Abstract
Lumbar hernia is a rare defect of the abdominal wall. It accounts for 2 % of all wall hernias. It is divided in two levels: superior lumbar hernia, also known as Grynfeltt’s hernia (GH), and an inferior lumbar hernia or Petit’s hernia. GH is more commonly encountered in practice, and it is mainly posttraumatic in origin. Spontaneous primary GH is quite rare. Only 250 to 300 of such cases have been reported the in literature so far. The treatment of choice is retroperitoneal surgical approach and a meshplasty after complete reduction of its contents. Prognosis is usually excellent.
Keywords: Primary, Grynfeltt’s, Hernia, Lumbar
Case History
A 68-year-old Hindu male patient, a manual laborer by occupation, came with chief complaints of swelling on the left side of his back since 6 months. The patient had pain within swelling since 2 months. The patient was apparently all right 6 months back when he first noticed the swelling in the left loin. It was smaller initially and was reducible. It used to get prominent on exertion. There was a mild dull aching pain associated with the swelling.
The patient had breathlessness on exertion and also during his routine work. He had dry cough since 5 years for which he was on conservative treatment since then. There was no history of (H/O) any trauma to the area involved. He had no other major medical illnesses or any surgery done specially in that region. His bowel and bladder habits were within normal limits (WNL).
On examination, vital parameters were WNL. On local examination, he had solitary, globular swelling in the left superior lumbar triangle measuring 5 cms × 4 cms × 3 cms in dimensions. It had smooth surface, and skin over the swelling was WNL (Fig. 1). There was no evidence of any scars/sinuses or dilated veins over the swelling. It had a visible expansile cough impulse, and it was spontaneously reducible on lying down laterally. On palpation, it was reducible with a fascial defect of 3 cms × 4 cms in the lumbar triangle.
Fig. 1.
Typical location of Grynfeltt’s hernia at the superior lumbar triangle. Abdominal examination was WNL. Digital per rectal examination was WNL
All basic investigations were WNL. An ultrasound of the abdomen and pelvis revealed superior lumbar hernia with 3 cms × 4 cms fascial defect. The kidney was WNL. A decision to perform open hernioplasty with use of polypropylene mesh was taken.
The patient was explored under local anesthesia in view of pulmonary restrictive airway disease. The sac was meticulously dissected, and all contents reduced. A retroperitoneal polypropylene meshplasty was done (Fig. 2). The patient withstood the surgery well. Postoperative recovery was uneventful. Suture removal was done on the tenth postoperative day. At follow-up, the patient is asymptomatic and under treatment for pulmonary disease.
Fig. 2.
Open meshplasty done for patient after complete reduction
Discussion
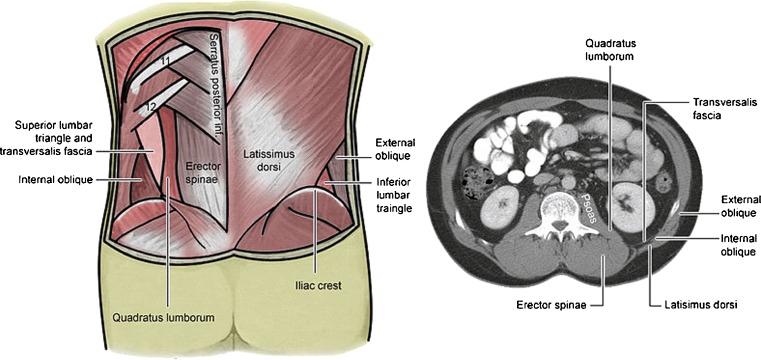
The superior triangle is more consistently found in cadavers [1] and is a more common site of herniation; however, the inferior lumbar triangle is often simply called the lumbar triangle, perhaps owing to its more superficial location and ease in demonstration (Fig. 3).
Fig. 3.
Location (left) & surgical anatomy of lumbar traingles (right)
Lumber hernias may be congenital and acquired. Congenital hernias appear during infancy as the origin of a defect in the musculoskeletal system of the lumbar region and are associated with other malformations. Acquired lumbar hernias are usually primary—or spontaneous—and secondary, depending on the existence of a causal factor such as surgery, infection, or trauma. Predisposing factors in spontaneously acquired lumbar hernia are age, obesity, extreme thinness, chronic debilitating disease, muscular atrophy, intense slimming, chronic bronchitis, wound infection, and postoperative sepsis. They are also usually associated with strenuous physical activity.
Classifications proposed in the literature have a unifactorial, epidemiological nature, not a therapeutic orientation [2, 3].
According to location: (1) superior lumbar (Grynfeltt–Lesshaft triangle, lumbocostal, or costoiliac of Larrey); (2) inferior lumbar (Petit’s triangle, suprailiac of Huguier, or lumboiliac); and (3) diffuse (postoperative, costal incisional, or traumatic).
According to contents: (1) extraperitoneal (with no peritoneal sac); (2) paraperitoneal (peritoneum sliding and adhering to the viscera); and (3) intraperitoneal (with a complete peritoneal sac around the visceral contents).
According to etiology: congenital or acquired; and traumatic, infectious, or surgical. Posterior lateral tumor: the most common clinical manifestation is a palpable mass that increases with coughing and strenuous activity:
Back pain or lumbago: According to Light [4], it is a diagnosis to consider in young women and athletes with back pain.
Bowel obstruction.
Urinary obstruction [5]
Other rare forms of manifestation reported in publications are pelvic mass and retroperitoneal and gluteal abscess [6].
Though rare defects, lumbar hernias have a 25 % risk of incarceration and a >8 % chance of strangulation [7].
Various repair techniques have been proposed such as simple anatomical repair, rotational musculofascial pedicle flap grafts, free grafts, fascial strip repair, and various synthetic mesh repairs. Failure of these repairs may be due to limited fascial strength, weakness of the surrounding tissues, and difficulty in sewing the bony portion of the hernia boundaries after the introduction of prosthetic repairs. Recurrence rates following conventional (open) ventral abdominal wall hernia repairs have fallen to between 12.5 and 19 % [8].
In our case, the patient presented with spontaneous primary Grynfeltt’s hernia where a standard open retroperitoneal meshplasty was performed.
Footnotes
Dr. Dewoolkar, Dr. Amit and Dr. Ushna are no longer affiliated with K J Somaiya Medical College. However, this work was done during thier stay in the organization.
References
- 1.Goodman EH, Speese J. Lumbar Hernia. Ann Surg. 1916;63:548. doi: 10.1097/00000658-191605000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thorek M. Lumbar hernia. J Int Coll Surg. 1950;14:367–393. [PubMed] [Google Scholar]
- 3.Geis WP, Hodakowski GT. Lumbar hernia. In: Nyhus LM, Condon RE, editors. Hernia. 4. Philadelphia: Lippincott; 1995. pp. 412–423. [Google Scholar]
- 4.Light HG. Hernia of the inferior lumbar space: a cause of back pain. Arch Surg. 1983;118:1077–1080. doi: 10.1001/archsurg.1983.01390090061014. [DOI] [PubMed] [Google Scholar]
- 5.Hide IG, Pike EE, Uberoi R. Lumbar hernia: a rare cause of large bowel obstruction. Postgrad Med J. 1999;75:231–233. doi: 10.1136/pgmj.75.882.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Biotois H, Couinaud C. A case of lumbar hernia favoring the formation of a mass in the pelvic colon. J Chir (Paris) 1969;98:27–30. [PubMed] [Google Scholar]
- 7.Heniford BT, Ianniti DA, Gagner M. Laparoscopic inferior and superior lumbar hernia repair. Arch Surg. 1997;132:1141. doi: 10.1001/archsurg.1997.01430340095017. [DOI] [PubMed] [Google Scholar]
- 8.Bauer JJ, Harris MT, Kreel I, Gelernt IM. Twelve-year experience with expanded polytetrafluoroethylene in the repair of abdominal wall defects. Mt Sinai J Med. 1999;66:20–5. [PubMed] [Google Scholar]