Abstract
Mitral valve endocarditis complicating hypertrophic cardiomyopathy is rare especially in the absence of significant mitral regurgitation. The occurrence of large vegetation and an abscess formation is even rarer. Endocarditis occurs predominantly on the left ventricular aspect of the anterior mitral leaflet. We report a case of a 34-year-old woman with asymptomatic obstructive hypertrophic cardiomyopathy who developed mitral valve endocarditis with large vegetation and subsequently an abscess caused by a rare organism Gemella morbillorum, following dental extraction. The patient underwent antibacterial therapy followed by successful mitral valve replacement for severe mitral regurgitation and her postoperative course has been asymptomatic so far. This case is unique in describing endocarditis by a rare organism as a cause of large vegetation and an abscess on an unusual site on the mitral valve leaflet without predisposition of haemodynamically significant mitral regurgitation and illustrates the potential lifesaving role of timely intervention.
Background
Infective endocarditis (IE) is a relatively rare complication of hypertrophic cardiomyopathy (HCM). This has been reported previously and is known to be associated with substantial morbidity and mortality. However, the literature which is available on the association of endocarditis in HCM is scarce. The cumulative probability of developing endocarditis over a period of 10 years in cases of HCM having significant intracavitary obstruction is <5%.1 While IE is an uncommon complication within the overall HCM population it can be potentially devastating and can damage cardiac structure and valvular function and can cause systemic embolisation which is also a potentially life-threatening complication. Failure to appropriately manage the patients who do not respond to antibiotics or who have evidence of abscess formation may lead to fatal outcome. We report the case of a 34-year-old woman with asymptomatic HCM and mitral valve endocarditis with Gemella morbillorum, a rare organism causing endocarditis with only a few reported cases.
Case presentation
A 34-year-woman presented to us with low-grade fever since the past 2 weeks associated with swelling of lower limbs, facial puffiness and breathlessness on exertion since 1 week. The patient had undergone dental extraction 3 weeks ago. She had been previously diagnosed of having hypothyroidism and had been on irregular treatment. The patient was diagnosed of having HCM during routine evaluation for a murmur and was not on any treatment. Examination revealed tachycardia, normal blood pressure and oxygen saturation. Pallor and pedal oedema were evident. Examination showed elevated jugular venous pulse, hyperdynamic apex and ejection systolic murmur at the lower left sternal border. She also had basal crepitations and a palpable spleen.
Investigations
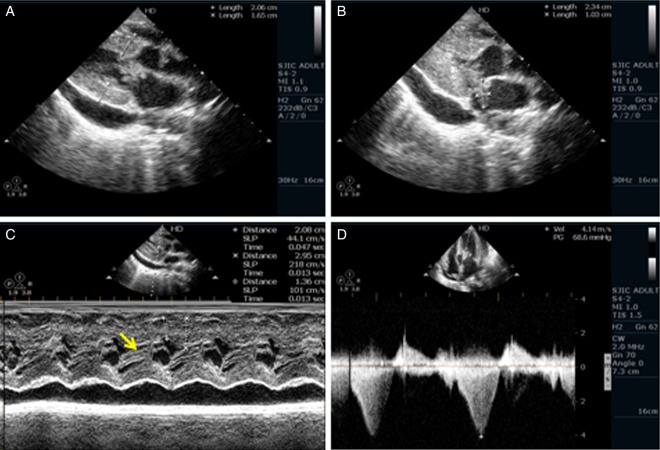
Initial blood tests showed raised inflammatory markers (C reactive protein 204 mg/L, erythrocyte sedimentation rate 45 mm), thrombocytopenia and mildly deranged renal function. ECG showed major left ventricular hypertrophy and abnormal repolarisation in the lateral ECG leads. Two-dimensional echocardiography showed localised septal hypertrophy (2.2 cm; figure 1A, video 1).There was a large (22×12 mm), mobile vegetation on the anterior mitral leaflet (AML; figure 1B, video 2) and mitral regurgitation (MR) was quantified as mild. Mild pericardial effusion was also seen. The M mode confirmed the systolic anterior motion of the AML (figure 1C). Continuous-wave Doppler gave a maximal predicted gradient of 68 mm Hg across the left ventricular outflow (LVOT; figure 1D).
Figure 1.
(A) Parasternal long axis (PLAX) view of septal hypertrophy and a vegetation on the anterior mitral leaflet (AML). (B) PLAX view of a large vegetation on AML and pericardial effusion. (C) M-mode echocardiography showing systolic anterior motion of AML. (D) Continuous wave Doppler showing significant left ventricular outflow gradient of 68 mm Hg.
Parasternal long axis (PLAX) view showing septal hypertrophy and a vegetation on Anterior Mitral Leaflet (AML).
PLAX view showing a large vegetation on AML and pericardial effusion.
Blood cultures drawn at presentation showed Gram-positive cocci in clumps at 2 days, presumptively identified as coagulase-negative staphylococci; however, 4 days later the final identity of the microorganism was confirmed as G. morbillorum, sensitive to penicillin, cephalosporins and quinolones.
Treatment
Treatment with intravenous crystalline penicillin and levofloxacin was initiated and the case was discussed with a microbiologist and a cardiothoracic surgeon. Bearing in mind the large size of vegetation and virulence of the organism, early surgery was planned. The patient initially did not consent for surgery.
However, the patient did not respond to the antibiotic therapy along with the heart failure medications and the fever persisted, dyspnoea worsened. Review echocardiogram showed a large ruptured abscess over AML (figure 2A, video 3) with severe MR (figure 2B, video 4). After 2 weeks of antibiotic therapy and a negative blood culture the patient was subjected for mitral valve replacement.
Figure 2.
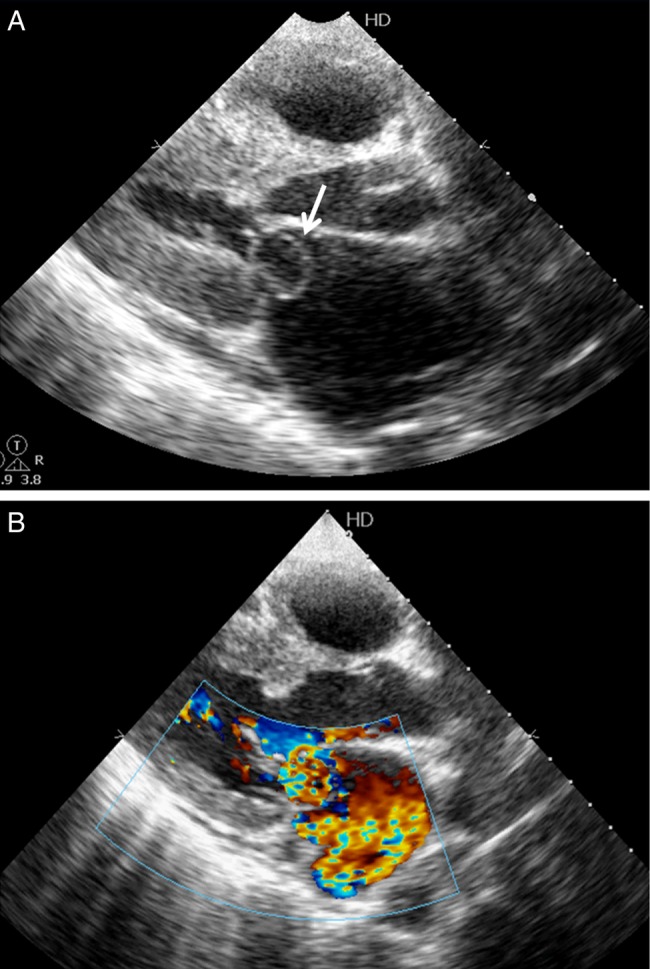
(A) Parasternal long axis view of a large abscess over the anterior mitral leaflet. (B) Colour Doppler showing severe mitral regurgitation caused by the endocarditis.
PLAX view showing a large abscess over AML.
Colour Doppler showing severe mitral regurgitation caused by the endocarditis.
Outcome and follow-up
Postoperatively the patient improved symptomatically and was discharged after completion of 6 weeks of parenteral antibiotic treatment. At 6 months of follow-up the patient is asymptomatic.
Discussion
In a comprehensive review of >800 patients with HCM, Spirito et al1 identified 10 patients with endocarditis .The prevalence of endocarditis in patients with HCM in this study was estimated at 3.7/1000 patients. All patients who developed endocarditis had LVOT obstruction under basal condition. This higher risk of endocarditis may be due to damage of the mitral and aortic valve endocardium caused by the high velocity and turbulence of blood flow during ejection and by the mitral septal contact during systole, as well as MR, which is often present in patients with outflow obstruction. Examination of excised mitral valves has indicated that vegetations were located most commonly on the septal aspect of the AML. Systolic anterior motion of the AML is thereby considered to be relevant to the pathogenesis of endocarditis.2
G. morbillorum is a commensal facultative anaerobic Gram-positive coccus found in the oropharynx and gastrointestinal, respiratory and urogenital tracts.3 It is a rare cause of endocarditis with few reported cases, although endocarditis is the most common manifestation of G. morbillorum infection. Gemella spp are related to the viridans group streptococci. Periodontitis is the most frequently implicated source of this organism.4 Association with colonic carcinoma has been described. It has been suggested that an immunocompromised status may contribute to the pathogenesis; however, our patient was not immunocompromised. Cephalosporins in combination with aminoglycosides are preferred; however, treatment should be based on sensitivity pattern.
Mitral valve surgery and the Morrow septal myectomy are accepted methods of treating symptomatic obstructive HCM refractory to medical treatment, but the two operations are rarely combined.5 Failure to operate on patients who do not respond rapidly to antibiotics or who have evidence of abscess formation often leads to a fatal outcome. Although current guidelines do not recommend antibiotic prophylaxis to prevent endocarditis in HCM, we believe it should be considered in high risk cases and the approach should be individualised. Cases that should be considered as high risk for endocarditis as those with a history of endocarditis, haemodynamically significant MR, coexistent structural mitral valve disease and significant prolapsed mitral valve. The importance of oral hygiene should be emphasised.
The occurrence of a large vegetation and abscess by this rare organism has rarely been described previously and its occurrence in this uncommon setting of HCM makes this case unique and previously unreported.
Learning points.
Hypertrophic cardiomyopathy (HCM) although not recommended as an indication for prophylaxis for infective endocarditis can rarely be associated with mitral valve endocarditis which is a potentially life-threatening complication.
Gemella Morbillorum is an extremely rare organism causing endocarditis and usually affects the immunocompromised population, although very rarely may be associated with disease even in the immunocompetent.
This organism can even lead to the occurrence of large vegetation and an abscess which has never been described previously.
Our case highlights the importance of timely surgery in the management and the importance of oral hygiene in the prevention of endocarditis in HCM.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Spirito P, Rapezzi C, Bellone P, et al. Infective endocarditis in hypertrophic cardiomyopathy: prevalence, incidence, and indications for antibiotic prophylaxis. Circulation 1999;99:2132–7 [DOI] [PubMed] [Google Scholar]
- 2.Roberts W, Kishel J, McIntosh C, et al. Severe mitral or aortic regurgitation, or both, requiring valve replacement for infective endocarditis complicating hypertrophic cardiomyopathy. J Am Coll Cardiol 1992;19:365–71 [DOI] [PubMed] [Google Scholar]
- 3.Reyes R, Abay A, Siegel M. Gemella morbillorum bacteremia associated with adenocarcinoma of the cecum. Am J Med 2001;111:164–5 [DOI] [PubMed] [Google Scholar]
- 4.Kuriyama T, Karasawa T, Nakagawa K, et al. Bacteriology and antimicrobial susceptibility of gram-positive cocci isolated from pus specimens of orofacial odontogenic infections. Oral Microbiol Immunol 2002;17:132–5 [DOI] [PubMed] [Google Scholar]
- 5.Ponoth P, Kerr A, Raudkivi P, et al. Surgical correction of hypertrophic obstructive cardiomyopathy: seventeen-year Green Lane experience. J Card Surg 1997;12:294–9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Parasternal long axis (PLAX) view showing septal hypertrophy and a vegetation on Anterior Mitral Leaflet (AML).
PLAX view showing a large vegetation on AML and pericardial effusion.
PLAX view showing a large abscess over AML.
Colour Doppler showing severe mitral regurgitation caused by the endocarditis.