Abstract
A 54-year-old man presented to our emergency department with fever and dyspnoea. He required vigorous haemodynamic support and mechanical ventilation for hypotensive distributive shock with hypoalbuminaemia, haemoconcentration, rhabdomyolysis and acute renal failure, consistent with idiopathic systemic capillary leak syndrome. Left lung consolidation and hypoxaemia were observed 6 days after admission. Sputum smear revealed the presence of acute angled branching hyphae, consistent with a diagnosis of invasive pulmonary aspergillosis. Antifungal therapy was administered and mechanical ventilation discontinued on day 66. The patient recovered and was discharged from the hospital on day 185.
Background
Invasive pulmonary aspergillosis (IPA) usually occurs in the presence of typical manifestations of immunocompromised state, such as prolonged neutropenia or haematopoietic stem cell transplantation.1 It has rarely been described in critically ill patients presenting with severe sepsis or septic shock.2 3
Idiopathic systemic capillary leak syndrome (ISCLS) is a rare disorder characterised by episodes of profound hypotension, hypoalbuminaemia and haemoconcentration,4 due to leakage of plasma to the extravascular compartment.5 The clinical manifestations of ISCLS resemble septic shock, although immunological disorders, instead of microbial infections, are its main causes.5 The management of ISCLS is extrapolated from the treatment of distributive shock. Prophylactic therapy with terbutaline and theophylline has been reported to achieve durable success in the prevention of episodes of ISCLS, despite a lack of understanding of their mode of action.6 Serious complications, such as compartment syndrome, rhabdomyolysis and renal failure, have been reported,7 though little is known about opportunistic infections associated with ISCLS. We report a near-fatal case of ISCLS complicated by IPA.
Case presentation
A 54-year-old man (height, 172 cm; weight, 98 kg) presented to our emergency department, reporting fever, fatigue and increasing dyspnoea for a week. He had a history of cerebral infarction 7 years earlier, without sequelae and received no medication other than a regimen of levofloxacin, 500 mg/day, introduced a few days before his admission for the management of acute sinusitis.
On admission, the patient's BP was 103/87 mm Hg and the heart rate was 86 bpm. He was alert, his limbs were cool and without oedema, and the heart and lung auscultation was normal. A few minutes later, however, his systolic BP decreased precipitously to 50 mm Hg, and he lost consciousness. He was immediately intubated and placed on a mechanical ventilator.
Investigations
Measurements of arterial blood gases on 100% oxygen revealed a pH of 6.7, a PaO2 of 257 mm Hg, a PaCO2 of 69.2 mm Hg, a HCO3− of 8.3 mmol/L and a lactate concentration of 17 mmol/L. On further laboratory screen, the serum haemoglobin was 22.5 g/dL, haematocrit 72.2%, total leucocyte count 15 700/μL, platelet count 61 000/μL, total serum protein 3.6 g/dL (albumin: 52.8%, α1: 4.0%, α2: 20.2%, β: 9.6%, γ: 13.4%, albumin/globulin ratio: 1.1), albumin 1.8 g/dL, total bilirubin 0.4 mg/dL, aspartate aminotransferase 110 U/L, alanine aminotransferase 39 U/L, lactate dehydrogenase 527 U/L, creatine kinase (CPK) 7438 U/L, blood urea nitrogen 54 mg/dL, creatinine 2.65 mg/dL, sodium 127 mEq/L, potassium 4.1 mEq/L, C reactive protein 1.48 mg/dL, procalcitonin 0.97 ng/mL, immunoglobulin (Ig)G 459 mg/dL, IgA 146 mg/dL, IgM 64 mg/dL, complement (C)3 39 mg/dL, C4 13.9 mg/dL, CH50 14 mg/dL, free T3 0.9 pg/mL, free T4 1.0 ng/dL, thyroid stimulating hormone 0.18 μU/mL.
Transthoracic echocardiography showed normal motion of the heart chambers and a collapsed inferior vena cava.
Differential diagnosis
We suspected sepsis as the cause of this severe hypovolaemic/distributive shock with acute organ failure. However, neither a putative source of infection was found nor a causal microbial pathogen isolated (figure 1). Moreover, the procalcitonin level was not high enough to confirm the diagnosis of severe sepsis.8 In the absence of evidence of other cause of diffuse capillary leak, such as allergies, Addisonian crisis, drugs or toxin-induced reactions,9 10 we made a diagnosis of ISCLS.
Figure 1.
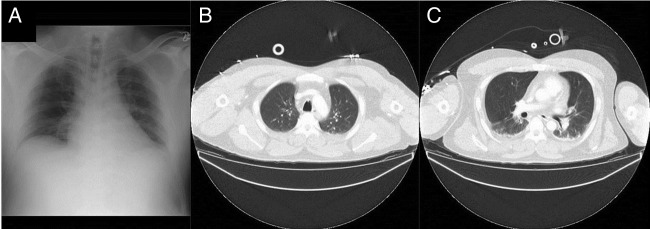
(A) Normal chest radiograph obtained on the day of admission. (B and C) Contrast-enhanced chest and abdominal CT on day 1; small subpleural opacities due to insufficient inspiration are present bilaterally.
Treatment
We empirically administered intravenous ampicillin/sulbactam, 12 g/day, and intravenous clindamycin, 2.4 g/day, for suspicion of infective necrotising fasciitis/myositis. The initial haemodynamic and pharmaceutical support also included crystalloids and albumin solutions, vasopressors, hydrocortisone, 300 mg/day and gammaglobulins, 7.5 g/day for 3 days. On day 2, we started continuous haemodiafiltration combined with plasma exchange, for the management of progressive acute renal failure with markedly elevated serum CPK concentrations, which peaked at 407 276 U/L on day 4, before decreasing gradually.
On day 6, a consolidation of the left upper lobe appeared on the chest radiograph, along with hypoxaemia (PaO2: 59.1 mm Hg, fraction of inspiratory oxygen: 0.3, positive end -expiratory pressure: 10 cm H2O). Aspergillus fumigatus was identified on microscopic examination and isolated in cultures of bronchoalveolar lavage fluid. The serum concentrations of galactomannan antigen was >5.0 ng/mL and β-d-glucan >300 pg/mL. Chest CT showed predominantly left nodular consolidations and bilateral bronchiolitis, consistent with IPA (figure 2).11 In the absence of neutropenia, history of HIV infection or immunosuppressive treatment, we strongly suspected IPA and administered intravenous voriconazole, 400 mg/day, followed by intravenous liposomal amphotericin B, 500 mg/day for 2 weeks, before discontinuing antifungal therapy in view of the patient's stable condition. However, bronchoscopy performed 3 weeks later revealed the presence of whitish caseous material occluding the left upper lobe bronchus, consistent with recurrent aspergilloma (figure 3). Antifungal therapy was thus reintroduced with intravenous micafungin, 150 mg/day, followed by voriconazole, 400 mg/day orally.
Figure 2.
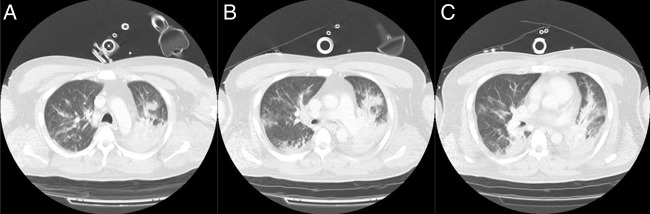
(A–C) Chest CT on day 7: bilateral nodular consolidations (predominant on the left) and centrilobular particulate opacities are present along the bronchi.
Figure 3.
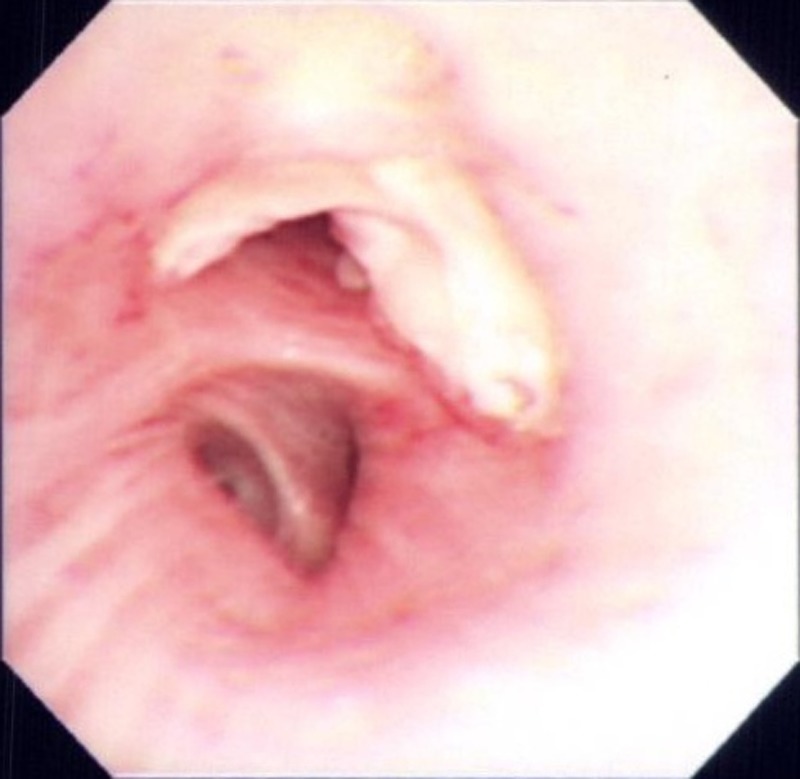
Bronchoscopy on day 52: the left upper lobe bronchus is filled with whitish caseous material.
Outcome and follow-up
On day 33, the serum IgG and complement concentrations had nearly returned to normal values. The patient's clinical status began to improve and the caseous material in the left upper lobe bronchus decreased after the introduction of micafungin. Haemodialysis was discontinued on day 59, mechanical ventilation on day 66 and antifungal therapy on day 181. He was discharged fully recovered from the hospital on day 185. Prophylactic terbutaline and theophylline were discontinued because of hypokalaemia. The patient has remained free from IPA and ISCLS over a follow-up of 3 months without any treatment.
Discussion
We observed a rare case of A. fumigatus pneumonia, which developed in the acute phase of ISCLS in the absence of other major pathology. We suspected that ISCLS was complicated by the development of an opportunistic infection. Although we did not collect confirmatory data, including human leucocyte antigen (HLA-DR) and pertinent cytokine profiles, we hypothesised that our patient was suffering from severe, transient immunoparalysis, due to exaggerated pro-inflammatory and anti-inflammatory responses.12 A monoclonal gammopathy has been observed in the majority of patients presenting with ISCLS.13 14 However, during the acute phase of the disease, the serum concentration of IgG and complements in our patient were low. Owing to vascular hyperpermeability, these proteins might leak through the endothelial barrier into the interstitium,5 compromising the immune system function.
The patient had also received hydrocortisone for suspected septic shock.15 16 Although it had been administered for only 3 days, it might have sufficed to weaken the cellular defence against A. fumigatus.17 Finally, because the pathophysiology of ISCLS remains uncertain, further studies are needed to exclude other causes of immunosuppression and immunodeficiency.
Learning points.
Invasive pulmonary aspergillosis can occur in critically ill patients in the absence of an immunocompromised status.
Inborn or acquired immunodeficiency in patients with idiopathic systemic capillary leak syndrome (ISCLS) may be complicated by opportunistic infections.
The immunosuppression associated with ISCLS is poorly understood and in need of further studies.
Acknowledgments
We are indebted to Dr Hideki Inoue and Dr Takahiro Kato for their assistance.
Footnotes
Contributors: NS and TM conceived this article, revised it critically for important intellectual content and approved the final version.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Segal BH. Aspergillosis. N Engl J Med 2009;360:1870–84 [DOI] [PubMed] [Google Scholar]
- 2.Meersseman W, Lagrou K, Maertens J, et al. Invasive aspergillosis in the intensive care unit. Clin Infect Dis 2007;45:205–16 [DOI] [PubMed] [Google Scholar]
- 3.Hartemink KJ, Paul MA, Spijkstra JJ, et al. Immunoparalysis as a cause for invasive aspergillosis? Intensive Care Med 2003;29:2068–71 [DOI] [PubMed] [Google Scholar]
- 4.Clarkson B, Thompson D, Horwith M, et al. Cyclical edema and shock due to increased capillary permeability. Am J Med 1960;29:193–216 [DOI] [PubMed] [Google Scholar]
- 5.Dhir V, Arya V, Malav IC, et al. Idiopathic systemic capillary leak syndrome (SCLS): case report and systematic review of cases reported in the last 16years. Intern Med 2007;46:899–904 [DOI] [PubMed] [Google Scholar]
- 6.Tahirkheli NK, Greipp PR. Treatment of the systemic capillary leak syndrome with terbutaline and theophylline. A case series. Ann Intern Med 1999;130:905–9 [DOI] [PubMed] [Google Scholar]
- 7.Dolberg-Stolik OC, Putterman C, Rubinow A, et al. Idiopathic capillary leak syndrome complicated by massive rhabdomyolysis. Chest 1993;104:123–6 [DOI] [PubMed] [Google Scholar]
- 8.Harbarth S, Holeckova K, Froidevaux C, et al. ; Geneva Sepsis Network . Diagnostic value of procalcitonin, interleukin-6, and interleukin-8 in critically ill patients admitted with suspected sepsis. Am J Respir Crit Care Med 2001;164:396–402 [DOI] [PubMed] [Google Scholar]
- 9.Zipponi M, Eugster R, Birrenbach T. High-dose intravenous immunoglobulins: a promising therapeutic approach for idiopathic systemic capillary leak syndrome. BMJ Case Rep 2011;2011:pii: bcr1220103599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kapoor P, Greipp PT, Schaefer EW, et al. Idiopathic systemic capillary leak syndrome (Clarkson's disease): the Mayo clinic experience. Mayo Clin Proc 2010;85:905–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horger M, Hebart H, Einsele H, et al. Initial CT manifestations of invasive pulmonary aspergillosis in 45 non-HIV immunocompromised patients: association with patient outcome? Eur J Radiol 2005;55:437–44 [DOI] [PubMed] [Google Scholar]
- 12.Volk HD, Reinke P, Docke WD. Clinical aspects: from systemic inflammation to 'immunoparalysis’. Chem Immunol 2000;74:162–77 [DOI] [PubMed] [Google Scholar]
- 13.Atkinson JP, Waldmann TA, Stein SF, et al. Systemic capillary leak syndrome and monoclonal IgG gammopathy; studies in a sixth patient and a review of the literature. Medicine (Baltimore) 1977;56:225–39 [DOI] [PubMed] [Google Scholar]
- 14.Zhang W, Ewan PW, Lachmann PJ. The paraproteins in systemic capillary leak syndrome. Clin Exp Immunol 1993;93:424–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sprung CL, Annane D, Keh D, et al. Hydrocortisone therapy for patients with septic shock. N Engl J Med 2008;358:111–24 [DOI] [PubMed] [Google Scholar]
- 16.Casserly B, Gerlach H, Phillips GS, et al. Low-dose steroids in adult septic shock: results of the Surviving Sepsis Campaign. Intensive Care Med 2012;38:1946–54 [DOI] [PubMed] [Google Scholar]
- 17.Lionakis MS, Kontoyiannis DP. Glucocorticoids and invasive fungal infections. Lancet 2003;362:1828–38 [DOI] [PubMed] [Google Scholar]


