Abstract
Objectives
Relationships between health literacy, self-efficacy, food label use, and dietary quality in young adults aged 18-29 were examined.
Methods
Health literacy, self-efficacy, food label use, and dietary quality were assessed. Participants were categorized into low, medium and high health literacy groups based on Newest Vital Sign score.
Results
Self-efficacy and health literacy were predictors of food label use, which positively predicted dietary quality. The low health literacy group had significantly lower use of food labels than the high health literacy group. However, there was no significant difference between medium and high health literacy groups.
Conclusion
Strategies to enhance health literacy, self efficacy and food label use should be developed to improve dietary quality and health outcomes.
Keywords: health literacy, food label, dietary quality
Young adulthood is an important transition period during which long-term health behavior patterns are established.1 Failure to form positive health behavior habits during this period makes young adults vulnerable to poor health outcomes and many chronic disorders later in life.1, 2 For instance, physical inactivity and unhealthy eating result in obesity which in turn increases the risk for developing Type 2 diabetes (T2D).2, 3 Young adults who develop T2D early are more likely to have a longer-term risk for poor glycemic control and they are at greater risk for developing diabetes complications than those with late-onset T2D.4
Over the last 4 decades, the prevalence of obese young adults has increased from 8% in 1971-1974 to 32.6% in 2009-2010.5 One of the important contributors to this trend is young adults’ eating habits.6, 7 Young adults are major consumers of fast food, soft drinks and “Fourth meal (the meal between dinner and breakfast)”.1 They consume less fruit, vegetables, milk, and more salty snacks than as children. Also, they eat almost the same foods everyday, which may lead to excesses or deficiencies of certain nutrients.1 Thus, their reported dietary quality is often very poor.1, 6, 7 Effective public health initiatives and/or behavioral interventions to promote healthy eating are necessary to prevent obesity and early onset T2D. 8, 9
In the US, dietary guidelines and food labels are available to help people select healthier food.8, 10, 11 In particular, food labels based on the dietary guidelines are mandatory on all pre-packaged foods.9, 12 However, this policy is only effective when people read food labels on pre-packaged food, accurately understand and effectively utilize these labels to select healthier choices.
Research shows that attitude, previous nutrition education, socio-demographic factors (eg, age, sex) are significant predictors of food label use behavior.13, 14 For instance, college men chose food without reading nutrition facts on the label as they regarded this action as feminine.13 Not having received previous education on how to use food labels was also a predictor of less frequent usage of food labels.14, 15
A study conducted with American adolescents found that about three-quarters of adolescents read food labels “always” or “sometimes”, but doing so did not affect their food choices.9, 16 However, studies with European Union (EU) adults showed different findings. About a quarter of people (27.0%) read food labels and it increased their selection of healthier food.8 Although different populations (adults vs. adolescents) may account for the differences in these findings, labeling methods may also contribute to the differences. While the U.S. has nutrition facts, the E.U. uses the Choices logo (eg, smart choice) and traffic light labeling.8, 9 Thus, Americans require sufficient numeracy and literacy skills to appropriately understand and utilize nutrition fact label information. Europeans, on the other hand, only need to understand the meanings of colors (traffic light color system) or logos (Choices logos) to select healthier food choices. Different type and level of health literacy may be a significant factor in food label use behavior and its impact on dietary quality.
Health literacy refers to an individuals’ capability to obtain and understand health information to make appropriate health-related decisions.17, 18 Not surprisingly, low health literacy is related to poor clinical outcomes. Sufficient health literacy is the key to improving treatment regimen adherence.17 As briefly addressed above, the US nutrition labels contain serving size, calories per serving, nutrient information, and percent of daily value based on 2000 Kcal diet on each packaged food item and a foot note on recommended daily value and ingredients in a block text.10 Therefore, Americans who are required to follow dietary regimens need to know their individual dietary recommendation based on their sex, age, physical activity level, first. Then, they must have appropriate literacy and numeracy skills to understand and recalculate the food label information presented. In addition, appropriate portion size estimation skills are necessary to follow and achieve dietary goals. Thus, it is important to identify the relationship between health literacy with food labels and food label use behaviors to design a nutrition education program to facilitate healthy eating in American young adults.
Although health literacy plays an important role in making informed decisions and behavioral changes, health behaviors are also influenced by psychosocial attributes, such as self-efficacy.1 Self-efficacy differs from wishful thinking in that it refers to individuals’ beliefs in their capabilities to perform a specific behavior in diverse situations.19, 20 People with higher self-efficacy are more likely to make necessary efforts to attain a desirable outcome despite barriers, and in less than ideal circumstances.21, 22 For instance, people with high self-efficacy were more likely to actively engage in healthy diets for weight loss than people with low self-efficacy.23 Therefore, successful past experiences coupled with knowledge and skills are major contributors to increased self-efficacy.22
Studies have emphasized the significance of dietary quality in preventing obesity and T2D, which are growing public health concerns for American young adults.11, 24, 25 Therefore, specific strategies to improve dietary quality for this age group should be developed. However, this population has been understudied.1, 26 Traditionally, young adults are considered a healthy population who need little attention from researchers and clinicians.1, 27 To reduce this scientific gap, this study examined relationships between health literacy and eating behavior self-efficacy, food label use behavior, and dietary quality in American overweight obese young adults using path analyses. The hypotheses were: 1) sufficient health literacy will increase eating behavior self-efficacy and food label use behavior as well as improve dietary quality; 2) higher eating behavior self-efficacy will increase food label use behavior and improve dietary quality; and 3) frequent food label use behaviors will improve dietary quality. The obtained information will help researchers and clinicians to develop an effective behavioral intervention for American young adults who need immediate help to improve their dietary quality in order to reduce their weights and health risk in the future.
METHODS
Design/ Setting/ Participants
A correlational cross-sectional study design was used. IRB approval from the appropriate institutions and informed consent from the participants were obtained prior to the study. Young adults, ages 18-29, who were physically inactive (leisure time activity < 90 minutes per week), overweight or obese (BMI ≥ 25), and residing in the metropolitan Atlanta area were recruited using flyers posted in colleges, universities, and student clinics, and through email invitations using a university’s student email list. Also, self-referral was used to recruit potential participants.
Individuals who were under physician-supervised dietary and exercise regimens, diagnosed with diabetes, or had blood diseases influencing A1C test results were excluded. Of 234 potential recruits, only 106 young adults were enrolled to complete data collection (Mean age (SD): 23.99 (3.25); age ranges: (18.69-29.95))
Variables and Measures
Sociodemographics
Age, race/ethnicity, sex, and education were measured by a Socio-Demographic Questionnaire (SDQ). Also, participants’ body mass indexes (BMI) were assessed based on the height and weight measured by a trained research nurse in a university research interaction unit. Overweight and obesity were defined using National Institutes of Health clinical guidelines on overweight and obesity.28 One item based on the transtheoretical model was developed by the first author and included to assess participants’ readiness to change eating habits.
Health literacy on food label use
Participants’ health literacy for reading food labels was assessed with the Newest Vital Sign Scale (NVS, 6 item, α = .76).29 The questionnaire includes 6 items to assess participants’ prose literacy, numeracy, and document literacy on an ice cream container.29 An example of the items is “how many calories will you eat if you eat the entire container?” Correct responses are scored 1 and incorrect responses are scored 0. Each response score is summed for a total NVS score, with the possible range of scores on the NVS being 0-6. It is suggested that scores are grouped into 3 categories, inadequate, limited, and adequate health literacy.29 In this study, scores of 0-2, 3-4, and 5-6 were defined as low (inadequate), medium (limited) and high (adequate) health literacy, respectively. In the current study, Cronbach’s alpha was .72.
Eating behavior self-efficacy
Self-efficacy related to eating behavior was measured with the Weight Efficacy Lifestyle Questionnaire. 30 The tool contained 20 items rated on a 10-point Likert scale [not confident (0) to highly confident (9)]. There are 5 subscales which measure self-efficacy to resist eating behaviors to manage weight in 5 separate situations: negative emotion, food availability, social pressure, physical discomfort, and other activities during eating (eg, TV watching).30 In the current study, the reported reliability of the overall Weight Efficacy Lifestyle Questionnaire was .93.
Food label use behavior
A self-reported item, “how often do you use the food label when making a food selection?” was used to assess the actual food label reading behavior. It was measured on a 5-point Likert scale ranging from never (1) to always (5). This self-reported item was developed by the first author of this study, and obtained face validity from potential participants prior to the study.
Dietary quality eating behavior
Dietary quality was assessed by a modified version of Dietary Quality Index - Revised (DQIR) consisting of 10 categories of dietary components. Groups of food (grains, vegetable, fruit, total fat, saturated fat), nutrients (cholesterol, calcium, Iron), diet diversity (grain, vegetables, fruit and protein diversity) and diet moderation (added fat, sodium, alcohol, and added sugar) were used to evaluate whether persons’ dietary quality met the dietary guidelines. When participants meet dietary recommendations, they obtain 10 points from each category, and thus the maximum possible score of DQIR is 100. For this study, we modified the DQIR in order to assess dietary quality for sedentary young adults (DQIR-Y). To obtain a DQIR-Y score, multiple steps were taken. First, participants were asked to complete a self-reported 152-item Youth/Adolescent Food Frequency Questionnaire (YAQ) which is a youth version of the Willet food frequency questionnaire.31, 32 Next, nutrient elements and serving size/ nutrient amount were recalculated based on the participants’ responses. Finally, the researchers reviewed several publications as well as the 2010 Dietary Guidelines for Americans to obtain an appropriate DQIR-Y score based on the most updated dietary guidelines.11, 25, 33, 34 During this step, several considerations were applied to modify the scoring for DQIR-Y. For instance, we did not include alcohol and discretionary fat consumptions when calculating dietary moderation since the literature did not clearly address alcohol effects on insulin sensitivity in this age group, and our dietary database was too vague to calculate the discretionary fat. Thus, the range of DQIR-Y scores is from 0 to 95 instead of 0 to 100.
Data Analysis
Data analysis was conducted with IBM SPSS 20.0 (IBM SPSS statistics) and Mplus version 7. A total of 106 participants enrolled in the study, 3 participants were excluded because one had undiagnosed diabetes and 2 participants did not complete all study measures (ie, the item regarding food label and Newest Vital Sign Scale) used in this study. Thus, only 103 participants were included for final data analysis.
A path analysis was performed on self-efficacy, food label use, and diet quality predicted by health literacy using mean and variance adjusted weighted least square (WLSMV) with bootstrapping in Mplus version 7. Food label use was analyzed as an ordinal variable. Health literacy was dummy coded into 2 variables (Low vs. High; Medium vs. High). WLSMV is one of the widely used estimation procedures used in structural equation modeling (SEM) with categorical variables. One thousand replications were performed for bootstrap to ensure accurate estimates of parameters. The model was saturated (ie, df = 0) and hence, no model fit statistics were reported. The model was tested in SEM to produce unbiased parameter estimates using WLSMV.
RESULTS
Sample Characteristics
The majority of study participants were female (78.6%), African Americans (70%), and college/undergraduate students (59.2%). Two-thirds of participants independently lived at a dormitory or off-campus housing without their parents. About half of participants reported less than $300 as monthly expenses, except rent. While 20% of participants were on diets (action or maintenance stage), 70% of participants were in the contemplation (considering starting the diet in 6 months) or preparation (considering starting the diet in a month) stages in changing eating behavior.
Caucasians had significantly higher health literacy and more years of education than African Americans. As expected, college graduates or above had significantly higher health literacy than high school graduates. Young adults living off-campus showed higher health literacy than young adults living with their parents. Interestingly, young adults in the preparation stage of changing their diet or with morbid obesity reported the lowest health literacy score although there was no statistically significant difference. In our study, eating behavior self-efficacy did not show any significant differences by socio-demographic variables (see Table 1).
Table 1.
Health Literacy and Eating Behavior Self-efficacy by Sample Characteristics (N = 103)
| Variables | Health literacy | Self-efficacy | ||||
|---|---|---|---|---|---|---|
| % (n) | Mean ± SD |
p - value |
Mean ± SD |
p - value |
||
| Gender | Male | 21.4(22) | 4.18±1.99 | .85 | 5.34± 1.68 | .64 |
| Female | 78.6(81) | 4.10±1.73 | 5.55±1.88 | |||
|
| ||||||
| Ethnicity / race | African Americans | 68.0(70) | 3.79±1.88 | 5.58±1.98 | ||
| Caucasian | 18.4(19) | 5.47±0.90 | .001 | 5.57±1.42 | .61 | |
| Asians and other | 13.6(14) | 3.93±1.27 | 5.05±1.57 | |||
|
| ||||||
| Education | Below high school or high school graduate |
17.5(18) | 2.89±2.05 | 5.31±1.83 | ||
| <.001 | .87 | |||||
| Some College | 59.2(61) | 4.07±1.68 | 5.56±1.86 | |||
| College graduate or above | 23.3(24) | 5.17±1.11 | 5.51±1.86 | |||
|
| ||||||
| Housing | Dormitory | 8.7(9) | 4.11±1.45 | 6.47±1.18 | ||
| Off campus housing | 56.3(58) | 4.42±1.66 | 5.55±1.68 | |||
| Parent house | 28.2(29) | 3.83±1.81 | .06 | 5.15±2.21 | .30 | |
| Other | 5.8 (6) | 2.50±2.59 | 5.28±2.01 | |||
| Missing | 1.0(1) | NA | NA | |||
|
| ||||||
| Monthly expense except rent |
Less than $100 | 11.7(12) | 3.25±2.05 | 5.88±1.79 | ||
| $100-299.99 | 35.0(36) | 4.42±1.50 | 5.59±1.65 | |||
| $300-499.99 | 20.4(21) | 3.62±2.09 | 5.62±1.71 | |||
| $500-799.99 | 16.5(17) | 4.71±1.40 | .10 | 5.39±2.56 | .80 | |
| $800-999.99 | 3.9(4) | 3.00±2.16 | 5.04±0.73 | |||
| More than $1000 | 10.7(11) | 4.45±1.86 | 4.83±1.92 | |||
| No response | 1.9(2) | NA | NA | |||
|
| ||||||
| Readiness to change eating behavior |
Precontemplation | 9.7(10) | 4.70±1.25 | 4.74±2.11 | ||
| Contemplation | 11.7(12) | 4.75±1.91 | 5.20±1.77 | |||
| Preparation | 57.3(59) | 3.72±1.90 | .12 | 5.64±1.85 | .64 | |
| Action | 16.5(17) | 4.53±1.38 | 5.68±1.48 | |||
| Maintenance | 4.9(5) | 4.80±1.10 | 5.53±2.49 | |||
|
| ||||||
| Overweight / obesity | Overweight ( 25 ≤ BMI <30) | 22.3(23) | 4.35±1.64 | 5.67±1.52 | ||
| Moderate obesity ( 30 ≤ BMI <35) |
31.1(32) | 4.25±1.70 | 5.13±1.68 | |||
| .56 | .38 | |||||
| Morbid obesity (BMI ≥35) | 46.6(48) | 3.92±1.90 | 5.67±2.04 | |||
Correlations Among Study Variables
African Americans were significantly less educated, and had higher BMI and lower health literacy. Educated persons had higher health literacy, used more food labels, and better quality of diet. However, when persons were more educated, they had higher BMI. When individuals were older, they were more likely to read food labels, but dietary quality was not significantly associated with age. Persons with higher self-efficacy were frequently using food labels. When persons frequently used food labels, they had better quality of diet (see Table 2).
Table 2.
Correlations Among Study Variables.
| 1.Gender | 2. Education | 3. Age | 4. BMI | 5. Health literacy | 6. Self-efficacy | 7. Food label use | 8. Dietary quality | |
|---|---|---|---|---|---|---|---|---|
| 1. Gender | 1.00 | .05 | .04 | .006 | −.05 | .05 | .10 | −.02 |
| 2.Education | 1.00 | 29** | −.20* | .48*** | .08 | .36*** | .29** | |
| 3. Age | 1.00 | −.006 | .07 | −.07 | .24* | .15 | ||
| 4. BMI | 1.00 | −.12 | .13 | .03 | −.09 | |||
| 5. Health literacy | 1.00 | .12 | .14 | .09 | ||||
| 6. Eating behavior self-efficacy | 1.00 | .25* | .11 | |||||
| 7. Food label use | 1.00 | .32** | ||||||
| 8. Dietary quality | 1.00 |
p < .05;
p < .01;
p < .001
In sex, men =0 and women=1
Hypotheses Testing
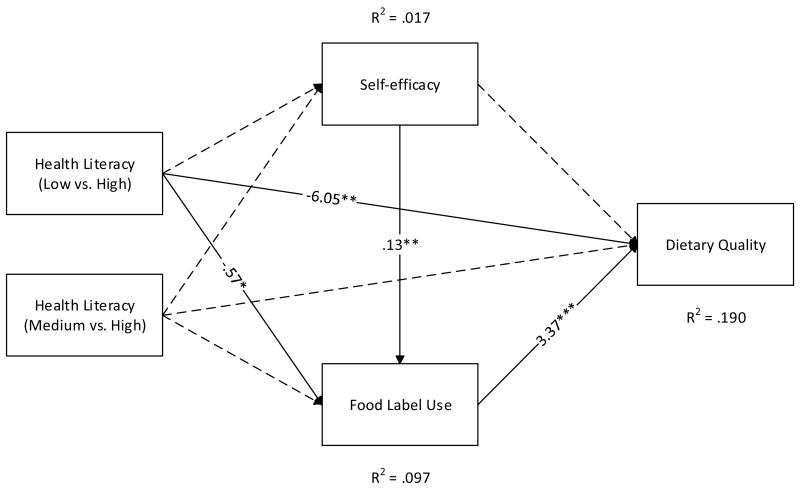
The level of health literacy did not predict eating behavior self-efficacy. Only about 2% of variability in self-efficacy was explained by health literacy groups. The low health literacy group was less likely to use food labels than the high health literacy group after adjusting for self-efficacy, p = .071. However, there was no significant difference between medium and high health literacy groups on food label use after adjusting for self-efficacy. Self-efficacy and health literacy were significant predictors of food label use behavior, which significantly positively predicted dietary quality. Overall, health literacy groups and self-efficacy explained about 10% of the variability in food label use.
The low health literacy group had significantly lower dietary quality than the high health literacy group. However, there was no significant difference between the medium and high health literacy groups. Unlike health literacy, there was no significant prediction of diet quality by self-efficacy. However, there was a marginal indirect effect of self-efficacy on diet quality through food label use, B = .44, z = 1.92, p = .055 (ie, self-efficacy affected food label use which in turn affected diet quality). The difference between low and high health literacy groups on diet quality was marginally partially mediated by self-efficacy and food label use, B = −2.14, z = −1.68, p = .093. Overall, nearly 20% of variability in dietary quality was explained by health literacy, self-efficacy, and food label use.
DISCUSSION
It is well known that a good quality diet is important for promoting health and preventing chronic disorders.33, 35, 36 For instance, a quality diet reduces cardiometabolic risks and insulin resistance, which are major causes of early onset type 2 diabetes (T2D).35 Despite well-known knowledge of healthy eating recommendations,37 practical strategies to improve dietary habits are still rare.
When people read labels, they consume low fat and low cholesterol food, and more fruits and vegetables.14, 26 Therefore, food label use is emphasized as a way to promote the selection of healthier choices.10 Our study supports this: frequent food label users had better dietary quality. However, food label use behavior can be affected by many other factors such as former nutritional education experiences, older age (in the 40s and 50s), sex (female participants), and meal planning responsibility.14, 26 Moreover, sufficient health literacy is a prerequisite to effectively using a food label to improve dietary quality. Very limited studies, however, examine the relationship among health literacy, food label use behavior, and dietary quality in Americans. In particular, to the best of our knowledge, no study has been conducted to examine the relationships among these variables in American overweight and obese young adults.
Unlike the findings of Sharif and Blank in overweight children,38 no significant relationship between health literacy and being overweight and obese was identified in young adults. However, the morbid obese group (BMI ≥ 35) had the lowest health literacy scores, which may be an extension of previous findings. Future research needs to re-examine the relationship between health literacy and overweight/obese condition in young adults with a larger sample.
As Vernon and colleagues addressed, low health literacy leads to ineffective and inefficient utilization of health systems and resources.39 For this reason, poor health literacy (ie,, below basic level) contributes to health disparities and improving health literacy is necessary to obtain health equity. However, health literacy levels may play a different role in health seeking behaviors and health outcomes. In the current study, young adults with low health literacy scores were less likely to use food labels to select food items and more likely to report poor diet quality. Thus, improving health literacy would be an important goal to improve dietary quality in young adults with low health literacy. However, there was no significant influence to use food labels or dietary quality by level of health literacy when persons reached at a certain level (ie, medium or above). In the current study, the effect of health literacy on health seeking behavior or behavioral outcome (dietary quality) appears abated when persons have medium and above health literacy. Rather, other factors (eg, self-efficacy) play a larger role in improving health seeking behavior and health outcomes. Thus, key remaining research questions are: 1) how to improve health literacy of persons with poor health literacy to sufficient levels in using food labels; 2) whether the current USA “nutrition facts” food labeling is an appropriate approach to provide enough health information to the public who need to follow a dietary regimen but have poor health literacy; 3) what types of information and food labeling approaches would be helpful for Americans to select healthier options if change the label and simplify the information; and 4) how to change persons’ psychosocial attributes (eg, attitude and self-efficacy) in order to increase the public’s likelihood of reading food labels?
One interesting finding from our study is that young adults living with their parents showed a relatively lower health literacy level than those living without parents which contrasts with a finding from a previous study which reported that persons living with others were more likely to use food label than persons living alone.15 This phenomenon may be related to situational factors such as meal planning responsibility and frequency of opportunities to read food labels.14, 15 When young adults live alone, they had increased responsibility to do grocery shopping and need to plan meals. Frequent personal grocery shopping may provide them with more opportunities to read food labels when selecting food options. Further study needs to examine the exact reasons why these differences are caused.
Our study found that eating behavior self-efficacy increases food label use behavior, but does not affect dietary quality although food label use behavior improves dietary quality. This finding may be related to the attributes of the eating behavior self-efficacy scale used in our study. As Bandura argues, self-efficacy is task specific.20 While the eating behavior self-efficacy scale assessed a person’s confidence to resist eating in various situations, our outcome variables in the current study were food label use behavior and dietary quality. That is, our self-efficacy scale did not ask participants about their level of confidence in understanding food labels or selecting healthier food options. Due to this discrepancy, our research may not have accurately captured the role of self-efficacy on the outcome variables assessed (food label use behavior and dietary quality). In the future, a study using an appropriate self-efficacy measure needs to be used to reexamine the role of self-efficacy in food label use behavior and dietary quality in this population.
Our study has several limitations that should be acknowledged. First, the small sample size limits the ability to generalize the findings. We were also not able to compare our model by socio-demographic variables, which may be confounders or moderators.14, 26 However, we used 1000 bootstrap replications to provide a more accurate parameter estimation. Also, SEM helps researchers to understand paths of study variable relationships. Because of convenience sampling method, we unexpectedly found that educated individuals had higher BMI. However, this finding should be carefully interpreted since our majority of participants (82.5%) were students attending college or university, and higher education years were positively correlated with age (r = .29, p < .01). That is, the relationship between education and BMI may actually be a relationship between age and BMI. A study with representative samples needs to be conducted to answer this question in the future.
Another limitation is related to measurements used in the current study. We already acknowledged a limitation related to the self-efficacy scale. Another limitation may also exist on the Newest Vital Sign (NVS), which is considered as a valid and reliable measure to assess health literacy.29, 38 Although Weiss and colleagues reported only 2.9 minutes (range = 1.5 - 6.2 minutes) with 24 participants for the time it took to administer the NVS,29 we observed much longer times during data collection for some participants. Since there was no specific scoring guideline for the administration time of the NVS, all participants had unlimited time to complete the NVS, resulting in higher health literacy scores than expected which may have produced different health literacy level cut-offs than Weiss’.29 In the future, more specific scoring guidelines need to be established to avoid any confusion and to accurately measure health literacy in American young adults.
Conclusions
Since both food label use and sufficient levels of health literacy predict better dietary quality, it is important for future studies to focus on identifying strategies to enhance health literacy and food label use behaviors in order to improve health behaviors and outcomes. Giving directions in plain language and using the teach-back method and pictorial images are known to be effective in low-literacy populations.18 Therefore, there is a need to identify whether these strategies are effective in increasing knowledge, skills and likelihood of food label use for American young adults as well helping them make informed decisions regarding healthy food choices. Another potential way to improve food label use behaviors in young adults is to raise awareness of the significance of food label use, specifically for young men. A campaign using social marketing may be a good approach to change their perception of reading food labels (eg, feminine behavior), and encourage them to frequently read food labels when they select pre-packaged food.13 Also, nutrition education to help overweight and obese young adults select healthier choices should be designed and implemented in practice settings where young adults are easily accessible and affordable.
Practice Implications
The findings of this study confirmed the significance of sufficient health literacy in assisting young adults to eat healthy. Thus, education programs to increase young adults’ health literacy must be implemented. Also, there is a need for the United States to develop and implement a standardized food labeling system that is easy to interpret for persons with low health literacy. Lastly, health care professionals should emphasize the use of food labels in selecting foods whenever they have an opportunity.
Figure 1.
Health Literacy and Diet Quality Path Analysis
(* p < .10, ** p < .05; *** p < .001).
§ In the model, the reference group was “high health literacy” group. Each path indicates a direct effect between variables.
§§ Bold line indicates paths showing significant direct effects between variables while dashed lines indicate paths that were included in the model but were not significant, not even marginally.
Table 3.
The Parameter Estimates of Health Literacy and Diet Quality.
| Dependent variable |
Independent variables | B | SE | z | p | R2 |
|---|---|---|---|---|---|---|
| Self-efficacy | .017 | |||||
| §Health Literacy (Low vs. High) | −.54 | .51 | −1.04 | .297 | ||
| §Health Literacy (Medium vs. High) | −.43 | .39 | −1.09 | .274 | ||
| Food Label Use | .097 | |||||
| Self-efficacy | .13 | .06 | 2.27 | .023 | ||
| §Health Literacy (Low vs. High) | −.57 | .32 | −1.80 | .071 | ||
| §Health Literacy (Medium vs. High) | −.19 | .25 | −.73 | .464 | ||
| Dietary Quality | .190 | |||||
| Food Label Use | 3.37 | 1.03 | 3.28 | .001 | ||
| Self-efficacy | −.06 | .53 | −.11 | .912 | ||
| §Health Literacy (Low vs. High) | −6.05 | 2.93 | −2.07 | .039 | ||
| §Health Literacy (Medium vs. High) | 3.52 | 2.34 | 1.50 | .133 |
In the model, the reference group was “ high health literacy” group
Acknowledgments
This study was supported by: (1) National Institute Health /National Institute of Nursing Research (K01NR012779), (2) University Research Committee and Atlanta Clinical & Translational Science Institute (ACTSI) collaborative grant, and (3) PHS grant (UL1 RR025008) from the Clinical and Translational Science Award Program, National Institute of Health, National Center for Research Resources. The authors are very grateful to Dr. Judith A. Erlen (University of Pittsburgh School of Nursing) and Dr. Venkat Narayan, K. M (Emory University Rollins School of Public Health) for their mentoring of Dr. EunSeok Cha. The authors also thank study staff, participants, and community partners.
Footnotes
Human Subjects Statement
This study received approval from Emory University Institutional Review Board (IRB00047820).
Conflict of Interest Statement
No conflict of interest
Contributor Information
EunSeok Cha, Emory University Nell Hodgson Woodruff School of Nursing, Atlanta, GA.
Kevin H. Kim, University of Pittsburgh Psychology in Education and Business Administration in the Joseph M. Katz Graduate School of Business, Pittsburgh, PA.
Hannah M. Lerner, Emory College, Atlanta, GA.
Colleen R. Dawkins, Emory University Nell Hodgson, Woodruff School of Nursing, Atlanta, GA.
Morenike K. Bello, Emory University Rollins School of Public Health, Atlanta, GA.
Guillermo Umpierrez, Emory University School of Medicine, Atlanta, GA.
Sandra B. Dunbar, Emory University Nell Hodgson Woodruff School of Nursing, Atlanta, GA.
REFERENCES
- 1.Nelson MC, Story M, Larson NI, et al. Emerging adulthood and college-aged youth: an overlooked age for weight-related behavior change. Obesity (Silver Spring, Md) 2008;16(10):2205–2211. doi: 10.1038/oby.2008.365. [DOI] [PubMed] [Google Scholar]
- 2.Center for Disease Control and Prevention [Accessed September 5, 2013];National Diabetes Fact Sheet. 2011 Available: http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf.
- 3.Finkelstein EA, Trogdon JG, Cohen JW, et al. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff. 2009;28(5):w822–831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 4.Eborall H, Davies R, Kinmonth AL, et al. Patients’ experiences of screening for type 2 diabetes: prospective qualitative study embedded in the ADDITION (Cambridge) randomised controlled trial. BMJ. 2007;335(7618):490. doi: 10.1136/bmj.39308.392176.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Kit BK, et al. [Accessed September 5, 2013];Prevalence of obesity in the United States, 2009-2010. Available: http://www.cdc.gov/nchs/data/databriefs/db82.htm.
- 6.Schulze MB, Hoffmann K, Manson JE, et al. Dietary pattern, inflammation, and incidence of type 2 diabetes in women. Am J Clin Nutr. 2005;82(3):675–684. doi: 10.1093/ajcn.82.3.675. quiz 714-675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holm-Denoma JM, Joiner TE, Vohs KD, et al. The “freshman fifteen” (the “freshman five” actually): predictors and possible explanations. Health Psychol. 2008;27(1 Suppl):S3–9. doi: 10.1037/0278-6133.27.1.S3. [DOI] [PubMed] [Google Scholar]
- 8.Storcksdieck Genannt Bonsmann S, Wills JM. Nutrition Labeling to Prevent Obesity: Reviewing the Evidence from Europe. Curr Obes Rep. 2012;1(3):134–140. doi: 10.1007/s13679-012-0020-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Campos S, Doxey J, Hammond D. Nutrition labels on pre-packaged foods: a systematic review. Public Health Nutr. 2011;14(8):1496–1506. doi: 10.1017/S1368980010003290. [DOI] [PubMed] [Google Scholar]
- 10.Rothman RL, Housam R, Weiss H, et al. Patient understanding of food labels: the role of literacy and numeracy. Am J Prev Med. 2006;31(5):391–398. doi: 10.1016/j.amepre.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 11.U. S. Department of Agriculture and U. S Department of Health and Human Service . Dietary guidelines for American 2010. US Government Printing Office; Washinton DC: 2010. [Google Scholar]
- 12.Roberto CA, Shivaram M, Martinez O, et al. The Smart Choices front-of-package nutrition label. Influence on perceptions and intake of cereal. Appetite. 2012;58(2):651–657. doi: 10.1016/j.appet.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 13.Levi A, Chan KK, Pence D. Real men do not read labels: the effects of masculinity and involvement on college students’ food decisions. J Am Coll Health. 2006;55(2):91–98. doi: 10.3200/JACH.55.2.91-98. [DOI] [PubMed] [Google Scholar]
- 14.Misra R. Knowledge, attitudes, and label use among college students. J Am Diet Assoc. 2007;107(12):2130–2134. doi: 10.1016/j.jada.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 15.Guthrie JF, Fox JJ, Cleveland LE, et al. Who uses nutrition labeling, and what effects does label use have on diet quality? J Nutr Educ. 1995;27(4):163–172. [Google Scholar]
- 16.Huang TT, Kaur H, McCarter KS, et al. Reading nutrition labels and fat consumption in adolescents. J Adolesc Health. 2004;35(5):399–401. doi: 10.1016/j.jadohealth.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Huizinga MM, Carlisle AJ, Cavanaugh KL, et al. Literacy, numeracy, and portion-size estimation skills. Am J Prev Med. 2009;36(4):324–328. doi: 10.1016/j.amepre.2008.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Network of Libraries of Medicine [Accessed April 29, 2013];Health Literacy. Available: http://nnlm.gov/outreach/consumer/hlthlit.html.
- 19.Adams RJ, Piantadosi C, Ettridge K, et al. Functional health literacy mediates the relationship between socio-economic status, perceptions and lifestyle behaviors related to cancer risk in an Australian population. Patient Educ Couns. 2013;91(2):206–212. doi: 10.1016/j.pec.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 20.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 21.Bandura A. Human Agency in Social Cognitive Theory. 1989;44(9):1175–1184. doi: 10.1037/0003-066x.44.9.1175. [DOI] [PubMed] [Google Scholar]
- 22.Resnick B. Self-efficacy. In: Peterson SJ, Bredow TS, editors. Middle range theories. Lippincott Williams & Wilkins; New York: 2004. [Google Scholar]
- 23.Linde JA, Rothman AJ, Baldwin AS, et al. The impact of self-efficacy on behavior change and weight change among overweight participants in a weight loss trial. Health Psychol. 2006;25(3):282–291. doi: 10.1037/0278-6133.25.3.282. [DOI] [PubMed] [Google Scholar]
- 24.Tobias DK, Hu FB, Chavarro J, et al. Healthful dietary patterns and type 2 diabetes mellitus risk among women with a history of gestational diabetes mellitus. Arch Intern Med. 2012;172(20):1566–1572. doi: 10.1001/archinternmed.2012.3747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.American Diabetes Association Standards of medical care in diabetes-2013. Diabetes care. 2013;36(Sppl 1):S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Graham DJ, Laska MN. Nutrition label use partially mediates the relationship between attitude toward healthy eating and overall dietary quality among college students. J Acad Nutr Diet. 2012;112(3):414–418. doi: 10.1016/j.jada.2011.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gores SE. Addressing nutritional issues in the college-aged client: strategies for the nurse practitioner. J Am Acad Nurse Pract. 2008;20(1):5–10. doi: 10.1111/j.1745-7599.2007.00273.x. [DOI] [PubMed] [Google Scholar]
- 28.National Institutes of Health Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. National Institutes of Health. Obes Res. 1998;6(Suppl 2):51S–209S. [PubMed] [Google Scholar]
- 29.Weiss BD, Mays MZ, Martz W, et al. Quick Assessment of Literacy in Primary Care: The Newest Vital Sign. Ann Fam Med. 2005;3(6):514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clark MM, Abrams DB, Niaura RSE, C A, et al. Self-efficacy in weight management. J Consult Clin Psychol. 1991;59:739–744. doi: 10.1037//0022-006x.59.5.739. [DOI] [PubMed] [Google Scholar]
- 31.Rockett HR, Breitenbach M, Frazier AL, et al. Validation of a youth/adolescent food frequency questionnaire. Prev Med. 1997;26(6):808–816. doi: 10.1006/pmed.1997.0200. [DOI] [PubMed] [Google Scholar]
- 32.Rockett HR, Wolf AM, Colditz GA. Development and reproducibility of a food frequency questionnaire to assess diets of older children and adolescents. J Am Diet Assoc. 1995;95(3):336–340. doi: 10.1016/S0002-8223(95)00086-0. [DOI] [PubMed] [Google Scholar]
- 33.Fung TT, McCullough ML, Newby PK, et al. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr. 2005;82(1):163–173. doi: 10.1093/ajcn.82.1.163. [DOI] [PubMed] [Google Scholar]
- 34.Newby PK, Hu FB, Rimm EB, et al. Reproducibility and validity of the Diet Quality Index Revised as assessed by use of a food-frequency questionnaire. Am J Clin Nutr. 2003;78(5):941–949. doi: 10.1093/ajcn/78.5.941. [DOI] [PubMed] [Google Scholar]
- 35.Lutsey PL, Steffen LM, Stevens J. Dietary intake and the development of the metabolic syndrome: the Atherosclerosis Risk in Communities study. Circulation. 2008;117(6):754–761. doi: 10.1161/CIRCULATIONAHA.107.716159. [DOI] [PubMed] [Google Scholar]
- 36.McCullough ML, Feskanich D, Stampfer MJ, et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am J Clin Nutr. 2002;76(6):1261–1271. doi: 10.1093/ajcn/76.6.1261. [DOI] [PubMed] [Google Scholar]
- 37.Van Horn L. Development of the 2010 US Dietary Guidelines Advisory Committee Report: perspectives from a registered dietitian. J Am Diet Assoc. 2010;110(11):1638–1645. doi: 10.1016/j.jada.2010.08.018. [DOI] [PubMed] [Google Scholar]
- 38.Sharif I, Blank AE. Relationship between child health literacy and body mass index in overweight children. Patient Educ Couns. 2010;79(1):43–48. doi: 10.1016/j.pec.2009.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vernon JA, Trujillo A, Rosenbaum S, et al. [Accessed May 1, 2013];Low health literacy: Implications for national health policy. Available: http://sphhs.gwu.edu/departments/healthpolicy/CHPR/downloads/LowHealthLiteracyReport10_4_07.pdf.