Abstract
Preduodenal portal vein (PDPV) is a rare developmental anomaly. In infants, this is often associated with duodenal obstruction or biliary atresia. It is generally asymptomatic in adults (Ooshima et al., Hepato-Biliary-Pancreat Surg 5(4):455–458, 1998). Here, we report a singular case of adult PDPV that was discovered accidentally during emergency laparotomy for peritonitis due to gastric perforation in a 38-year-old lady. A plethora of congenital anomalies was uncovered, which is consistent with the reported cases of classical polysplenia syndrome, viz., multiple spleens of equal volume, visceral heterotaxia, right (Rt.)-sided stomach, a left (Lt.)-sided or a large midline liver, malrotation of intestine, a short pancreas, PDPV and IVC abnormalities (Gayer et al., Abdom Imaging 24:178–184, 1999). In addition, abnormalities like anamolous origin of Lt. gastric and splenic arteries from the abdominal aorta with absent celiac trunk, hepatic artery arising from the superior mesenteric artery, hepatic veins draining directly to Rt. atrium, etc. along with hypertrophic and lipomatous interatrial septum have also been detected during further investigations. As of now, we have come across 29 cases of adult PDPV reported in world literature and we are reporting our unique case with a review of literature on anomalies of visceral organs associated with PDPV.
Keywords: PDPV in adult, Heterotaxy, Polysplenia, IVC abnormality, Anomalous origin of arteries, Pancreatic agenesis
Introduction
Preduodenal portal vein (PDPV) is a rare congenital anomaly in which the portal vein passes anterior to the duodenum instead of posterior to the duodenum. In children, it is usually associated with features of intestinal obstruction either due to compression of duodenum by the abnormal portal vein itself or by the coexisting congenital anomalies like duodenal atresia, duodenal web, annular pancreas, intestinal malformation, biliary atresia, etc. It is extremely rare in adults and is often found incidentally during laparotomy/investigation for an unrelated condition. PDPV was first described as an autopsy finding by Knight [3] in 1921 and was first operated by Schnitzler for PDPV causing duodenal obstruction in 1926 [4]. The importance of this condition lies in the fact that the operations on the biliary tract and duodenum are fraught with danger of damage to the portal vein and the disastrous consequences due to its anterior placement. On encountering this condition as a surprise during emergency surgery for peritonitis due to perforated gastric ulcer, we have attempted a detailed study of the anatomical aberrations [2] and also a review of the available literature on the subject matter.
Case Report
A 38-year-old lady presented to us in the emergency room with severe pain abdomen of 2 days duration with history suggestive of gastritis on and off earlier. There was no significant past, personal, or family history. She is a mother of three children and is still in the reproductive age. Clinically, she is a moderately built and nourished lady. She was febrile, and her pulse rate was 90/minute, BP 110/80 mmHg, and RR 20/minute. There was localized guarding in the right (Rt.) lower abdomen associated with rebound tenderness in the Rt. lower abdomen. Routine biochemical investigations were within normal limits.
Plain X-ray of the abdomen in erect posture revealed a thin crest of air under the Rt. dome of diaphragm and a distended loop of colon under the left (Lt.) dome of diaphragm. Ultrasonography was suggestive of peritonitis.
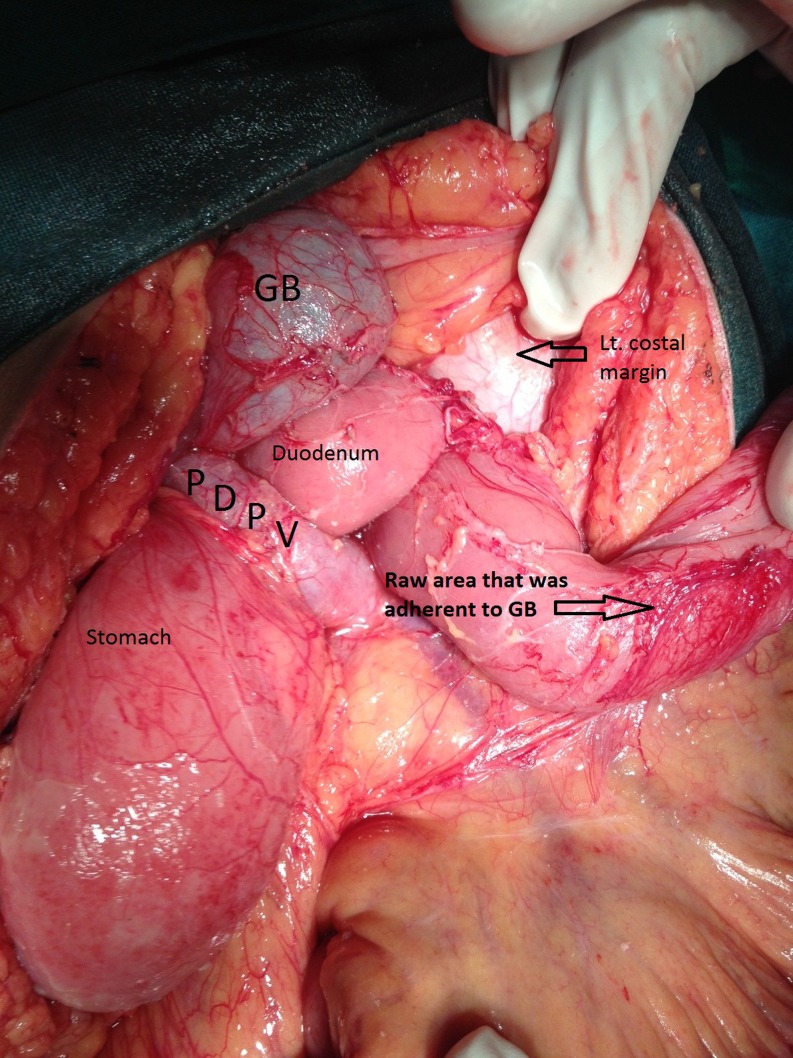
With a diagnosis of peritonitis due to hollow viscous perforation, probably a perforated appendix, emergency exploratory laparotomy was performed late in the night. There was plenty of collection in the peritoneal cavity. Appendix was found to be normal. Stomach and transverse colon were not visible in its normal position. There was a small band of about 1 in. width between a loop of small bowel and fundus of gall bladder. On releasing it, the following anatomy was uncovered: (a) Lt. lobe of liver was occupying the Lt. subdiaphragmatic area; (b) stomach was in the Rt. hypochondrium; (c) there was no C loop of duodenum; (d) portal vein was running on the anterior surface of duodenum; and (e) the neck of gall bladder disappeared behind the portal vein (Figs. 1 and 2).
Fig. 1.
Anatomy that was found upon releasing the band
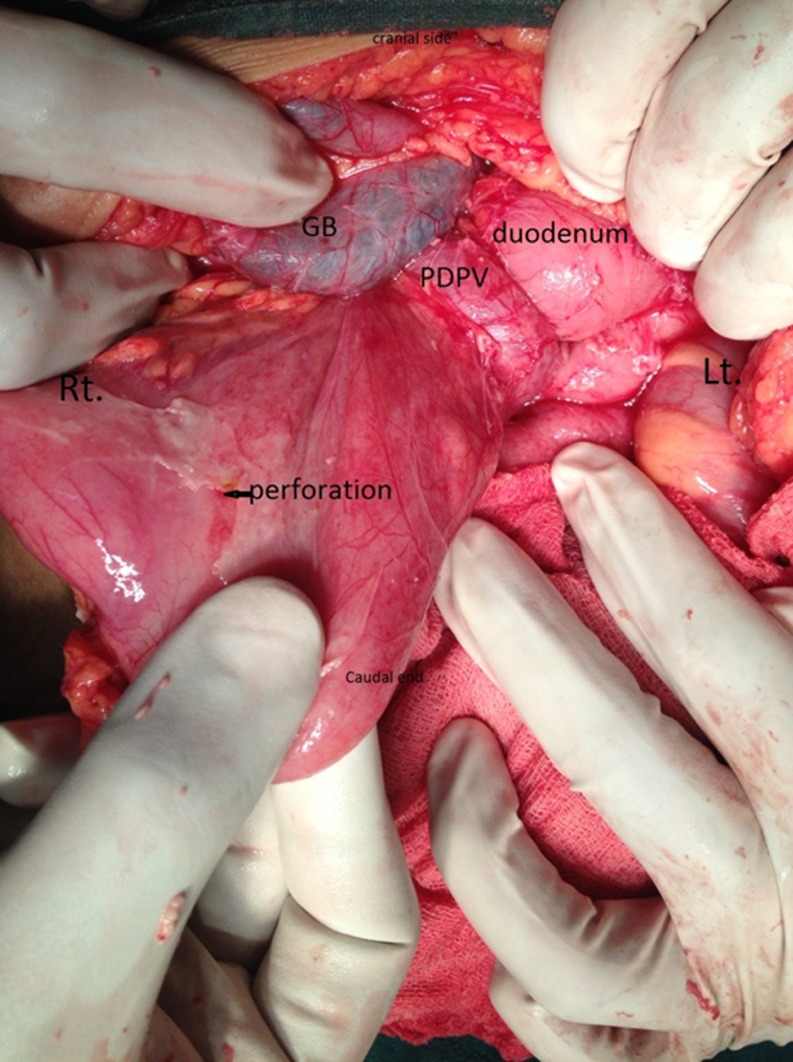
Fig. 2.
Site of perforation
The site of perforation was not immediately visible. On continued and thorough exploration, a small perforation in the antrum of the stomach was found, which was closed with an omental patch.
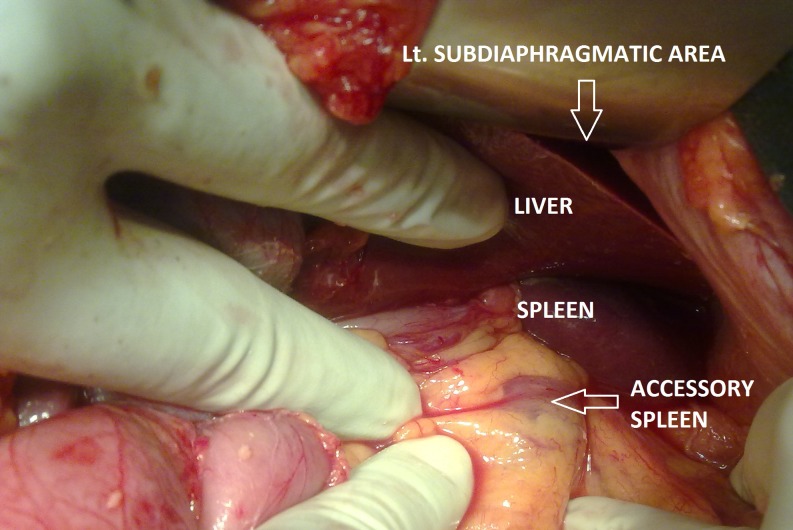
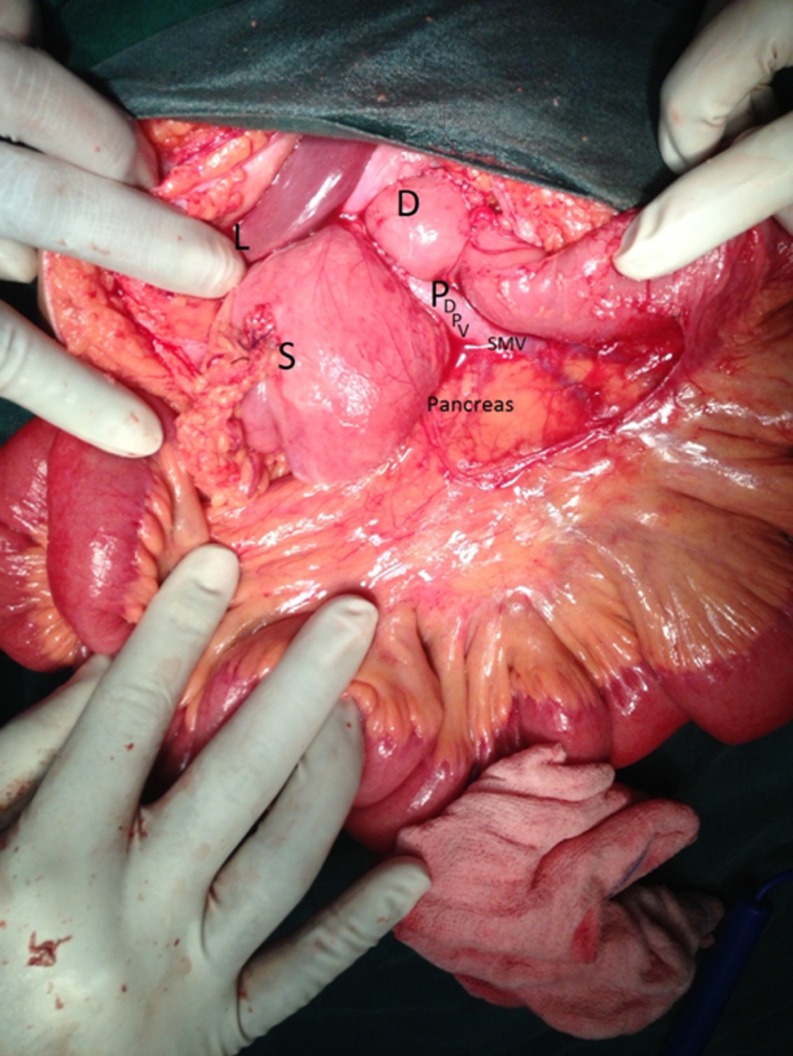
On further exploration, (a) the spleen was found to be in the normal position and was of normal size, but an additional splenic nodule was found in the mesentery; (b) only pancreatic head and a small part of the body were visible; (c) most of the small bowel was in the upper abdomen; (d) tributaries of portal vein were clearly visible; and (e) large bowel was in the lower abdomen with caecum appendix in the RIF (Figs. 3 and 4).
Fig. 3.
Additional splenic nodule found in mesentery with left lobe of the liver in left subdiaphragmatic area
Fig. 4.
Pancreatic head and a small part of the body were visible
Her postoperative period was uneventful. Since the case was unique, further imaging studies were done during the late postoperative period for compilation of data/document for academic study and review purposes.
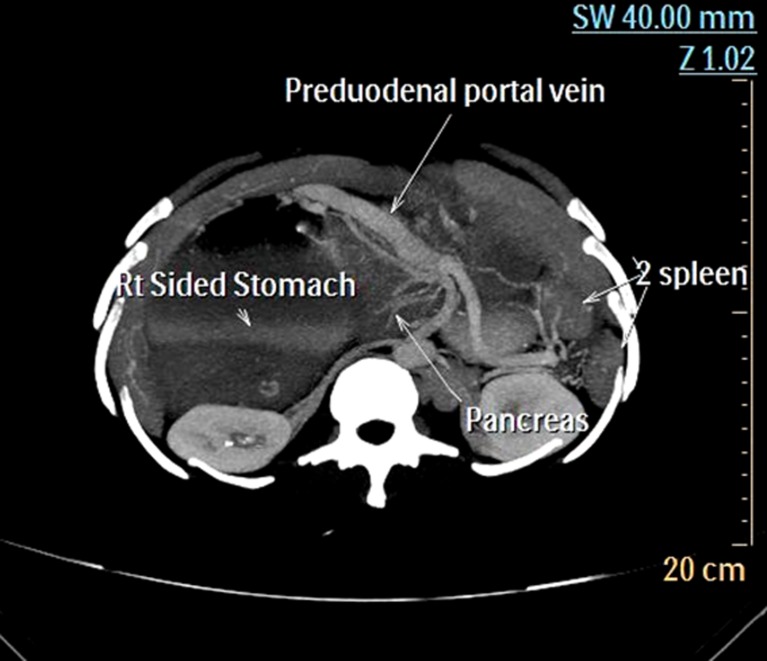
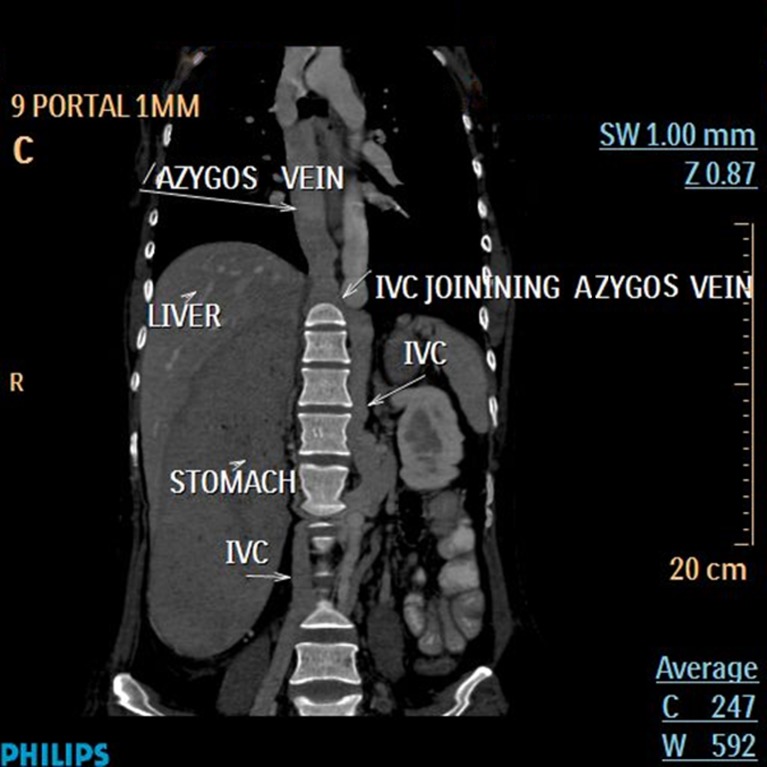
CECT abdomen revealed the following findings: (a) fundus of stomach in the left, but body and pylorus extend to the Rt. of the abdomen with duodenum extending to left upper abdomen; (b) portal vein running anteriorly at the gastroduodenal junction causing mild compression on it; (c) head and part of the body of the pancreas was visualized with rest of the body and tail was absent; (d) two small spleens in the left upper abdomen; (e) left lobe of liver overlapping the spleen; (f) gall bladder in the midline; (g) inferior vena cava (IVC) on the right in the lower abdomen which joins the prominent azygos vein at the level of left renal vein; (h) hepatic veins draining directly to the right atrium; (i) splenic artery and left gastric artery arising separately from upper abdominal aorta; and (j) hepatic artery arising from superior mesenteric artery (Figs. 5 and 6).
Fig. 5.
Demonstrating PDPV, Rt. sided stomach, two spleens and short pancreas
Fig. 6.
IVC on the Rt. lower abdomen and continues above with prominent azygos vein
Echocardiogram showed hypertrophic and lipomatous interatrial septum.
Discussion
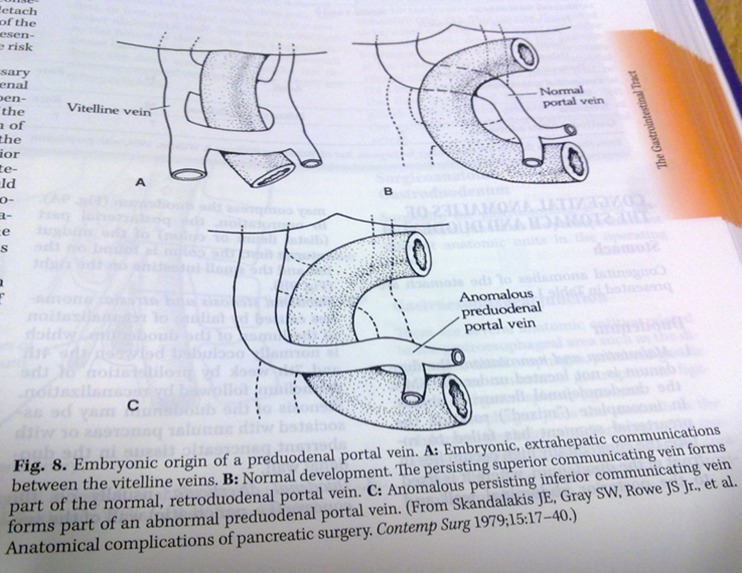
The occurrence of PDPV can be explained by the embryonic development of portal vein from the vitelline veins [5] (Fig. 7). Although the etiology of malrotation is not well understood, genetic mutations may predispose the host to malrotation. For instance, mutations in gene BCL6 resulting in absence of Lt. side expression of its transcript lead to reversed cardiac orientation, defective ocular development, and malrotation [6]. In non-rotation, the post-arterial part (distal ileum and colon) of midgut returns to abdomen first and the colon is found on the Lt. and the small intestine on the Rt. [5]. Although the exact cause of polysplenia is unknown, studies have suggested that it is caused by various factors including embryogenic, genetic, and teratogenic components.
Fig. 7.
The occurrence of PDPV can be explained by the embryonic development of Portal vein from the vitelline veins
Most patients with PDPV have other congenital anomalies requiring urgent surgical operations in infancy and childhood due to duodenal atresia, annular pancreas, biliary atresia, intestinal malrotation, etc. Hence, adult PDPV is rare and few diagnostic images have been reported prior to surgery. It is an incidental finding at surgery for an unrelated condition. Our case had a mild gastric dilatation and delayed emptying due to pressure of PDPV at the gastroduodenal junction, but was not severe enough to warrant surgical intervention. According to Waldschmidt [17], PDPV is an extrinsic cause of duodenal obstruction that rarely needs bypass procedures. Duodeno-duodenal anastomosis anterior to the portal vein is the procedure of choice to manage this anomaly.
Since Knight reported the first case of PDPV in 1921, about 30 adult cases including the present one have been reported in the world literature [1, 7–16] (Table 1). There could be more.
Table 1.
PDPV in adults
| Pt. no. | Age/sex | Symptoms related to PDPV | Other associated anomalies | Indication for laparotomy | Operative procedure |
|---|---|---|---|---|---|
| 1 [11] | 22/M | Duodenal obstruction | Scoliosis | Duodenal obstruction | Gastrojejunostomy with jejunojejunostomy |
| 2a | 38/Fa | None | Heterotaxia of gut, dilatation of stomach due to extrinsic pressure of PDPV on G-D junction polysplenia, interruption of IVC with continuation of azygos vein, agenesis of body and tail (dorsal bud) of pancreas and other vascular anamolies like independent origin of Lt. gastric and splenic A from abdominal aorta, hepatic A. from superior mesenteric A., hepatic veins draining directly into Rt. atrium, hypertrophied lipomatous interatrial septum | Peritonitis due to perforated gastric ulcer | Perforation closure and peritoneal toileting and drainage |
| 3 [10] | 41/F | None | Polysplenia, intrahepatic ductal stones | Intrahepatic ductal stones | Lt. lateral sectionectomy with cholecystectomy |
| 4 [16] | 49/F | None | Polysplenia with agenesis of dorsal pancreas with pancreatitis | ||
| 5 [15] | 50/F | None | Malrotation, polysplenia | Cholecystolithiasis | Cholecystectomy |
| 6 [12] | 56/F | None | Degenerative ampullome, polysplenia, absent IVC, anastomosis between IVC and azygos vein, complete common mesentery | Not available | Not available |
| 7 [8] | 56/M | Duodenal obstruction | Intestinal malrotation, hypoplastic IVC with prominent azygos vein, short pancreas and polysplenia | Duodenal obstruction and obstructive jaundice | Cholecystectomy, biliodigestive bypass and gastrojejunostomy |
| 8 [9] | 60/M | Duodenal obstruction | Duodenal obstruction | Gastrojejunostomy | |
| 9 [13] | 62/F | Stasis, dilated CBD, choldocolithiasis | Midline liver, multiple splenunculi, agenesis of pancreatic tail and body, stomach to the Rt. IVC to the Lt. of midline and crossed to Rt. at the hiatus, B/L hyparterial bronchi | Obstructive jaundice | Cholecystectomy and choledocolithotomy |
| 10 [14] | 63/M | None | Intestinal malrotation, polysplenia, interruption of IVC with continuation of azygos vein | Gastric cancer | |
| 11 [7] | 65/M | None | Polysplenia, azygos continuation, and anomalous portal branches | Not available | Not available |
These data are in continuation and addition to the published data in Table 1 of reference 1
CBD common bile duct, G-D gastroduodenal, B/L bilateral
aPresent case under report
Analysis
The age profile of the 30 patients analyzed is between 22 and 85 years. The male/female ratio is 12:18. Only six patients (20 %) reportedly presented with symptoms due to PDPV. Of these, five cases were of duodenal obstruction in the male/female ratio of 4:1. One female patient had obstructive jaundice.
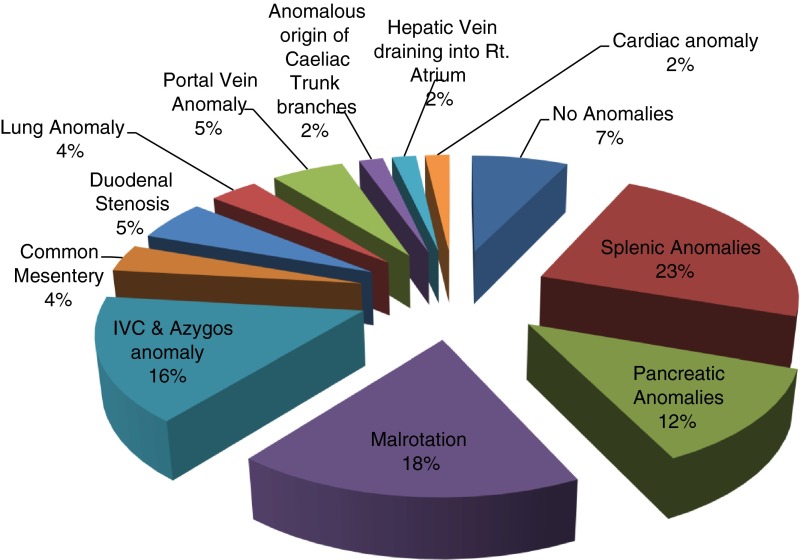
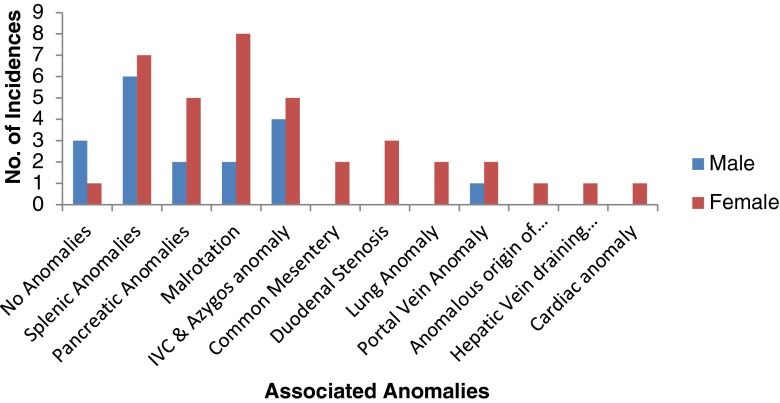
Associated anomalies with PDPV are shown in Figs. 8 and 9. The present reported case had most of the anamolies listed. It is observed that majority of the patients with PDPV had associated anamolies mainly polysplenia, malrotation of gut, and pancreatic and IVC anamolies. The occurrence of more numbers and types of the anamolies is seen in females than in males.
Fig. 8.
Distribution of associated anomalies
Fig. 9.
Incidence of associated anomalies
Summary
The polysplenia syndrome reported herein exhibits a host of congenital anomalies reported in the literature, however, with additional vascular anomalies in the form of abnormal origin of splenic and left gastric arteries from abdominal aorta and hepatic artery (A.) from superior mesenteric A., as also hepatic veins draining directly to the right atrium, and cardiac anomaly in the form of hypertrophic and lipomatous interatrial septum, etc. which makes this case unique. The postoperative CT finding of mild compression of gastroduodenal junction caused by PDPV does not warrant surgical intervention, since the patient has been asymptomatic all along. The risk of inadvertent injury leading to disastrous bleeding in such patients during surgery is high—especially surgery of the biliary tree and duodenum. This necessitated extra caution and gentle handling in identifying and managing the perforation. The combination of multiple congenital anomalies presented diagnostic difficulties both clinically and during exploratory laparotomy.
References
- 1.Ooshima I, Maruyama T, et al. Preduodenal portal vein in the adult. J Hepato-Biliary-Pancreat Surg. 1998;5(4):455–458. doi: 10.1007/s005340050072. [DOI] [PubMed] [Google Scholar]
- 2.Gayer G, Apter S, Jonas T, et al. Polysplenia syndrome detected in adulthood; report of 8 cases and review of literature. Abdom Imaging. 1999;24:178–184. doi: 10.1007/s002619900471. [DOI] [PubMed] [Google Scholar]
- 3.Knight HO. An anomalous portal vein with its surgical dangers. Ann Surg. 1921;74:697–699. doi: 10.1097/00000658-192112000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schnitzler J. UeberEine Cigentumlicle “Missbildung mit Stenosierung des Mlagenausgangs”. Medklin. 1926;22:723. [Google Scholar]
- 5.Bland KI, Jones DB, Fischer JE, et al. Fischer's mastery of surgery, 6th edition. Riverwoods: Lippincott, Williams & Wilkins; 2012. p. 961. [Google Scholar]
- 6.Brunicardi F, Andersen D, Billiar T, et al. Schwartz's principles of surgery. 9. New York: McGraw-Hill; 2009. p. 1428. [Google Scholar]
- 7.Kamitani T, Tajima T, Kakihara D, Yabuuchi H, Iwashita I, Kawamoto K. Anomalous portal branches associated with polysplenia syndrome: imaging findings. CMIG Extra: CASES. 2004;28(2):15–19. doi: 10.1016/j.compmedimag.2003.07.003. [DOI] [Google Scholar]
- 8.Plata-Munoz JJ, Hernandez-Ramirez D, Anthon FJ, Podgaetz E, Avila-Flores F, Chan C. Polysplenia syndrome in the adult patient. Ann Hepatology. 2004;3(3):114–117. [PubMed] [Google Scholar]
- 9.John AK, Gur U, Aluwihare A, Cade D. Pre duodenal portal vein as a cause of duodenal obstruction in an adult. ANZ J Surg. 2004;74(11):1032–1033. doi: 10.1111/j.1445-1433.2004.03226.x. [DOI] [PubMed] [Google Scholar]
- 10.Seo HI, Jeon TY, Sim MS, Kim S. Polysplenia syndrome with PDPV detected in adults. World J Gastro- enterol. 2008;14:6418–6420. doi: 10.3748/wjg.14.6418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Masumuto K, Teshina R, Esumi G, et al. Duodenal stenosis resulting from PDPV and operation for scoliosis. World J of Gastroenterology. 2009;15(31):3950–3953. doi: 10.3748/wjg.15.3950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wailly P, Metzler P, Sautot-Vial N, Olivier D, Meunier B, Faure JP. Pre-duodenal portal vein in polysplenia syndrome: clinical effects and surgical application. Surg Radiol Anat. 2011;33(5):451–454. doi: 10.1007/s00276-010-0768-4. [DOI] [PubMed] [Google Scholar]
- 13.Low JP, Williams D, Chaganti JR. Polysplenia syndrome with agenesis of the dorsal pancreas and preduodenal portal vein presenting with obstructive jaundice—a case report and literature review. Br J Radiol. 2011;84(1007):e219–e222. doi: 10.1259/bjr/27680217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mimatsu K, Oida T, Kano H, Kawasaki A, Fukino N, Kida K, Kuboi Y, Amano S. Preduodenal portal vein, intestinal malrotation, polysplenia, and interruption of the inferior vena cava: a review of anatomical anomalies associated with gastric cancer. Surg Radiol Anat. 2012;34(2):179–180. doi: 10.1007/s00276-011-0894-7. [DOI] [PubMed] [Google Scholar]
- 15.Anand U, Chaudhary B, Priyadarshi R, et al. Polysplenia syndrome with preduodenal portal vein. Ann Gastroenterol. 2012;26:1. [PMC free article] [PubMed] [Google Scholar]
- 16.Jeong JH, Kim GH, Song GA, et al. Polysplenia syndrome with congenital agenesis of dorsal pancreas presenting as acute pancreatitis. Korean J Gastroenterol. 2012;60(1):47–51. doi: 10.4166/kjg.2012.60.1.47. [DOI] [PubMed] [Google Scholar]
- 17.Waldschmidt J et al. (2001) Pediatric surgery update, vol.16, January