Abstract
A female patient suffered from gradual decline of vision for few months. She presented with bilateral multiple pigmented choroidal tumours, associated with overlying retinal changes. The clinical presentation suggested bilateral diffuse uveal melanocytic proliferation (BDUMP) syndrome, which is a paraneoplastic disease, although there was no evidence of any concurrent malignancy. The periodic systemic surveillance that was undertaken for the following 4 years failed to reveal any occult cancer. Nevertheless, there has been relentless progressive deterioration in vision as a consequence of BDUMP syndrome. The management of the declining vision in BDUMP syndrome is challenging and controversial.
Background
Bilateral diffuse uveal melanocytic proliferation (BDUMP) is a paraneoplastic syndrome that affects the eyes of patients with systemic malignancy.1 It is characterised by proliferation of uveal melanocytes, producing pigmented and non-pigmented uveal tumours with associated exudative retinal detachment and rapidly developing cataract. A characteristic manifestation is the presence of multiple orange-red geographical patches and areas of focal retinal pigment epithelial loss that forms a striking fluorescein angiography (FA) pattern.2 In BDUMP syndrome, systemic carcinoma is often detected after the ocular manifestations,1–4 and the majority of patients expire within 3 years of their initial presentation.2 4 The response of BDUMP to different interventions, including treating the underlying malignancy, is generally poor. Typically, most patients suffer precipitous severe vision loss. This patient has demonstrated atypical course with failure to detect any occult malignancy despite repeated systemic workup after 50 months of BDUMP presentation. BDUMP has led to gradual loss of vision by several mechanisms. The ocular and systemic treatments undertaken in this patient failed to halt the progression of vision loss, presenting a treatment dilemma.
Case presentation
A 75-year-old female patient was evaluated for bilateral pigmented fundus lesions associated with decrease in vision OU of 4 months duration. Her visual acuity was 20/50 OD and 20/30 OS at initial presentation. Anterior segment examination revealed early cataract in both eyes. Intraocular pressure was 18 mm Hg OU. Fundus examination revealed bilateral four flat to minimally raised pigmented choroidal lesions, each was 4–5 mm in basal diameter, with orange-brown, giraffe-skin-like geographic patches at the level of retinal pigment epithelium (RPE) (figure 1A). The patient was unaware of concurrent malignancy; however, she had a history of partial urinary bladder resection 5 years before for low-grade transitional cell carcinoma. The following yearly assessments thereafter revealed no evidence of recurrence or metastases.
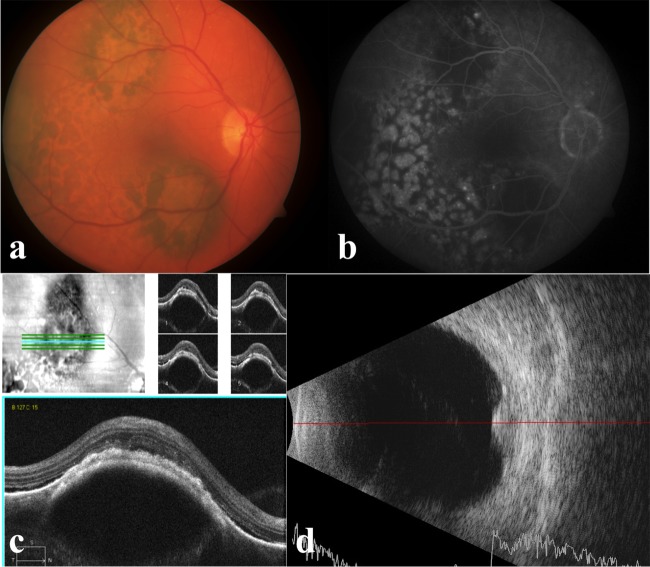
Figure 1.
Manifestations of bilateral diffuse uveal melanocytic proliferation at initial presentation: (A) fundus photo showing flat to minimally raised pigmented choroidal lesions, each was 4–5 mm in basal diameter, with orange-brown, giraffe-skin-like oval patches; (B) fluorescein angiography showing areas of hypofluorescence corresponding to the pigmented choroidal tumours. Hyperfluorescent spots alternating with reticular areas of blocked fluorescence; (C) optical coherence tomography showing the pigmented lesions as areas of focal choroidal thickening, with overlying areas of retinal pigment epithelium atrophy and depositions; (D) ultrasonography showing the pigmented lesions as multiple focal choroidal thickenings with medium internal reflectivity and focal retinal detachments.
Investigations
FA performed at the initial assessment revealed areas of hypofluorescence corresponding to the pigmented choroidal tumours. Hyperfluorescent spots alternating with reticular areas of blocked fluorescence were observed (figure 1B). Optical coherence tomography revealed that the pigmented lesions represent areas of focal choroidal thickening, with overlying areas of RPE atrophy and depositions (figure 1C). With ultrasonography, the pigmented lesions appeared as multiple focal choroidal thickenings with medium internal reflectivity and focal retinal detachments (figure 1D).
The patient was subjected to a series of investigations in search for any occult malignancy. They included CT scans of the chest, abdomen and pelvis, mammography, full blood count, tumour markers including CEA, CA-125 and LDH. Colonoscopy, dermatological assessment and genitourinary oncology were also performed. The results did not reveal any evidence of systemic cancer.
Differential diagnosis
Differential diagnosis of BDUMP includes multiple choroidal metastases from skin melanoma, which do not produce the characteristic giraffe-skin appearance and run a highly aggressive course. Multiple choroidal naevi, as in association with neurofibromatosis-I, can be bilateral but are stationary and are not associated with retinal changes.
Treatment
Along the following 50 months after the initial presentation, full body imaging and tumour markers were repeated every 3–6 months, which failed to detect any occult cancer.
Plasma exchange to reduce the presumed antibody burden was undertaken over seven sessions, 2 years after the initial presentation. Plasma exchange started daily for three consecutive days and then every other day until end of the course, and involved exchange of one plasma volume with 5% albumin solution in each session. Plasma exchange did not exhibit positive impact on the BDUMP manifestations. Conversely, serial anterior segment photos after plasma exchange showed growth of new iris-pigmented masses (figure 2A). There was gradual increase of pigment dispersion on iris surface, corneal endothelium and angle, with subsequent development of pigmentary glaucoma (figure 2B).
Figure 2.
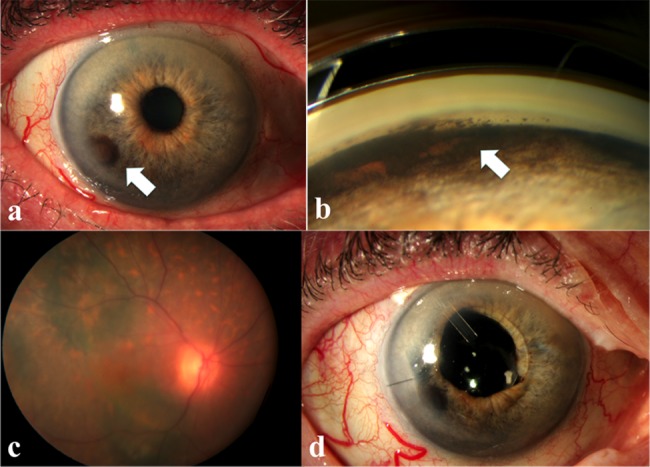
Progression of bilateral diffuse uveal melanocytic proliferation after 50 months of initial presentation: (A) anterior segment photo showing growth of new iris-pigmented masses after plasma exchange; (B) increased pigment deposition in the angle; (C) increase in the dimensions of the pigmented choroidal lesions; (D) appearance of the eye after phacoemulsification and Ahmed valve surgeries.
Similarly, serial fundus photographs showed gradual increase in the dimensions and number of the pigmented choroidal lesions (figure 2C).
The patient eventually underwent bilateral phacoemulsification for progressive cataract, Ahmed valve implant and 180° transcleral cyclodiode laser to control the refractory pigmentary glaucoma (figure 2D).
Outcome and follow-up
Cataract surgeries resulted in minimal visual improvement because of the coexisting glaucoma and focal exudative retinal detachments.
Her vision gradually deteriorated as she continued to slowly develop new BDUMP lesions. Despite the glaucoma filtration surgery, the intraocular pressure continued to rise with further accumulation of pigmented iris lesions and pigment accumulation. The latest visual acuity is counting fingers at 1 m OD, and 20/80 OS.
Discussion
This case of BDUMP syndrome displayed the typical characteristic ocular features, but showed atypical clinical course. The patient remains rather healthy with no detectable cancer for 55 months since the initial BDUMP presentation. Her vision has been gradually deteriorating along the course of the disease, despite surgical interventions. This course is dissimilar to the majority of published reports where BDUMP syndrome cases became legally blind within 1 year and died within 3 years of BDUMP diagnosis.2 4
The pathogenesis of BDUMP is stipulated to result from circulating antiretinal autoantibodies and humoral factors that selectively induce melanocyte proliferation.5 6
Nevertheless, treating BDUMP with systemic steroids has been reported to be ineffective.1 7
Moreover, it has been suggested that BDUMP represents a part of an autoimmune response against a systemic cancer, and suppression of this response could trigger cancer growth.8
Elimination of antibodies in BDUMP syndrome through plasma exchange or plasmapheresis has been reported and should theoretically avoid the side effects of steroids and immunosuppressants.6 9 Nonetheless, multiple frequent courses of plasma exchange or plasmaphresis carries potential morbidities from immunosuppression, and quick relapse was reported to occur soon after plasmapheresis is completed.6
Despite using plasma exchange in our patient, her vision continued to deteriorate with progression of the BDUMP lesions and development of new iris tumours shortly after completing the course.
In summary, BDUMP represents a management dilemma to the clinician. The ocular manifestations that cause progressive visual deterioration are the result of an autoimmune paraneoplastic process that thought to suppress an occult cancer. Hence, attempts at suppressing this autoimmune process to halt the BDUMP-induced vision loss may enhance cancer growth.
Patients with BDUMP should be counselled on their first presentation about the possible long course of the disease, the ineffectiveness of the current treatments to preserve vision and the need for repeated investigations in search for an occult malignancy.
Learning points.
Bilateral diffuse uveal melanocytic proliferation (BDUMP) syndrome is an ocular paraneoplastic syndrome that often heralds an occult cancer.
This patient showed an atypical course with no detectable cancer, and gradual progressive visual deterioration for 55 months after initial BDUMP presentation.
The results of immunosuppression, for example, with plasmapheresis or plasma exchange are disappointing and carry a potential risk of fulminating occult cancer.
Patients with BDUMP should be counselled with respect to the poor visual expectations of their disease and the ineffectiveness of the current treatments to preserve vision.
Footnotes
Contributors: SA and HK contributed to the concept and design, and interpretation of the results. SA, AAA and HK were involved in writing the manuscript and approved the final draft.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Gass JD, Gieser RG, Wilkinson CP, et al. Bilateral diffuse uveal melanocytic proliferation in patients with occult carcinoma. Arch Ophthalmol 1990;108:527–33 [DOI] [PubMed] [Google Scholar]
- 2.Chahud F, Young RH, Remulla JF, et al. Bilateral diffuse uveal melanocytic proliferation associated with extraocular cancers: review of a process particularly associated with gynecologic cancers. Am J Surg Pathol 2001;25:212–18 [DOI] [PubMed] [Google Scholar]
- 3.Navajas EV, Simpson ER, Krema H, et al. Cancer-associated nummular loss of RPE: expanding the clinical spectrum of bilateral diffuse uveal melanocytic proliferation. Ophthalmic Surg Lasers Imaging 2011;42:e103–6 [DOI] [PubMed] [Google Scholar]
- 4.O'Neal KD, Butnor KJ, Perkinson KR, et al. Bilateral diffuse uveal melanocytic proliferation associated with pancreatic carcinoma: a case report and literature review of this paraneoplastic syndrome. Surv Ophthalmol 2003;48:613–24 [DOI] [PubMed] [Google Scholar]
- 5.Miles SL, Niles RM, Pittock S, et al. A factor found in the IgG fraction of serum of patients with paraneoplastic bilateral diffuse uveal melanocytic proliferation causes proliferation of cultured human melanocytes. Retina 2012;32:1959–66 [DOI] [PubMed] [Google Scholar]
- 6.Mets RB, Golchet P, Adamus G, et al. Bilateral diffuse uveal melanocytic proliferation with a positive ophthalmoscopic and visual response to plasmapheresis. Arch Ophthalmol 2011;129:1235–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sen J, Clewes AR, Quah SA, et al. Presymptomatic diagnosis of bronchogenic carcinoma associated with bilateral diffuse uveal melanocytic proliferation. Clin Exp Ophthalmol 2006;34:156–8 [DOI] [PubMed] [Google Scholar]
- 8.Chan C, O'Day J. Melanoma-associated retinopathy: does autoimmunity prolong survival? Clin Exp Ophthalmol 2001;29:235–8 [DOI] [PubMed] [Google Scholar]
- 9.Jaben EA, Pulido JS, Pittock S, et al. The potential role of plasma exchange as a treatment for bilateral diffuse uveal melanocytic proliferation: a report of two cases. J Clin Apheresis 2011;26:356–61 [DOI] [PubMed] [Google Scholar]