Abstract
Background
The prevalence of human immunodeficiency virus (HIV) in men having sex with men (MSM) is generally higher than that in the average adult male population. In Hong Kong a permanent deferral mechanism is in place to minimise viral transmission during the window period. As regards donor deferral, the attitudes and behaviours of MSM in the community are crucial to ensuring blood safety.
Materials and methods
A web-based questionnaire was constructed in the Chinese language. Through online advertisement and the assistance of outreach workers, sexually active MSM were recruited to participate in the survey. The questionnaire was composed of items on: (i) demographics, (ii) history and frequency of blood donations, (iii) profile of sexual practice, and (iv) views on time-limited vs permanent deferral.
Results
Over a 6-week period in 2012, 250 MSM, three-quarters of whom were aged between 16 and 30 years old, were recruited. Almost half (47.6%) gave a history of blood donation. The majority (75.6%) were repeat donors, one-third of whom gave blood every 3–6 months. Compared to non-donors, a higher proportion of blood donors had had anal sex and multiple partners in the preceding year, while their condom usage rate was similar. Current donors were inclined to agree with time-limited deferral. With the latter’s implementation, the number of donors would increase, but the compliance rate might vary widely.
Discussion
Blood donation is common among MSM in Hong Kong. The risk of HIV transmission depends largely on their compliance with the deferral mechanism applied, irrespectively of whether it is permanent or time-limited.
Keywords: transfusion, MSM, self-deferral, blood safety
Introduction
While blood transfusion is an uncommon route of spread of human immunodeficiency virus (HIV)1, its importance is often highlighted in national public health strategies, both because of the high efficiency of viral transmission in this setting and because of the availability of effective screening to prevent the transmission. As a result of methodological advances and system improvements, the standard of blood safety has continued to rise. HIV may still, however, be transmitted to transfusion recipients if a donation is made during the window period of virus infection, which is estimated to be about 1 week with the use of nucleic acid amplification testing (NAT) in conjunction with serological testing2. As part of risk management, potential donors who may be harbouring the infection during the window period are deferred3.
Strategically, self-deferral of men having sex with men (MSM) from blood donation plays a key role in protecting blood safety because of the higher prevalence of HIV in this group. In metropolitan Hong Kong, for example, the prevalence of HIV in the population is less than 0.1% whereas it is about 4% among MSM4. This observation underlies the rationale for excluding MSM from blood donation, through deferral mechanisms which are either time-limited or permanent. The policy in place in Hong Kong is life-time deferral. Studies have, however, shown that MSM continue to account for a small proportion of blood donors because of failure of self-deferral. This proportion ranged from 1 to 3% in the numerous surveys5–8. Logically, it can be inferred that the risk of transfusion-related HIV transmission is dependent on the compliance of MSM with the self-deferral procedure. To date, research has largely been pursued through post-donation surveys, which could have underestimated the actual practice of blood donation in MSM communities. Against this background, we set out to research MSM in the community to understand their donation behaviours as well as attitudes towards blood safety with regards to HIV transmission. Methodologically this was a feasibility study using an online platform that hosted a specifically designed survey to reach the MSM population. Through the survey we examined the attitudes of MSM towards permanent vs time-limited self-deferral, and their profile of sexual risk behaviours. It was intended that the results of the study would provide information for supporting any change of strategy in the deferral of MSM from blood donation.
Materials and methods
An online questionnaire was constructed in Chinese, field-tested and hosted on a designated website for access by MSM in Hong Kong. Over a 6-week period (1 March to 9 April 2012), an online advertisement publicising the study as a blood donation survey, was placed at a popular gay website to invite the participation of men who met the following entry criteria: (i) Chinese, (ii) aged ≥16 years, and (iii) had had anal and/or oral sex with a man or men. Two online outreach volunteers were recruited and trained to contact potentially eligible MSM through other local internet-based or mobile phone-based social networking platforms, inviting them to log in and join the survey. As a token of appreciation, a HKD20 (USD1=HKD7.8) cash coupon was posted to any participant who completed the survey and provided a postal address to receive the incentive. The survey was conducted anonymously without collection of any personal identifying information.
The survey questionnaire was composed of four categories of items: (i) demographics, including age, educational level, occupation and resident location; (ii) history and frequency of blood donation in Hong Kong; (iii) awareness and attitude towards deferral of MSM -time-limited vs permanent deferral, the latter currently implemented at the Hong Kong Red Cross Blood Transfusion Service which involves the completion of a Health Screening Questionnaire. The Questionnaire is divided into Part A, a one-page description about blood safety; and Part B, a three-page questionnaire with itemised deferrable behaviours which should be declared by all donors before donation. Having sex with a man/men is specifically included in Part B as a permanently deferrable behaviour; (iv) prevalence of unprotected sexual practices.
Data collected from the online survey were transcribed to form a study dataset using Microsoft Excel (Microsoft, Redmond, WA, USA). The statistical analysis was conducted with PASW Statistics 18 (SPSS Inc. Chicago, IL, USA). To compare categorical differences, chi square tests were applied and odds ratios determined. Population means were compared using Student’s t test. For the multivariate analysis comparing sexually active donors and non-donors, logistic regression was applied using the “enter” method, with the following variables: age, employment, education, residency in Hong Kong, sexual debut, sex in the preceding year, multiple sexual partners, having ever paid for sex, sex with females, screening for HIV/sexually transmitted infections (STI), and clinic attendance for STI. P values <0.05 were considered statistically significant. Approval was sought from the Survey and Behavioural Research Ethics Committee of the Chinese University of Hong Kong prior to conducting the survey.
Results
Out of 743 people who visited the online survey platform, 250 (33.6%) MSM completed the survey. Table I gives an overall description of the characteristics of all respondents. Classified by 5-year age bands from 16 to 60, about three-quarters (75.2%) fell between the age of 16 and 30. Half (n=136, 54.4%) were in employment, while 40.4% were students. Some 54.4% had attained university education or above. A majority (86%) were normally resident in Hong Kong. Geographically, Hong Kong can be divided into 18 administrative districts and 412 sub-districts called District Council Constituency Areas (DCCA), each containing a similar size of resident population. The respondents had come from all 18 districts, and 169 (41.0%) of the DCCA (map not shown). The median number of respondents per DCCA was one (range, 0 to 9). Almost half (n=119, 47.6%) of the MSM gave a history of previous blood donation in Hong Kong, of whom 90 (75.6%) were repeat donors. For those who provided their age at first donation (n=114), 78.9% did so at or before the age of 18. Schools (75.6%) and donation centres (62.2%) were both popular locations for donating blood. Excluding the 29 one-time donors, the frequencies of donations among repeat donors (n=90) were: 3-monthly (21.1%), half-yearly (13.3%), yearly (14.4%), every 2 years or more (4.4%). Their total numbers of donations were: 2–5 times (58.9%), 6–10 times (24.4%) and over 10 times (16.7%).
Table I.
Demographic characteristics of MSM joining the online survey on blood donation in Hong Kong (n=250).
| Demographic characteristics | n | % | |
|---|---|---|---|
| Age | 16–20 | 60 | 24.0% |
| 21–25 | 85 | 34.0% | |
| 26–30 | 43 | 17.2% | |
| 31–35 | 32 | 12.8% | |
| 36–40 | 15 | 6.0% | |
| 41–45 | 13 | 5.2% | |
| >45 | 2 | 0.8% | |
|
| |||
| Education | Primary or below | 1 | 0.4% |
| Secondary | 43 | 17.2% | |
| Post-secondary | 70 | 28.0% | |
| University | 136 | 54.4% | |
|
| |||
| Residence | Hong Kong Island | 43 | 17.2% |
| Kowloon Peninsula | 75 | 30.0% | |
| New Territories | 126 | 50.4% | |
| Outside Hong Kong | 6 | 2.4% | |
|
| |||
| Occupational status | |||
| In employment | 136 | 54.4% | |
| Professionals | 46 | 18.4% | |
| Clerks | 30 | 12.0% | |
| Associate professionals | 20 | 8.0% | |
| Service and shop sales | 19 | 7.6% | |
| Managers and administrators | 16 | 6.4% | |
| Elementary occupations | 3 | 1.2% | |
| Crafts and related | 1 | 0.4% | |
| Skilled agricultural & fishery workers, and unclassifiable | 1 | 0.4% | |
| Student | 101 | 40.4% | |
| Not employed | 13 | 5.2% | |
A comparison was made between sexually active MSM who had ever donated blood and those who had not. Ten one-time donors who had given blood before their sexual debut were excluded from the analysis. The demographic profile of the two groups was generally comparable in terms of age and location of residence. More donors were in employment (61.5% vs 48.1%, χ2=4.29, p=0.038), reflecting an older age (though not statistically significant) of the donor population. Overall, donors were more sexually active with more donors having had anal sex (83.5% vs 67.9%, χ2=7.67, p<0.01), and with over five partners (27.5% vs 19.8%, χ2=1.95, p=0.162) in the preceding year, although the difference for the latter did not reach statistical significance. While the proportion of those who consistently used (every intercourse) a condom for anal sex was similar, only 2.2% of donors never used a condom, compared to 10.1% of non-donors (p=0.027). The use of condom for oral sex was uniformly low at <5% in both groups, with the majority never using a condom on any occasion (79.3% and 80% of non-donors and donors, respectively). About one-third had attended clinical services for suspected STI. Screening for STI or HIV was not uncommon, being reported by about half of all respondents. A total of 67 (27.9%) had previously undergone screening for HIV at STI services (30.3% of donors and 26.0% of non-donors). The odds ratios (OR) were calculated to evaluate factors which may be associated with donation (Table II). Only being in employment and having had anal sex in the preceding year were significantly associated with donation behaviour, while the attainment of post-secondary education carried an odds ratio of 1.93 (95% CI: 0.91–4.11) without a statistically significant difference. On multivariate analysis, only anal sex in the preceding year and having attained post-secondary education remained significantly associated with blood donation.
Table II.
Comparison between sexually active MSM who had donated blood (donors, n=109) and those who had not (non-donors, n=131) using univariate and multivariate analyses.
| Donor (n=109) | Non-donor (n=131) | P for χ2 | Odds ratio | 95% CI | Adjusted OR | 95% CI | |||
|---|---|---|---|---|---|---|---|---|---|
| Demographic | |||||||||
| Age >20 years | 87 | 79.8% | 94 | 71.8% | 0.148 | 1.56 | (0.82–2.97) | 1.218 | (0.516–2.872) |
| In employment | 67 | 61.5% | 63 | 48.1% | 0.03* | 1.80** | (1.02–3.20) | 1.786 | (0.845–3.774) |
| Normally in Hong Kong | 96 | 88.1% | 111 | 84.7% | 0.45 | 1.33 | (0.59–3.01) | 1.588 | (0.676–3.729) |
| Attained post-secondary education | 95 | 87.2% | 102 | 77.9% | 0.06 | 1.93 | (0.91–4.11) | 2.373** | (1.070–5.266) |
| Sexual behaviour | |||||||||
| Sexual debut at age ≤ 16 | 43 | 39.4% | 42 | 32.1% | 0.233 | 1.38 | (0.78–2.43) | 1.853 | (0.950–3.615) |
| Anal sex in the preceding year | 91 | 83.5% | 89 | 67.9% | 0.006* | 2.39** | (1.23–4.68) | 2.273** | (1.013–5.104) |
| Consistent condom use# for anal sex | 45 | 49.5% | 39 | 43.8% | 0.449 | 1.25 | (0.67–2.35) | ||
| Oral sex in the preceding year | 100 | 91.7% | 116 | 88.5% | 0.411 | 1.44 | (0.56–3.74) | 0.654 | (0.224–1.908) |
| Consistent condom use# for oral sex | 4 | 4.0% | 5 | 4.3% | 0.909 | 0.93 | (0.18–4.43) | ||
| >5 sex partners in preceding year | 30 | 27.5% | 26 | 19.8% | 0.162 | 1.53 | (0.81–2.92) | 1.106 | (0.532–2.300) |
| Has ever paid for sex | 13 | 11.9% | 11 | 8.4% | 0.36 | 1.48 | (0.59–3.73) | 1.088 | (0.394–3.003) |
| Sex with females | 5 | 4.6% | 4 | 3.1% | 0.533 | 1.53 | (0.32–7.88) | 1.179 | (0.236–5.901) |
| Health- seeking behaviours | |||||||||
| Screening for STI or HIV in the past | 63 | 57.8% | 67 | 51.1% | 0.303 | 1.31 | (0.76–2.26) | 0.973 | (0.497–1.903) |
| Attended clinic for suspected STI | 35 | 32.1% | 33 | 25.2% | 0.236 | 1.40 | (0.77–2.56) | 0.997 | (0.471–2.111) |
consistent condom use refers to the use of condom for every sexual contact in the preceding 1 year.
Significant for chi-square test;
Significant for odds ratio.
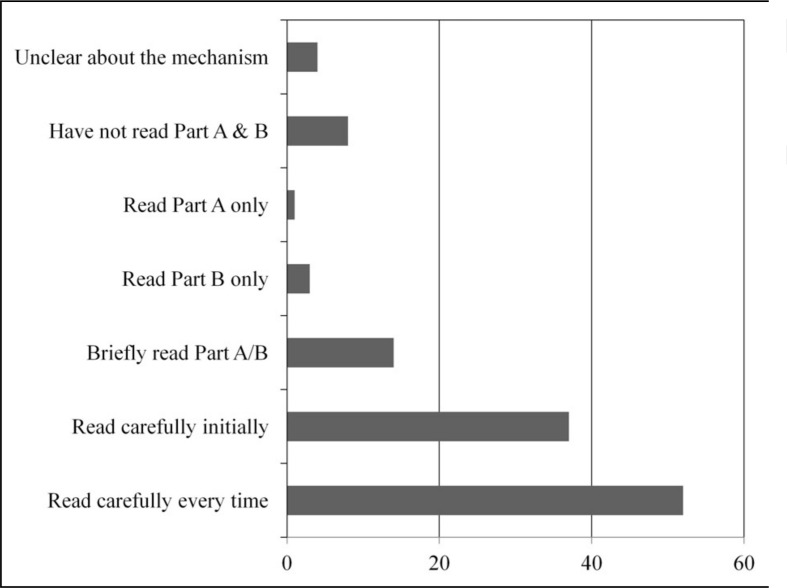
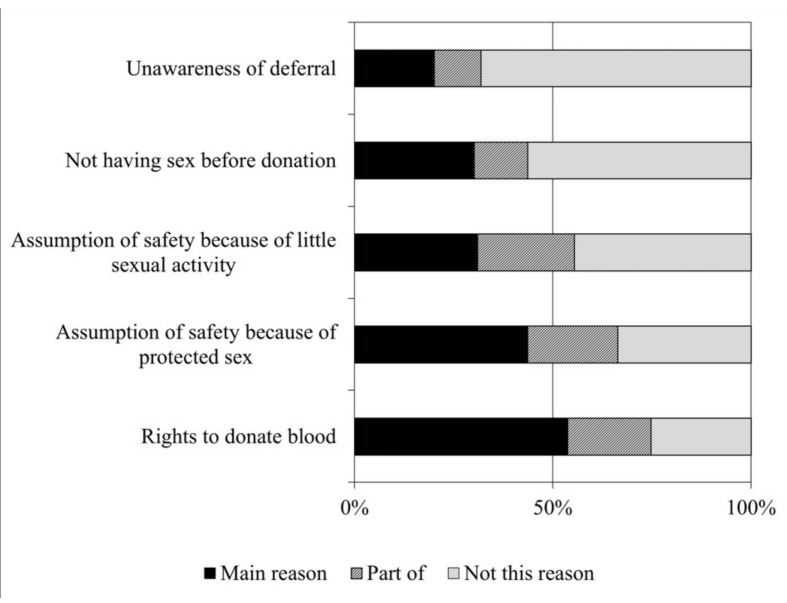
Figure 1 shows the attitudes of donors towards the Health Screening Questionnaire. Four (3.4%) were unclear about what the deferral mechanism was, while less than half (43.7%) had read both parts in detail for every donation. Non-compliance to donor deferral was largely due to the respondents’: (i) belief of their right to donate (53.8% giving this as the main reason); and (ii) confidence about the safety of their blood at the time of donation (43.7% as the main reason) (Figure 2). MSM were further questioned about their views on time-limited deferral. Overall, 56.4% agreed and 24.8% disagreed/objected to changing from permanent to time-limited deferral. If implemented, 34.3% of the non-donors would likely or definitely go for donation (Table IIIa) while more donors would increase (32.8%) rather than decrease (15.1%) their frequency of donation. By adding the number of non-donors indicating intention to donate to the pool of donors, the number of sexually active donors would increase from the current number of 109 to between 122 and 194. Table IIIb shows the number and proportion of MSM who would comply with time-limited deferral by declaring their MSM status on the Health Screening Questionnaires, in the event they went for blood donation when the new mechanism became operative. Only 21.8% of current MSM donors would definitely declare. The proportion who would not declare was 18.5% for current donors and 15.3% for non-donors. Of all future donors (current donors who would continue to donate plus current non-donors who may begin to donate) only half would complete the Health Screening Questionnaire if time-limited deferral is implemented. The number of non-compliant donors would range from 89 to 139, or 35.6% to 55.6% of all MSM (calculations not shown).
Figure 1.
Awareness of and response to the Health Screening Questionnaire before donation (n=119).
Part A gives a general explanation about blood safety, while Part B is the questionnaire which every donor must complete before proceeding to donation.
Figure 2.
Reasons for non-compliance with the current donor deferral mechanism.
Table IIIa.
Attitudes of MSM towards time-limited deferral of blood donors.
Intention to donate blood if permanent deferral is replaced by time-limited deferral, as claimed by non-donors (n=131) and donors (n=119).
| Non-donor | Donor | |||
|---|---|---|---|---|
|
|
||||
| n | % | n | % | |
| Would definitely go for donation | 21 | 16.0% | - - | - - |
| Very likely go for donation | 24 | 18.3% | - - | - - |
| Possibly go for donation | 30 | 22.9% | - - | - - |
| Would not go for donation | 33 | 25.2% | - - | - - |
| Currently undecided | 23 | 17.6% | - - | - - |
| Would donate more frequently | - - | - - | 39 | 32.8% |
| Would donate less frequently | - - | - - | 18 | 15.1% |
| Same frequency of donation | - - | - - | 62 | 52.1% |
|
| ||||
| Total | 131 | 100.0% | 119 | 100.0% |
Table IIIb.
Attitudes of MSM towards time-limited deferral of blood donors.
Intention to comply* with time-limited deferral among non-donors (n=131) and donors (n=119).
| Non-donor | Donor | |||
|---|---|---|---|---|
|
|
||||
| n | % | n | % | |
| Would definitely declare | 47 | 35.9% | 26 | 21.8% |
| Likely to declare | 25 | 19.1% | 45 | 37.8% |
| Possibly; may not declare | 24 | 18.3% | 15 | 12.6% |
| Would not declare | 20 | 15.3% | 22 | 18.5% |
| Currently undecided | 15 | 11.5% | 11 | 9.2% |
|
| ||||
| Total | 131 | 100.0% | 119 | 100.0% |
Compliance means the declaration of an individual that he is a MSM while completing the Health Screening Questionnaire before donation.
Discussion
On a global scale, transmission of HIV through blood transfusion is distinctly uncommon, accounting for an insignificant proportion of reported HIV infections in most countries. In places where effective screening is in force, the residual risk of HIV transmission during the window period is estimated to be less than 1 per 1–4 million donations9–11. Theoretically HIV transmission from MSM donors could not occur if they self-defer permanently. Our current study on MSM recruited online in Hong Kong revealed that almost half (43.6%) of the sexually MSM who participated in the study have not complied with this policy. Elsewhere, in the United Kingdom, one study involving MSM reported that 10.6% had donated blood12. As the sampling frame was different, comparisons of these results are not possible. The MSM donors in our study were sexually more active as evidenced by the report of more sexual activity in the preceding year. This does not necessarily equate to a higher risk of HIV transmission as more donors practised protected anal sex, compared to non-donors. The slightly higher proportion of donors above the age of 20 may mean that given time, more MSM would give blood when they become familiar with the activity.
This was a unique study in which the feasibility of online community sampling was tested to address the issue of blood donor deferral in MSM in a Chinese population in Asia. The alarming proportion of blood donors in the survey suggested that they could have been drawn from a highly selected population of MSM in the community. Sampling bias could be a major limitation. A potential pitfall could have been the attraction of donors to the survey, as the study was advertised as one relating to blood donation. As a result, donors were probably over-represented. From a demographic perspective, the study targeted MSM actively surfing the internet, many of whom could have been using the same platform to seek partners13,14. It was, therefore, hardly surprising to find relatively young MSM with a high prevalence of risky behaviours, as has been reported in other studies14. The broad spatial distribution of all enrolled MSM could not be taken as de facto proof of representativeness. Despite the wide coverage, caution should be taken with extrapolating the study’s results to the wider MSM community. Surprisingly, the high proportion of donors in this study contrasts significantly with the small number of MSM who were self-deferred (only 56 in 2012) by the Blood Transfusion Service, against the background of some 80,000 male donors who had given blood in the same year.
As donation-linked HIV transmission is associated with non-compliance with deferral, it is important to elicit reasons for failure in effectively completing the Health Screening Questionnaire. Our results suggest that MSM had a poor appreciation of the importance of self-deferral, as less than half indicated that they had read the Questionnaire in details. Lack of understanding of deferral criteria could be an important reason for non-compliance, as elicited in another study12. Anal/oral sex is not specifically mentioned in the Screening Questionnaire and this may also affect the responses of potential donors as regards the definition of man-with-man sex15. As a significant proportion of donors considered it their right to give blood, it is not surprising that they are determined to continue to donate blood irrespective of whether the deferral is life-time or time-limited. Worldwide, there is a trend towards switching to deferral based on the practice of risk behaviours, a strategy that has also gained the support of the public6. From our results, switching to time-limited deferral would invariably increase the number of MSM donors, as some who did not donate in the past would go for donation. Whether this would mean an additional risk of HIV transmission depends a lot on the future compliance of donors12. Motivation would likewise be another dimension, as a significant proportion considered donation as a means of health screening, thus attracting test-seekers to join the pool of donors16–17. If more MSM were to donate blood and most complied with the deferral strategy, the larger number of donors would not lead to a higher risk of transmission of HIV. However, our findings cannot demonstrate that this would be the case, as the proportion of non-compliant donors could range between a level higher to one lower than the current proportion of donors in the MSM community.
The survey and its results did, however, enable us to draw two main conclusions. Firstly, an online survey is a feasible means of accessing MSM in the community, though we do acknowledge that the sample could be highly selected. Secondly, despite drawbacks in sampling, non-compliance to permanent deferral of MSM at the transfusion service is common. From the results of the study, it is envisaged that the future risk of HIV transmission arising from blood transfusion would hinge on the actual level of non-compliance to the self-deferral mechanism in place. In the future development of self-deferral policies, it is important to consider the inclusion of measures which may enhance compliance, for example, public education, provision of relevant information before donation, and working closely with the MSM community to develop common understanding of blood safety. As donor deferral constitutes only one aspect of strategies for blood transfusion safety, other interventions such as further shortening the window period of testing methodologies would need to be pursued in parallel.
Acknowledgements
We thank Horas Wong and two online outreach volunteers for helping in the recruitment of MSM to join the survey. The advice of the staff of the Hong Kong Red Cross Blood Transfusion Service is acknowledged. This work was supported by the Council for the AIDS Trust Fund (MSS189R), Hong Kong Special Administrative Region Government.
Footnotes
The Authors declare no conflicts of interest.
References
- 1.Takei T, Amin NA, Schmid G, et al. Progress in global blood safety for HIV. J Acquir Immune Defic Syndr. 2009;52(Suppl 2):S127–31. doi: 10.1097/QAI.0b013e3181baf0ac. [DOI] [PubMed] [Google Scholar]
- 2.Busch MP, Glynn SA, Stramer SL, et al. NHLBI-REDS NAT Study Group. A new strategy for estimating risks of transfusion-transmitted viral infections based on rates of detection of recently infected donors. Transfusion. 2005;45:254–64. doi: 10.1111/j.1537-2995.2004.04215.x. [DOI] [PubMed] [Google Scholar]
- 3.Leiss W, Tyshenko M, Krewski D. Men having sex with men donor deferral risk assessment: an analysis using risk management principles. Transfus Med Rev. 2008;22:35–57. doi: 10.1016/j.tmrv.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 4.Special Preventive Programme, Centre for Health Protection. HIV Surveillance Report-2010 Update. Hong Kong: Department of Health; 2011. [Accessed on 21/01/2013]. Available at: http://www.info.gov.hk/aids/english/surveillance/sur_report/hiv10.pdf. [Google Scholar]
- 5.Sanchez AM, Schreiber GB, Nass CC, et al. Retrovirus Epidemiology Donor Study. The impact of male-to-male sexual experience on risk profiles of blood donors. Transfusion. 2005;45:404–13. doi: 10.1111/j.1537-2995.2005.03421.x. [DOI] [PubMed] [Google Scholar]
- 6.Goldman M, Yi QL, Ye X, et al. Donor understanding and attitudes about current and potential deferral criteria for high-risk sexual behavior. Transfusion. 2011;51:1829–34. doi: 10.1111/j.1537-2995.2011.03078.x. [DOI] [PubMed] [Google Scholar]
- 7.Stigum H, Bosnes V, Ørjasaeter H, et al. Risk behavior in Norwegian blood donors. Transfusion. 2001;41:1480–5. doi: 10.1046/j.1537-2995.2001.41121480.x. [DOI] [PubMed] [Google Scholar]
- 8.Lau JT, Thomas J, Lin CK. HIV-related behaviours among voluntary blood donors in Hong Kong. AIDS Care. 2002;14:481–92. doi: 10.1080/09540120208629667. [DOI] [PubMed] [Google Scholar]
- 9.Zou S, Dorsey KA, Notari EP, et al. Prevalence, incidence, and residual risk of human immunodeficiency virus and hepatitis C virus infections among United States blood donors since the introduction of nucleic acid testing. Transfusion. 2010;50:1495–504. doi: 10.1111/j.1537-2995.2010.02622.x. [DOI] [PubMed] [Google Scholar]
- 10.Kim MJ, Park Q, Min HK, Kim HO. Residual risk of transfusion-transmitted infection with human immunodeficiency virus, hepatitis C virus, and hepatitis B virus in Korea from 2000 through 2010. BMC Infect Dis. 2012;12:160. doi: 10.1186/1471-2334-12-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hourfar MK, Jork C, Schottstedt V, et al. German Red Cross NAT Study Group. Experience of German Red Cross blood donor services with nucleic acid testing: results of screening more than 30 million blood donations for human immunodeficiency virus-1, hepatitis C virus, and hepatitis B virus. Transfusion. 2008;48:1558–66. doi: 10.1111/j.1537-2995.2008.01718.x. [DOI] [PubMed] [Google Scholar]
- 12.Grenfell P, Nutland W, McManus S, et al. Views and experiences of men who have sex with men on the ban on blood donation: a cross sectional survey with qualitative interviews. BMJ. 2011;343:d5604. doi: 10.1136/bmj.d5604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sullivan PS, Khosropour CM, Luisi N, et al. Bias in online recruitment and retention of racial and ethnic minority men who have sex with men. J Med Internet Res. 2011;13:e38. doi: 10.2196/jmir.1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elford J, Bolding G, Davis M, et al. Web-based behavioral surveillance among men who have sex with men: a comparison of online and offline samples in London, UK. J Acquir Immune Defic Syndr. 2004;35:421–6. doi: 10.1097/00126334-200404010-00012. [DOI] [PubMed] [Google Scholar]
- 15.O’Brien SF, Ram SS, Yi QL, Goldman M. Donor’s understanding of the definition of sex as applied to predonation screening questions. Vox Sang. 2008;94:329–33. doi: 10.1111/j.1423-0410.2007.01034.x. [DOI] [PubMed] [Google Scholar]
- 16.Damesyn MA, Glynn SA, Schreiber GB, et al. NHLBI Retrovirus Epidemiology Donor Study. Behavioral and infectious disease risks in young blood donors: implications for recruitment. Transfusion. 2003;43:1596–603. doi: 10.1046/j.1537-2995.2003.00532.x. [DOI] [PubMed] [Google Scholar]
- 17.Goncalez TT, Sabino EC, Murphy EL, et al. Human immunodeficiency virus test-seeking motivation in blood donors, São Paulo, Brazil. Vox Sang. 2006;90:170–6. doi: 10.1111/j.1423-0410.2006.00743.x. [DOI] [PubMed] [Google Scholar]