Abstract
We report a case of cavernous sinus thrombosis in a 55-year-old Chinese man who presented with headache, ophthalmoplegia and ptosis. Campylobacter rectus was eventually isolated from the blood cultures. He was treated with broad-spectrum antibiotics, anticoagulation and steroids with improvement in his condition. To our knowledge, this is the first documented case of septic cavernous sinus thrombosis caused by C. rectus.
Background
Cavernous sinus thrombosis is a rare but serious disease associated with significant morbidity and mortality. The diagnosis is based on clinical findings and is confirmed by imaging. Common pathogens reported are Staphylococcus aureus and β-haemolytic Streptococcus. Early diagnosis and prompt treatment is crucial to improve outcomes in this potentially fatal disease.
Case presentation
A 55-year-old Chinese male tourist with no medical history presented with headache for 8 days. One day prior to admission, he developed fever, double vision and complete ptosis of his left eye. The patient did not have ocular discharge, sinus tenderness, sore throat and neck pain. The patient did not have toothache but had an uncomplicated left upper molar tooth extraction for dental caries 3 months previously. At the emergency department, he was noted to be febrile at 38.2°C, but non-toxic and haemodynamically stable. Physical examination was remarkable for left eye ptosis, proptosis and chemosis with a fixed dilated left pupil. A careful neurological examination revealed left third, fourth and sixth nerve palsies with loss of sensation over the left forehead.
Investigations
Laboratory results on admission showed a haemoglobin level of 14 g/dL, white cell count (WCC) 14 600 (normal reference range 3.6–11.1/mm3), bands 6%, thrombocytopaenia 63 000 and a low sodium level 127. On peripheral smear, there were no schistocytes or clumped platelets. Prothrombin time and partial thromboplastin time were normal and the C reactive protein was elevated at 251. Lumbar puncture was performed and the cerebrospinal fluid (CSF) analysis revealed pleocytosis (36 WCC/mm3) with a neutrophil predominance of 58%, normal glucose level 78 mg/dL, elevated protein level 75 mg/dL and negative Gram stain.
Initial MRI of the brain showed fullness of the left cavernous sinus (figure 1) and dilated left superior ophthalmic vein (figure 2) consistent with cavernous sinus thrombosis. Within hours of admission, the patient developed new proptosis, ophthalmoplegia and marked chemosis of his right eye. Bilateral carotid artery angiogram excluded a carotid-cavernous fistula. CT angiogram of the neck showed right internal jugular vein thrombosis extending into the right sigmoid sinus, while CT of the chest revealed solid and cavitary pulmonary nodules consistent with septic pulmonary emboli. A brain MRI performed 2 days later showed progression of thrombosis to the contralateral cavernous sinus and thrombosis of left superior ophthalmic vein (figure 3). There was interval development of left posterior genu cavernous internal carotid arterial pseudoaneurysm (figure 4). MR venogram was remarkable for lack of flow in the right transverse, sigmoid sinuses and visualised internal jugular vein (figure 5). Blood cultures eventually grew Campylobacter rectus identified by 16S ribosomal RNA (16S rRNA) sequencing while CSF cultures were sterile.
Figure 1.
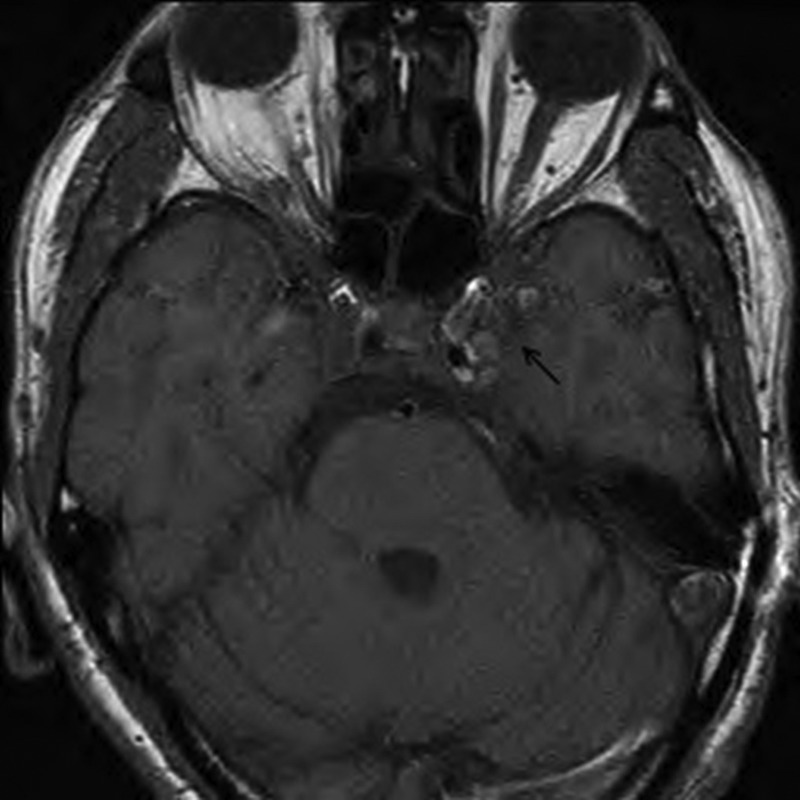
Axial MRI (T1) of cavernous sinus showing fullness of left cavernous sinus.
Figure 2.
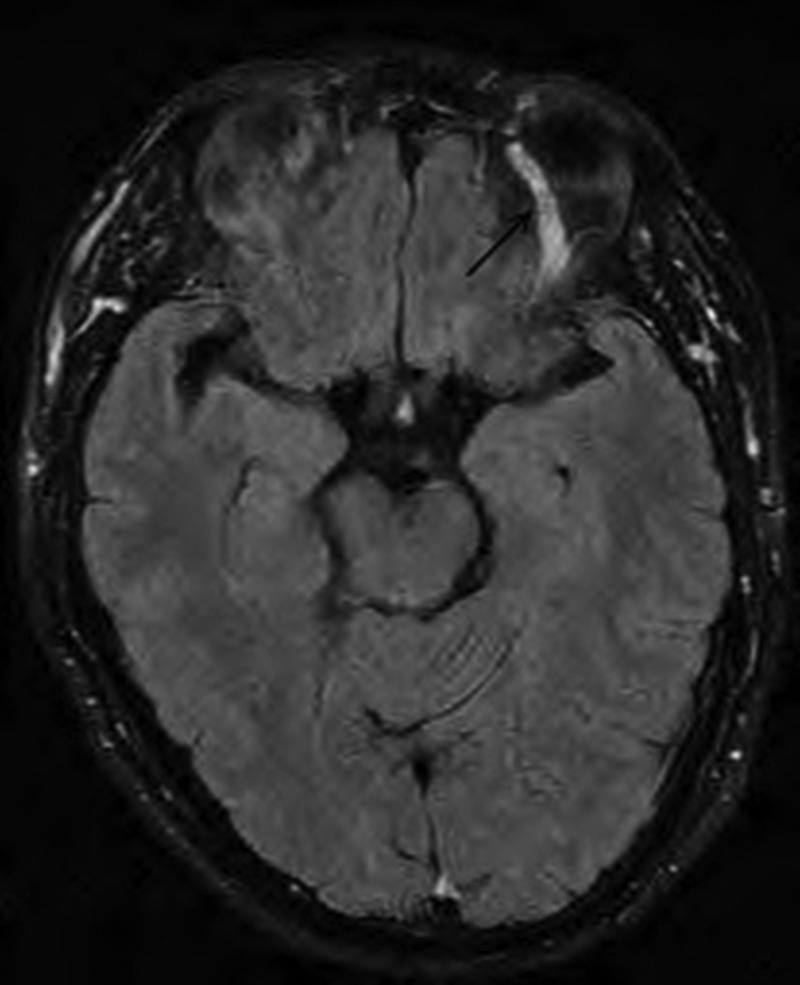
Axial MRI (Flair) of orbits showing dilated left superior ophthalmic vein.
Figure 3.
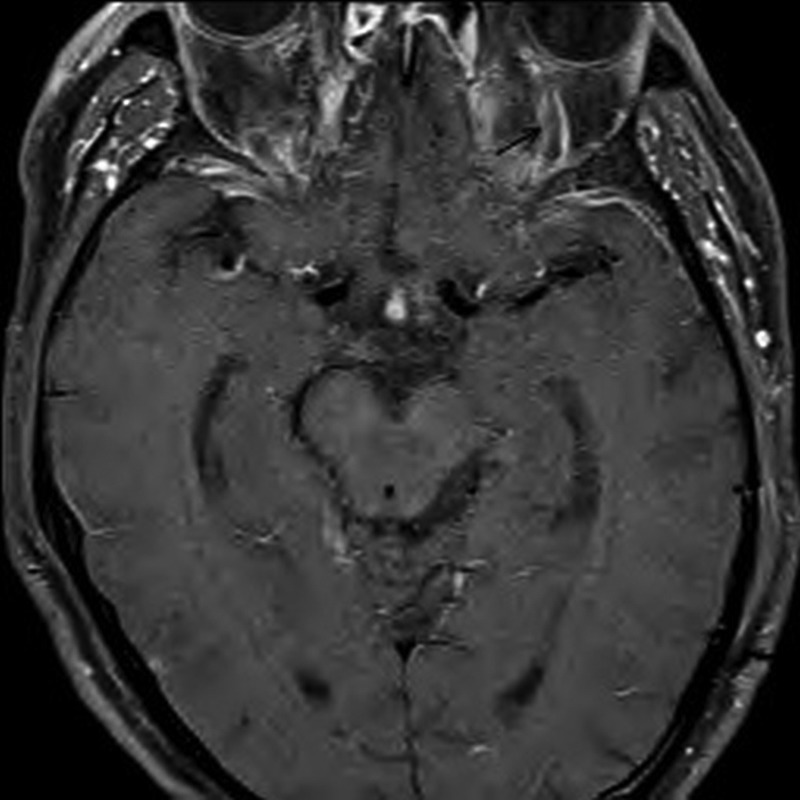
Contrast-enhanced MRI (T1) of orbits showing abnormal filling defect of left superior ophthalmic vein indicating thrombosed left superior ophthalmic vein.
Figure 4.
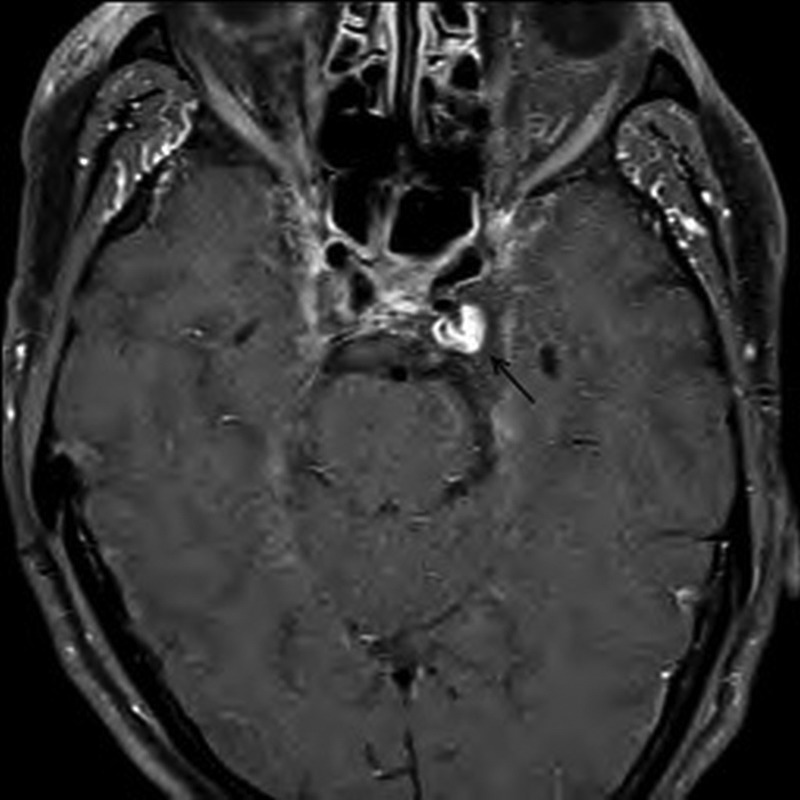
Contrast-enhanced MRI (T1) of cavernous sinus showing left posterior genu cavernous internal carotid arterial pseudoaneurysm.
Figure 5.
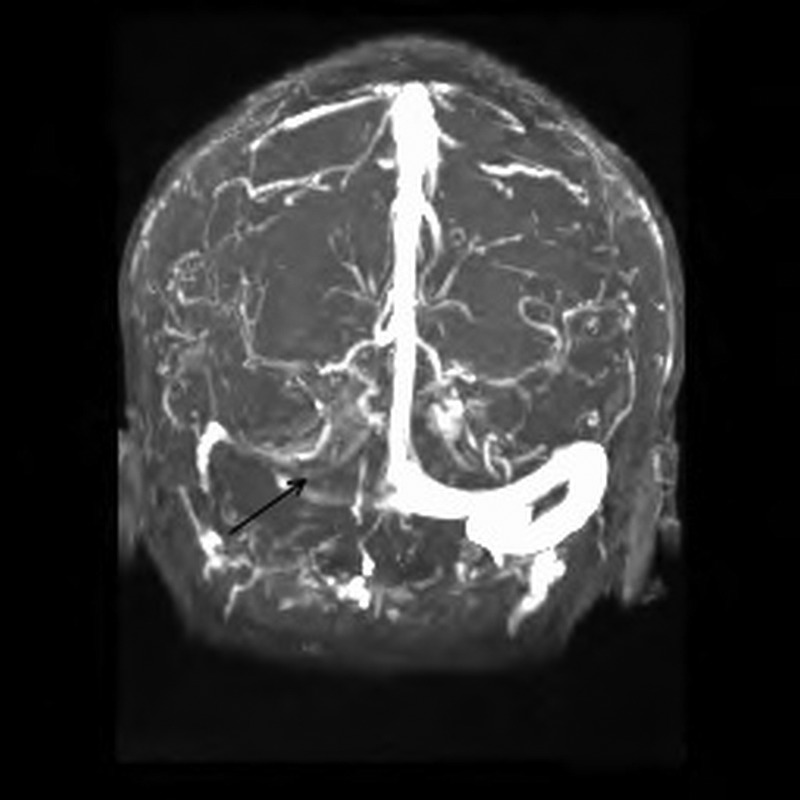
MR venogram showing decreased flow in the right transverse sinus and right sigmoid sinus.
Differential diagnosis
Differential diagnosis of septic cavernous sinus thrombosis include aseptic thrombosis resulting from trauma, superior orbital fissure syndrome, orbital cellulitis, aneurysm of the internal carotid artery, carotid-cavernous fistula or Tolosa-Hunt syndrome.
Treatment
The patient was treated with vancomycin, clindamycin and piperacillin/tazobactam for septic cavernous thrombosis together with anticoagulation and steroids. With the development of pseudoaneurysm, a neurointerventionalist was consulted. He recommended against coil embolisation due to high risk of seeding infection and coil decompaction within the cavernous clot as it progressed to recanalise. The patient was informed about the risk of direct carotid-cavernous fistula formation. In the event of a fistula formation, treatment might require additional embolisation.
Outcome and follow-up
The patient's fever and leucocytosis resolved with treatment. His proptosis and chemosis also resolved and visual acuity of his right eye returned back to normal. However, despite treatment his cranial nerve palsies persisted, necessitating a left eye patch to prevent diplopia. After hospitalisation for 10 days, the patient was deemed stable for discharge from our hospital to continue medical care back in his home country. His antibiotics were switched to intravenous ertapenem to facilitate administration during his flight back home.
Discussion
Septic thrombosis of the cavernous sinus is a potentially lethal illness with mortality rates reported between 20% and 30%.1 Sinusitis, especially involving the sphenoid and ethmoid sinuses, is the most common cause of cavernous sinus thrombosis while other locoregional infections involving dental aetiology are less common.2
Patients with cavernous sinus thrombosis present with headache, fever, vomiting, facial redness and pain, and eyelid oedema. The most frequent signs are fever, proptosis, chemosis (due to obstruction of the ophthalmic veins) and cranial nerve palsies (III, IV, V1, VI), leading to ptosis, ophthalmoplegia and supraorbital paraesthesia.1 Within 24–48 h, spread of the clot through the circular sinus to the contralateral cavernous sinus may result in bilateral signs and symptoms.3
Diagnosis of cavernous sinus thrombosis is confirmed by imaging, contrasted CT scan or MRI. Radiographic signs include enlargement of cavernous sinus (figure 1), abnormal irregular filling defects and dilation (figure 2) or thrombosis (figure 3) of the superior ophthalmic vein.
The two predominant pathogens in reported cases of cavernous sinus thrombosis are S. aureus (50–60%) and β-haemolytic Streptococcus (20%), followed by Streptococcus pneumoniae, Haemophilus influenzae and Bacteroides.3 Blood cultures are positive in approximately 70% of cases while CSF cultures are positive in nearly 20% of cases.1
C. rectus is a small, unbranched, anaerobic, Gram-negative rod. It is a member of the human oral flora that is associated with human periodontal disease.4 C. rectus is a difficult organism to identify and culture4 and in our case, was identified only by 16S rRNA gene sequencing.
Very few cases of invasive C. rectus infections have been reported in the literature. To our knowledge, this is the first reported case of septic cavernous sinus thrombosis caused by C. rectus. We hypothesised that the patient's infection likely started from the left upper molar removal causing bacteraemia and resulting in left cavernous sinus and right internal jugular vein thromboses with septic pulmonary emboli. Complications of cavernous sinus thrombosis include meningitis, encephalitis, brain abscess, pituitary infection, and epidural and subdural empyema.
Management of cavernous sinus thrombosis should include the treatment of primary infection. Empirical therapy should include vancomycin to cover for methicillin-resistant S. aureus, third-generation or fourth-generation cephalosporin and metronidazole or clindamycin, especially if dental infection is suspected. The duration of antibiotic therapy is at least 3–4 weeks.1
The role of anticoagulation is controversial because of possible bleeding complications and extension of the infectious thrombophlebitis. One retrospective study reported a decrease in mortality in patients with unilateral cavernous sinus thrombosis who received heparin early5 while another study demonstrated no statistically significant decrease in mortality when anticoagulation was used in combination with antibiotic therapy but noted a decrease in morbidity (blindness, stroke, ophthalmoplegia, hypopituitarism and seizures).6 Duration of anticoagulation is unknown but 4–6 weeks have been suggested.6
The use of steroids in the treatment of cavernous sinus thrombosis is controversial too and there is insufficient evidence to support its routine use. There are case reports that corticosteroids use may reduce inflammation and subsequently cranial nerve dysfunction and orbital congestion.2
In summary, we have described a case of cavernous sinus thrombosis caused by C. rectus. An odontogenic source of infection should always be considered in patients with cavernous sinus thrombosis.
Learning points.
Early recognition and appropriate treatment of cavernous sinus thrombosis is crucial to improve mortality and morbidity of this potentially fatal disease.
Dental infections may result in serious complications and an odontogenic source of infection should always be considered in patients with septic cavernous sinus thrombosis.
Campylobacter rectus is an oral anaerobe that is capable of causing human diseases such as cavernous sinus thrombosis.
Antibiotics remain the cornerstone of treatment for cavernous sinus thrombosis. Anticoagulation and steroids use may be helpful.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ebright JR, Pace MT, Niazi AF. Septic thrombosis of the cavernous sinuses. Arch Intern Med 2001;161:2671–6 [DOI] [PubMed] [Google Scholar]
- 2.Desa V, Green R. Cavernous sinus thrombosis: current therapy. J Oral Maxillofac Surg 2012;70:2085–91 [DOI] [PubMed] [Google Scholar]
- 3.Lazow SK, Izzo SR, Vazquez D. Do dental infections really cause central nervous system infections? Oral Maxillofac Surg Clin North Am 2011;23:569–78, vii [DOI] [PubMed] [Google Scholar]
- 4.Mahlen SD, Clarridge JE., III Oral abscess caused by Campylobacter rectus: case report and literature review. J Clin Microbiol 2009;47:848–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Southwick FS, Richardson EP, Jr., Swartz MN. Septic thrombosis of the dural venous sinuses. Medicine (Baltimore) 1986;65:82–106 [DOI] [PubMed] [Google Scholar]
- 6.Levine SR, Twyman RE, Gilman S. The role of anticoagulation in cavernous sinus thrombosis. Neurology 1988;38:517–22 [DOI] [PubMed] [Google Scholar]


