Abstract
Purpose
Little is currently known about how parents experience the medical genetics appointment at which their child receives a genetic diagnosis.
Methods
We conducted semi-structured in-person interviews with 13 parents of 10 index children to explore their experience in the medical genetics appointment in which they received their child’s genetic diagnosis. Guided by grounded theory, we used a constant comparative approach to data analysis, and the transcribed interviews were coded and sorted, and thematic categories identified.
Results
61.5% of parents experienced the diagnosis session as negative, 23% felt the experience was positive, and 15.5% were ambivalent. Receiving emotional support, an outline of the follow-up plans, and messages of hope and perspective during the session seemed to positively influence parents’ experience, while feeling that their role was as a passive receiver of information and using difficult medical terminology negatively influenced parents’ overall experience. Parental preparedness for the information, and the parents’ emotional reaction to the diagnosis were also factors that influenced the parental experience. Few participants understood the role of the genetic counselor.
Conclusion
Our results provide in-depth insight into the parental experience of the pediatric medical genetics diagnosis session. We propose a mechanism through which parental experience shapes their perception of the medical genetics session.
Keywords: Genetic diagnosis, parental experience, receiving bad news, pediatric genetics, genetic counseling
INTRODUCTION
Studies have highlighted the desire of parents to receive an etiological diagnosis in relation to their child’s severe developmental disability [Carmichael et al., 1999, Graungaard and Skov, 2007], and explored how parents value having a genetic diagnosis for their child [Makela et al., 2009] Other studies have investigated the parental experience of the referral process for pediatric genetics appointments [Skirton, 2006, Barr and McConkey, 2007]. However, although less is known about how parents experience receiving a genetic diagnosis for their child in the specific context of a medical genetics setting, some evidence suggests that these encounters may be suboptimal from the parental perspective.
First, a recent study [Waxler et al., 2013] used an online survey to explore the parental experience of receiving a diagnosis of Williams syndrome for their child. Respondents were not specifically asked whether or not they had received the diagnosis during an appointment at medical genetics, and many parents reported receiving the diagnosis from a pediatrician or other physician. However, over a third reported a primarily negative experience with the diagnostic process.
Second, though it did not specifically address the diagnostic appointment at medical genetics, a survey of parents whose children had been diagnosed with a chromosomal disorder revealed that respondents were disheartened by the genetics services they received [Lipinski et al, 1997]. Third, a review of doctor-patient communication in a genetic counseling setting in the UK suggested that the terminology used is often confusing and misunderstood by the families [Chapple et al, 2006]. Last, a discourse analysis of 10 pediatric genetics diagnosis appointments showed that the healthcare providers spoke more than the patients in majority of the sessions, and that the human voice of parents only emerged when counselors focused more on building rapport [Babul-Hirji et al., 2010]. This pattern of communication is potentially problematic given that the patient needs are best addressed and the best patient outcomes are achieved when the content of the session provides more space for the patients to speak [Meiser et al 2008].
Although much is known about the process of breaking bad news, (for reviews see: Minichiello et al., 2007, Schoefl 2008, Boyd 2001, Harrison and Walling, 2010), the data summarized above offer circumstantial and/or suggestive evidence that pediatric clinical genetics appointments may not be optimal from the parents’ perspective. To our knowledge, no studies to date have purposively and directly explored parental experiences of receiving a genetic diagnosis for their child in the specific context of a medical genetics encounter.
MATERIALS AND METHODS
We designed a qualitative semi-structured interview-based study, which was approved by the University of British Columbia Research Ethics Board and Children’s and Woman’s Health Centre of British Columbia (H12-01254), and was conducted at the Provincial Medical Genetics Program (PMGP) at Children’s and Women’s Hospital in Vancouver, British Columbia. The PMGP is a tertiary care centre that is staffed by 15 clinical geneticists (sharing 6 full time equivalents (FTEs) for clinical care) and 20 genetic counselors (sharing 15.5FTEs). The PGMP provides assessment, diagnoses, and genetic counseling for prenatal, pediatric and adult patients and their families referred for concerns about birth defects and/or genetic diseases. Access to the PGMP requires a physician referral. Pediatric cases (such as those that constitute the focus of this study) are typically ~1.5 hours in length, and usually involve both a geneticist and genetic counselor.
All participants had attended the PMGP to receive a genetic diagnosis for their child, were fluent in English, and had a child who was the first individual in the family to have been diagnosed with the condition. Participants were recruited through study advertisements directed towards the membership of the Rare Disease Foundation, and through review of PMGP charts. Specifically, study invitation packages were sent to parents who signed a consent form at the time of their child’s appointment to allow researchers to contact them about future research studies.
In-person interviews were conducted with eligible participants. The interview comprised questions to capture demographic information (age of child, time lapsed since diagnosis, and level of education of the parent), followed by a semi-structured interview consisting of prompts to explore: the participants’ experience of referral to medical genetics, the diagnosis session at the medical genetics department, views of and experience with genetics service provider, and the factors that they felt influenced their experience at the medical genetics clinic at the time of the diagnosis. Participants were encouraged to provide recommendations for improvements that could be made to the diagnosis session. All participants received a $25 thank you gift card for their participation.
The interviewer (SA) had past employment experience as a community support worker to individuals with developmental disabilities, and was in her second year of training for genetic counseling at the time of conducting the interviews. Interviews were audio-taped, transcribed verbatim and de-identified, including redaction of details about the identity of the genetics professionals (e.g. sex), and checked for accuracy. Guided by grounded theory methodology, we approached analysis of the data using a strategy of constant comparison, whereby data are collected and analyzed concurrently and each interview is informed by analysis of data from previous interviewees [Corbin 2008]. After multiple readings of the transcripts and making memos summarizing ideas, two of the co-investigators (SA and NM) independently coded, sorted, recoded and resorted to find recurring thematic categories, then met to discuss and reach consensus [Denzin 1989, Morgan 1998]. Participants were recruited until no further themes emerged (saturation).
RESULTS
Sample Characteristics
In total, 13 parents (10 mothers and three fathers) of 10 index children (5 male, and 5 female, eight of whom were 4 years old or younger, and two were 5 or older) were interviewed, parents of three index children were recruited through the Rare Disease Foundation, and the remainder was recruited through invitations sent following chart review at the PMGP. All participants were married and had some level of higher education, and three had medical backgrounds. The average age of the participants was 43.6, and most (62%) were Caucasian. The average time lapsed since their child’s diagnosis was 3.7 years. On average, the interviews lasted 45.4 minutes.
All of the index children had developmental delay and received care from multiple different specialists in the healthcare system. As diagnoses are each rare, to protect the anonymity of participants, we do not provide them here, but the genetic diagnoses of four of the index children were made through physical exam and/or karyotype/FISH analysis, and genetic diagnoses were established for six children through comparative genomic hybridization (CGH) array analysis. The genetic tests of three index children had been ordered by non-geneticists, but all families were sent to the PGMP to receive the specific results. Of these, the parent of one child knew that an abnormality of some kind had been found, and the parents of another were not aware that results were available at the time of their appointment.
With regards to the setting where the diagnosis was delivered, the parents of two index children received the diagnosis while their children were hospitalized as in-patients, while all others reported receiving the diagnosis at the genetics clinic and during a pre-scheduled appointment. All participants but one reported that their diagnosis session had been facilitated primarily by a geneticist, and while a genetic counselor was often reported to have been present, s/he was not perceived as having a particularly active role in the session. Indeed, lack of clarity around the role of the genetic counselor was common - most participants explicitly expressed uncertainty and curiosity regarding what the role of a genetic counselor was “supposed to be”, and three parents specially asked the interviewer during the interview process to explain the role of a genetic counselor. Two participants recalled that a resident or student was present during their appointment.
Overall Impressions: Good/Bad, Forgiveness/Appreciation
All parents found that receiving a genetic diagnosis for their child was a difficult experience, and 8/13 (61.5%) parents recalled the experience as essentially negative (e.g., “a really poor, poor experience”), three (23%) recalled the experience as primarily positive (e.g., “It [the diagnosis] was delivered in a very, very excellent way. I don’t have any complaints in how it was delivered to us”), and two (15.5%) recalled the experience as “different” and reported a combination of negative and positive experiences during the session; as one mother recalled: “It was very matter of fact. I remember it [being] weird”.
Many participants who felt their experiences were primarily negative expressed appreciation and forgiveness for the situation and the healthcare providers despite this, for example a father said: “but when you think about it, there are a lot of people who don’t have access to any of this [genetic expertise]. So, we are tremendously fortunate and appreciative.” Forgiveness was expressed by others, for example: “I think it could have been presented.... better but literally it was just a choice of language […] It’s a very difficult disease, this is the problem, to describe to people”.
Parents as Passive Receivers of Information
The majority of the participants recalled their Medical Genetics experience as one where their role was to passively receive information. For instance, a father recalled: “…we didn’t do much talking, just listening to what they had to say...” Some parents expressed frustration with this passive role: “…when [the geneticist] finally got to the end of what [s/he] was explaining to me and let me talk…” Sometimes this frustration was expressed passionately: “their focus was about whether we wanted to have a second child and you know, that’s all well and good but in that initial meeting, I care about this child […] honestly, I don’t give a flying fuck about my potential second child in this moment. We can deal with that later.”
Knowledge is Power?
A few parents expressed sentiments reflecting the adage that “knowledge is power”, for example: “So at least with us, we know [the diagnosis] and that gives me some reassurance at what kind of direction we’re getting into.” Most, however, expressed frustration and helplessness, and feelings that the knowledge was not empowering: “With genetics its like, we give you information and then it stops. But… there is no service from genetics. There is no program… It’s just information. And information without anything to follow it up doesn’t help you, doesn’t do anything for you.”
Emotional Response as a Barrier to Comprehension/Participation
Parents reported feelings ranging from shock, devastation, fear, and sadness, to relief. Most parents commented on the diagnosis session as a process in which their powerful emotional responses blocked their ability to process the information: “Ya, ‘cause when you get a diagnosis of anything you don’t know your head from your butt basically. You’re like so confused”. And another said: “it’s not that [the geneticist] wasn’t listening to us - because we weren’t saying anything. We were in shock right?” Parents identified a need for information to take away with them, as a result of the impact of their emotional response: “it’s helpful to have stuff you can look at a little bit later when you’re more ready to deal with it because you can only deal with so many things at one time right?”
The Importance of Attending to Parents’ Emotions
Only a handful of parents felt they had received emotional support during the diagnosis session, but all perceived their experience as positive. One mother recalled the emotional support that she was offered: “[the geneticist] said, you have to let yourself grieve on this, that you don’t have that perfect child that you want[ed]... And [the geneticist] was right.”
Other parents felt that the genetics service providers didn’t acknowledge their emotional responses or provide the counseling they would have wanted: “… the counseling, it wasn’t really, there was no counseling, so I don’t know why I really went.” Another parent said: “Tread lightly people. Ya, as I said it’s like, she might be your everyday but she’s my everything, [crying], I don’t think about it much any more. But I think it’s something that’s often lost sight of. It’s just sort of, ya, there’s the idiot kid in this room and that kid in that room and people lose sight of the gravity of the things they are saying...”
Perceptions of the Terminology
While the three parents who reported having a medical background were comfortable with the scientific description of the condition that was provided, there was acknowledgment that the language used could present problems for those without a medical background: “it’s a lot of garbley-goop if you don’t have any [medical] experience at all”. This was reinforced by sentiments expressed by parents with no medical background; for example, one father recalled how the terminology used had “floored” him: “ [phrases] like “hundreds of genes missing” […] “constellation of difficulties”, “chromosome deletion” you know, uh, there were all like these things that [the geneticist] said and I wrote them down, took them home.”
The Need for Hope
When parents felt that the manner in which the information was presented was hopeful, this was gratefully appreciated. For example: “I was just listening to [the geneticist] in shock but you know, when [s/he] said that [child] can go to school, just like normal, like you know, I felt like that’s not so bad. You know, I was just like, not as broken-hearted”. On the other hand, when parents felt that hope was absent in the manner in which the diagnosis was presented, it was identified as something they would very much have liked. A father described this as follows: “They could have said... well, just love her, try to teach her. She’ll learn something right? Would have been different hearing that… But what we kind of heard was like, she’s not going to learn nothing or do nothing. Kind of give up hope on her kind of thing…”
Another mother reflected on the message she wished she had received at the time of the diagnosis session: “this is going to be hard and your life is going to be a lot different but it’s going to be ok […] There’s great families and there’s great organizations and I think that message needs to be driven home solidly when you are getting that kind of news because, you need to know you’re going to be ok.”
The Need for a Broader Perspective
All parents expressed the desire for information with regards to the implications of a diagnosis beyond the affected child, for the family unit. As one parent put it: “I came out of that feeling like, “so what does this mean?” Now what do we do? What is the implication not, dealing with not just, [child’s] own physical health but what does it mean for us…”
Parents often reflected on the value that their child had brought to their lives. In fact, all parents who felt they had received information focusing on the negative aspects of the condition at the time of diagnosis contrasted this perspective with their lived experience of their child’s accomplishments and the value and joy s/he had brought to their lives. As one mother described: “in lots of ways, ya, we’re reminded about the preciousness of life and how, you know, how value can’t be measured in terms of IQ, or, and [our daughter] is very unconventionally smart [...] She understands lots of things, surprises us… I guess what I am saying is that it’s good to be cautious about the language of this being a big tragedy. Because, there is a whole person there and uh, many good things can come of living with such an unusual person.”
The Right Place at the Right Time
In cases when parents reported a primarily negative experience, recollections of the location and timing were sometimes vivid: “We were in the hospital ‘cause [child] had just had surgery in the morning and […] my husband and I were probably in our pajamas, we’re both leaning against the window sitting on the bed, and in comes the geneticist and says “By the way, we just found out, look what we found out!” […] and I remember we sat the whole time. They stood…”
The timing of a diagnosis was a theme present in most of the interviews, and in most cases it was in relation to the child’s circumstances (such as child’s age and physical health) at the time of diagnosis. Some parents spoke of “the right time” for, or being “ready” to receive the diagnosis. One mother who reported a positive experience recalled: “Maybe, just, we were ready for it.” In the same vein, another mother whose child went through a 5-year diagnostic odyssey said: “I had gone through so many things. So many tests and so many procedures, that this was just really nothing. I mean, maybe I was just actually relieved that “Ok, that’s it. No more tests and no more procedures.”
So, Now What?
When parents had established an on-going relationship with the genetics team this was associated with great satisfaction: “I never stop emailing [the geneticist] if I have questions. [laughs] I would always ask him/her for his/her view before I ask [other] specialists”. But many parents reported feeling uncertain regarding what sorts of questions they could call the medical genetics team with in follow-up, and whether there was an ongoing role for medical genetics in their child’s care: “What would have been nice to [know], I don’t really know what the role of Medical Genetics is in [daughter’s] future… Like, do we need to follow-up with them? And, I think I asked that at the time and they said “No, no, if you have questions you can come back” but, there was always, “it’s up to you.” […] So I don’t know… are they just there for diagnosis and then that’s it or is there more to it?”
DISCUSSION
The present study provides direct data regarding parents’ experiences of receiving their child’s genetic diagnosis, as delivered specifically in the context of a medical genetics appointment. Many elements of our work support and corroborate the findings of previous studies in related areas, but several additional elements seem to have emerged, and most importantly, our data offer a suggestion for a mechanism through which parental perception of their experience of the medical genetics diagnosis appointment is shaped.
Specifically, our data support and corroborate previous work in related areas in several important ways. First, all participants reported that receiving their child’s diagnosis was a difficult experience, but 61.5% of participants perceived their diagnostic experience as being primarily negative. In this, and in the importance to parents of receiving a message that includes hope, our findings are broadly comparable to those of Waxler et al [Waxler et al., 2013].
Second, as in previous studies, we found that the use of technical language was perceived as problematic by parents [Chapple et al, 2006,Reiff et al, 2012,Davies et al, 2003]. Third, consistent with previous findings in closely related areas [Barr and McConkey, 2007, Barr and Millar, 2003], parents in our study reported (some with considerable frustration) feeling that they were primarily passive receivers of information, and that there was not much opportunity to ask questions or raise their concerns. Fourth, as has been found in other settings, parents in this study felt that their emotions impaired their ability to process the information they received [Skotko, 2005]. Last, in agreement with previous work [Davies et al., 2003], lack of emotional support emerged as a strong theme in relation to sessions that were perceived as negative experiences, and conversely, when parental emotional reactions were acknowledged and addressed during the diagnosis session, parents reported their experiences as being more positive, and felt more able to respond to the information they received.
Some additional elements seem to have emerged from our data. Specifically, first, the location and timing of diagnosis emerged as having an important impact on the parental experience, with a pre-arranged meeting time and a private setting for delivery of the diagnosis being perceived as important. This provides further empirical support for published recommendations regarding how healthcare providers should approach the delivery of a diagnosis of Down syndrome to parents [Skotko et al., 2009, Dent and Carey, 2006], and suggests that translation of existing guidelines into clinical practice remains challenging [Dent and Carey, 2006].
Second, our data revealed a suggestion that diagnosis sessions were perceived less negatively by parents who had experienced a longer “diagnostic odyssey”, and that parents were perhaps more “ready” to receive a diagnosis. In general, of the parents who reported more positive experiences, the child’s first developmental concerns were initially noted some time before the diagnosis was delivered, and parents reported feeling more “ready”. Given that the expansion of newborn screening programs to include a broader range of conditions [Moyer et al., 2008], could result in many more diagnoses being made earlier, perhaps before the clear identification of developmental concerns, parents could be caught unprepared (not “ready”) for a diagnosis, so work may be needed to determine how best to ensure that these families have the best experience possible with receiving their diagnosis.
Third, the perception of the nature of the family’s relationship with medical genetics was an important factor in how parents remembered the diagnosis session, with all parents who reported an ongoing relationship with the geneticist reflecting positively on their diagnostic experience. But parental uncertainty at the time of the diagnosis about the role of medical genetics in their child’s care going forward seemed to correlate strongly associated with the report of a negative diagnostic experience. The stories shared by participants in this study suggest that it is not sufficient to encourage parents to “call anytime with questions”, and that it may be helpful to implement (and inform parents about) a routine post-appointment follow-up appointment or telephone call, or to provide parents with examples of the sorts of questions they could approach medical genetics with in the future.
Last, though it has previously been suggested that parents do not easily forget or forgive if the delivery of a genetic diagnosis is perceived negatively [Roche 2006], most of the participants in this study expressed much forgiveness, understanding, and appreciation towards medical genetics.
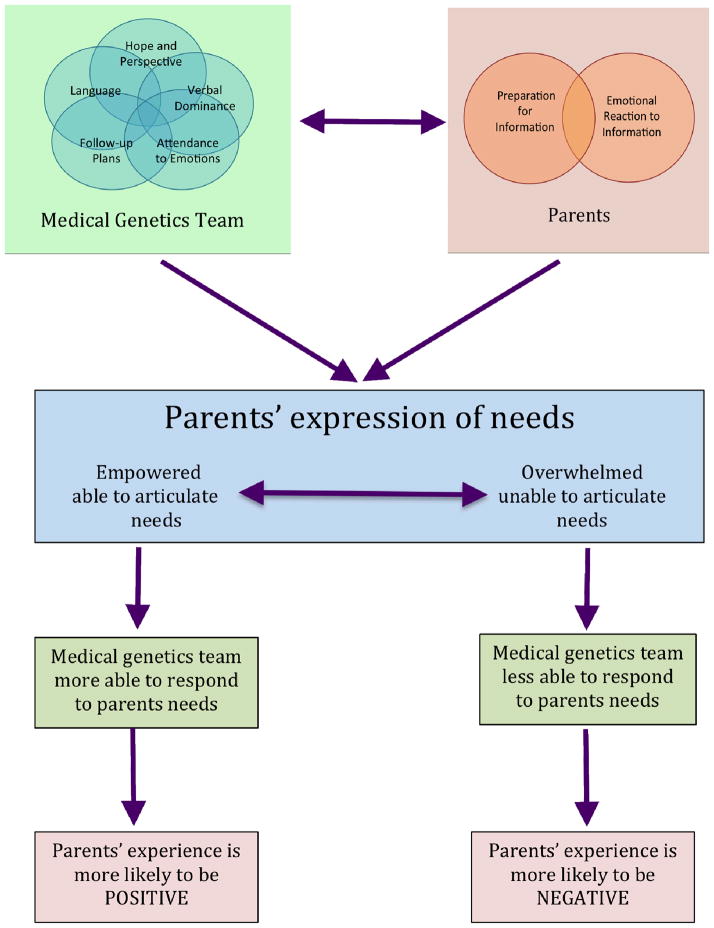
A Proposed Mechanism through which Parental Experience Shapes their Perception of the Medical Genetics Session
Most importantly, our data suggest a possible mechanism through which the parental experience of the medical genetics diagnosis session shapes their ultimate perception of it as being positive or negative (Figure 1). Though the model that emerged from our data is well supported by the existing literature, we are not aware of it having been articulated in this way previously.
FIGURE 1.
Model illustrating the factors shaping parents’ experience of receiving their child’s genetic diagnosis at the Medical Genetics clinic.
Specifically, it seems that the parents’ experiences tend to be perceived as negative when the medical genetics team is verbally dominant, and/or pays insufficient attention to uncovering and addressing parents’ emotions, and/or uses difficult language, and/or does not provide hope or perspective or explain follow-up plans. Particularly in circumstances when the emotional impact of the diagnosis is especially acute, and parents’ ability to process information and ask questions is impaired (for example, when parents are not adequately prepared or “ready” for a diagnosis), this may create a situation in which parents become overwhelmed, unable to articulate their needs, and become passive. The net result of these circumstances is that there is less probability of parents’ needs being met, which results in the diagnostic experience being perceived negatively.
On the other hand, more positive diagnostic experiences seem to be reported when the medical genetics team is less verbally dominant, and/or provide sufficient emotional support and counseling, and/or uses less jargon-intense language, and/or provide hope and perspective and explain follow-up plans. This is in addition to parents perceiving the emotional impact of the information as less significant, and/or when parents are either prepared (“ready”) for a diagnosis. These circumstances tend to create a net result whereby the parents’ ability to process information and ask questions is not as impaired, and they are able to take a more active role and articulate their needs, this increases the probability of the healthcare team meeting those needs, and thus the diagnostic experience as a whole is more likely to be perceived as positive.
Further exploration of the interaction between families and medical genetics healthcare providers is especially important given that studies have shown that these experiences can have a significant and long-term effect on parental coping [Davies et al., 2003, Taanila et al., 2002].
Waxler et al [Waxler et al., 2013] identified significant correlation between positive parental experience of their diagnostic experience and the presence of a genetic counselor and suggested that this was perhaps related to the extensive specialized training genetic counselors receive regarding the delivery of difficult news, providing emotional support and resources. In this study, although a genetic counselor was reported to have been present in most sessions, participants did not recall much interaction with them, and many were not clear on why the counselor had been present in the session other than to act as a contact person so that the parent did not directly contact the geneticist. Taken together with the data of Waxler [Waxler et al., 2013], one interpretation of our findings is that in this context, the genetic counselors in genetic diagnosis sessions may not be playing a sufficiently active role in the session for the emotional support that parents may require to be perceived. A larger role for the genetic counselor, and a focus on emotional support in pediatric diagnosis sessions may be one route through which parents’ experiences could be improved.
There are limitations to this study. First, given that this was a qualitative study involving participants who had all been seen at one genetics clinic, our findings are not generalizable. Second, the index children had a range of diagnoses, and the reactions experienced by parents may vary as a function of the exact nature of this diagnosis. Third, it is possible that the finding that a majority of parents recalled their experience negatively is a function of selection bias –perhaps parents who had a negative experience were more likely to choose to participate in our research. However, our results constitute the first in-depth insight into the parental experience of the pediatric medical genetics diagnosis session. Our data contest the idea that parents will always “shoot the messenger” (specifically, that parents will always have a negative experience at medical genetics when receiving their child’s diagnosis because the nature of the information received is “negative”), indeed, some parents explicitly stated that the experience was positive. Last, this was a retrospective study, and as such dependent on participants’ recollection. Our data also suggest an explanatory mechanism through which parental experience shapes their perception of the medical genetics session. Future research is warranted to determine whether parents’ perceptions of their experiences can be improved through paying explicit attention to the issues highlighted here, and to explore parents’ experiences of receiving different specific diagnoses.
Acknowledgments
We would like to express our sincere appreciation to all the parents who participated in this research, as well as to the Rare Disease Foundation, the Research Special Interest Group of the National Society of Genetic Counselors, and the Master of Science Program in Genetic Counseling at the University of British Columbia for supporting this work. JA was supported by the Canada Research Chairs Program, the Michael Smith Foundation for Health Research, and BC Mental Health and Addictions Services.
References
- Babul-Hirji R, Hewson S, Frescura M. A sociolinguistic exploration of genetic counseling discourse involving a child with a new genetic diagnosis. Patient Educ Couns. 2010;78(1):40–45. doi: 10.1016/j.pec.2009.06.007. [DOI] [PubMed] [Google Scholar]
- Barr O, Millar R. Parents of Children with Intellectual Disabilities: Their Expectations and Experience of Genetic Counselling. J Appl Res Intellect Disabil. 2003;16:189–204. [Google Scholar]
- Barr O, McConkey R. A different type of appointment: the experiences of parents who have children with intellectual disabilities referred for genetic investigation. J Res Nurs. 2007;12(6):637–652. [Google Scholar]
- Boyd JR. A process for delivering bad news: supporting families when a child is diagnosed. J Neurosci Nurs. 2001;33(1):14–20. doi: 10.1097/01376517-200102000-00003. [DOI] [PubMed] [Google Scholar]
- Carmichael B, Pembrey M, Barnicoat GTA. Diagnosis of fragile-X syndrome: the experiences of parents. J Intellect Disabil Res. 1999;43(Pt1):47–53. doi: 10.1046/j.1365-2788.1999.43120157.x. [DOI] [PubMed] [Google Scholar]
- Chapple A, Campion P, May C. Clinical Terminology: anxiety and confusion amongst families undergoing genetic counseling. Patient Educ Couns. 2006;32:81–91. doi: 10.1016/s0738-3991(97)00065-7. [DOI] [PubMed] [Google Scholar]
- Corbin JM, Strauss AL. Basics of Qualitative Research. 3. Los Angeles, CA: Sage; 2008. [Google Scholar]
- Davies R, Davis B, Sibert J. Parents’ stories of sensitive and insensitive care by paediatricians in the time leading up to and including diagnostic disclosure of a life-limiting condition in their child. Child Care Health Dev. 2003;29:77–83. doi: 10.1046/j.1365-2214.2003.00316.x. [DOI] [PubMed] [Google Scholar]
- Dent KM, Carey JC. Breaking difficult news in a newborn setting: Down syndrome as a paradigm. Am J Med Genet. 2006;142C(3):173–179. doi: 10.1002/ajmg.c.30100. [DOI] [PubMed] [Google Scholar]
- Denzin N. The research act: A theoretical introduction to sociological methods. New York: McGraw-Hill; 1989. [Google Scholar]
- Graungaard AH, Skov L. Why do we need a diagnosis A qualitative study of parents experiences, coping and needs when the newborn child is severely disabled. Child Care Health Dev. 2007;33(3):296–307. doi: 10.1111/j.1365-2214.2006.00666.x. [DOI] [PubMed] [Google Scholar]
- Harrison ME, Walling A. What Do We Know About Giving Bad News? A Review. Clinical Pediatrics. 2010;49(7):619–626. doi: 10.1177/0009922810361380. [DOI] [PubMed] [Google Scholar]
- Lipinski SE, Lipinski MJ, Biesecker LG, Biesecker BB. Uncertainty and perceived personal control among parents of children with rare chromosome conditions: The role of genetic counseling. Am J Med Genet. 1997;142C:232–240. doi: 10.1002/ajmg.c.30107. [DOI] [PubMed] [Google Scholar]
- Makela NL, Birch PH, Friedman JM, Marra CA. Parental perceived value of a diagnosis for intellectual disability (ID): A qualitative comparison of families with and without a diagnosis for their child’s ID. Am J Med Genet. 2009;149A(11):2393–2402. doi: 10.1002/ajmg.a.33050. [DOI] [PubMed] [Google Scholar]
- Meiser B, Irle J, Lobb E, Barlow-Stewart K. Assessment of the content and process of genetic counseling: a critical review of empirical studies. J Genet Couns. 2008;17(5):434–51. doi: 10.1007/s10897-008-9173-0. [DOI] [PubMed] [Google Scholar]
- Minichiello TA, Ling D, Ucci DK. Breaking bad news: a practical approach for the hospitalist. J Hosp Med. 2007;2(6):415–421. doi: 10.1002/jhm.271. [DOI] [PubMed] [Google Scholar]
- Morgan DL. Practical strategies for combining qualitative and quantitative methods: Applications to health research. Qual Health Res. 1998;8:362–376. doi: 10.1177/104973239800800307. [DOI] [PubMed] [Google Scholar]
- Moyer VA, Calonge N, Teutsch SM, Botkin JR. Expanding newborn screening: process, policy, and priorities. United States Preventive Services Task Force. Hastings Cent Rep. 2008;38(3):32–9. doi: 10.1353/hcr.0.0011. [DOI] [PubMed] [Google Scholar]
- Reiff M, Bernhardt BA, Mulchandani S, et al. “What does it mean?”: Uncertainties in understanding results of chromosomal microarray testing. Genet Med. 2012;14(2):250–258. doi: 10.1038/gim.2011.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roche M. Genetic Counseling Considerations in Molecular Diagnosis. In: Coleman WB, Tsongalis GJ, editors. Molecular Diagnostics: For the Clinical Laboratorian. 2. Humana Press, a part of Springer Science + Business Media, LLC; 2006. pp. 525–544. [Google Scholar]
- Schoefl R. Breaking bad news. Dig Dis. 2008;26(1):56–8. doi: 10.1159/000109388. [DOI] [PubMed] [Google Scholar]
- Skirton H. Parental experience of a pediatric genetic referral. Am J Matern Child Nurs. 2006;31(3):178–84. doi: 10.1097/00005721-200605000-00010. [DOI] [PubMed] [Google Scholar]
- Skotko B. Mothers of children with Down syndrome reflect on their postnatal support. Pediatrics. 2005;115:64–77. doi: 10.1542/peds.2004-0928. [DOI] [PubMed] [Google Scholar]
- Skotko BG, Capone GT, Kishnani PS for the Down Syndrome Diagnosis Study Group. Postnatal Diagnosis of Down Syndrome: Synthesis of the Evidence on How Best to Deliver the News. Pediatrics. 2009;124(4):e751–e758. doi: 10.1542/peds.2009-0480. [DOI] [PubMed] [Google Scholar]
- Taanila A, Syrjälä L, Kokkonen J, Järvelin MR. Coping of parents with physically and/or intellectually disabled children. Child Care Health Dev. 2002;28(1):73–86. doi: 10.1046/j.1365-2214.2002.00244.x. [DOI] [PubMed] [Google Scholar]
- Waxler JL, Cherniske EM, Dieter K, Herd P, Pober BR. Hearing from parents: The impact of receiving the diagnosis of Williams syndrome in their child. Am J Med Genet. 2013;161(3):534–541. doi: 10.1002/ajmg.a.35789. [DOI] [PubMed] [Google Scholar]