Abstract
Knee arthroscopy is an important diagnostic and therapeutic tool in the management of disorders of the knee. In a series of 4 articles, the basics of knee arthroscopy are reviewed. In this article (part 2), surface anatomy and the anterolateral and anteromedial portals are reviewed. Accurate portal placement is critical to both diagnostic and operative arthroscopy. Mastery of the surface anatomy allows accurate and reproducible portal placement.
Knee arthroscopy is the most commonly performed orthopaedic procedure. Indications include diagnostic arthroscopy, meniscectomy, loose body removal, chondroplasty, microfracture, irrigation and debridement, and ligament reconstruction. In this series of articles, we present a comprehensive review of the complete surgical technique for basic knee arthroscopy.1,2
Knee surface anatomy and portal placement are reviewed in this article and Video 1. Accurate portal placement is critical to both diagnostic and operative arthroscopy. Mastery of the surface anatomy allows accurate and reproducible portal placement. Proper placement of the anterolateral portal just superior to the lateral meniscus and just lateral to the patellar tendon allows optimal visualization of the compartments of the knee and proper access for the operative instruments. Proper placement of the anteromedial portal just superior to the medial meniscus but inferior enough for instruments to reach the posterior horn of the meniscus is also critical.
Surgical Technique
This article will review the relevant surface anatomy as well as placement of the anterolateral and anteromedial portals (Fig 1). Beginning arthroscopists will find it beneficial to mark out the surface anatomy as a reference for portal placement. The palpable borders of the patella, tibial tubercle, and patellar tendon, the medial and lateral tibial joint line, and the head of the fibula are marked on the skin. Typically, the lateral joint line is slightly more superior than the medial joint line. The marks will give a reference for placement of the arthroscopic portals. The anterolateral and anteromedial portals can be vertical or horizontal. Horizontal portals are more cosmetic, but if they are placed too high or too low, they may be difficult to correct, so the beginning arthroscopist may prefer a vertical portal. The superomedial portal is an optional portal typically used for fluid outflow. The anterolateral portal is placed 1 cm above the joint line and just next to the patellar tendon in a palpable soft spot. The anteromedial portal is placed 1 cm above the joint line and 1 cm medial to the patellar tendon, also in a palpable soft spot. The placement of the anteromedial portal can be confirmed with a spinal needle using the arthroscope.
Fig 1.
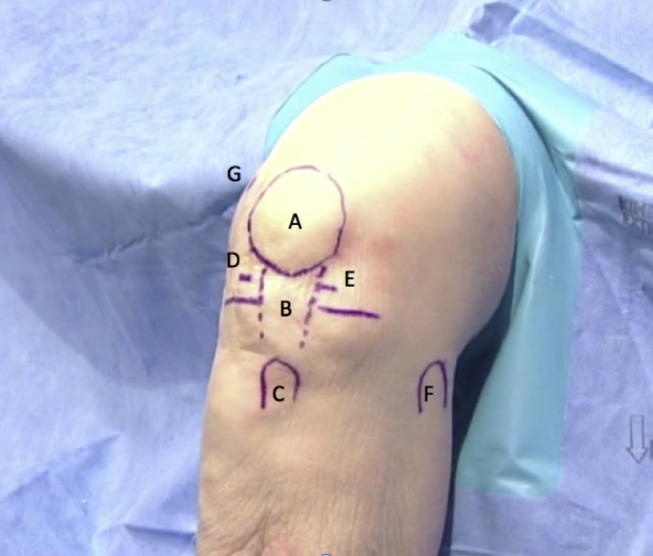
Surface anatomy markings for a left knee: (A) patella, (B) patellar tendon, (C) tibial tubercle, (D) anteromedial portal, (E) anterolateral portal, (F) fibular head, and (G) superior medial portal (optional portal for fluid outflow).
After marking, the portals are typically injected with a local anesthetic. A No. 15 or 11 blade with the blade facing away from the patellar tendon is used to make a 4- to 5-mm portal. The skin and the joint capsule are incised, with care taken not to damage the ligaments or cartilage and to stay above the meniscus. The arthroscopic cannula with a blunt obturator is then brought into the field and held with the index finger along the cannula. The cannula is inserted into the anterolateral portal at an angle parallel to the tibial plateau and directed between the condyles. The cannula is then pushed into the intercondylar notch. This motion is repeated a few times to ensure that the cannula moves freely through the portal and fat pad. Then, the cannula is pulled back just enough to be outside of the intercondylar notch, the knee is straightened into full extension, and the cannula is advanced under the patella into the suprapatellar pouch. The obturator is removed, and the arthroscopic camera is locked into the cannula. The fluid flow is then started, and the arthroscopic procedure is begun. Basic diagnostic and operative arthroscopy will be discussed in the subsequent articles.
The anteromedial portal is the main working or instrumentation portal. The placement of this portal is critical for effectively reaching the various intra-articular structures with the arthroscopic instruments. It is recommended to create this portal under direct vision using the arthroscope. A spinal needle is inserted into the medial compartment through the previously marked portal. The needle is held toward the tip so as not to over-penetrate and damage the cartilage. The needle is inserted just above the meniscus. Under direct vision, the needle is advanced to touch the posterior horn of the medial meniscus (Fig 2). If the entry angle is too high or too vertical, the femur will prevent access to the posterior structures. After an optimal position is found, the needle is removed and the No. 15 or 11 blade is used again to cut the skin approximately 5 mm. The knife is then advanced, and an inline capsulotomy is performed. Fluid escape from the portal is seen when an adequate capsulotomy has been performed. At this point, a beginning arthroscopist and even some advanced arthroscopists will put a cannula into the portal. A hemostat can also be used to spread the portal to make the passage of instruments easier.
Fig 2.
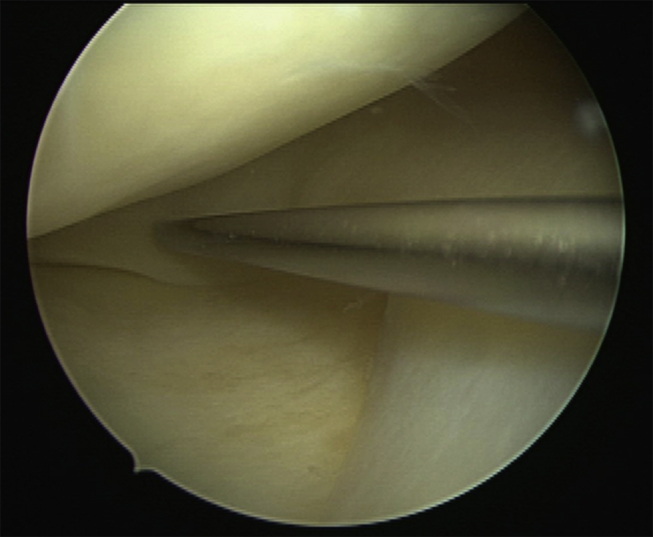
Arthroscopic view, left knee, of medial compartment taken from the anterolateral portal. A spinal needle is used to determine the placement of the anteromedial portal. The needle should enter the knee just superior to the medial meniscus and inferior enough to reach the posterior horn of the medial meniscus.
Discussion
Knee arthroscopy is a valuable diagnostic and therapeutic procedure for the treatment of various knee disorders. Precise placement of the anterolateral and anteromedial portals allows for full access to the compartments of the knee. A key point to remember in marking the surface anatomy is that the lateral tibial plateau is usually slightly superior to the medial tibial plateau. Marking the surface anatomy will facilitate accurate placement of the portals. The anterolateral portal should be placed just superior to the lateral meniscus and close to the patellar tendon. The anteromedial portal is the main working portal and therefore should be placed under direct visualization to ensure that the instruments will be able to reach the posterior meniscus and other structures.
Footnotes
The authors report the following potential conflict of interest or source of funding: B.D.W. receives support from Arthrex Fellows Forum Travel and Hotel; J.H.L. receives support from SNE, Arthrex, Ivivi, AANA, law firms not related to the orthopaedic industry (i.e., medical malpractice defense, ski industry defense), Breg, Donjoy, Smith & Nephew, MTF, DCI, patents pending with Arthrex not related to manuscript, Taos Orthopaedic Institute, Taos Center for Sportsmedicine and Rehabilitation, and Taos MRI.
Supplementary Data
Demonstration and review of key principles of surface anatomy and anterior portal placements for basic knee arthroscopy.
References
- 1.Phillips B.B. Arthroscopy of the lower extremity. In: Canale S.T., Beaty J.H., editors. Campbell's operative orthopaedics. Ed 11. Mosby Elsevier; Philadelphia: 2008. pp. 2811–2893. [Google Scholar]
- 2.Aviles S.A., Allen C.R. Knee arthroscopy: The basics. In: Wiesel S.W., editor. Operative techniques in orthopaedic surgery. Lippincott Williams & Wilkins; Philadelphia: 2011. pp. 248–256. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Demonstration and review of key principles of surface anatomy and anterior portal placements for basic knee arthroscopy.


