Abstract
We present two cases of spontaneous fractures of the S-ROM femoral stem prosthesis implanted by different surgeons within 5 years of implantation. Both the stems fractured in the mid-distal stem at the junction of the main body and the slotted portion. Both fractures affected the posterior tine only. Our aim in publication is to ensure that this is an isolated problem and not an under-reported phenomenon. We are not aware of any previous reports of spontaneous fracture of the distal stem.
Background
The current hot topic in orthopaedics is implant safety after several high profile recalls and complications with prostheses. This has encouraged surgeons to report prosthesis-related complications to ensure that there are no hidden trends. Additionally, it was interesting to note that the pain caused in both cases was transient and successfully treated conservatively.
Case presentation
The S-ROM modular hip system has been used successfully for more than 27 years in several hundred thousand cases with studies showing more than 98% long-term survivorship.1–3 The design of the stem features flutes to enhance torsional stability and the distal third has a coronal slot to reduce the stiffness of the distal stem. This was intended to reduce the modulus mismatch between the prosthesis and the bone and is thought to reduce the risk of femoral fracture during insertion and/or reduce anterior thigh pain.4 5 The slot allows the stem to bend with the anterior bow of the femur and is thought to enhance stem fixation.6 7
We present two cases of spontaneous fracture of the distal stem. We are not aware of any previous reports of fractures in this part of the stem.
Case report
Case 1: A 75-year-old woman had a spontaneous onset of right-sided thigh pain when bearing weight. There were no reported episodes of trauma and she continued to be able to bear weight. She had an uncomplicated primary hip arthroplasty in September 2008 for osteoarthritis via a posterior approach. The stem was an S-ROM (DePuy) 16×11×150 with a 36+6 lateral offset neck through a 16F XXL ZT hydroxyapatite-coated proximal sleeve. The patient's medical history included a contralateral total hip replacement (THR) in 1990 (revised in 2000 for polyethylene wear and osteolysis), osteoporosis and breast cancer in 1989.
The patient attended clinic a month after the onset of pain (4 years after insertion of stem). Clinical examination did not reveal any abnormality and she had a good range of movement.
Case 2: A 68-year-old woman had a sudden onset of left-sided thigh and knee pain. There were no reported episodes of trauma, and she continued to be able to bear weight although the pain worsened over the 6 weeks prior to consultation. The latest hip replacement was performed in August 2008; this was a single-stage revision for infection where the S-ROM stem and bearing surfaces were replaced resulting in the following construct: 16×11×150 with a 36+6 lateral offset neck through the pre-existing hydroxyapatite-coated proximal sleeve (size not recorded).
The patient's medical history includes developmental hip dysplasia for which she underwent a Salter osteotomy in 1975. She subsequently underwent a complex primary THR using an uncemented S-ROM femoral prosthesis in 1991. This was revised for polyethylene wear and osteolysis in 2003 (original sleeve left in situ and new stem replaced). She also had the contralateral hip replaced in 1997, and ongoing medical problems include Charcot-Marie-Tooth syndrome, hyperthyroidism and recurrent urinary tract infections.
The patient presented 6 weeks after the onset of pain (4 years after insertion of stem). Clinical examination was unremarkable.
Investigations
Case 1: Radiographs (figures 1 and 2) showed a fracture of the posterior tine of the slotted section of the femoral prosthesis.
Figure 1.

Case 1: Antero-posterior radiograph of the right hip.
Figure 2.
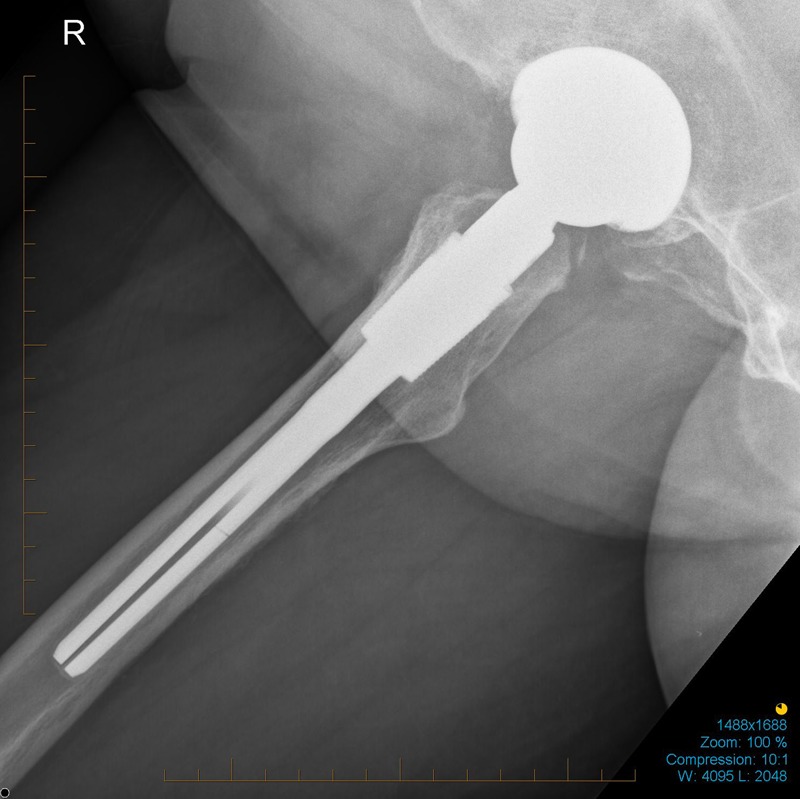
Case 1: Lateral radiograph of the right hip.
Case 2: Radiographs (figures 3 and 4) show a fracture of the posterior tine of the slotted section of the femoral prosthesis.
Figure 3.
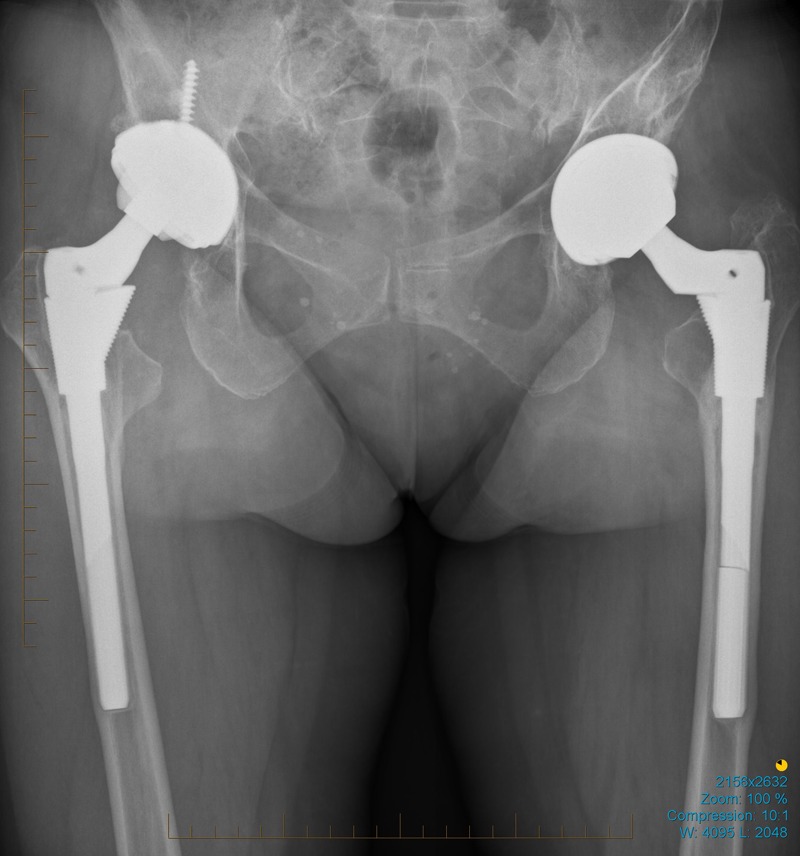
Case 2: Antero-posterior radiograph of the pelvis.
Figure 4.
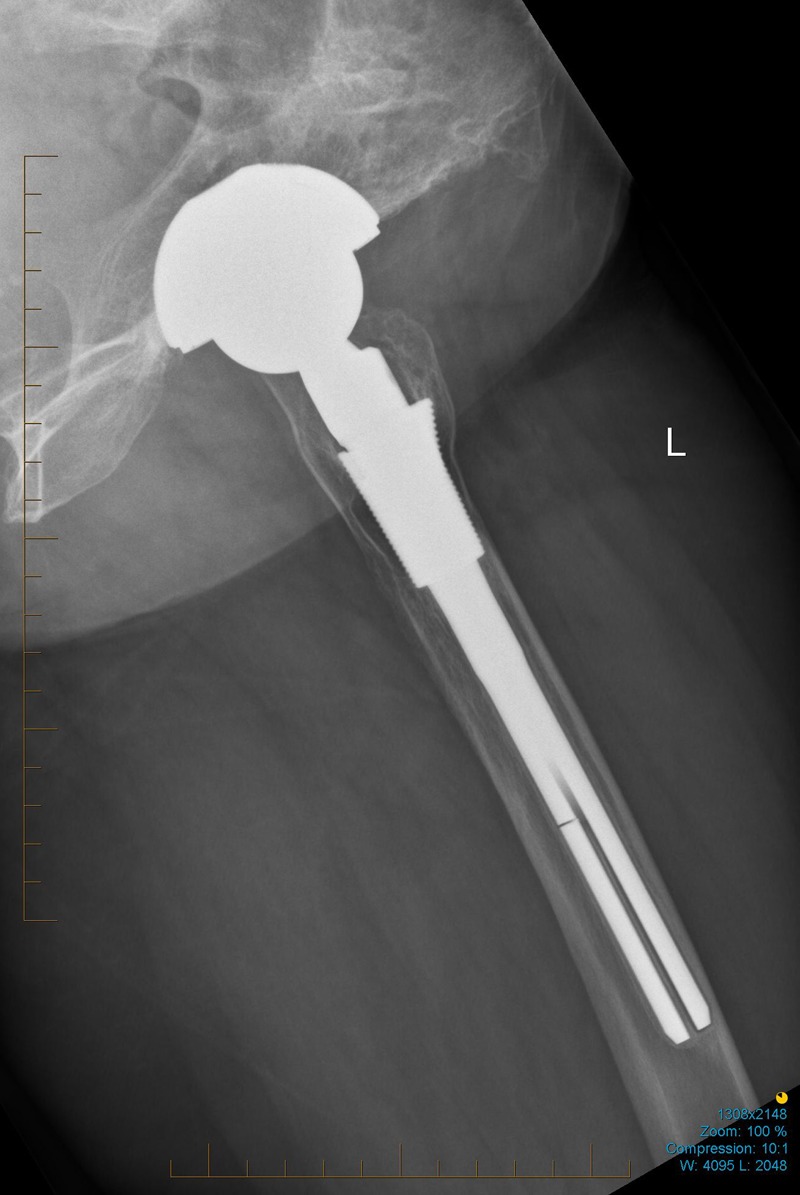
Case 2: Lateral radiograph of the left hip.
Treatment
Both patients were managed conservatively with analgesics and protective weight bearing using a walking stick.
Outcome and follow-up
The pain gradually resolved and disappeared 8 weeks after onset in both patients. The most recent clinical review several months after presentation did not reveal any abnormality and both the patients remain asymptomatic.
Discussion
The Specialist Orthopaedic Group has implanted 1722 S-ROM prosthesis since 1987 by three surgeons with excellent results8 9 predominantly in complex primary and revision cases. Two spontaneous stem fractures implanted by different surgeons within 5 years of implantation were therefore a cause for concern. A literature search did not reveal any other reports of spontaneous stem fracture. In both our cases, the problem has been managed conservatively, although it clearly had a clinical impact on the patient in the form of weeks of pain. The mechanism of failure is likely to be a fatigue fracture, and we have calculated approximate figures for torsional and bending stresses of each particular implant accounting for each patient's weight and the location of the fracture. The shear stress was found to be above the ultimate shear for Ti6Al4V ELI. The fatigue stress in each patient was also found to be several times the materials limit. The calculations make several assumptions including the fulcrum being a single point and there being no proximal support, so are intended as being illustrative only. This may reopen the debate on the efficacy of the coronal slot in the design of the stem. Part of the design rationale cites Cameron's paper5 after stating that the slotted design has been shown to reduce thigh pain. Cameron stated that this objective appears to have been achieved when commenting on the split reducing the bending stiffness and the hope that this would reduce the incidence of thigh pain. However, this was based on a cohort of five solid implants only. Gillies et al10 performed biomechanical tests on cadaveric implants showing that the addition of slots did not alter the cortical strain distribution. Musgrave et al11 comments that the decreased modulus mismatch or enhanced torsional stability achieved by the coronal slot has not been proven to be causally related to thigh pain. His study showed that slotted stems resulted in decreased sagittal plane femoral bending in the unloaded state, not the loaded state. Therefore, the relationship between decreased postimplantation sagittal plane femoral bending with slotted stems and the occurrence of thigh pain could not be determined from this study either.
We also explored some of the similarities relating to this case. Both femoral stems were exactly of the same size and were implanted within a month of each other. The implant stickers were retrieved and found to have different lot numbers. This was double checked with the manufacturers who confirmed that they were from different batches. Our aim in publication is to ensure that this is an isolated problem and not an under-reported phenomenon.
Learning points.
The S-ROM prosthesis is widely used with excellent long-term follow-up and few complications.
Prosthetic fracture causing thigh pain can happen spontaneously without trauma.
Prosthetic fracture does not always cause periprosthetic fracture of the femur.
Prosthetic fracture can be treated conservatively with success.
Prosthetic complications should be reported in peer-reviewed literature to help identify any trends in failure rate.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Le D, Smith K, Tanzer D, et al. Modular femoral sleeve and stem implant provides long-term total hip survivorship. Clin Orthop Relat Res 2011;469:508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adamany DC, Politi JR, Hauser WH. S-ROM hip prosthesis: 10- to 14-year results. Orthopedics 2008;31:220. [DOI] [PubMed] [Google Scholar]
- 3.Christie MJ, DeBoer DK, Trick LW, et al. Primary total hip arthroplasty with use of the modular S-ROM prosthesis. Four to seven-year clinical and radiographic results. J Bone Joint Surg Am 1999;81:1707–16 [DOI] [PubMed] [Google Scholar]
- 4.Skinner HB, Curlin FJ. Decreased pain with lower flexural rigidity of uncemented femoral prostheses. Orthopedics 1990;13:1222. [DOI] [PubMed] [Google Scholar]
- 5.Cameron HU. The 3- to 6-year results of a modular noncemented low-bending stiffness hip implant: a preliminary study. J Arthroplasty 1993;8:239. [DOI] [PubMed] [Google Scholar]
- 6.Ohl DO, Whiteside LA, McCarthy DS, et al. Torsional fixation of a modular femoral hip component. Clin Orthop Relat Res 1993;287:135. [PubMed] [Google Scholar]
- 7.Whiteside LA, Arima J, White SE, et al. Fixation of the modular total hip femoral component in cementless total hip arthroplasty. Clin Orthop Relat Res 1994;298:184. [PubMed] [Google Scholar]
- 8.Lusty PJ, Walter WL, Walter WK, et al. Cementless hip arthroplasty in Paget's disease at medium-term follow-up (average of 6.7 years). J Arthroplasty 2007;22:692–6 [DOI] [PubMed] [Google Scholar]
- 9.Murphy PG, Walter W, Zicat B. Cementless hip arthroplsty in the dysplastic hip. J Bone Joint Surg Br 2002;84-B:(Suppl III):252 [Google Scholar]
- 10.Gillies RM, Morberg PH, Bruce WJM, et al. The influence of design parameters on cortical strain distribution of a cementless titanium femoral stem. Med Eng Phys 2002;24:109–114 [DOI] [PubMed] [Google Scholar]
- 11.Musgrave DS, Glisson RR, Graham RD, et al. Effects of coronally slotted femoral prostheses on cortical bone strain. J Arthroplasty 1997;12:657–69 [DOI] [PubMed] [Google Scholar]


