Abstract
Background
Hospitals are constantly being challenged to provide high-quality care despite ageing populations, diminishing resources, and budgetary restraints. While the costs of care depend on the patients' needs, it is not clear which patient characteristics are associated with the demand for care and inherent costs. The aim of this study was to ascertain which patient-related characteristics or models can predict the need for medical and nursing care in general hospital settings.
Methods
We systematically searched MEDLINE, Embase, Business Source Premier and CINAHL. Pre-defined eligibility criteria were used to detect studies that explored patient characteristics and health status parameters associated to the use of hospital care services for hospitalized patients. Two reviewers independently assessed study relevance, quality with the STROBE instrument, and performed data analysis.
Results
From 2,168 potentially relevant articles, 17 met our eligibility criteria. These showed a large variety of factors associated with the use of hospital care services; models were found in only three studies. Age, gender, medical and nursing diagnoses, severity of illness, patient acuity, comorbidity, and complications were the characteristics found the most. Patient acuity and medical and nursing diagnoses were the most influencing characteristics. Models including medical or nursing diagnoses and patient acuity explain the variance in the use of hospital care services for at least 56.2%, and up to 78.7% when organizational factors were added.
Conclusions
A larger variety of factors were found to be associated with the use of hospital care services. Models that explain the extent to which hospital care services are used should contain patient characteristics, including patient acuity, medical or nursing diagnoses, and organizational and staffing characteristics, e.g., hospital size, organization of care, and the size and skill mix of staff. This would enable healthcare managers at different levels to evaluate hospital care services and organize or reorganize patient care.
Introduction
As health expenditures continue to rise, hospitals are challenged to provide more efficient and affordable services without compromising on quality. Efficient and high-quality hospital care is generally determined by three aspects. First, the size and educational level of the medical and nursing staff [1], [2]; second, the organization of care [3]; and third, the number of patients treated and their disease severity [4].
Because healthcare costs and consequently its affordability are related to the severity of a patient's condition (need for health care), and to the services requested (demand for health care), it is important for hospital managers to identify the factors that determine the demand [5]. If these factors could be identified, managers would be able to generate information on cost issues and substantiate trends in the demand for hospital care services over time. Furthermore, university hospitals could better define their top-referral patient populations and plan for capacity and capability through staff levels and facility planning.
At present, it is still unclear which individual, and preferably objective, patient characteristics are associated with the demand for hospital care services and their inherent costs. In recent attempts to reveal these characteristics, the focus was on specific patient populations [6], or different reference standards were used for analysing the characteristics and produced conflicting results [7].
When searching for associations between patient characteristics and the demand for hospital care services, it is necessary to define ‘demand for hospital care services’ or the product of this demand, i.e., ‘use of hospital care services’. Although the WHO defines ‘demand for health services’ as: The health care expectations expressed by individuals or communities, a more detailed interpretation of the term is lacking. For the purpose of this review, we further define the term ‘demand for hospital care services’ as the need for medical treatment and nursing care (i.e. personnel costs for medical and nursing staff as well as costs for therapeutic and diagnostic interventions), as determined by the individual patient's diagnosis and wishes.
During the nineteen-eighties and nineties, researchers put effort into matching the demand for hospital care services with nursing supplies. This was fuelled by economic pressures (i.e. nursing shortages [8] and the knowledge that the amount of nursing care needed varies substantially between diagnosis-related groups (DRGs) [9]). The above resulted in various definitions for ‘nursing care’ as well as various ways of predicting the demand for, or the measurement of nursing care actually given [10]. Clinical nursing care is most clearly expressed as ‘nurse hours per patient day’ (NHPPD) [11]. It is also customary to use the term for the product of the demand for care, i.e., ‘nursing care intensity’ or ‘workload’, [10], [12] as measured with a range of patient classification systems (PCS). In addition, other methods have been proposed, such as DRG nurse costing models or nurse-patient ratios [13]. Although these methods are commonly used, they have been criticized because nurses do not perceive them as a reflection of the ‘real’ nursing workload and these methods do not take into account changes in practice, e.g., a rise in care complexity or nursing care intensity [13], [14]. In addition, NHPPD, DRG costing models, and nurse-patient ratios are merely a proxy for the nursing care offered (personnel staffing) with the underlying assumption that all patients and all patient days are equal in terms of the use of health services.
In the medical world, the use of hospital care services is generally measured by costs for care as determined by DRG costing models [7], or length of stay (LOS) [15]. However, it is widely known that the intensity of patient care, and therefore the utilization of health services, increases as the LOS is shortened. Furthermore, LOS is substantially influenced by non-medical, for example, organizational factors [16], [17] and therefore not useful as an expression of the demand for medical services.
In the most favourable case scenario, the utilization of clinical hospital care services is defined as costs made during hospitalization, including the costs incurred for medical, nursing, diagnostic and therapeutic services. However, considering the variety of the measures and the shortcomings of some of them, we decided to study the use of hospital care services by using hospitalization costs, nursing workload and nursing care intensity. We therefore conducted a systematic literature review to search for associations between factors or models and the patient's demand for medical and nursing hospital care services in non high-care hospital wards.
Methods
This systematic review was conducted according to the PRISMA Preferred Reporting Items for Systematic Reviews and Meta-analysis-statement [18].
Eligibility criteria
Articles were eligible if they: 1) explored associations between health status parameters or patient characteristics and the demand for hospital care services; 2) focused on hospitalized patients on general wards; and 3) used regression or correlation analyses to explore possible associations.
We applied no restrictions on study design, but excluded other reviews including systematic reviews and original studies that merely described relative measures such as staffing levels, health outcomes, or length of hospital stay.
Literature search and information sources
MEDLINE, Embase, CINAHL and Business Source Premier were searched from inception through June 2013 to find articles that predicted or explained the demand for hospital care services; there were no limits regarding publication status, date or language. The complete search strategy for each database is given in Appendix S1 (MEDLINE), Appendix S2 (Embase), and Appendix S3 (for CINAHL and Business Source Premier). The search was designed and conducted with the help of a clinical librarian.
Study Selection
Eligible articles were independently selected by two reviewers (HV and DU) based on the relevance of their titles and abstracts as retrieved by the search. If articles met the inclusion criteria, full-text versions of the articles were obtained and further scrutinized for eligibility by CO and JHV. Authors were contacted for irretrievable articles. HV and DU also made the final selection of articles to be included. CO was involved in any cases of disagreement where consensus was reached through discussion. The reference lists of included articles were checked to detect any potential additional studies. Also, experts in healthcare services research were asked for potentially eligible studies.
Study quality appraisal
The STROBE statement for cohort studies was used to assess the methodological quality of the included studies [19]. This standard contains general methodological aspects that are important and applicable to the studies included. Appraisal was undertaken by two reviewers independently (CO and JHV) and cross-checked afterwards. Quality items were judged as ‘−’ (not described) or ‘+’ (described) as according to the definition in the STROBE statement. Items scoring ‘+/−’ were partially present, e.g., when the study population was described in terms of the medical diagnosis rather than the patient characteristics.
Data extraction and data items
Data extraction was performed by using a predefined, structured data-abstraction sheet and was double-checked during the process by CO and JHV. The following data were extracted: author, year of publication, setting, research design, sample size and specialty, (resource) reference standard, possible associated factors, measures of association with the demand for hospital care services, expressed as correlation coefficient (ρ), beta-coefficient (β) of a linear regression analysis, or odds ratio (OR) as derived from a logistic regression analysis, including their p-values and 95% confidence intervals (CI). We also documented whether the associations given had been corrected for other factors by means of a multivariable analysis. Where there was some uncertainty about the data, CO and JHV contacted the authors by e-mail.
Data analysis
All models and factors in the included studies that were investigated for their association with the use of hospital care services were summarized. Associations were judged significant if P <0.05 or their CI did not enclose the value of 0 or 1.
Meta-analysis was intended if study designs, reference standards, and outcomes were homogeneous. Otherwise, the findings are described and categorized by the various models and factors found.
Results
Study selection and characteristics
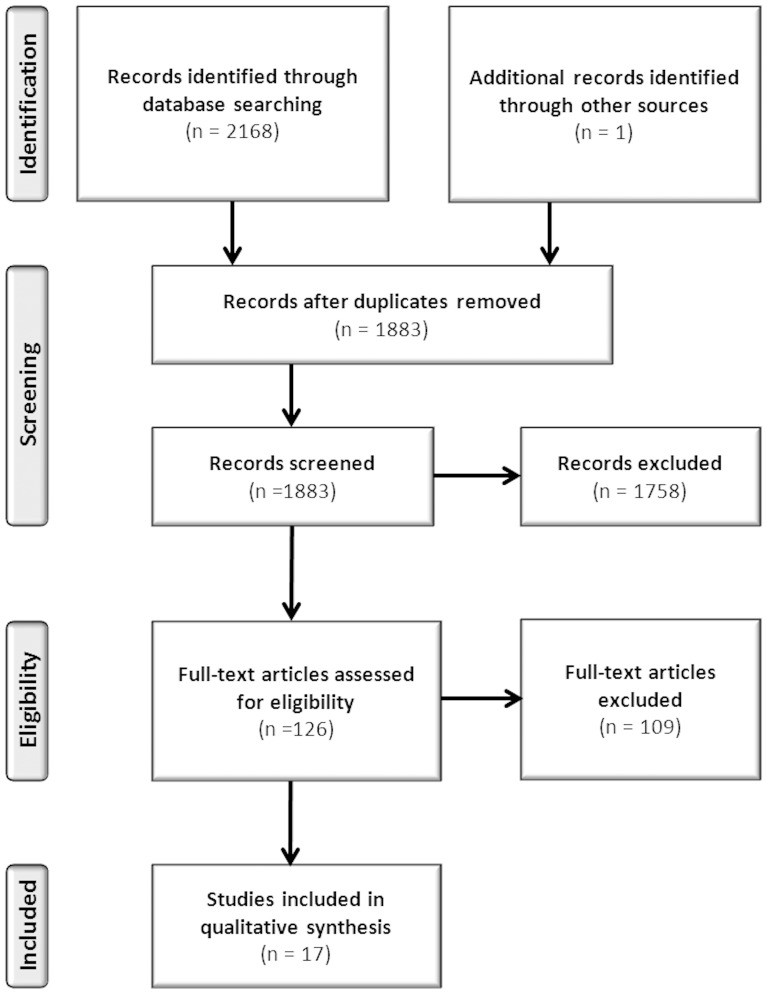
The search identified 2,168 studies from the four databases. After removing the duplicates and reviewing the titles and abstracts, 124 studies remained that met the inclusion criteria. Based on the full texts, a further 109 studies were excluded. Most of these studies (n = 83; 76%) did not report patient characteristics. For nine studies, all dissertations, the researchers received no reply to their queries for more information. Two authors replied to questions about their statistical analyses, but no extra data were obtained. One study was included after checking the references of one included publication. Another study was included because it was known by the researchers. Eventually, 17 studies were identified for this review (Figure 1).
Figure 1. Summary of search strategy.
The studies included (Table 1) were published between 1983 and 2013. Twelve out of the 17 studies (70%) had a retrospective design, while five studies (30%) were prospective cohort studies. Ten studies (59%) were conducted in the United States, five in Europe (30%) and two in Canada (11%). Data were taken from hospital sources including hospitalizations on different wards e.g. pulmonary, medical, surgery, obstetrics and gynaecology, intensive care, paediatrics, orthopaedics, geriatrics, and cardiology units. Study sizes ranged from 206 to 298,691 patients.
Table 1. Study characteristics.
| Author | Setting | Design | N, specialty | Resource | Reference standard | Predictive factors | Results | Corrected | Statistical analysis |
| Bostrom, 1991 | University hospital, United States, 600 beds | Retrospective | n = 1,372 patients | Medicus | average daily and total nursing hours per hospital stay | SII per DRG (14, 15, 89, 96, 138, 148, 182, 294, 320, 468) | daily range: r0.27 to r0.53 | NA | correlation |
| total range: r0.64 to r0.80 | |||||||||
| Bostrom, 1994 | University hospital, United States, 600 beds | Retrospective | n = 1,164 patients | Medicus | average daily and total nursing hours per hospital stay | SII per DRG (14, 15, 89, 96, 138, 148, 182, 294, 320, 468) | daily range: r20.04; NS to r20.30; p<0.001 | corrected for physician practice | multivariable regression analysis |
| total range: r20.17; p<0.05 to r20.49; p<0.001 | |||||||||
| Campbell, 1997 | Hospital, United Kingdom | Retrospective | n = 798 patients, respiratory medicine unit | TEAMWORK | weekly worked nursing hours | CMG cystic fibrosis | 18% | NA | univariable regression analysis |
| Caterinicchio, 1983 | 8 hospitals (5 teaching), New Jersey, range 155–550 beds | Prospective | n = 2,660, medical-surgical, obstetric-gynaecologic, psychiatric and intensive care units | RNEUSI (grand total minutes corrected for skill level) | nursing resource use | Age | r0.2326; P>0.0001 | NA | Pearson correlation analysis |
| Fagerström, 2000 | Hospital, Finland | Prospective | n = 19,324 OPC records, on 8 units: 3 internal, 2 surgical, 1 gynaecological and 2 paediatric units | PAONCIL | daily nursing workload measure for ward organization | OPC | r20.37 | multivariable regression analysis | |
| Age per ward | r20.001; NS | corrected for OPC score | |||||||
| r20.09; p0.0488 | |||||||||
| r20.064; p0.0008 | |||||||||
| Gender per ward | r20.006;p0.37 | ||||||||
| r20.000%; NS | |||||||||
| Geissler, 2012 | 712 hospitals, across 10 European countries: Finland, France, Germany, Spain, Sweden, Austria, Ireland, Poland, England and Estonia | Retrospective | n = 125,698 with hip replacement | national routine patient-level data samples from 2008 | hospitalization costs, admission to discharge | Age 1 (1–60) | range r20.068 to r2-0.004 | corrected for DRG 1–14 (ordered by weight), DRG other, no. of procedures and adverse events | multivariable regression analysis |
| Age 2 (61–70) | RC | ||||||||
| Age 3 (71–75) | range β0.017 to β-0.082 | ||||||||
| Age 4 (76–80) | range β0.051 to β-0.049 | ||||||||
| Age 5 (>80) | range β0.070 to β0.051 | ||||||||
| Gender | range β0.026 to β-0.007 | ||||||||
| No. of diagnoses | range β0.036 to β-0.013 | ||||||||
| Transfer in | range β0.114 to β-0.125 | ||||||||
| Transfer out | range β0.112 to β-0.071 | ||||||||
| Emergency | range β0.117 to β-0.053 | ||||||||
| Deceased | range β0.346 to β-0.233 | ||||||||
| CCI 1 | range β0.004 to β-0.030 | ||||||||
| CCI 2 | range β0.137 to β-0.060 | ||||||||
| Urinary tract infection | range β0.178 to β-0.396 | ||||||||
| Wound infection | range β1.474 to β-0.027 | ||||||||
| Fracture | range β0.110 to β-0.06 | ||||||||
| Partial replacement | range β0.019 to β-0.318 | ||||||||
| Revisions of implants | range β0.399 to β0.154 | ||||||||
| Halloran, 1985 | Hospital, United States, 279 beds | Retrospective | n = 2,560 patients, every adult patient both admitted and discharged to one hospital | Rush-Medicus patient classification | daily nursing workload measure | Age | r0.198; p<0.001; <4% | correlation, stepwise multivariable regression analysis | |
| Marital status | NS | ||||||||
| Payer | NS | ||||||||
| Age, sex & race | r20.043; p<0.001 | ||||||||
| DRG (3, 4, 11, 59, 75, 110, 121, 124, 132, 144, 156, 158, 189, 226, 227, 228, 264, 265, 266, 267, 271, 278, 282, 304, 322, 323, 348, 350, 355, 362, 382) | r20.263; p<0.0001; range β17.855 to β-19.138 | ||||||||
| Nursing diagnoses & DRG | r20.603; p<0.0001 | ||||||||
| Nursing diagnoses (37) | r2 0.532; range β0.158 to β-0.093 | ||||||||
| Mahmoud, 2009 | 196 hospitals, United States | Retrospective | n = 25,825 patients, adults undergoing elective colon procedures | Premier Perspective database | mean daily hospital costs (>US$15,000) (medical/surgical room and board, pharmacy, nursing, intensive care unit, central supply, laboratory, diagnostic imaging and operating room charges) | Surgical Site Infection | OR7.46 (CI 6.47–8.60) | corrected for antibiotic regimen | logistic regression analysis |
| Age > 65years | OR 1.71 (CI 1.61–1.82) | ||||||||
| Female sex | OR-0.87 (CI 0.8–0.93) | ||||||||
| Caucasian race | OR-0.81 (CI 0.75–0.86) | ||||||||
| BMI >30 | OR 1.29 (CI 1.19–1.40) | ||||||||
| High SENIC (risk of infection) score | OR 3.30 (CI3.02–3.70) | ||||||||
| McMahon, 1992 | University hospital, Michigan, United States | Retrospective | n = 1,920 patients, ICU, general medicine and medical subspecialty units | RVU (costs without non direct patient costs) | hospital resource consumption | DRG (89, 96, 125, 127, 138, 140, 182, 183, 296, 410, 112, 124, 320) | r20.10; p<0.0001 | stepwise multivariable regression analysis | |
| DRG and FIRST (first APACHE-L in 24hours of admission) | r20.14; p<0.0001; range r20.18–r20.00 | ||||||||
| DRG and FIRST WORST (worst APACHE-L in 24 hours) | r20.18; p<0.0001; range r20.23–r20.00 | ||||||||
| DRG and WORST (value having highest APACHE-L weight during admission) | r20.25; p<0.0001; range r20.38–r20.00 | ||||||||
| Mion, 1988 | Cleveland Metropolitan General/Highland View Hospital, Canada | Prospective | n = 351 patients, 4 general medical units, 28 beds | PAS | total nursing workload score | PSI | r0.60; p<0.0001 | corrected for LOS | Pearson's correlation, stepwise multivariable regression analysis |
| r20.48; p<0.0001 | |||||||||
| Age | r0.25; p0.0001 | ||||||||
| Gender | p<0.30 | ||||||||
| Race | p<0.30 | ||||||||
| Marital status | p<030 | ||||||||
| Admission source | r0.35, p0.0001 | ||||||||
| Discharge disposition | r0.54, p0.0001 | ||||||||
| O'Brien-Pallas, 1989 | University hospital, Canada, 1,000 beds | Prospective | n = 206 patients, diagnoses for diseases and disorders of the nervous system and circulatory system | GRASP; Medicus; PRN | daily and average nursing hours | CMG, LOS, age and sex | multivariable regression analysis | ||
| PRN | r20.58; p<0.0001 | ||||||||
| Medicus | r20.56; p<0.0001 | ||||||||
| GRASP | r20.57; p<0.0001 | ||||||||
| van Oostveen, 2013 | Academic medical center, The Netherlands, 1,000 beds | Prospective | n = 174 patients, surgical wards | time and motion research, hospital database | hospitalization costs (costs for physician services, nurse services, paramedics, all diagnostic tests, therapeutics, surgical procedures) | Age | β0.004; CI 0.001–0.007; p0.004 | univariable regression analysis, stepwise multivariable regression analysis | |
| Gender (males) | β-0.015; CI −0.118–0.87; p0.767 | ||||||||
| Number of co-morbidities | β0.000; CI −0.031–0.030; p0.978 | ||||||||
| Number of complications | β0.221; CI 0.144–0.299; p0.000 | ||||||||
| ASA-class | |||||||||
| 1 | RC | ||||||||
| 2 | β0.168; CI 0.057–0.279; p0.003 | ||||||||
| RC | |||||||||
| 3 | β0.234; CI 0.081–0.387; p0.003 | ||||||||
| β0.067; −0.071–0.204; p0.339 | |||||||||
| BMI at admission | β-0.006; CI −0.015–0.003; p0.189 | ||||||||
| Nutritional status | β0.018; CI 0.010–0.026; p0.000 | ||||||||
| Number of medications during hospitalization | β0.031; CI 0.022–0.040; p0.000 | ||||||||
| Admission type | β-0.210; CI −0.360–0.061; p0.006 | ||||||||
| Surgical specialty | |||||||||
| TRAUMA | RC | ||||||||
| URO | β0.776; CI 0.511–1.042; p0.000 | ||||||||
| ORTHO | β0.758; CI 0.505–1.012; p0.000 | ||||||||
| ABDO | β1.152; CI 0.900–1.405; p0.000 | ||||||||
| SHORT | β0.644; CI 0.368–0.920; p0.000 | ||||||||
| PLAST | β0.622; CI 0.381–0.943; p0.000 | ||||||||
| VASC | β0.786; CI 0.502–1.071; p0.000 | ||||||||
| ORAL | β0.679; CI 0.380–0.977; p0.000 | ||||||||
| Age, number of comorbidities, number of complications, number of medication during hospitalization, surgical specialty | r20.562; p<0.000 - β0.002; CI 0.000–0.005; p0.072/β-0.038; CI −0.064–0.012; p0.005/β0.072; CI 0.005–0.139; p0.036/β0.013; CI 0.004–0.023; p0.007/ range β1.005 to β0.610; p<0.001 | ||||||||
| Sermeus, 2008 | 115 acute hospitals, Belgium | Retrospective | n = 298,691 patients, ICU, surgical, internal medicine, geriatric and mixed surgical and internal medicine wards units | B-NMDS hospital financing and nurse staffing decisions | Prinqual 1; nurse care intensity | SJ | r20.70 | multivariable regression analysis | |
| Hospital type, hospital size, age, department type, DRG, severity of illness, DRG*severity of illness | r20.40 | ||||||||
| SJ, hospital type, hospital size, age, department type, DRG, severity of illness, DRG*severity of illness | r20.78 | ||||||||
| Shukla, 1992 | 84 community hospitals, United States, average 196 beds ranging between 50 and 670 beds | Retrospective | n = 84 community hospitals, medical-surgical units | actual staffing and skill mix data using standard hourly wages | nursing costs by staffing/skill mix per ward per day | Patient acuity (GRASP) | r0.18; p0.19 | NA | correlation |
| CMI | r0.38; p<0.01 | ||||||||
| GRASP | Patient acuity | Age | r0.26; p<0.05 | ||||||
| CMG | r0.12; p0.37 | ||||||||
| Titler, 2007 | One academic medical center, United States | Retrospective | n = 523 patients, >60 years older adults (568 hospitalizations) admitted for treatment for hip fracture or elective hip procedure | medical record database multiplied by cost to charge ratio hospital costs corrected for the fiscal year | hospital costs (general services, ICU/special care, pharmacy, laboratory, radiology, operating room, supplies and ancillary services) | Total number of medications | β0.0197; p<0.0001 (US$287,32 more costs) | corrected for nursing unit characteristics, medical treatments, individual treatments, individual medications, individual nursing interventions (fluid management, bathing, tube care and surgical preparation) | correlation, multivariable regression analysis - *only significant results given with direction of result of the correlation analysis |
| Depression | Β-0.0943; p0.0078 (US$1299,59 lower costs) | ||||||||
| Patient characteristics* | |||||||||
| Gender | p0.2306 | ||||||||
| Age | p0.0003+ | ||||||||
| Religion | p0.7334 | ||||||||
| Race | p0.4908 | ||||||||
| Marital Status | p0.5109 | ||||||||
| Occupation | p0.0630 | ||||||||
| Severity of illness | p<0.0001+ | ||||||||
| Medical diagnoses* | |||||||||
| Non traumatic joint disorders | p<0.0001− | ||||||||
| Complications of device, implant or graft | p<0.0001+ | ||||||||
| Comorbidities* | |||||||||
| Congestive heart failure | p0.0271+ | ||||||||
| Arrhythmias | p0.0137+ | ||||||||
| Valvular disease | p0.0043+ | ||||||||
| Pulmonary circulation disease | p0.0088+ | ||||||||
| Paralysis | p0.0098− | ||||||||
| Other neurological disorders | p0.0077+ | ||||||||
| Diabetes | p0.0155+ | ||||||||
| Peptic ulcer disease without bleeding | p0.0404+ | ||||||||
| Lymphoma | p0.0409+ | ||||||||
| Metastatic cancer | p0.0189+ | ||||||||
| Coagulopathy | p0.0043+ | ||||||||
| Obesity | p0.0791− | ||||||||
| Weight loss | p<0.0001+ | ||||||||
| Fluid and electrolyte disorders | p0.0102+ | ||||||||
| Chronic blood loss anaemia | p<0.0001+ | ||||||||
| Deficiency anaemia's | p0.1055+ | ||||||||
| Depression | p0.1263− | ||||||||
| Titler, 2008 | Academic medical center in the Midwest, 843 beds | Retrospective | n = 1,075 patients, >60 years older heart failure patients (1,435 hospitalizations) | medical record database multiplied by cost to charge ratio hospital costs corrected for the fiscal year | hospital costs (costs for general services, ICU/special care, pharmacy, laboratory, radiology, operating room, supplies and other ancillary services) | Age | NS | corrected for nursing unit characteristics, multidisciplinary treatments, individual medications and nursing interventions | correlation, generalised estimate equations |
| Gender | NS | ||||||||
| Ethnicity | NS | ||||||||
| Marital status | NS | ||||||||
| Religion | NS | ||||||||
| Occupation | NS | ||||||||
| Primary diagnosis | |||||||||
| Heart failure without hypertension | NS | ||||||||
| Acute myocardial infarction | NS | ||||||||
| Other cardiac conditions | NS | ||||||||
| Conduction disorders | NS | ||||||||
| Peripheral vascular disease | NS | ||||||||
| Non-cardiac circulatory diseases | NS | ||||||||
| Comorbidities | |||||||||
| Deficiency anaemia | β0.0500; p0.483 (US$536.00 more costs) | ||||||||
| Severity of illness | |||||||||
| Severe | β-0.0318; p0.6355 (-US$327.22 lower costs) | ||||||||
| Major | β-0.0062 ; p0.9187 (-US$64.62 lower costs) | ||||||||
| Moderate | β-0.0840; p0.1699 (-US$842.29 lower costs) | ||||||||
| Minor | RC | ||||||||
| Total number of different medications | β0.017; p<0.0001 (US$179.24 more costs) | ||||||||
| Wang, 2010 | US, dataset MarketScan Commercial Claims and Encounters inpatient | Retrospective | n = 23,216 heart failure related hospitalizations | dataset MarketScan Commercial Claims and Encounters inpatient | hospitalization costs (costs for physician services, all diagnostic tests, therapeutics, supplies and room fees) | Age | corrected for urban, region, LOS and secondary diagnosis | multivariable regression analysis | |
| 18–39 years | US$388; p0.689 | ||||||||
| 40–54 years | US$962; p0.038 | ||||||||
| 55–64 years | RC | ||||||||
| Gender | US$4316.7; p<0.001 | ||||||||
| CCI | US$229.5; p0.047 |
B-NMDS = Belgium Nursing Minimal Data Set, BMI = Body Mass Index, CCI = Charlson Comorbidity Index, CMG = Case Mix Group, CMI = Case Mix Index, DRG = Diagnose Resource Group, GRASP = Grace Reynolds Application and Study of PETO, LOS = Length of Stay, NANDA = North American Nursing Diagnosis Association, NA = not applicable, NS = not significant, OPC = Oulu Patient Classification, OR = Odds Ratio, PAS = Patient Acuity Scale, PAONCIL = Professional Assessment of Optimal Nursing Care Intensity Level, PRN = Project Resource Nursing, Prinqual 1 = self-care (dependency level), PSI = Patient Severity Index, RC = reference category, RNEUSI = Registered nurse equivalents Units of Service index, RVU = relative value unit, SENIC = Study of the Efficacy of Nosocomial Infection Control, SII = Horn's Severity of Illness index, SJ = San Joaquin
From the 17 studies, various factors associated with the demand for hospital care services were investigated. These comprised patient characteristics [7], [12], [20], [21], [22], [23], [24], [25], [26], [27], Case Mix Group (CMG), DRG (Appendix S4), nursing diagnoses [7], [21], [24], [28], [29], [30] (Appendix S4), severity of illness [9], [22], [23], [25], [26], [30], [31], [32] (Appendix S5), patient acuity [12], [24], [30] (Appendix S5), comorbidities [7], [23], complications [7], [23], [25], [26], [33] and admission and discharge factors [22]. Three studies [21], [23], [30] investigated models estimating the demand for hospital care services.
Different outcomes were used to determine the amount of hospital care services demanded: five studies used nursing hours spent [9], [28], [29], [31], two studies used resource consumption [20], [32], three studies used nursing workload [12] or nursing workload as measured by a PCS [21], [22], Sermeus et al. [30] only used nursing care intensity, and seven studies used hospitalization costs [7], [23], [24], [25], [26], [27], [33]. Physician services, if investigated at all, were done so only indirectly.
As a result, only factors tested in multivariable analyses and individual factors (i.e. univariable and correlation analyses) are described. For the results of all univariable analyses and correlations between the utilization of hospital care services and associated factors please see Table 1. Because of large range of definitions of demand for health care services, we refrained from doing a meta-analysis.
Methodological quality of studies
Overall, the methodological quality of the included studies was moderate to good (Table 2). Rationale, participants, variables and level of measurement, sample size and statistical methods were clearly reported. However, only eight (47%) studies mentioned their study design and provided an informative abstract. As most studies used large databases, the assessment of bias was hardly possible and limited to the data validation as reported by the investigators. Only six studies (35%) explained how missing data were handled, and in eight (56%) studies the characteristics of study participants were described. Seven studies that described the number of DRGs included, scored this as ‘partially present’ (31%). The precision of adjusted and unadjusted estimates was given in eight studies (47%).
Table 2. Methodological quality assessment.
| STROBE items* | 1 | 2 | 3 | 4 | 5 | 6a | 7 | 8 | 9 | 10 | 12a | 12b | 12c | 14a | 16a | 17 | 18 | 19 | 20 | 21 | 22 |
| Bostrom, 1991 | - | + | + | - | + | + | + | + | +/− | + | + | + | + | +/− | +/− | - | + | - | + | + | - |
| Bostrom, 1994 | - | + | + | - | + | + | + | + | + | + | + | + | - | +/− | + | + | + | + | - | + | - |
| Campbell, 1997 | + | + | + | + | +/− | + | + | + | + | + | + | + | + | - | - | - | + | + | +/− | + | - |
| Caterinicchio, 1983 | + | + | + | + | + | + | + | +/− | + | + | + | + | + | + | + | + | + | - | - | + | + |
| Fagerström, 2000 | + | + | + | + | + | + | + | + | + | + | + | + | +/− | NA | +/− | + | + | + | +/− | - | - |
| Geissler, 2012 | +/− | + | + | + | + | + | + | + | - | + | + | + | - | +/− | + | + | - | + | - | - | - |
| Halloran, 1985 | + | + | + | + | + | + | + | + | + | - | + | + | + | + | +/− | + | + | + | - | + | + |
| Mahmoud, 2009 | +/− | + | + | + | + | + | + | + | - | + | + | + | - | + | + | + | + | + | + | - | + |
| McMahon, 1992 | +/− | + | + | + | + | + | +/− | + | + | + | + | + | - | - | +/− | + | + | + | - | - | + |
| Mion, 1988 | - | + | + | + | + | + | + | + | + | + | + | + | - | + | +/− | + | + | - | + | + | - |
| O’Brien-Pallas, 1989 | +/− | + | + | + | + | + | + | + | + | + | + | + | - | - | +/− | + | + | + | + | + | - |
| van Oostveen, 2013 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Sermeus, 2008 | + | + | + | + | + | + | + | + | + | + | + | + | - | + | +/− | + | + | + | + | + | + |
| Shukla, 1992 | +/− | + | + | + | +/− | + | + | + | - | - | + | +/− | - | +/− | - | + | + | + | + | + | - |
| Titler, 2007 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | - | + |
| Titler, 2008 | + | + | + | + | + | + | + | + | + | + | + | + | - | +/− | + | + | + | + | + | + | + |
| Wang, 2010 | +/− | + | +/− | + | + | + | + | + | +/− | + | + | + | - | + | + | + | +/− | + | + | - | + |
| Percentage positive judgments | 47% | 100% | 94% | 88% | 88% | 100% | 94% | 94% | 71% | 88% | 100% | 94% | 35% | 56% | 47% | 88% | 88% | 82% | 59% | 65% | 53% |
*1. title and abstract, 2. background, 3. objectives, 4. study design, 5. setting, 6. participants, 7. variables, 8. data sources/measurement, 9. bias, 10. study size, 11. quantitative variables, 12 statistical methods, 14a. descriptive data, 16a. main results, 17. other analyses, 18. key results, 19. limitations, 20. interpretation, 21. generalizability, 22. funding. Items 12d, 12e, 13, 14 b, 14c, 15, 16b en 16c were not applicable for assessing the included studies.
+ = present, +/− = partially present, - = not present, NA. = not applicable.
Models
Three models were found that could predict the use of hospital care services to a certain extent [21], [23], [30]. Halloran [21] reported a model comprising the patient's age, gender, and race, which explained only 4.3% of the nursing workload. In addition, Halloran described a model with nursing diagnoses and DRGs that explained 60% of the nursing workload as measured by a PCS. More than 20 years later, Sermeus et al. [30] could explain 78.7% of nursing care intensity as measured by a Nursing Minimal Data Set (NMDS) Prinqual 1, including hospital type, hospital size, department type, patient's age, San Joaquin system scores, DRG, and the interaction between DRG and severity of illness. By removing the San Joaquin scores, the model explained only 40.8% of nursing care intensity. Recently, van Oostveen et al. [23] reported a model comprising age, medication during hospitalization, complications, co-morbidity and medical specialty, explaining 56.2% of hospitalization costs for surgical patients.
Individual patient characteristics
Five studies reported different results on the association between age and the use of hospital care services. Geissler et al. [7] reported a significant association between age and hospitalization costs (younger patients <61 years were more costly), while Mahmoud et al. [33] found older patients (>65 years) more likely to account for hospitalization costs over USD 15.000. Fagerström et al. [12] and Wang et al. [27] found that age contributed slightly but significantly to nursing workload and hospitalization costs. The study by Oostveen et al. [23] reported that age had no significant influence on hospitalization costs.
Three studies investigated the association of gender, race and BMI with costs. Geissler et al. [7] found lower costs for women than for men in three out of the seven countries investigated. This result was confirmed by Mahmoud et al. [33] and Wang et al. [27]. Additionally, Mahmoud et al. [33] found a decrease in costs for Caucasian patients and a cost increase for patients with a higher BMI score (>30).
Diagnosis, DRG, CMG, case mix index & nursing diagnoses
DRGs and CMGs contributed 10% to hospital resource consumption [32] 18% to nursing hours [28], and 26.3% to nursing workload as measured by a PCS [21]. Sermeus et al. [30] performed a regression analysis including DRGs and a possible interaction between DRGs and severity of illness, but no significant interaction was found.
DRGs and nursing diagnoses together explained 60% of the variance for nursing workload as measured by a PCS. Nursing diagnoses alone contributed 53.2% [21]. One study [7] reported significantly more costs for hip replacement in patients with fractures (in three out of seven countries studied), lower costs in patients receiving a partial replacement (4/7 countries) and higher costs for revision of a hip implant (7/7) (Table 1). Van Oostveen et al. [23] found that the surgical specialties urology, orthopaedics, gastro-intestinal surgery, short-stay surgery, plastic surgery, vascular surgery and oral and maxillofacial surgery, as proxies for diagnosis, were more costly than trauma surgery. All specialties together explained 46% of the variance for hospitalization costs.
Severity of illness/Physical health status
Severity of illness as measured by Susan Horns' Patient Severity Index (Appendix S5) contributed 48% to nursing workload as measured by a PCS [22]. The contribution of severity of illness to nursing hours varied widely per DRG (total range 17% to 49%) [31]. McMahon et al. [32] also found wide ranges for laboratory measurements, as a proxy for severity of illness, in the different DRGs. Although Titler et al. [26] showed a significant correlation between severity of illness and costs, they found no further significant differences in costs in their final model between different levels of severity.
Patient acuity
Sermeus et al. [30] found the San Joaquin scores could explain most of the variance (70%) of nursing intensity, while Fagerström et al. [12] found their PCS contributed only 37% to nursing workload.
Comorbidity and Complications
Two studies assessed comorbidity via the Charlson comorbidity index (CCI) in association with hospitalization costs [7], [27]. One of these studies found contradictory results [7] whereas Wang et al. [27] found an increase in hospitalization costs of USD 229.50 per index shift in the CCI. Patients with hip fractures and depression as comorbidity had reduced hospital costs by an average of USD 1299.59 [25]. In heart failure patients, only one comorbidity (deficiency anaemia) was associated with higher hospital costs (USD 536.00) [26]. The quantity of different medications being used by patients were also related to hospital costs [25], [26]. Geissler et al. [7] revealed higher costs for the total number of diagnoses as well as for urinary tract complications or wound infection. Van Oostveen et al. [23] reported significant effects of the total number of comorbidities −9%, complications +18%, and quantity of medications −3%, on hospitalization costs. For patients with high SENIC risk scores (Appendix S5) for surgical wound infections, the chance of costs rising above USD 15.000 was three times higher than in patients with low or moderate scores [33].
Correlation
In five studies factors in their univariable or correlational analyses were used without testing them in multivariable analyses. Mion et al. [22] and van Oostveen et al. [23] reported a significant association between admission type (elective and emergency) and the hospital care services used. Mion et al. [22] also found a significant positive relationship for the type of discharge. Four research teams tested marital status [21], [22], [25], [26], religion and occupation [25], [26] as possible influencing factors, but no significance was found. The payer was also found not to influence nursing workload significantly [21].
The American Society of Anesthesiologists (ASA)-class was used by van Oostveen et al. [23] to measure the physical health status of patients. They found only two categories (1-2/1-3) of ASA-classes significantly associated with hospitalization costs.
Fourteen out of 30 specific comorbidities recorded in patients diagnosed with hip fractures were positively associated with hospital costs [25], while three comorbidities, i.e. depression, paralysis and obesity, showed a negative correlation. Primary diagnoses in heart failure patients were found not to influence hospital costs significantly [26].
Discussion
This systematic review of 17 studies shows that the use of hospital care services is both defined and composed (i.e., financial components) differently across countries, disciplines and studies. Both organization-related and patient-related factors contribute to the use of hospital care services. In particular, age, gender, medical diagnosis, nursing diagnosis, severity of illness, patient acuity, comorbidity, and complications have been investigated the most and have been found to be associated significantly with the use of hospital care services.
The best combination of factors, explaining nearly 80% of the nursing care intensity, contained hospital type, hospital size, department type, age, severity of illness, DRG, and the San Joaquin system score [30]. However, this model contains patient characteristics as well as organizational factors, and explains nursing rather than medical services used. The second best model [23], containing only patient characteristics, explained 56.2% of the use of hospital care services. This implies that a combination of patient characteristics, including patient acuity, and organizational factors, results in the best model for explaining the use of hospital care services.
All models found examined individual patient characteristics as explanatory factors for the use of hospital care services, which suggests that these characteristics are important predictors for care demand. The characteristics found in this review can be used as predictors if they are known prior to a patient's admission, or as explanatory factors if they occur during admission, for example, to monitor trends in time regarding the demand for care. Therefore, the results of this review may be integrated into a practical dashboard for healthcare managers and policy-makers to manage and (re)organize their delivery of clinical hospital care at operational, tactic and strategic levels of decision-making. This will help substantiate their top-referral patient population, reorganize patient care, up-scale wards, planning budgets, capacity and capability, and evaluate the hospital care services themselves.
CMGs, DRGs and medical specialty [7], [23], [28], [30], [32] indicators for the medical diagnosis, were better suited for predicting the demand for hospital care services than the patient characteristics. Consequently, these indicators appear to be more suitable for explaining the use of hospital care services than individual diagnoses – apparently because the aggregate of this predictor corrects for variation at individual patient level. Nursing diagnoses [21] and the San Joaquin score for patient acuity [30], predicted the use of hospital care services even better than the indicators for the medical diagnosis. This seems plausible because nursing diagnoses and patient acuity scores contain similar elements regarding a patient's condition and aspects of nursing [21]. However, this characteristic cannot be derived easily from hospital databases, which poses difficulties to its practical application.
Contradictory results were found for factors like comorbidities and complications [7], [23], [25], [26], [27], [33]. In another review, Gijsen et al. stated that some negative associations found between comorbidity and the use of hospital care services may be due to the fact that the severity of the various comorbidities was not weighed in these studies [34]. Furthermore, less severe comorbidities may have been managed easily and less expensively with medication, while patients with more severe comorbidities may have had more expensive treatments.
One of the three models also addressed some organizational factors concerning hospital structure (e.g. hospital size, department type) [30]. Although the individual predictive values of most organizational factors were either not reported or small, they do determine efficient and high-quality hospital care [3]. Hence, these factors have to be included in any explanatory or prediction model for the use of hospital care services. This also holds for the size and educational level of the medical and nursing staff [1], [2], [35], but none of the studies in this review investigated these factors.
The limitations of this review are firstly, the heterogeneity of the reference standard ‘use of hospital care services’. Because hospitalization costs are defined differently in different countries, hospital databases are also set up differently resulting in the study aims being different. Hence, it is impossible to pool data and hardly possible to provide a clear result for each predictor. Secondly, the reference standard provides information on the amount of care delivered, which can be based on revenues rather than on the needs of patients [35]. Furthermore, the methodological quality of the included studies was fairly good, but 50% of the studies were somewhat dated. For instance, confidence intervals came into use during the nineteen-nineties [36] and were rarely reported earlier. Potential sources of bias and funding were also poorly reported, which may have flawed the validity of the results.
Conclusion
This systematic literature review has revealed several patient characteristics that are significantly associated with the need or demand for healthcare services in the hospital setting. The most prominent characteristics were age, gender, medical diagnosis and nursing diagnosis, severity of illness, patient acuity, comorbidity, and complications, most of which can be derived from hospital databases. Complete models that explain the use of hospital care services should contain patient characteristics, including patient acuity, medical or nursing diagnoses, organizational factors and staffing characteristics, as these factors do determine efficient and high-quality hospital care, and therefore the costs of care. These models appear useful for healthcare managers and policy-makers as predictors or to monitor trends in time regarding the demand for care.
Supporting Information
Search Embase.
(DOC)
Search MEDLINE.
(DOC)
Search CINAHL and Business Source Premier (EBSCO).
(DOC)
DRG –explanation.
(DOC)
Score explanation.
(DOC)
PRISMA checklist.
(DOC)
Acknowledgments
The investigators thank Faridi van Etten-Jahmaludin for her assistance in performing the literature search.
Funding Statement
The authors have no support or funding to report.
References
- 1. Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens SR, et al. (2011) Nurse staffing and inpatient hospital mortality. N Engl J Med. 364(11): 1037–45. [DOI] [PubMed] [Google Scholar]
- 2. Parikh A, Huang SA, Murthy P, Dombrovskiy V, Nolledo M, et al. (2012) Quality improvement and cost savings after implementation of the Leapfrog intensive care unit physician staffing standard at a community teaching hospital. Crit Care Med 40(10): 2754–9. [DOI] [PubMed] [Google Scholar]
- 3. Dubois C, d'Amour D, Tchouaket E, Clarke S, Rivard M, et al. (2013) Associations of patient safety outcomes with models of nursing care organization at unit level in hospitals. Int J Qual Health Care 25(2): 110–7. [DOI] [PubMed] [Google Scholar]
- 4. Mainz J (2013) Defining and classifying clinical indicators for quality improvement. Int J Qual Health Care 15(6): 523–30. [DOI] [PubMed] [Google Scholar]
- 5. Fries JF, Koop CE, Sokolov J, Beadle CE, Wright D (1998) Beyond health promotion: reducing need and demand for medical care. Health Affairs 17: 70–84. [DOI] [PubMed] [Google Scholar]
- 6. Robinson JC, Pozen A, Tseng S, Bozic KJ (2012) Variability in costs associated with total hip and knee replacement implants. J Bone Joint Surg Am 94(18): 1693–8. [DOI] [PubMed] [Google Scholar]
- 7. Geissler A, Scheller-Kreinsen D, Quentin W (2012) EuroDRG group (2012) Do diagnosis-related groups appropriately explain variations in costs and length of stay of hip replacement? A comparative assessment of DRG systems across 10 European countries. Health Econ 21 Suppl 2103–15. [DOI] [PubMed] [Google Scholar]
- 8. Giovannetti P, Johnson JM (1990) A new generation patient classification system. J Nurs Adm 20(5): 33–40. [PubMed] [Google Scholar]
- 9. Bostrom J, Mitchell M (1991) Relationship of direct nursing care hours to DRG and severity of illness. Nurs Econ 9(2): 105–111. [PubMed] [Google Scholar]
- 10. Morris R, MacNeela P, Scott A, Treacy P, Hyde A (2007) Reconsidering the conceptualization of nursing workload: literature review. J Adv Nurs (5): 463–471. [DOI] [PubMed] [Google Scholar]
- 11. Van den Heede K, Sermeus W, Diya L, Clarke SP, Lesaffre E, et al. (2009) Nurse staffing and patient outcomes in Belgian acute hospitals: cross-sectional analysis of administrative data. Int J Nurs Stud 46(7): 928–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fagerström L, Ainio A, Auhala A, Nojonen K (2000) Validation of a new method for patient classification, the Oulu Patient Classification. J Adv Nurs 31(2): 481–490. [DOI] [PubMed] [Google Scholar]
- 13. Twigg D, Duffield C (2009) A review of workload measures: a context for a new staffing methodology in Western Australia. Int J Nurs Stud 46(1): 131–9. [DOI] [PubMed] [Google Scholar]
- 14. Fasoli DR, Haddock KS (2010) Results of an integrative review of patient classification systems. Annu Rev Nurs Res 28: 295–316. [DOI] [PubMed] [Google Scholar]
- 15. Polverejan E, Gardiner JC, Bradley CJ, Holmes-Rovner M, Rovner D (2003) Estimating mean hospital cost as a function of length of stay and patient characteristics. Health Econ 12(11): 935–47. [DOI] [PubMed] [Google Scholar]
- 16. Ishak KJ, Stolar M, Hu M, Alvarez P, Wang Y, et al. (2012) Accounting for the relationship between per diem cost and LOS when estimating hospitalization costs. BMC Health Serv Res 1 12: 439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tump E, Maaskant JM, Brölmann FE, Bosman DK, Ubbink DT (2013) What brings children home? A prognostic study to predict length of hospitalisation. Eur J Pediatr 172(10): 1379–85. [DOI] [PubMed] [Google Scholar]
- 18.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 21;6(7) Available: http://www.prisma-statement.org/2.1.2%20-%20PRISMA%202009%20Checklist.pdf. Accessed 06-08-2013 [PMC free article] [PubMed]
- 19.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, et al. (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 16;4(10) Available: http://www.strobe-statement.org/fileadmin/Strobe/uploads/checklists/STROBE_checklist_v4_combined.pdf. Accessed 2013 Aug 6. [DOI] [PMC free article] [PubMed]
- 20. Caterinicchio RP, Davies RH (1983) Developing a client-focused allocation statistic of inpatient nursing resource use: an alternative to the patient day. Soc Sci Med 17(5): 259–72. [DOI] [PubMed] [Google Scholar]
- 21. Halloran EJ (1985) Nursing workload, medical diagnosis related groups, and nursing diagnoses. Research in Nursing & Health 8: 421–433. [DOI] [PubMed] [Google Scholar]
- 22.Mion LC, McLaren CE, Frengley JD (1988) The impact of patients' severity of illness and age on nursing workload. Nursing Management 19: : 26–8, 30, 32–3. [PubMed] [Google Scholar]
- 23. van Oostveen CJ, Vermeulen H, Gouma DJ, Bakker PJ, Ubbink DT (2013) Explaining the amount of care needed by hospitalised surgical patients: a prospective time and motion study. BMC Health Serv Res 4 13: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Shukla RK (1992) Factors and perspectives affecting nursing resource consumption in community hospitals. Health Serv Manage Res 5(3): 174–85. [DOI] [PubMed] [Google Scholar]
- 25. Titler M, Dochterman J, Kim T, Kanak M, Shever L, et al. (2007) Cost of care for seniors hospitalized for hip fracture and related procedures. Nurs Outlook 55(1): 5–14. [DOI] [PubMed] [Google Scholar]
- 26. Titler MG, Jensen GA, Dochterman JM, Xie XJ, Kanak M, et al. (2008) Cost of hospital care for older adults with heart failure: medical, pharmaceutical, and nursing costs. Health Serv Res 43(2): 635–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wang G, Zhang Z, Ayala C, Wall HK, Fang J (2010) Costs of heart failure-related hospitalizations in patients aged 18 to 64 years. Am J Manag Care 16(10): 769–76. [PubMed] [Google Scholar]
- 28. Campbell T, Taylor S, Callaghan S, Shuldham C (1997) Case mix type as a predictor of nursing workload. Journal of Nursing Management 5: 237–240. [DOI] [PubMed] [Google Scholar]
- 29. O'Brien-Pallas L, Tritchler D, Till J (1989) Variability in nursing workload within CMGs (case mix groups). Healthcare Management Forum/Canadian College of Health Service Executives 2: 26–31. [DOI] [PubMed] [Google Scholar]
- 30. Sermeus W, Delesie LK, Diya L, Lesaffre E (2008) Measuring the intensity of nursing care: making use of the Belgian Nursing Minimum Data Set. International Journal of Nursing Studies 45: 1011–1021. [DOI] [PubMed] [Google Scholar]
- 31. Bostrom JM (1994) Impact of physician practice on nursing care. Nursing Economic$ 12: 250–255. [PubMed] [Google Scholar]
- 32. McMahon LF Jr, Hayward RA, Bernard AM, Rosevear JS, Weissfeld LA (1992) APACHE-L: a new severity of illness adjuster for inpatient medical care. Med Care 30(5): 445–52. [DOI] [PubMed] [Google Scholar]
- 33. Mahmoud NN, Turpin RS, Yang G, Saunders WB (2009) Impact of Surgical Site Infections on Length of Stay and Costs in Selected Colorectal Procedures Surgical Infections. 10(6): 539–544. [DOI] [PubMed] [Google Scholar]
- 34. Gijsen R, Hoeymans N, Schellevis FG, Ruwaard D, Satariano WA, et al. (2001) Causes and consequences of comorbidity: A review. Journal of Clinical Epidemiology 54: 661–674. [DOI] [PubMed] [Google Scholar]
- 35. Aiken LH, Clarke SP, Sloane DM (2002) International Hospital Outcomes Research Consortium. Hospital staffing, organization, and quality of care: cross-national findings. Int J Qual Health Care 14(1): 5–13. [DOI] [PubMed] [Google Scholar]
- 36. Gardner MJ, Altman DG (1986) Confidence intervals rather than P values: estimation rather than hypothesis testing. Brit Med J. (Clinical Research Ed.) 292: 746–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search Embase.
(DOC)
Search MEDLINE.
(DOC)
Search CINAHL and Business Source Premier (EBSCO).
(DOC)
DRG –explanation.
(DOC)
Score explanation.
(DOC)
PRISMA checklist.
(DOC)