Abstract
Apophyseal injuries are particularly common in adolescents when the growth spurt that accompanies puberty places increased strain on developing bones and muscles. Bone growth in particular exceeds that of soft tissues resulting in relatively tight musculature and subsequent excessive strain at these sites of tendon insertion into bone. We describe a case of a young athlete who presented with chronic hip pain after an anterior inferior iliac spine apophyseal injury with subsequent haematoma formation under the iliacus muscle. There was no evidence of a bleeding disorder. In view of the late presentation, he was managed non-operatively. This injury requires a low threshold for early cross-sectional imaging. The delay in management in this case did not lead to any long-term sequelae.
Background
Apophyseal injuries of the pelvis are relatively uncommon and are seen in adolescents aged between 14 and 25 years who are involved in competitive sports.1 These include apophysitis (inflammation of the apophyses from repetitive muscle pull) and apophyseal avulsion fractures. With an increasing number of younger individuals taking up competitive sports, the incidence of these injuries is likely to rise. We describe a rare case of a young athlete who presented with chronic hip pain after an anterior inferior iliac spine (AIIS) apophyseal injury and was found to have a large haematoma under the iliacus muscle. Literature on AIIS apophyseal injuries is limited and they are often mistaken for muscle and tendon injuries. There have been no previous cases reported with an associated submuscular haematoma leading to long-term hip pain limiting activity. Although not seen in our patient, iliacus haematoma formation carries a significant risk of femoral nerve palsy which may persist even after surgical decompression.2–4 Our case highlights the importance of early cross-sectional imaging in adolescent athletes with injuries around the pelvic apophyses, with the view to avoid misdiagnosis and identify associated injuries with potential long-term sequelae.
Case presentation
A 14-year-old athlete presented with a 10-month history of right-sided hip pain following a minor fall during a football match. He had recently undergone a growth spurt. The patient had persistent hip pain which was exacerbated by activity and although he continued participating in sports, the pain did not allow him to run at full speed or play to his full potential. At no point during his history did he develop any weakness or para-aesthesia of the affected side. He had no significant medical history and there was no family history of a bleeding disorder. He was not taking any medication.
He was 5 feet 10 inches tall and of slim stature. There was no gross asymmetry of the spine and his level gait was normal. Examination of the hips revealed no focal tenderness or deformity. External rotation was limited to 30° on the right compared with 60° on the left. Internal rotation of the right hip was limited to 10° and reproduced his hip pain. All other movements were normal and there was no neurovascular deficit.
Investigations
All blood markers and coagulation parameters were within normal limits. Plain X-rays (figure 1) ruled out slipped upper femoral epiphyses (SUFE) as a cause of his symptoms. MRI of the pelvis (figure 2) was therefore requested and revealed bone marrow oedema and widening of the apophyseal plate at the right AIIS, suggesting an injury to this site. A 6 cm×7 cm haematoma was seen tracking under the right iliacus muscle and communicating with the AIIS.
Figure 1.
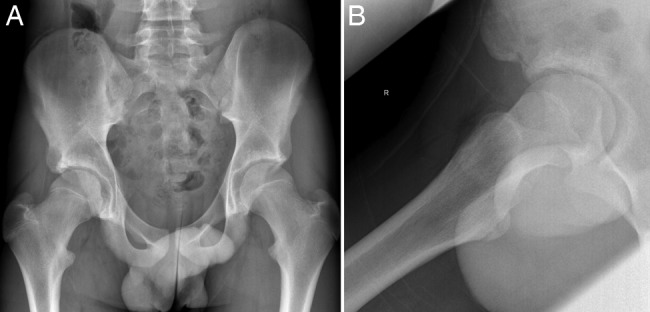
Plain X-ray of the pelvis (A) and right hip (B) did not reveal any obvious abnormality.
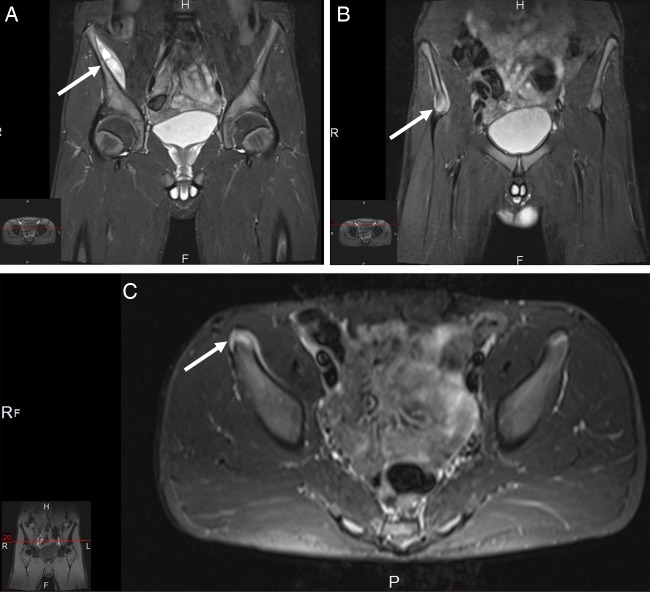
Figure 2.
Fat-saturated coronal and axial MRI of the pelvis. White arrows show (A) a lentiform collection under the right iliacus muscle communicating with (B and C) inflammatory changes around the anterior inferior iliac spine (AIIS) and widening of the right AIIS apophyses.
Differential diagnosis
When considering hip pain in the adolescent patient, there are numerous differentials to consider. Bony pathologies such as stress and avulsion fractures, SUFE or Perthe’s disease were high on the list of possible diagnoses, however plain film X-ray was used to rule out these early in the diagnostic process. Infectious causes such as septic arthritis, osteomyelitis and tuberculosis were also considered, however the fact that the patient was systemically well, symptoms were relatively mild and all inflammatory markers were within normal limits resulted in a low probability of infection as the cause of the symptoms. A rarer cause of chronic hip pain would be due to a neoplastic process, however this was again excluded using the imaging modalities described. The chronic and relatively mild nature of the symptoms, the history of a sports injury and the results of relevant blood tests and imaging, all pointed towards the identified AIIS avulsion and subiliacus haematoma as the cause of the patient’s condition.
Treatment
The patient was managed non-operatively with regular physiotherapy, quadriceps strengthening exercises and no restriction of activity.
Outcome and follow-up
His symptoms resolved over a period of 6 weeks. A repeat MRI at 6 months following conservative management demonstrated a resolution of the AIIS bone marrow oedema and the previously noted subiliacus haematoma. No residual functional or structural deformity at 6-month follow-up was observed.
Discussion
The AIIS is the site of attachment of the direct head of the rectus femoris muscle (RFM). The indirect (reflected) head of the RFM originates from the lateral acetabular rim.5 6 It is a biarticular muscle in that it crosses the hip as well as the knee joints and inserts into the base of the patella via a common quadriceps tendon. When the hip is flexed, the RFM is only a weak extensor of the knee. This is a result of active insufficiency as the RFM is already shortened. However with the hip extended, it exerts a powerful extension moment on the knee. During activities involving strenuous running and kicking, the RFM is exposed to significant stresses in the form of stretching, eccentric and concentric contractions.7 These place its proximal attachment at the AIIS apophyses at high risk of injury in skeletally immature individuals involved in sports such as soccer and rugby.
The AIIS is one of the most common sites of pelvic apophyseal injury and accounts for more than 20% of such injuries in adolescent athletes.8 Rossi and Dragoni investigated pelvic apophyseal fractures in 203 adolescent athletes and found the ischial tuberosity to be the most common site of injury followed by the AIIS, and then the anterior superior iliac spine (ASIS), superior corner of pubic symphysis and iliac crest. The AIIS therefore appears to be frequently injured despite later closure of the ASIS apophyseal cartilage9 (closure between 20 and 25 years old, compared with AIIS closure between 16 and 18 years old). Clinically, acute AIIS apophyseal injuries present with tenderness in the anterior groin and pain on resisted active and passive flexion of the hip and knee.10 11 In our case, there was a delay in presentation and these acute signs were not present on examination.
Submuscular and intramuscular iliopsoas haematomas may be precipitated by trauma alone4 but have characteristically been described in patients with haemophilia and those on anticoagulation therapy.2 3 The presentation is that of groin pain, left iliac fossa mass, fixed flexion deformity of the hip and characteristic signs of femoral nerve compression often requiring surgical intervention if progressive.5 Goodfellow et al9 described the mechanism of femoral nerve compression in these cases by demonstrating how fluid (haematoma) increased pressure in the fibrous iliacus compartment and compressed the nerve within the fascia of the iliacus muscle as it thickens and narrows distally.1 In a review looking at patients who underwent surgical decompression, Barrington8 was the first to describe two distinct types of haemorrhagic femoral neuropathy; subperiosteal haematomas lifting the iliacus muscle off the iliac blade and haematomas within the body of the iliacus muscle.2 He argued whether operating on these patients made any difference to outcome. Recently, researchers have reported complete resolution of symptoms and return to full activity after non-operative management of iliacus haematomas in adolescents who presented with femoral neuropathy and had no worsening of their neurological findings.12 13
We present a unique case of late presentation of an apophyseal injury of the AIIS which resulted in a large subiliacus haematoma in an adolescent athlete without any of the characteristic signs and symptoms described previously and with no history of a bleeding diathesis. The only abnormality on examination was decreased internal and external rotation compared with the contralateral hip. The patient's symptoms resolved with non-operative management. In agreement with previous reports, a subiliacus haematoma with no signs of progressive femoral nerve compression may well be managed non-operatively.
Learning points.
The anterior inferior iliac spine (AIIS) accounts for more than 20% of all pelvic apophyseal injuries.
AIIS injuries can present with submuscular haematomas that can potentially cause long-term disability.
Young athletes with injuries around the pelvic apophyses should be investigated early with three-dimensional imaging.
Footnotes
Contributors: MAK collected patient-related data and imaging, wrote and revised the manuscript. He is the guarantor. SRW and MSI helped in acquiring clinical data, and had drafted and revised the manuscript. FSH acquired case notes, interpreted the case report findings, revised and approved the final draft, identified and managed the case.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Orchard JW. Intrinsic and extrinsic risk factors for muscle strains in Australian football. Am J Sports Med 2001;29:300–3 [DOI] [PubMed] [Google Scholar]
- 2.Bordalo-Rodrigues M, Rosenberg ZS. MR imaging of the proximal rectus femoris musculotendinous unit. Magn Reson Imaging Clin N Am 2005;13:717–25 [DOI] [PubMed] [Google Scholar]
- 3.Rossi F, Dragoni S. Acute avulsion fractures of the pelvis in adolescent competitive athletes: prevalence, location and sports distribution of 203 cases collected. Skeletal Radiol 2001;30:127–31 [DOI] [PubMed] [Google Scholar]
- 4.Browning KH. Hip and pelvis injuries in runners: careful evaluation and tailored management. Phys Sports Med 2001;29:23–34 [DOI] [PubMed] [Google Scholar]
- 5.Hasselman CT, Best TM, Hughes C, IV, et al. An explanation for various rectus femoris strain injuries using previously undescribed muscle architecture. Am J Sports Med 1995;23:493–9 [DOI] [PubMed] [Google Scholar]
- 6.Rockwood CA, Beaty JH, Kasser JR. Rockwood and Wilkins’ fractures in children. In: Beaty JH, Kasser JR. eds 7th edn; associate editors, David L. Skaggs, John M. Flynn, Peter M. Waters. eds Philadelphia, PA; London: Lippincott Williams & Wilkins, 2010:840 [Google Scholar]
- 7.Resnick JM, Carrasco CH, Edeiken J, et al. Avulsion fracture of the anterior inferior iliac spine with abundant reactive ossification in the soft tissue. Skeletal Radiol 1996;25:580–4 [DOI] [PubMed] [Google Scholar]
- 8.Barrington RL. Haemorrhagic femoral neuropathy. Injury 1982;14:170–3 [DOI] [PubMed] [Google Scholar]
- 9.Goodfellow J, Fearn CB, Matthews JM. Iliacus haematoma. A common complication of haemophilia. J Bone Joint Surg Br 1967;49:748–56 [PubMed] [Google Scholar]
- 10.Gertzbein SD, Evans DC. Femoral nerve neuropathy complicating iliopsoas haemorrhage in patients without haemophilia. J Bone Joint Surg Br 1972;54:149–51 [PubMed] [Google Scholar]
- 11.Patel A, Calfee R, Thakur N, et al. Non-operative management of femoral neuropathy secondary to a traumatic iliacus haematoma in an adolescent. J Bone Joint Surg Br 2008;90:1380–1 [DOI] [PubMed] [Google Scholar]
- 12.Scott WN, Nisonson B, Nicholas JA. Principles of sports medicine. Baltimore; London: Williams & Wilkins, 1984 [Google Scholar]
- 13.Seijo-Martinez M, Castro del Rio M, Fontoira E, et al. Acute femoral neuropathy secondary to an iliacus muscle hematoma. J Neurol Sci 2003;209:119–22 [DOI] [PubMed] [Google Scholar]