confidence interval.
Discussion
In this analysis of patients with advanced cancer receiving ongoing oncologic care, we found frequently reported unmet palliative care needs in all domains, with nearly two-thirds of participants identifying unmet symptom and psychological/emotional needs. Unmet needs in these domains were associated with a higher patient perceived need for subspecialty palliative care services. However, there was no association between unmet needs and patient-reported likelihood of requesting palliative care. Most patients reported that they would be very likely to see a palliative care specialist if recommended by their oncologist.
One of the challenges in efforts to improve the quality of life for patients with advanced cancer is matching provision of subspecialty palliative care to the patients who need it most. One approach has been to encourage patients and families to request palliative care. However, our data suggest that while patients with unmet symptom and psychological/emotional needs are more likely to perceive a need for subspecialty palliative care services, they are not more likely to request them. Similarly, in our prior analysis we did not find that using language preferred by the public in a national survey to describe palliative care12 or substituting the term supportive care increased patient-reported likelihood of requesting these services.10 Power imbalances in the doctor–patient relationship may inhibit patient-initiated discussion of palliative care needs or requests for additional services beyond those provided by their oncologists, irrespective of how well these services are understood or the extent to which they are needed. Additional work is necessary to identify barriers to patient requests for palliative care and identify patient-centered approaches to increase appropriate service use.
Our data indicate that patients are more likely to pursue subspecialty palliative care if recommended by their oncologist. These findings signal the importance of ensuring that oncologist referrals reflect patient needs. Recommending palliative care for all patients with advanced cancer and/or a high symptom burden, as suggested by recent guidelines, would vastly overwhelm limited subspecialty palliative care resources.16 Easily-administered screening tools may help oncologists identify and refer their patients who would most benefit from palliative care services. Targeting education about the benefits of palliative care to oncologists may also help to increase appropriate referrals. Finally, this data highlights the importance of facilitating and improving delivery of palliative care within oncology practices.
Our study has several limitations. First, the survey was conducted at two academic cancer centers with well-established palliative care clinics. Results may differ in other settings where palliative care services are less available. Second, half of identified patients completed the survey. However, our enrollment rate compares favorable to other telephone surveys17,18 and the demographics of nonrespondents did not differ significantly from respondents. Third, our sample was predominantly Caucasian. A prior study demonstrated that awareness of palliative care may be lower among African Americans.11 Fourth, while all participants were receiving current care from an oncologist, we do not have information on the types of cancer treatment being provided; we were therefore unable to control for treatment received in our analysis. Additional work is needed to explore possible associations between different types of cancer treatments, unmet patient needs, and interest in receiving palliative care services. Finally, our cross-sectional design did not allow us to measure actual use of palliative care services.
In summary, we find that significant unmet symptom and psychological/emotional needs among patients with advanced cancer are associated with an interest in receiving subspecialty palliative care, but not a plan to request these services. Additional work is needed to ensure that patients with advanced cancer are referred to appropriate services to alleviate persistent unmet palliative care needs.
Supplementary Material
Acknowledgments
Dr. Schenker was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (KL2TR000146) and by the Junior Scholar Award from the University of Pittsburgh Department of Medicine. Dr. Maciasz was supported by a Doris Duke Clinical Research Fellowship. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors would like to thank Galen Switzer, PhD and his research team for guidance on survey design and interview techniques.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Levy MH, Adolph MD, Back A, Block S, Codada SN, Dalal S, Deshields TL, Dexter E, Dy SM, Knight SJ, Misra S, Ritchie CS, Sauer TM, Smith T, Spiegel D, Sutton L, Taylor RM, Temel J, Thomas J, Tickoo R, Urba SG, Von Roenn JH, Weems JL, Weinstein SM, Freedman-Cass DA, Bergman MA; NCCN (National Comprehensive Cancer Network): Palliative care. J Natl Compr Cancer Netw 2012;10:1284–1309 [DOI] [PubMed] [Google Scholar]
- 2.Smith TJ, Temin S, Alesi ER, Abernethy AP, Balboni TA, Basch EM, Ferrell BR, Loscalzo M, Meier DE, Paice JA, Peppercorn JM, Somerfield M, Stovall E, Von Roenn JH: American Society of Clinical Oncology provisional clinical opinion: the integration of palliative care into standard oncology care. J Clin Oncol 2012;30:880–887 [DOI] [PubMed] [Google Scholar]
- 3.Quill TE, Abernethy AP: Generalist plus specialist palliative care: Creating a more sustainable model. N Engl J Med 2013;368:1173–1175 [DOI] [PubMed] [Google Scholar]
- 4.Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, Dahlin CM, Blinderman CD, Jacobsen J, Pirl WF, Billings JA, Lynch TJ: Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733–442 [DOI] [PubMed] [Google Scholar]
- 5.Bakitas M, Lyons KD, Hegel MT, Balan S, Brokaw FC, Seville J, Hull JG, Li Z, Tosteson TD, Byock IR, Ahles TA, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA 2009;302:741–749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rabow MW, Dibble SL, Pantilat SZ, McPhee SJ: The comprehensive care team: A controlled trial of outpatient palliative medicine consultation. Arch Intern Med 2004;164:83–91 [DOI] [PubMed] [Google Scholar]
- 7.Osta BE, Palmer JL, Paraskevopoulos T, Pei BL, Roberts LE, Poulter VA, Chacko R, Bruera E: Interval between first palliative care consult and death in patients diagnosed with advanced cancer at a comprehensive cancer center. J Palliat Med 2008;11:51–57 [DOI] [PubMed] [Google Scholar]
- 8.Get Palliative Care: www.getpalliativecare.org/ (Last accessed July25, 2013)
- 9.Hansen C: ACS CAN launches new advertising campaign to focus on palliative care. Cancer Candor; 2012. www.acscan.org/content/cancer-candor/acs-can-launches-new-advertising-campaign-to-focus-on-palliative-care/ (Last accessed March12, 2014)
- 10.Maciasz R, Arnold R, Chu E, Park S, Borgenheimer L, Schenker Y: Does it matter what you call it? a randomized trial of language used to describe palliative care services. J Pain Symptom Manage 2013;45:359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matsuyama RKP, Balliet WP, Ingram KP, Lyckholm LJMD, Wilson-Genderson MP, Smith TJMD: Will patients want hospice or palliative care if they do not know what it is? J Hosp Palliat Nurs 2011;13:41–46 [Google Scholar]
- 12.McInturff B, Harrington L: Public opinion strategies. Presentation of 2011 Research on Palliative Care Center to Advance Palliative Care, American Cancer Society Cancer Action Network; 2011. www.capc.org/tools-for-palliative-care-programs/marketing/public-opinion-research/2011-public-opinion-research-on-palliative-care.pdf (Last accessed August6, 2013)
- 13.Rainbird KJ, Perkins JJ, Sanson-Fisher RW: The Needs Assessment for Advanced Cancer Patients (NA-ACP): A measure of the perceived needs of patients with advanced, incurable cancer. A study of validity, reliability and acceptability. Psychooncology 2005;14:297–306 [DOI] [PubMed] [Google Scholar]
- 14.Schofield P, Gough K, Ugalde A, Dolling L, Aranda S, Sanson-Fisher R: Validation of the needs assessment for advanced lung cancer patients (NA-ALCP). Psychooncology 2012;21:451–455 [DOI] [PubMed] [Google Scholar]
- 15.Borneman T, Ferrell B, Puchalski CM: Evaluation of the FICA Tool for Spiritual Assessment. J Pain Symptom Manage 2010;40:163–173 [DOI] [PubMed] [Google Scholar]
- 16.Lupu D, American Academy of H, Palliative Medicine Workforce Task Force: Estimate of current hospice and palliative medicine physician workforce shortage. J Pain Symptom Manage 2010;40:899–911 [DOI] [PubMed] [Google Scholar]
- 17.Curtin R, Presser S, Singer E: Changes in telephone survey non response over the past quarter century. Public Opin Q 2005;69:87–98 [Google Scholar]
- 18.Blumberg SJ, Foster EB, Frasier AM, Satorius J, Skalland BJ, Nysse-Carris KL, Morrison HM, Chowdhury SR, O'Connor KS: Design and operation of the National Survey of Children's Health, 2007. Vital Health Stat 1 2012;June(55):1–149 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.