Abstract
The study was carried out to compare the efficacy of subfascial endoscopic perforator surgery (SEPS) and open subfascial ligation of perforators in varicose veins. This study was conducted on 100 patients of varicose veins from January 2006 to December 2010. Clinical scoring and color Doppler were performed in all the patients before surgery. Patients were divided into two groups: Group A and Group B alternately. Management of the perforators was done by subfascial endoscopic perforator surgery (SEPS) in Group A and by open subfascial ligation of perforators in Group B. Fifty patients were treated in each group. All the patients underwent ligation of incompetent saphenofemoral junction with stripping of long saphenous veins wherever the junction was incompetent with multiple ligation of superficial prominent veins. SEPS was done by two-port method without any tourniquet or balloon dissector. Total numbers of perforators ligated were 178 in Group A and 136 in Group B. Patients in both the groups got symptomatic relief of symptoms, but ulcer healing in 33 % patients in Group A was faster as compared to Group B. However, at 3 months of follow-up the ulcers healed in all the patients in both groups. Incidence of wound infection was higher in group B (16 %) as compared to group A (0 %). There were residual perforators in 8 % of patients on color Doppler at 3 months of follow-up in Group B while there was no residual incompetent perforator in Group A. Subfascial endoscopic perforator vein surgery is a safe and effective method for treating incompetent perforating veins. The number of perforators ligated in SEPS was more as compared to the open subfascial ligation group. Possibly some perforators may be missed on Doppler localization and missed ligation, which may be a cause of future recurrence in varicose veins. Early relief of symptoms in terms of ulcer healing was better in the SEPS group with less wound complication rate; however, all the ulcers healed in both the groups at 3 months of follow-up. Cosmetic results were equal in both the groups. Major advantage of SEPS was less incidence of wound complications and less incidence of residual incompetent perforators. Hence, SEPS should be added for the management of perforators along with conventional surgery in varicose veins.
Keywords: Subfascial endoscopic perforator surgery, Varicose veins, Perforator incompetence
Introduction
Dilated tortuous and thickened veins are known as varicose veins. Severity of the disease may vary from telangiectatic veins to venous ulceration. Perforating veins perform a normal function in transporting superficial venous blood inward to the deep veins for further transit to the heart. If perforating veins become incompetent and transmit outward flow, it may lead to chronic venous insufficiency. Deep venous reflux accompanies superficial venous reflux in 20 % of limbs with varicose veins [1]. The usual starting point of this retrograde circuit is the saphenofemoral junction, but it may start from one of the perforators like mid-thigh Hunterian or the anteromedial Boyd perforator or a calf perforator. This circuit must be broken by removing the superficial part of the circuit and by ligating the incompetent perforators. The Hammarsten group measured the diameter of long saphenous veins at four different levels after ligating the incompetent perforators and incompetent saphenofemoral junction, and it was found that diameter of the long saphenous vein was reduced by 40 % [2]. Hence, incompetent perforators which are sometimes very big in size have a definite role in the pathophysiology of chronic venous insufficiency, and they need ligation either by open surgery or by subfascial endoscopic perforator surgery (SEPS). Subfascial endoscopic perforator surgery has the advantage of better wound healing in an already compromised skin; at the same time, results comparable to classic Linton’s procedure can be achieved.
Patients and Methods
This study was performed on 100 patients of varicose veins with perforator incompetence. After taking a detailed history, a thorough clinical examination was done. Color Doppler was done in all the patients. Patients were graded as per CEAP classification. Deep veins were patent in all the patients and no patient of deep vein thrombosis was included in the study. Patients were divided into two groups: Group A and Group B, alternately. Localization of the incompetent perforators was done preoperatively by clinical examination, and color Doppler and perforators were marked. High ligation of saphenofemoral junction (SFJ) with ligation of all the tributaries and stripping of thigh portion of long saphenous vein was done for saphenofemoral incompetence wherever it was present. Saphenopopliteal junction (SPJ) was also ligated if it was incompetent. For perforators, Group A patients underwent subfascial endoscopic perforator surgery by the two-port method. All the visualized big perforators were ligated endoscopically by clips, and small perforators were coagulated with electrocautery. Group B patients were subjected to open subfascial ligation of perforators at the sites marked by color Doppler. Both the groups were studied for incidence of hematoma, pain, wound infection, and saphenous nerve injury. Incidence of residual incompetent perforators was noted by doing color Doppler at 3 months of follow-up. Relief of symptoms was noted at 14 days and 3 months on a linear visual analog scale. Cosmetic result was judged by the patient as good, moderate, and poor at 14 days and 3 months of follow-up.
Technique of Subfascial Endoscopic Perforator Surgery
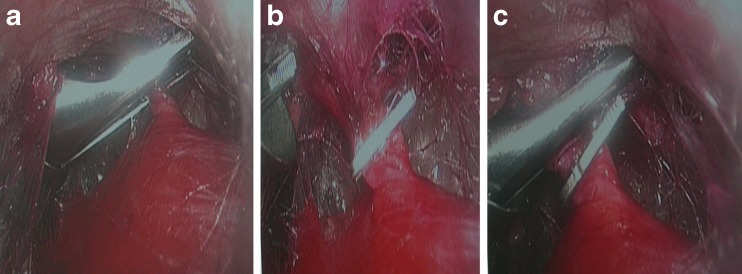
Since the original description of procedure by Hauer in 1985, the technique of SEPS has undergone many modifications [3]. In the present study, SEPS was done by the two-port method. No tourniquet was used in the present study. The knee was flexed at 90 ° and the hip was flexed and abducted (Fig. 1). A 10 mm endoscopic port was placed on the medial side of the calf, 5–7 cm distal to tibial tuberosity, under direct vision by incising the fascia. A pocket was created and carbon dioxide insufflation was used to widen the space and facilitate access after port placement. The distal 5 or 10 mm port was placed posteromedially and slightly inferior to the first port under direct visualization with the camera. Carbon dioxide was insufflated in the subfascial space and the pressure was maintained at 30 mm Hg to create a space in the subfascial plane to visualize the perforators. The subfascial space was explored and all the big perforators were clipped (Fig. 2a–c), and small perforators were coagulated with electrocautery. By rotating the ports, whole of the leg was explored and all the perforators were ligated or coagulated. After completing the procedure, the instruments and ports were removed and carbon dioxide was expressed out manually. Subfascial negative suction drain was put in cases where excessive oozing was present in the subfascial space. The wounds were closed and the limb was elevated and wrapped in an elastic bandage.
Fig. 1.
Ports placed on the medial side of the leg
Fig. 2.
a–c Clipping of perforators
Observations
Maximum number of patients (58 out of 100) in our study were between 16 and 35 years of age with a mean of 33.6 years. There were 70 males and 30 females in our study. In Group A, there were 38 males and 12 females. In Group B, there were 32 males and 18 females. The right side was involved in 48 patients and the left side was involved in 42 patients. Bilateral involvement was observed in 10 patients. In case of bilateral involvement, surgery was done on the more affected side (the right side in 3 patients, and the left side in 7 patients).
Dilated and tortuous veins were the commonest presenting complaints. They were present in all the patients. Thirty-six patients complained of pain during walking, while 12 patients had swelling feet as the main complaint. Pigmentation and ulceration were found in 22 and 12 patients, respectively (Table 1).
Table 1.
Patient classification according to CEAP
| Clinical status | Number | Anatomical | Number |
|---|---|---|---|
| C2 (Group A 27, Group B 27) | 54 | Superficial | 74 |
| C3 (Group A 6, Group B 6) | 12 Perforator | 100 | |
| C4 (Group A 12, Group B 10) | 22 | Deep | Nil |
| C5 | Nil | ||
| C6 (Group A 6, Group B 6) | 12 | ||
| Etiology | Pathophysiology | ||
| Primary | 100 | Reflux | 100 |
| Secondary | 0 | Obstruction | Nil |
| Congenital | 0 | Reflux and obstruction | Nil |
In this study, the saphenofemoral junction was incompetent in 74 patients while the saphenopopliteal junction was incompetent in 12 patients. All the patients with saphenopopliteal incompetence had concomitant saphenofemoral incompetence, and isolated saphenopopliteal incompetence was not present in any of the patients in both the groups. A significant number of patients (n = 26) had perforator incompetence as sole cause of their varicose veins.
In this study, a total of 178 perforators were ligated in Group A in 50 limbs, averaging 3.5 (minimum 1 and maximum 5), and the commonest perforators ligated were in the Cockett group (n = 84) followed by the paratibial group (n = 62). In Group B, maximum numbers of perforators ligated were the paratibial group of perforators (n = 60) followed by Cockett perforators (n = 42). A total of 136 perforators were ligated in 50 limbs in Group B, averaging 2.7 (minimum 1 and maximum 5) perforators per limb (Table 2). Hence, the average number of perforators ligated per limb was more in Group A (n = 178) as compared to Group B (n = 136).
Table 2.
Operative findings showing location of perforators
| Level of incompetence | Group A | Group B | Total | |||
|---|---|---|---|---|---|---|
| No. of patients | Perforators | No. of patients | Perforators | No. of patients | Perforators | |
| Cockett | 42 | 84 | 26 | 42 | 68 | 126 |
| Boyd | 22 | 22 | 22 | 22 | 44 | 44 |
| Paratibial | 44 | 62 | 40 | 60 | 84 | 122 |
| Posterior/lateral | 6 | 10 | 8 | 12 | 14 | 22 |
| Total | 50 | 178 | 50 | 136 | 100 | 314 |
Thus, in this study, a total of 314 perforators were ligated in 100 limbs, averaging 3.1 (minimum 1 and maximum 5) perforators per limb. Maximum numbers of incompetent perforators were in the Cockett group (n = 126) followed by the paratibial perforators (n = 122).
In Group A, one patient required negative suction drainage in subfascial space because of excessive oozing and he had small hematoma formation which resolved within a week. There was no incidence of paraesthesia in any patient in Group A. In Group B patients, there was wound infection in 8 (16 %) patients at the site of open subfascial ligation of perforators which healed after local dressings, but there was no wound infection in Group A, and the difference was statistically significant (P = 0.002). One patient in Group B had paraesthesia, but there was no hematoma formation in any patient (Table 3).
Table 3.
Complications in group A and group B
| Complication | Group A (n = 50) | Group B (n = 50) | P* value |
|---|---|---|---|
| Wound infection | 0 | 8 (16 %) | 0.002 |
| Hematoma | 1 (2 %) | 0 | 0.50 |
| Paraesthesia | 0 | 2 (4 %) | 0.24 |
*Fisher’s exact test.
Symptom Relief
All the patients were examined clinically for relief of symptoms at 14 days at the time of suture removal and at 3 months. On comparison of both groups, it was observed that ulcer healing was quicker in Group A patients (Fig. 3). Ulcer healing was complete in 2 patients at 14 days of follow-up in Group A, while none of the patients had complete healing of ulcer at 14 days in Group B. However, ulcer got healed in all the patients in both groups at 3 months of follow-up. The ankle swelling subsided very quickly in both groups, and there was no evidence of any prominent vein in the leg after surgery at 14 days of follow-up. The pigmentation persisted in all the patients at 14 days and 3 months of follow-up irrespective of the procedure done on them. Patients presenting with complaints of pain during walking could walk without feeling discomfort at 14 days and at 3 months of follow-up in both groups. Cosmetic results were good in all the patients in both the groups.
Fig. 3.

Healing ulcer after SEPS
Color Doppler examination done at 3 months of follow-up showed residual incompetent perforators in 4 patients in Group B but the patients were asymptomatic, while none of the patients in Group A showed incompetent perforator on color Doppler at 3 months of follow-up. These residual perforators may be the cause of recurrence in future on long-term follow-up.
Discussion
There have been considerable changes in the perforator management in varicose veins. In 1938 Linton described a technique for perforator management by giving a large subfascial incision and ligating all the perforators, but it was frequently complicated by wound infections [4]. Gradually, it was replaced by Doppler localization and ligation of perforators by giving small subfascial incisions, but it also required incision in the unhealthy skin. Subfascial endoscopic perforator surgery was first introduced by Hauer in 1985 [3]. The main advantage of SEPS is that it avoids incisions in the unhealthy areas of skin, and any perforator if missed by clinical examination or Doppler can also be clipped. Since then it has undergone many modifications. The ports can be 5 or 10 mm depending on availability of instruments. Initially the tourniquet was used to avoid any incidence of carbon dioxide embolism, but it was observed that risk of embolism was more of theoretical one. Now, it is done without tourniquet and with or without the balloon dissector in the subfascial space.
Maximum numbers of patients in the present study were in the age group of 16–35 years (58 %), with a mean age of 33.6 years. This age group requires maximum long-standing activities for earning for their families. In literature, the age distribution of varicose veins in most of studies varies from 30 to 40 years [5]. There were 70 % males and 30 % females in the present study, but as per literature the females are affected more commonly as compared to the males [6–8]. Sybrandy et al. have reported 31 % males and 69 % females in their study, comparing endoscopic versus open subfascial ligation of incompetent perforators in the treatment of chronic venous insufficiency [9]. Tenbrook et al. have compared data from 20 studies and the overall average of sex distribution in their study was 51 % females and 49 % males [10]. The predominance of males in our study may be due to male-dominant society, and more males turned up for the treatment.
In our study, the right side was more commonly involved (48 %) than the left side (42 %), and bilateral involvement was observed in 10 % cases. In the literature there is varied presentation on the left and right sides in different studies. Gloviczki et al. reported right-side involvement in 49 %, left-side involvement in 46 %, and bilateral involvement in 5 % of patients [11]. Hauer et al. reported right-side involvement in 19 %, left-side involvement in 35 %, and bilateral involvement in 46 % of patients [7].
In the present study, the saphenofemoral junction (SFJ) was incompetent in 74 patients, while the saphenopopliteal junction (SPJ) was incompetent in 12 patients. Twenty-six patients had perforator incompetence as sole cause of their varicose veins. Hoare et al. have reported SFJ incompetence in 96 % and SPJ incompetence in 35 % of patients [12]. Ting et al. have reported SFJ incompetence in 87 % and SPJ incompetence in 13 % of patients in their study [13]. Hence, in most of the patients it is saphenofemoral and saphenopopliteal junction incompetence associated with perforator incompetence. However, in a significant number of patients isolated perforator incompetence is the cause of symptoms as in the present study, indicating the significance of perforators in pathogenesis of varicose veins.
A total of 314 perforators were ligated in 100 limbs in the present study, averaging 3.1 perforators per limb. Pierik et al. have reported a total of 54 perforators with a range of 1–6 perforators, averaging 2.9 perforators per limb [14]. Jugenheimer et al. have reported a total of 456 perforators with a range of 2–11 perforators, averaging 4 perforators per limb [15]. In both the studies reported in the literature, perforators of the Cockett group were most commonly found to be incompetent, followed by perforators of the paratibial group as in the present study.
We did not find any evidence of paraesthesia in the SEPS group, while it was present in 4 % cases in the open ligation group in the present study. In the literature paraesthesia has been reported in 0–11 % cases in open ligation of perforators and in 0–7 % cases in the SEPS group [9, 10, 16]. The possible reason for paraesthesia in the open ligation group is incidental ligation of nerves along with veins. In the present study, we had small hematoma formation in 1 patient (2 %) in the SEPS group, while Tenbrook et al. reported hematoma in 9 % cases [10]. Wound infection was seen in 16 % cases in the open subfascial ligation group as compared to 0 % observed in the SEPS group. In literature wound infection has also been reported in high percentage of patients in open subfascial ligation of perforators—in 32.4 % cases by Stuart et al. and 53 % cases by Sybrandy et al. while it was 10 % and 0 % in the SEPS group respectively [9, 16]. Tenbrook et al. in reported wound infection in 6 % cases following SEPS procedure in their study [10]. Baron et al. reported no hematoma, wound infection, paraesthesia, redness, ecchymosis, and pain in patients undergoing SEPS procedure in their study [17]. The high incidence of wound infection in the open group is because of incision in already compromised skin which causes delayed wound healing and increases chances of infection. In the present study, there was no redness, ecchymosis, and pain at the site of incisions in both the groups as reported in literature [9, 16].
Baron et al. noted decrease in edema, regression of changes, and subjective improvement in physical performance in all the patients in their study. Out of 53 limbs with ulceration, primary healing occurred in 41 within 12 weeks following the SEPS procedure. In the remaining 12 cases, healing took longer time, but none exceeded 6 months [17].
In the present study, SEPS was done in 50 limbs with 6 (12 %) limbs showing ulceration. Wound complications were found to be 0 % and ulcer healing was 100 %. Table 4 compares the results of various studies on SEPS in patients of advanced chronic venous disease. The wound complications in most series of the SEPS group were significantly low ranging from 0 to 6.1 % and are comparable to our study. However, Nelzen reported a wound complication rate of 16 % in his study of 37 patients. Ulcer healing ranged from 66 to 100 % in various studies reported in the literature, while it was 100 % in our cases (Table 4). Luebke and Brunkwall have also reported significant lower rate of wound infection with SEPS and concluded that it benefits most patients of chronic venous insufficiency [22]. Kurdal et al. could also achieve sustainable wound healing with SEPS [23].
Table 4.
Clinical results of SEPS for the treatment of advanced chronic venous disease
| Reference | Year | No. of limbs treated | No. of limbs with ulcer | Concomitant saphenous ablation no. (%) | Wound complications (%) | Ulcer healing No. (%) |
|---|---|---|---|---|---|---|
| Kalra et al. [18] | 2003 | 614 | 273 | 416 (67) | 6.1 % | 246 (90) |
| Tenbrook et al. [10] | 2004 | 1140 | 526 | 718 (63) | 6 % | 463 (88) |
| Baron et al. [17] | 2004 | 98 | 53 | 98 (100) | 0 % | 53 (100) |
| Roka et al. [19] | 2006 | 92 | 21 | 89 (96.7) | 4.3 % | 21 (100) |
| Uncu [20] | 2007 | 28 | 6 | 28 (100) | Nil | 4 (66) |
| Nelzen [21] | 2011 | 37 | 10 | 37 (100) | 16 % | 10 (100) |
| Present study | 2011 | 50 | 6 | 37 (74) | 0 % | 6 (100) |
In the present study healing was quicker in the SEPS group compared to the open subfascial ligation group, with 33 % of limbs in the SEPS group showing complete healing at 14 days compared to none in the open subfascial ligation group. However, all the ulcers in both the groups healed by 3 months. Sybrandy et al. have reported comparable healing rates in both the groups, 95 % in the SEPS and 100 % in the open subfascial ligation group. The ulceration healed within 4 months after surgery in 17 of 20 patients [9]. The healing rate reported by them was also comparable for both the groups, but they reported slightly faster healing in the open subfascial group than in the SEPS group. Tenbrook et al. reported median time of ulcer healing as 30–60 days [10]. Gloviczki et al. also analyzed the contribution of operative experience with SEPS and reported that ulcer healing was longer in centers with fewer than 10 operations [11].
In our study, residual reflux at the perforator level on color Doppler examination done at 3 months was observed in 4 patients (8 %) after open subfascial ligation of perforators, but these patients were asymptomatic. Possibly these perforators missed detection on color Doppler and clinical examination. These missed perforators may be a cause of future recurrence of varicose veins on long-term follow-up. There was no perforator reflux after SEPS in the present study. Sybrandy et al. reported persistent perforators in 20 % of patients in the SEPS group also [9]. A possible explanation could be their subfascial course in the septum intermusculare medialis, which sometimes obscures incompetent perforators. Another explanation could be an erroneously placed or dislodged clip [15]. The difference in results may become more significant on long-term follow-up as the missed perforators in the open ligation group may be a cause of future recurrence. Cosmetic results were good in both the groups in the present study.
Conclusion
Subfascial endoscopic perforator vein surgery is a safe and effective method for treating incompetent perforating veins. The number of perforators ligated in SEPS was more as compared to the open subfascial ligation group. Possibly some perforators may be missed on Doppler localization and ligation, which may be a cause of future recurrence in varicose veins in the open ligation group. Early relief of symptoms in terms of ulcer healing was better in the SEPS group; however, all the ulcers healed in both the groups at 3 months of follow-up. Other major advantage of SEPS was fewer incidences of wound complications which were considerably high in the open ligation group because of incisions in the already compromised skin. Hence, SEPS should be added to varicose vein surgery for the management of incompetent perforators to reduce long-term recurrences and better immediate wound healing.
References
- 1.Almgren B, Eriksson L. Primary deep venous incompetence in limbs with varicose veins. Acta Chir Scand. 1989;155:455–460. [PubMed] [Google Scholar]
- 2.Hammarsten J, Berniad P, Campanello M, Falkenberg M, Henrikson O, Jenson A. A study of mechanisms by which haemodynamic functioning improves following long saphenous vein saving surgery. Phlebology. 1996;11:102–105. [Google Scholar]
- 3.Hauer G. The endoscopic subfascial division of the perforating veins-preliminary report (in German) Vasa. 1985;14:59–61. [PubMed] [Google Scholar]
- 4.Linton RR. The communicating veins of the lower leg and the operative technique for their ligation. Ann Surg. 1938;107:582. doi: 10.1097/00000658-193804000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leach BC, Gold MP. Venous digest. Dermatol Surg. 2003;29:612–615. doi: 10.1046/j.1524-4725.2003.29148.x. [DOI] [PubMed] [Google Scholar]
- 6.Tibbs DJ (1992) Treatment of varicose veins and other manifestations of superficial vein incompetence. In: Varicose Veins and Related Disorders. Oxford: Butterworth heinmann Jordan Hill Ltd., pp. 397–422
- 7.Hauer G, Bergan JJ, Werner A, Mitterhusen M, Nasralla F. Development of endoscopic dissection of perforating veins and fasciotomy for treatment of chronic venous insufficiency. Ann Vasc Surg. 1999;13(4):357–364. doi: 10.1007/s100169900269. [DOI] [PubMed] [Google Scholar]
- 8.Weiss RA, Feied CF, Weiss MA (2001) Vein Diagnosis and Treatment: A comprehensive Approach, 1st ed. McGraw-Hill, pp. 1–304
- 9.Sybrandy JE, van Gent WB, Pierik EG, Wittens CH. Endoscopic versus open subfascial division of incompetent perforating veins in the treatment of venous leg ulceration: long-term follow-up. J Vasc Surg. 2001;33(5):1028–1032. doi: 10.1067/mva.2001.114812. [DOI] [PubMed] [Google Scholar]
- 10.Tenbrook JA, Iafrati MD, Odonnell TF, Wolf MP, Hoffman SN, Pauker SG, et al. Systematic review of outcomes after surgical management of venous disease incorporating subfascial endoscopic perforator surgery. J Vasc Surg. 2004;39(3):583–589. doi: 10.1016/j.jvs.2003.09.017. [DOI] [PubMed] [Google Scholar]
- 11.Gloviczki P, Bergan JJ, Menawat SS, Hobson RW, Kistner RL, Lawrence PF, et al. Safety, feasibility, and early efficacy of subfascial endoscopic perforator surgery: a preliminary report from the North American registry. J Vasc Surg. 1997;25(1):94–105. doi: 10.1016/s0741-5214(97)70325-2. [DOI] [PubMed] [Google Scholar]
- 12.Hoare MC, Nicolaids AN, Miles CR. The role of primary varicose veins in venous ulceration. Surgery. 1982;92:450–453. [PubMed] [Google Scholar]
- 13.Ting ACW, Cheng SWK, Pei H, Jensen TCP. Reduction in deep venous reflux after concomitant subfascial endoscopic perforating vein surgery and superficial vein ablation in advanced primary chronic venous insufficiency. J Vasc Surg. 2006;43:546–550. doi: 10.1016/j.jvs.2005.11.020. [DOI] [PubMed] [Google Scholar]
- 14.Pierik EG, van Urk H, Wittens CH. Efficacy of subfascial endoscopy in eradicating perforating veins of the lower leg and its relation with venous ulcer healing. J Vasc Surg. 1997;26(2):255–259. doi: 10.1016/s0741-5214(97)70186-1. [DOI] [PubMed] [Google Scholar]
- 15.Jugenheimer M, Junginger T. Endoscopic subfascial sectioning of incompetent perforating veins in treatment of primary varicose veins. World J Surg. 1992;16:971–975. doi: 10.1007/BF02067007. [DOI] [PubMed] [Google Scholar]
- 16.Stuart WP, Adam DJ, Bradbury AW, Ruckly CV. Subfascial endoscopic perforator surgery is associated with significantly less morbidity and shorter hospital stay than open operation (Linton’s procedure) Br J Surg. 1997;84:1364–1365. doi: 10.1002/bjs.1800841008. [DOI] [PubMed] [Google Scholar]
- 17.Baron HC, Wayne MG, Santiago CA, Grossi R. Endoscopic subfascial perforator vein surgery for patients with severe, chronic venous insufficiency. Vasc Endovasc Surg. 2004;38(5):439–442. doi: 10.1177/153857440403800507. [DOI] [PubMed] [Google Scholar]
- 18.Kalra M, Gloviczki P. Surgical treatment of venous ulcers: role of subfascial endoscopic perforator vein ligation. Surg Gynecol Obstet. 1968;127:289–290. doi: 10.1016/S0039-6109(02)00198-6. [DOI] [PubMed] [Google Scholar]
- 19.Roka F, Binder M, Bohler-Sommeregger K. Mid-term recurrence rate of incompetent perforating veins after combined superficial vein surgery and subfascial endoscopic perforating vein surgery. J Vasc Surg. 2006;44(2):359–363. doi: 10.1016/j.jvs.2006.04.028. [DOI] [PubMed] [Google Scholar]
- 20.Uncu H. Subfascial endoscopic perforator vein surgery using balloon dissector and saphenous vein surgery in chronic venous insufficiency. Phlebology. 2007;22(3):131–136. doi: 10.1258/026835507780807220. [DOI] [PubMed] [Google Scholar]
- 21.Nelzen O, Fransson I, Swedish Study Group Early results from a randomised trial of saphenous surgery with or without subfascial endoscopic perforator surgery in patients with a venous ulcer. Br J Surg. 2011;98:495–502. doi: 10.1002/bjs.7370. [DOI] [PubMed] [Google Scholar]
- 22.Luebke T, Brunkwall J. Meta-analysis of subfascial endoscopic perforator vein surgery (SEPS) for chronic venous insufficiency. Phlebology. 2009;24(1):8–16. doi: 10.1258/phleb.2008.008005. [DOI] [PubMed] [Google Scholar]
- 23.Kurdal AT, Cerrahoglu M, Iskesen I, Eserdag M, Sirin H. Subfascial endoscopic perforator surgery ameliorates the symptoms of chronic venous ulcer (C6) patients. Int Angiol. 2010;29(1):70–74. [PubMed] [Google Scholar]