Abstract
We report a case of a 11-year-old boy who presented with a massive soft tissue right cervical painless and progressive lesion displacing trachea to the left and extending into the anteriosuperior mediastinum which was diagnosed to be a lipomatous mass on chest CT scan. Subsequent biopsy and total excision proved it to be a giant cervicomediastinal thymolipoma. It was successfully excised with excellent prognosis and long-term results. A giant paediatric cervicomediastinal thymolipoma is a rare, benign, mediastinal mass of thymic origin. It may remain asymptomatic despite massive size and up to 50% in some series are associated with autoimmune disease. CT scan gives fat density and encapsulated benign nature and biopsy usually establishes the diagnosis. Preoperative tissue diagnosis is important as now the availability of thoracoscopic option is best suited to reduce morbidity. Treatment of choice is total excision using open surgical, minimal invasive techniques or robotic surgery and the prognosis is excellent.
Background
Athymolipoma as the name suggests is a rare benign tumour of the thymus gland in the anterior mediastinum containing mature thymic and adipose tissue together. Lange reported it for the first time in 1916 and the term thymolipoma was first coined by Hall in 1948.They are less common than a mediastinal lipoma, form about 6% of all thymic tumours and mean age of presentation is 22 years and the range is 3–56 years. We wish to report a giant mediastinal thymolipoma extending into the right cervical region of a young boy.
Case presentation
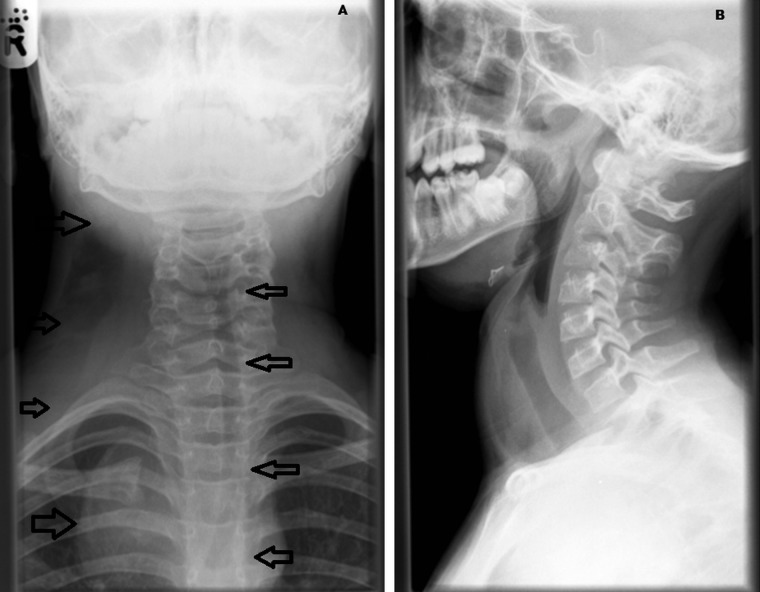
An 11-year-old boy presented with a painless progressively growing right cervical mass disappearing into the right upper chest of 3 months duration. Examination revealed a massive, lobulated, smooth, non-tender, non-transilluminant soft tissue mass extending from behind the right neck and disappearing under the sternum and right chest (figures 1 and 2).
Figure 1.
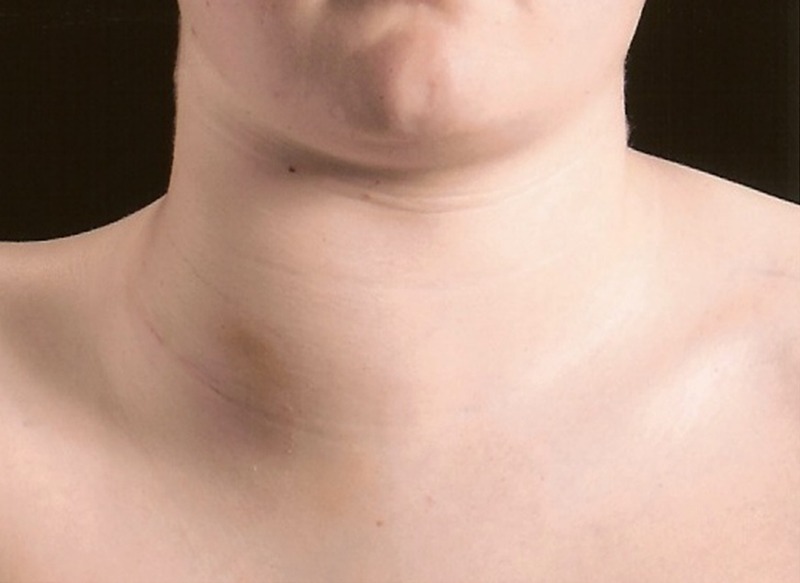
Front view of the neck and upper chest showing the site and size of the tumour.
Figure 2.

Lateral view of the right neck showing posterior extent of the tumour till midline.
Investigations
Complete blood count showed haemoglobin 93 g/L, leucocytes 6.58×109/L, neutrophils 3.85×109/L, platelets 218 × 109/L. Coagulation screen showed prothrombin time 14.9 s, activated partial thromboplastin time 32 s, thrombin clotting time 13.5 s and fibrinogen 1.6 g/L Glandular fever screen and blood culture were negative. Renal functions including urate levels were within normal limits. C reactive protein was <1 mg/L. Bone profile was normal except serum calcium being 2.14 mol/L and magnesium 0.63 mmol/L. Liver functions including all enzymes were within normal limit apart from total protein 52 g/L and albumin 29 g/L.
Anteroposterior and lateral neck radiographs showed deviation of trachea and mediastinal structures away to the left and a soft tissue mass on the right cervical region projected anterior to the trachea but does not appear to compromise calibre of the trachea (figure 3A, B). Chest radiograph showed large right cervical soft tissue shadow with well-defined lateral border and its extension into the right paratracheal area in the anterior mediastinum (figure 4). The slight lucent quality of the mass on plain films raised the suspicion of mass being of fatty density and a CT scan was recommended.
Figure 3.
Anteroposterior and lateral cervical radiograph—note lateral displacement of trachea to the left by right sided mass but there is no anteroposterior compression on the lateral view.
Figure 4.
Chest radiograph showing mediastinal extension of the soft tissue tumour.
He underwent CT of the neck (3.75 mm sections) and torso (5 mm sections). The CT scan revealed a giant mass with fat density involving the right cervical region deviating right upper pharynx and trachea just off the midline to the left. It was displacing large neck vessels anteriorly and medially. There was no invasion of any muscles. On its posterolateral aspect, there were two nodules joined by a strand of soft tissue density structures—larger measuring 12 mm and the smaller one 5.5 mm. Mass was lying immediately deep to the sternomastoid muscle bounded medially by the paravertebral muscle and no invasion to spinal canal. It extended around the whole of the supraclaviclular area and the anterior portion of the mass was continuous down into the anterior and then middle mediastinum accounting for the right para-tracheovertebral mass on the chest radiograph. It extended posteriorly into the neck involving the anterior mediastinum predominantly on the right side with some extension into the pericardiac and aortic region anteriorly without any lymphadenopathy or abnormal fat.
A need for tissue biopsy was considered in the multidisciplinary meeting. He underwent biopsy through a small cervical incision initially which confirmed the diagnosis of mature thymolipoma and a combined paediatric surgical and cardiothoracic surgical team approach was organised.
Differential diagnosis
A variety of neoplastic lesions including lymphoma, lipoma, lipomatosis, lipoblastoma, lipoblastomatosis and thymolipoma were initially considered and the therapeutic implications in each of these groups being different, it was thought prudent to get the tissue diagnosis first so that the accurate treatment can then be performed with excellent prognosis.
Treatment
Subsequently he underwent exploration via trapdoor right cervical incision encircling the previous biopsy scar in the right supraclaviclular region and extending into the anterior mediastinum via midline sternotomy allowing extensive exposure and safe surgery. Total surgical excision of the giant thymolipomatous mass was achieved without any complications (figure 5).
Figure 5.
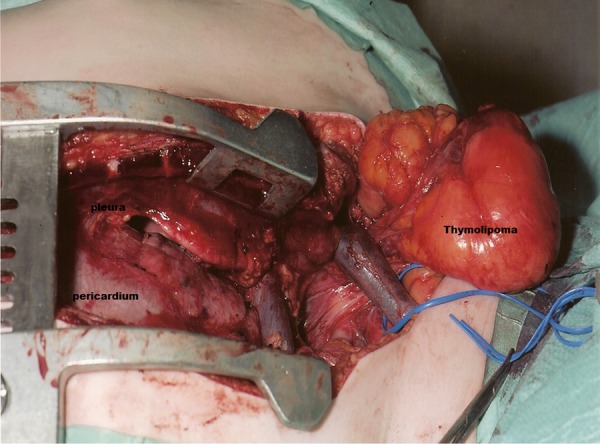
Intraoperative photograph showing the nature and extent of the tumour via right cervical-sternal trapdoor incision.
Outcome and follow-up
The patient recovered uneventfully. Gross specimen showed an encapsulated homogenous fatty mass weighing 1.8 kg and measuring 170×90 × 30 mm in size. Few areas of focal fibrosis were seen but there was no haemorrhage, necrosis or degeneration. Histopathological examination demonstrated lobules of mature adipose tissue interspersed with islands of mature thymic tissue and prominent Hassall's corpuscle confirming benign mature thymolipoma (figure 6).
Figure 6.
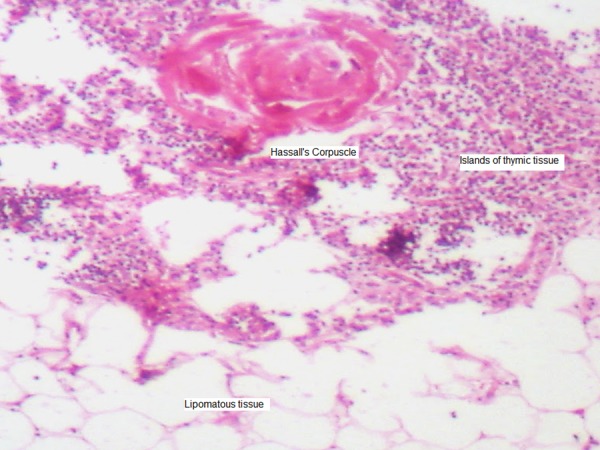
Photomicrograph showing islands of thymic tissue within a background of lipoma—note prominent Hassall's corpuscle in the top central area.
Discussion
Giant paediatric cervicomediastinal thymolipoma are very rare benign and exceptional tumour in children.1 Although it is rare, it should be considered in the differential diagnosis of a mass extending into the anterior mediastinum. It can take alarming proportions and can have expansive growth along the natural tissue planes and may present as cervical mass clinically as happened in our case which simulated a neck tumour rather than a mediastinal one.
The tumour is made up of mature adipose and thymic tissue and may remain asymptomatic till they attain giant proportions; and is found incidentally often during imaging for respiratory tract infection.2–4 Our case is a strong reminder of the fact that if we cannot go below the neck swelling, an extension into the chest and mediastinum should be suspected even in the absence of any symptoms.
Some of them present with mediastinal structure compression symptoms and rest may present with non-specific symptoms of cough, dyspnoea and chest pain. Some of them may be detected incidentally if they are purely thoracic. Our case had a gigantic proportion but was asymptomatic apart from the giant swelling.
It is therefore recommended that initial radiological assessment should include neck and chest radiographs. On plain film they appear like a large soft tissue mass in the neck and anterior mediastinum. Ultrasound may show lobulated soft tissue mass and colour Doppler may not show evidence of any hypervascularity of a malignant mass. CT scan shows fat density lesion and on MRI fat shows high T1 signal and thymic component—a more intermediate T1 signal. Our patient had some suspicious nodules and therefore a decision was taken to perform a biopsy to confirm the diagnosis and rule out liposarcoma or other malignant lesions and plan the treatment appropriately.
Although it is massive and extends into surrounding structures, total excision with preservation of vessels, nerves and vital structures is feasible through well-developed tissue planes. A minimally invasive option is now available and whenever possible thoracoscopic excision should be attempted provided an experienced team and appropriate equipment support is available. It is safe, effective, less painful, cosmetic and allows early discharge of the patient.
Recently, thoracoscopic excision in such cases has been successfully carried out and is feasible and safe with excellent cosmesis, less pain and early discharge from the hospital.5 A giant thymolipoma inan infant presenting with respiratory distress has been reported with successful surgical excision.6 The prognosis is excellent without any recurrence, metastasis or mortality.
Learning points.
A giant paediatric cervicomediastinal thymolipoma is a rare, benign, anterior mediastinal mass of thymic origin.
It may remain asymptomatic despite massive size and up to 50% in some series are associated with autoimmune disease.
CT scan gives fat density and encapsulated benign nature and biopsy usually establishes the diagnosis.
Preoperative tissue diagnosis is important as now availability of thoracoscopic option is best suited to reduce morbidity.
Treatment of choice is total excision using open surgical, minimally invasive techniques or robotic surgery; and the prognosis is excellent.
Acknowledgments
The authors are grateful to the paediatric oncology, anaesthetic, cardiothoracic and paediatric intensive care teams at the University Hospital of Wales, Cardiff for their help in the clinical management of this patient.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hudson H, Cohen DM, Cribbs R, et al. Massive thymolipoma involving both chest cavities. Pediatr Surg Int 1994;10:546–8 [Google Scholar]
- 2.Ganesh Y, Yadala V, Nalini Y, et al. Huge mediastinal mass with minimal symptoms: thymolipoma. BMJ Case Rep 2011;2011:bcr0520102984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steger C, Steiner HJ, Moser K, et al. A typical thymic carcinoid tumour within a thymolipoma: report of a case and review of combined tumours of the thymus. BMJ Case Rep 2010;2010:pii:bcr0420102958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gamanagatti S, Sharma R, Hatimota P, et al. Giant thymolipoma. AJR Am J Roentgenol 2005;85:283–4 [DOI] [PubMed] [Google Scholar]
- 5.Tan TW, Kim DS, Wallach MT, et al. Thoracoscopic resection of a giant thymolipoma in a 4-year-old girl. J Laparoendosc Adv Surg 2008;18:903–5 [DOI] [PubMed] [Google Scholar]
- 6.Parakh A, Singh V, Subramaniam R, et al. Giant thymolipoma in an infant. Paediatr Int Child Health. Published Online First: 6 Dec 2013. doi:10.1179/2046905513Y.0000000108 [DOI] [PubMed] [Google Scholar]