Pre-operative anaemia is present in 20–40% of patients scheduled for major elective orthopaedic procedures1–3. Pre-operative anaemia has been linked to post-operative infections, poorer physical functioning and recovery, decreased quality of life, and increased length of hospital stay and mortality1–6. It is not, however, clear whether anaemia is a modifiable risk factor of poorer outcomes and not simply a marker of other conditions that confer increased risk3.
Peri-operative blood loss during these surgical procedures leads to a significant post-operative decline in haemoglobin level. This in turn induces post-operative anaemia and/or worsens pre-existing anaemia7,8. As a result, a significant proportion of patients receive allogeneic blood to treat acute post-operative anaemia. The transfusion of allogeneic blood has, however, been linked to increased post-operative morbidity and mortality and longer hospital stays9–13.
Therefore, an orthodox approach to the Patient Blood Management (PBM) paradigm recommended that patients scheduled for major orthopaedic procedures should have a full blood cell counts, iron status and some inflammatory marker tested, preferably 30 days before the scheduled surgical procedure, to allow the implementation of appropriate treatment, if available14–17. Although the most common sources of anaemia among patients undergoing orthopaedic surgery are related to iron deficiency and chronic diseases, given their co-morbidity profile18, vitamin B12 and folic acid should also be measured and deficiencies replenished accordingly14,15.
Some studies have shown that, for patients presenting with iron deficiency and iron-deficiency anaemia, administration of ferrous salts (100–200 mg/day for 4–6 weeks) improves haemoglobin levels, reduces transfusion rates and, in some cases, shortens the time spent in hospital19,20. If there is poor absorption or poor tolerance of oral iron or an accelerated response to treatment is required, pre-operative intravenous iron supplementation, starting 3–4 weeks prior to the scheduled procedure, increases haemoglobin levels and/or corrects anaemia and reduces allogeneic blood transfusion requirements21–24.
As for patients presenting with moderate anaemia (haemoglobin between 10 and 13 g/dL), but without iron deficiency and/or with clinical or laboratory signs of inflammation, pre-operative administration of recombinant human erythropoietin (rHuEPO) has been proven to increase haemoglobin levels and reduce the rate of allogeneic blood transfusion25. The minimum effective dose of rHuEPO for this indication is presently unknown, but it has been shown that most patients attain the target haemoglobin level with one or two doses22,23,26.
In this issue of Blood Transfusion, Theusinger et al.27 report the results of a pragmatic approach to PBM in major orthopaedic surgery, which was successfully implemented at the Balgrist University Hospital in Zurich (2009–2011; n=6,721). We honestly believe that they must be congratulated for this initiative.
One fundamental pillar of their PBM programme was the detection of pre-operative anaemia, by contacting the patient’s general practitioner when the patient presented to the anaesthesiologist, at least 4 weeks prior to surgery. This highlights the overwhelming importance of enhancing communication/collaboration between primary health care workers and specialised medical staff, by unifying and sharing all patients’ electronic records, and by reducing the high rate of patients not presenting to the anaesthesiologist or presenting too late (70% of patients).
Among the reported patients (n=1,985), 9% were found to be anaemic and were initially treated with one dose of intravenous iron (1,000 mg), rHuEPO (40,000 IU) and vitamin B12 (1 mg), plus 5 mg folic acid orally per day for 4 weeks (n=178). After 14 days, only 15% (n=26) of these patients were still anaemic and received a second dose of intravenous iron, rHuEPO and vitamin B12. All treated patients had normal haemoglobin levels on the day of surgery. The PBM programme also included meticulous surgical technique, optimal surgical blood-saving techniques (cell salvage and/or topical haemostatic agents), and standardised transfusion triggers.
Interestingly, this PBM programme did not involve the use of tranexamic acid, as this may promote a hypercoagulable state in some patients (for example, those with pre-existing thromboembolic events, subjects undergoing hip fracture or cancer surgery, those aged over 60 years, women, etc.) and it has been suggested that individual risk-benefit analysis should be applied rather than routine use in these clinical settings16,28,29. Post-operative cell salvage has been shown to be safe and cost-effective, especially after knee arthroplasty30, but was also not considered despite its potential benefit for patients not reporting to the anaesthesiologists or having exclusion criteria for treatment of anaemia.
Overall, in comparison with the preceding year (2008, n=2,150), this PBM programme was associated with a lower incidence of immediate pre-operative anaemia (9.0% vs 15.4%, p<0.001), a reduction in loss of red blood cell mass (506 mL vs 586 mL, p<0.001), lower transfusion rate (12.8% vs 20.7%, p<0.001), and lower transfusion volume per transfused patient (2.6 Units vs 3.3 Units). Unfortunately, neither length of stay nor complications and serious adverse events could be analysed. Nevertheless, in addition to intra-operative surgical and anaesthetics measure, the effectiveness of this pragmatic blood-saving protocol seems to be due to:
- The stimulatory effect of mostly single rHuEPO doses on erythropoiesis, enhanced by the co-administration of intravenous iron which prevented rHuEPO-induced functional iron deficiency status. This resulted in correction of the pre-operative anaemia without exposing patients to an increased thrombotic risk31. Even when only relatively few general physicians assessed their patients’ iron status, the administered dose of intravenous iron (1,000 mg in 85% of cases) seemed to provide enough iron to correct the pre-operative anaemia and compensate for iron lost due to peri-operative bleeding, without exposing the patients to iron overdose32–34. A more accurate estimation of iron needs, taking into account both baseline haemoglobin level and foreseeable blood loss, would have allowed for a single dose, total iron replenishment using ferric carboxymaltose or iron isomaltoside-1000 and further enhancement of patient throughput.
- The pre-operative supplementation with oral folic acid (5 mg/day) and vitamin B12 (1 mg intramuscularly), as inexpensive and non-toxic treatments, to treat or prevent functional or absolute deficiency during anaemia correction with intravenous iron and rHuEPO in this older population whose levels were not routinely measured18.
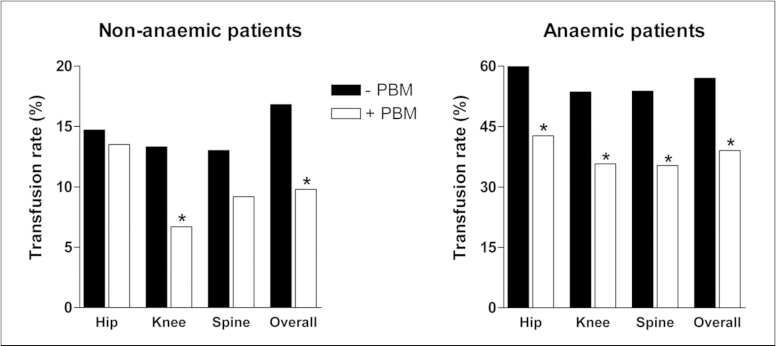
- The use of a restrictive transfusion threshold, as this is one of the most significant determinants of transfusion, thus avoiding overuse of allogeneic blood transfusion17,35–37. Importantly, this beneficial effect was especially relevant for anaemic patients not treated pre-operatively (Figure 1). However, as the mean number of transfused packed red cell units per transfused patient in the whole PBM series was 2.6, there might be room for improvement by not transfusing more than the minimum number of packed red cell units necessary to relieve symptoms of anaemia or to return a patient to a safe haemoglobin range16,17,35–38.
Figure 1.
Transfusion rates according to period, anaemia status and type of surgery.
Transfusion rates were obtained from Theusinger’s study data27.
− PBM: control (2008); + PBM: study period (2009–2011); *: p<0.001.
However, despite the above-mentioned recommendations, quite often we do not have an adequate time-frame to investigate anaemia and implement the appropriate treatment (e.g., patients not reported to the anaesthesiologist or reported too late). In a NATA consensus statement on the management of peri-operative anaemia, the panel suggested the administration of intravenous iron during the peri-operative period for patients undergoing orthopaedic surgery who are expected to develop severe postoperative anaemia14. In a recently published pooled analysis of 2,547 elective and non-elective lower limb procedures, peri-operative or post-operative treatment with intravenous iron (400–600 mg), with or without a single dose of rHuEPO (40,000 IU), plus a restrictive transfusion protocol (haemoglobin threshold <8 g/dL) was shown to reduce allogeneic blood transfusion requirements and shorten time spent in hospital, without having clinically relevant side effects12. Moreover, a retrospective, matched cohort study showed that post-operative administration of intravenous iron (600 mg) after elective lower limb arthroplasty did not increase blood management costs39.
Although the orthodox view is that early pre-operative anaemia assessment, classification and management is preferred, data from more pragmatic approaches suggest that anaemia treatment should always be attempted in major orthopaedic procedures, as any time may be a good time for patients to benefit from it. Future prospective trials of sufficient power should be designed to evaluate the long-term safety, efficacy and cost of these interventions.
Finally, it must be stressed that, although further refinements are needed, this well-defined PBM programme seems to be on the right path to fulfil the aim of performing major surgical orthopaedic procedures without the use of allogeneic blood transfusion and without placing the patient at risk of complications. As stated by the authors “Now that we have shown to everybody that a PBM Programme is successful, a second approach will be taken, trying to diagnose the patients in more detail and allowing a more specific treatment for the anaemia or iron deficiency27”.
Footnotes
Conflict of interest disclosure
Manuel Muñoz has received honoraria for consultancy or lectures and/or travel support from Stryker Ibérica (Spain), Wellspect HealthCare (Sweden), Ferrer Pharma (Spain), Roche (Spain), Vifor Pharma (Spain & Switzerland), PharmaCosmos (Denmark) and Zambon (Spain) but not for this work.
José Antonio García-Erce has received honoraria for lectures and/or consultancy and/or travel support from Vifor Pharma (Switzerland), Vifor Pharma España (Spain) and Amgen Oncology (Spain), but not for this work.
Susana Gómez-Ramírez has nothing to declare.
References
- 1.Spahn DR. Anemia and patient blood management in hip and knee surgery: a systematic review of the literature. Anesthesiology. 2010;113:482–95. doi: 10.1097/ALN.0b013e3181e08e97. [DOI] [PubMed] [Google Scholar]
- 2.Seicean A, Seicean S, Alan N, et al. Preoperative anemia and perioperative outcomes in patients who undergo elective spine surgery. Spine (Phila Pa 1976) 2013;38:1331–41. doi: 10.1097/BRS.0b013e3182912c6b. [DOI] [PubMed] [Google Scholar]
- 3.Wu WC, Schifftner TL, Henderson WG, et al. Preoperative hematocrit levels and postoperative outcomes in older patients undergoing noncardiac surgery. JAMA. 2007;297:2481–8. doi: 10.1001/jama.297.22.2481. [DOI] [PubMed] [Google Scholar]
- 4.Musallam KM, Tamim HM, Richards T, et al. Preoperative anaemia and postoperative outcomes in non-cardiac surgery: a retrospective cohort study. Lancet. 2011;378:1396–407. doi: 10.1016/S0140-6736(11)61381-0. [DOI] [PubMed] [Google Scholar]
- 5.Beattie WS, Karkouti K, Wijeysundera DN, Tait G. Risk associated with preoperative anemia in noncardiac surgery: a single-center cohort study. Anesthesiology. 2009;110:574–81. doi: 10.1097/ALN.0b013e31819878d3. [DOI] [PubMed] [Google Scholar]
- 6.Izuel Rami M, García Erce JA, Gómez-Barrera M, et al. Relationship between allogeneic blood transfusion, iron deficiency and nosocomial infection in patients with hip fracture. Med Clin (Barc) 2008;131:647–52. doi: 10.1157/13128722. [DOI] [PubMed] [Google Scholar]
- 7.Rosencher N, Kerkkamp HE, Macheras G, et al. Orthopedic Surgery Transfusion Hemoglobin European Overview (OSTHEO) study: blood management in elective knee and hip arthroplasty in Europe. Transfusion. 2003;43:459–69. doi: 10.1046/j.1537-2995.2003.00348.x. [DOI] [PubMed] [Google Scholar]
- 8.Colomina MJ, Bagó J, Pellisé F, et al. Preoperative erythropoietin in spine surgery. Eur Spine J. 2004;13(Suppl 1):S40–9. doi: 10.1007/s00586-004-0754-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bierbaum BE, Callaghan JJ, Galante JO, et al. An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am. 1999;81A:2–10. doi: 10.2106/00004623-199901000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Llevelyn CA, Taylor RS, Todd AA, et al. The effect of universal leukoreduction on postoperative infections and length of hospital stay in elective orthopedic and cardiac surgery. Transfusion. 2004;44:489–500. doi: 10.1111/j.1537-2995.2004.03325.x. [DOI] [PubMed] [Google Scholar]
- 11.Pedersen AB, Mehnert F, Overgaard S, Johnsen SP. Allogeneic blood transfusion and prognosis following total hip replacement: a population-based follow up study. BMC Musculoskelet Disord. 2009;10:167. doi: 10.1186/1471-2474-10-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Muñoz M, Gómez-Ramírez S, Cuenca J, et al. Very-short-term perioperative intravenous iron administration and postoperative outcome in major orthopedic surgery: a pooled analysis of observational data from 2547 patients. Transfusion. 2014;54:289–99. doi: 10.1111/trf.12195. [DOI] [PubMed] [Google Scholar]
- 13.Gruskay JA, Fu MC, Bohl DD, et al. Factors affecting length of stay following elective posterior lumbar spine surgery: a multivariate analysis. Spine J. 2013 doi: 10.1016/j.spinee.2013.10.022. pii: S1529-9430(13)01617-3. [DOI] [PubMed] [Google Scholar]
- 14.Beris P, Muñoz M, García-Erce JA, et al. Perioperative anaemia management: consensus statement on the role of intravenous iron. Br J Anaesth. 2008;100:599–604. doi: 10.1093/bja/aen054. [DOI] [PubMed] [Google Scholar]
- 15.Goodnough LT, Maniatis A, Earnshaw P, et al. Detection, evaluation, and management of preoperative anaemia in the elective orthopaedic surgical patient: NATA guidelines. Br J Anaesth. 2011;106:13–22. doi: 10.1093/bja/aeq361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leal-Noval SR, Muñoz M, Asuero M, et al. Spanish Consensus Statement on alternatives to allogeneic blood transfusion: the 2013 update of the “Seville Document”. Blood Transfus. 2013;11:585–610. doi: 10.2450/2013.0029-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liumbruno GM, Bennardello F, Lattanzio A, et al. Italian Society of Transfusion Medicine and Immunohaematology (SIMTI) Working Party. Recommendations for the transfusion management of patients in the peri-operative period. I. The pre-operative period. Blood Transfus. 2011;9:19–40. doi: 10.2450/2010.0074-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bisbe E, Castillo J, Saez M, et al. Prevalence of preoperative anemia and hematinic deficiencies in patients scheduled for elective major orthopedic surgery. Transf Altern Transf Med. 2008;10:166–73. [Google Scholar]
- 19.Cuenca J, Garcia-Erce JA, Martinez F, et al. Preoperative haematinics and transfusion protocol reduce the need for transfusion after total knee replacement. Int J Surg. 2007;5:89–94. doi: 10.1016/j.ijsu.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 20.Rogers BA, Cowie A, Alcock C, Rosson JW. Identification and treatment of anaemia in patients awaiting hip replacement. Ann R Coll Surg Engl. 2008;90:504–7. doi: 10.1308/003588408X301163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Theusinger OM, Leyvraz PF, Schanz U, et al. Treatment of iron deficiency anemia in orthopedic surgery with intravenous iron: efficacy and limits: a prospective study. Anesthesiology. 2007;107:923–7. doi: 10.1097/01.anes.0000291441.10704.82. [DOI] [PubMed] [Google Scholar]
- 22.Gonzalez-Porras JR, Colado E, Conde MP, et al. An individualized pre-operative blood saving protocol can increase pre-operative haemoglobin levels and reduce the need for transfusion in elective total hip or knee arthroplasty. Transfus Med. 2009;19:35–42. doi: 10.1111/j.1365-3148.2009.00908.x. [DOI] [PubMed] [Google Scholar]
- 23.Bisbe E, García-Erce JA, Díez-Lobo AI, Muñoz M. A multicentre comparative study on the efficacy of intravenous ferric carboxymaltose and iron sucrose for correcting preoperative anaemia in patients undergoing major elective surgery. Br J Anaesth. 2011;107:477–8. doi: 10.1093/bja/aer242. [DOI] [PubMed] [Google Scholar]
- 24.Basora M, Colomina MJ, Tio M, et al. Optimizing preoperative haemoglobin with intravenous iron. Br J Anaesth. 2013;110:488–90. doi: 10.1093/bja/aes587. [DOI] [PubMed] [Google Scholar]
- 25.Weber EWG, Slappendel R, Hémon Y, et al. Effects of epoetin alfa on blood transfusions and postoperative recovery in orthopaedic surgery: the European Epoetin Alfa Surgery Trial (EEST) Eur J Anaesthesiol. 2005;22:249–57. doi: 10.1017/s0265021505000426. [DOI] [PubMed] [Google Scholar]
- 26.Rosencher N, Poisson D, Albi A, et al. Two injections of erythropoietin correct moderate anemia in most patients awaiting orthopedic surgery. Can J Anesth. 2005;52:160–5. doi: 10.1007/BF03027722. [DOI] [PubMed] [Google Scholar]
- 27.Theusinger OM, Kind SL, Seifert B, et al. Patient blood management in orthopaedic surgery – a four-year follow-up of transfusion requirements and blood loss from 2008 to 2011 at the Balgrist University Hospital in Zurich, Switzerland. Blood Transfus. 2014;12:195–203. doi: 10.2450/2014.0306-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kozek-Langenecker SA, Afshari A, Albaladejo P, et al. Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol. 2013;30:270–382. doi: 10.1097/EJA.0b013e32835f4d5b. [DOI] [PubMed] [Google Scholar]
- 29.Muñoz M, Páramo JA. Antifibrinolytic agents in current anaesthetic practice: use of tranexamic acid in lower limb arthroplasty. Br J Anaesth. 2014;112:766–7. doi: 10.1093/bja/aeu078. [DOI] [PubMed] [Google Scholar]
- 30.Muñoz M, Ariza D, Campos A, et al. The cost of post-operative shed blood salvage after total knee arthroplasty: an analysis of 1,093 consecutive procedures. Blood Transfus. 2013;11:260–71. doi: 10.2450/2012.0139-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Henry DH, Dahl NV, Auerbach MA. Thrombocytosis and venous thromboembolism in cancer patients with chemotherapy induced anemia may be related to ESA induced iron restricted erythropoiesis and reversed by administration of IV iron. Am J Hematol. 2012;87:308–10. doi: 10.1002/ajh.22262. [DOI] [PubMed] [Google Scholar]
- 32.Cuenca J, García-Erce JA, Martínez F, et al. Perioperative intravenous iron may reduce transfusion requirements and hasten the recovery from postoperative anaemia after knee replacement surgery. Transf Med. 2006;16:335–41. doi: 10.1111/j.1365-3148.2006.00682.x. [DOI] [PubMed] [Google Scholar]
- 33.García-Erce JA, Cuenca J, Haman-Alcober S, et al. Efficacy of preoperative recombinant human erythropoietin administration for reducing transfusion requirements in patients undergoing surgery for hip fracture repair. An observational cohort study. Vox Sang. 2009;97:260–7. doi: 10.1111/j.1423-0410.2009.01200.x. [DOI] [PubMed] [Google Scholar]
- 34.Muñoz M, Naveira E, Seara J, Cordero J. Effects of postoperative intravenous iron on transfusion requirements after lower limb arthroplasty. Br J Anaesth. 2012;108:532–4. doi: 10.1093/bja/aes012. [DOI] [PubMed] [Google Scholar]
- 35.Liumbruno GM, Bennardello F, Lattanzio A, et al. Italian Society of Transfusion Medicine and Immunohaematology (SIMTI) Working Party. Recommendations for the transfusion management of patients in the peri-operative period. II. The intra-operative period. Blood Transfus. 2011;9:189–217. doi: 10.2450/2011.0075-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carson JL, Grossman BJ, Kleinman S, et al. Red blood cell transfusion: a clinical practice guideline from the AABB. Ann Intern Med. 2012;157:49–58. doi: 10.7326/0003-4819-157-1-201206190-00429. [DOI] [PubMed] [Google Scholar]
- 37.Muñoz M, Leal-Noval SR. Restrictive transfusion triggers in major orthopaedic surgery: effective and safe? Blood Transfus. 2013;11:169–71. doi: 10.2450/2013.0276-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Choosing Wisely. Five Things Physicians and Patients Should Question. American Society of Hematology; 2013. [Accessed on 26/02/2014]. Available at: http://www.choosingwisely.org/wp-content/uploads/2013/12/ASH-5things-List_dec2013.pdf. [Google Scholar]
- 39.Muñoz M, Gómez-Ramírez S, Martín-Montañez A, et al. Cost of postoperative intravenous iron therapy in total lower limb arthroplasty: a retrospective, matched cohort study. Blood Transfus. 2014;12:40–9. doi: 10.2450/2013.0088-13. [DOI] [PMC free article] [PubMed] [Google Scholar]