Abstract
Marchiafava-Bignami disease (MBD) is a form of toxic demyelinating disease more often seen in chronic alcoholics. The disease process typically involves the corpus callosum and clinically often presents with altered sensorium, neurocognitive defects or seizures with acute cases often deteriorating to comatose state. The death rate is high. We report a rare case of MBD with complete clinical recovery. A 50-year-old male patient presented in an unconscious state and underwent MRI of the brain which showed significant lesions involving the corpus callosum. Following treatment with thiamine and supportive therapy, he improved clinically and a follow-up MRI revealed significant resolution of the earlier lesions. Diffusion-weighted MRI showed the changes more conspicuously as compared with conventional imaging. The clinical resolution corresponded well with the MRI pattern. The case highlights that diffusion-weighted MRI is an extremely useful tool in evaluation and prognostication of MBD.
Case presentation
A 50-year-old chronic alcoholic living in isolation presented in an unconscious state to the emergency department. The patient was not a known diabetic or hypertensive, and there was no other significant medical history. On examination, the patient was non-comprehensive and the Glasgow Coma Scale score of the patient was 11/15 with poor word output and localisation to painful stimulus. Laboratory analysis of the patient revealed random blood glucose levels of 95 mg/dL, sodium 107 mmol/L and potassium 4.9 mmol/L. The renal function tests, liver function and other laboratory tests were within normal limits.
Investigations
CT of the brain which was performed outside the hospital showed subtle hypodensity in the corpus callosum. MRI of the brain showed bilateral subdural hygroma, swollen splenium and posterior body of the corpus callosum with hyperintense signal on FLAIR (fluid attenuation inversion recovery) and T2 images (figure 1A, B), with diffusion restriction noted as hyperintensity and corresponding hypointensity on ADC (apparent diffusion coefficient) images in the involved region (figure 1C, D). There was minimal cortical white matter involvement in the left parietal lobe which showed subtle hyperintensity on FLAIR with diffusion restriction (figure 1E, F).
Figure 1.
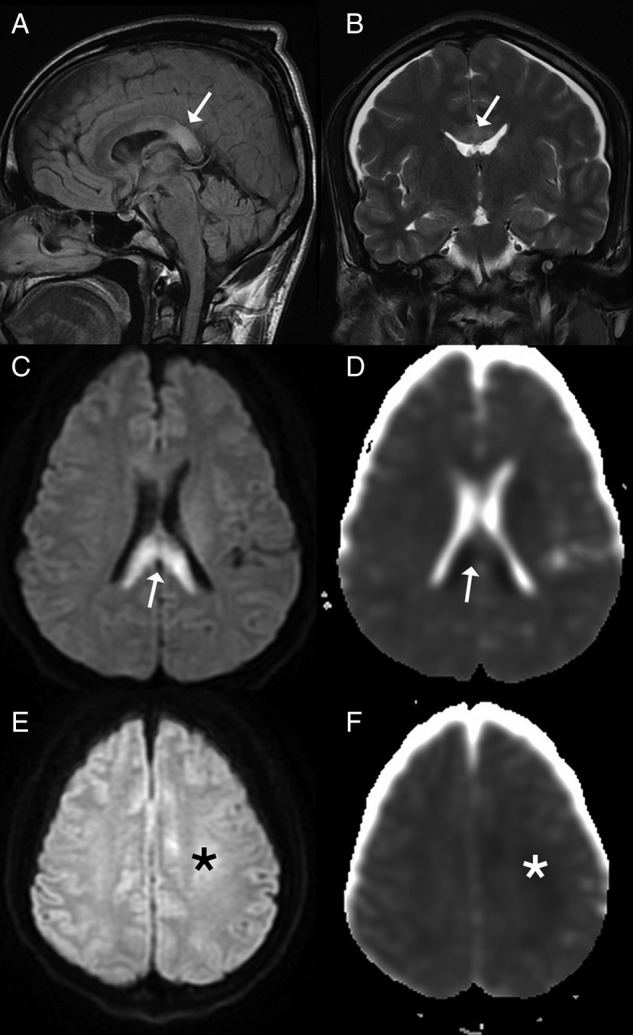
(A, B) Sagittal fluid attenuation inversion recovery (FLAIR) and coronal T2 images show hyperintensity in the splenium of the corpus callosum (arrow) with associated chronic subdural hygromas along the cerebral convexities. (C, D) Diffusion-weighted images show hyperintensity involving the splenium of the corpus callosum (arrow) with corresponding hypointensity on apparent diffusion coefficient (ADC) images. (E, F) Diffusion-weighted images show subtle hyperintensity in the left parietal subcortical white matter (*) with corresponding changes on ADC images.
A follow-up MRI following complete clinical recovery revealed a decrease in size of the primary area of involvement with no significant diffusion restriction (figure 2A–C). Hyperintense signal on diffusion-weighted images was due to T2 shine through as the ADC images were normal. A final diagnosis of Marchiafava-Bignami (MB) disease was considered on the basis of clinical course and MRI findings.
Figure 2.
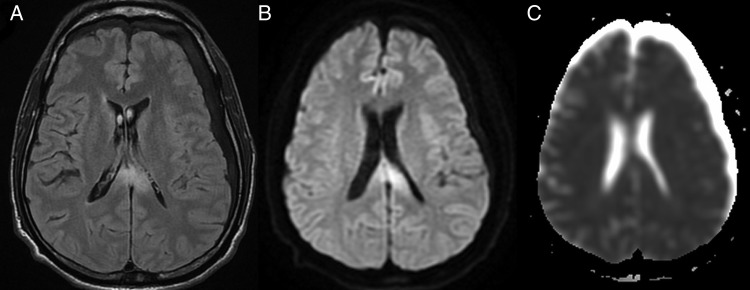
(A, B) Follow-up MRI fluid attenuation inversion recovery (FLAIR) and diffusion images revealed persistent hyperintensity in the splenium. (C) Apparent diffusion coefficient images do not reveal corresponding hypointensity suggestive of T2 shine through. As compared with the prior MRI, there is a significant decrease in the extent of involvement.
Differential diagnosis
Wernicke's encephalopathy, pontine and extrapontine myelinolysis and alcohol withdrawal syndrome with seizures are the differential diagnoses for MB disease in a chronic alcoholic. The overlapping features of Wernicke's encephalopathy can be differentiated by lack of involvement of the medial thalamic nuclei, hypothalamus, mamillary bodies and periaqueductal grey matter. Pontine and extrapontine myelinolysis can also be differentiated by the involvement of the central pons, basal ganglia, thalami, lateral geniculate body, cerebellum and cerebral cortex.
Alcohol withdrawal syndrome with seizures may reveal diffusion restriction secondary to cytotoxic oedema on MRI during the acute and subacute phases and significant volume loss in temporal regions.
Treatment
The patient was started on thiamine, and sodium supplementation was started in view of low sodium levels. Low sodium levels were attributed to SIADH (syndrome of inappropriate antidiuretic hormone secretion) and subsequently got corrected during the hospital stay.
Outcome and follow-up
Following thiamine and other supportive therapy, gradually over a period of 1 week, the patient started improving and was ambulant at the end of 10 days of treatment.
Discussion
MB disease is a rare disorder which typically causes degeneration of the corpus callosum which can range from demyelination to frank necrosis on pathological examination.1 2 Clinically, different conditions in alcoholics like Wernicke's encephalopathy, delirium tremens, osmotic demyelination or encephalitis may have very similar presentation and their features may overlap. Hence neuroimaging plays a significant role in accurate diagnosis of MB disease and helps in early intervention.3
Pathologically, MB disease is characterised by symmetrical demyelination and necrosis of the central part of the corpus callosum, with relative sparing of thin upper and lower edges. Necrosis subsequently leads to cavitation and atrophy of the corpus callosum in chronic stages.1 4 5
CT is not the preferred modality of neuroimaging and may be unable to pick up early lesions in cases of acute MB disease. MRI plays a crucial role in early diagnosis of the disease and accurately assesses the degree of brain involvement3 like in the present case. The classical MRI includes symmetric involvement of the corpus callosum with affection of the body of the corpus most commonly followed by the genu and finally the splenium. The other sites which have been described and can be involved include the cerebral peduncles, middle cerebellar peduncles, hemispheric white matter as well as internal capsules. Cortical involvement in acute MB disease is a poor prognostic indicator. During the acute phase, the involved regions become oedematous with or without demyelination and appear hypointense on T1-weighted image (T1WI) and hyperintense on T2WI and FLAIR. Diffusion-weighted imaging reveals hyperintensity in acute cases of callosal as well as cortical involvement with corresponding hypointensity and decreased values on ADC mapping. Diffusion restriction and low ADC values are associated with poor outcome, however do not predict irreversibility of the lesions.3 6 7
The differential diagnosis for MB disease includes Wernicke's encephalopathy, pontine and extrapontine myelinolysis and alcohol withdrawal syndrome.8–10 They are differentiated from MB disease as described in the differential diagnosis section.
There are certain conditions which can present as splenial hyperintensity on T2/FLAIR like epilepsy, antiepileptic drug withdrawal, multiple sclerosis, acute disseminated encephalomyelitis, infarction, viral and bacterial infections, especially influenza, HIV and hypoglycaemia, etc. These conditions can be differentiated on the basis of clinical and laboratory analyses.11
Learning points.
In a given clinical setting, whenever the corpus callosum is involved Marchiafava-Bignami disease should be kept as the first differential.
Early diagnosis is important as this entity is reversible if treated on time.
MRI is the imaging option and diffusion-weighted images in particular can be used as prognostic indicators as clinical recovery and neuroradiological changes correlate well.
Acknowledgments
The authors would like to acknowledge Dr Rajgopal KV and Dr VRK Rao for their support.
Footnotes
Contributors: KP edited and approved the article. CK and AP collected the details and written the article.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Bourekas EC, Varakis K, Bruns D, et al. Lesions of the corpus callosum: MR imaging and differential considerations in adults and children. AJR Am J Roentgenol 2002;179:251–7 [DOI] [PubMed] [Google Scholar]
- 2.Ellison D, Love S, Chimmeli L, et al. Neuropathology. A reference text of CNS pathology. 2nd edn Philadelphia: Mosby, 2004:489–90 [Google Scholar]
- 3.Tung CS, Wu SL, Tsou JC, et al. Marchiafava Bignami disease with widespread lesions and complete recovery. AJNR Am J Neuroradiol 2010;31:1506–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ruiz-Martinez J, Martinez Perez-Balsa A, Ruibal M, et al. Marchiafava-Bignami disease with widespread extracallosal lesions and favourable course. Neuroradiology 1999;41:40–3 [DOI] [PubMed] [Google Scholar]
- 5.Leong ASY. Marchiafava Bignami disease in a non-alcoholic Indian male. Pathology 1979;11:241–9 [DOI] [PubMed] [Google Scholar]
- 6.Méneégon P, Sibon I, Pachai C, et al. Marchiafava-Bignami disease: diffusion weighted MRI in corpus callosum and cortical lesions. Neurology 2005; 65:475–77 [DOI] [PubMed] [Google Scholar]
- 7.Oster J, Doherty C, Grant PE, et al. Diffusion-weighted imaging abnormalities in the splenium after seizures. Epilepsia 2003;44:852–4 [DOI] [PubMed] [Google Scholar]
- 8.Zuccoli G, Pipitone N. Neuroimaging findings in acute Wernicke's encephalopathy: review of the literature. AJR Am J Roentgenol 2009;192:501–8 [DOI] [PubMed] [Google Scholar]
- 9.Chua GC, Sitoh YY, Lim CC, et al. MR findings in osmotic myelinolysis. Clin Radiol 2002;57:800–6 [PubMed] [Google Scholar]
- 10.Sullivan EV, Marsh L, Mathalon DH, et al. Relationship between alcohol withdrawal seizures and temporal lobe white matter volume deficits. Alcohol Clin Exp Res 1996;20:348–54 [DOI] [PubMed] [Google Scholar]
- 11.Singh P, Gogoi D, Vyas S, et al. Transient splenial lesion: further experience with two cases. Indian J Radiol Imaging 2010;20:254–7 [DOI] [PMC free article] [PubMed] [Google Scholar]


