Abstract
Recently, surgical treatment of a symptomatic unicameral cyst of the proximal femur has been achieved with less invasive procedures than traditional open curettage with an autologous bone graft. In this article we introduce endoscopic surgery for a symptomatic unicameral cyst of the proximal femur. The presented technique, which includes minimally invasive endoscopic curettage of the cyst and injection of a bone substitute, not only minimizes muscle damage around the femur but also enables sufficient curettage of the fibrous membrane in the cyst wall and the bony septum through direct detailed visualization by an endoscope. Furthermore, sufficient initial strength after curettage can be obtained by injecting calcium phosphate cement as a bone substitute.
Unicameral bone cysts are benign, fluid-filled cavities that tend to expand and weaken the local area, and these cysts affect predominantly patients aged younger than 20 years.1 The most common site is the femur, followed by the proximal humerus.1 For a unicameral bone cyst of the femur, surgical intervention is actively recommended because of the high-stress weight-bearing area of the bone.1 Although open curettage and autologous bone grafting have conventionally been used as the definitive treatment for unicameral bone cysts,2 indicating such surgical methods is problematic because of long-term morbidity.
Recently, a number of minimally invasive surgical procedures for unicameral bone cysts of the femur—such as continuous decompression with intramedullary nailing3,4 and minimally invasive curettage and injection of bone substitute5-7—have been reported. However, there has been no report about the application of endoscopy for curettage of a unicameral bone cyst of the proximal femur. We introduce our endoscopic surgery technique, which includes injection of a bone substitute for a unicameral bone cyst of the proximal femur.
Surgical Technique
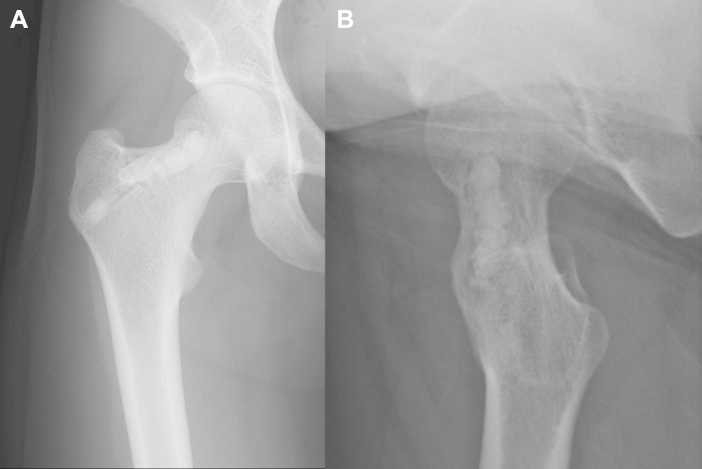
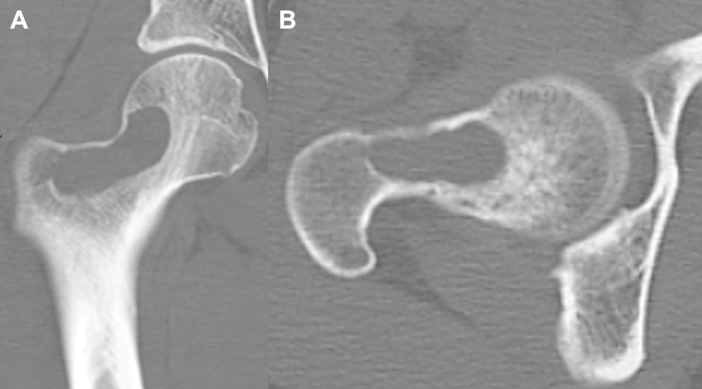
Plain radiography shows a cystic lesion in the right proximal femur that extends from the femoral neck to the intertrochanteric region. Similarly, computed tomography shows a cystic lesion in the proximal femur with destruction of the anterior and superior cortical wall, which has a risk of pathologic fracture (Fig 1). T1- and T2-weighted magnetic resonance images show hypointense and hyperintense masses, respectively, that are brighter than the surrounding fat tissue (Fig 2). These radiologic findings support the diagnosis of a unicameral bone cyst of the proximal femur.
Fig 1.
(A) Coronal and (B) axial views on preoperative computed tomography scans of the right proximal femur show a cystic lesion. The anterior and superior cortical wall of the cyst is at risk of pathologic fracture.
Fig 2.
(A) An axial T1-weighted magnetic resonance image of the right proximal femur shows a hypointense mass. (B) A coronal T2-weighted image on the same part shows a hyperintense mass. These findings are evidence for the diagnosis of a unicameral bone cyst of the right proximal femur.
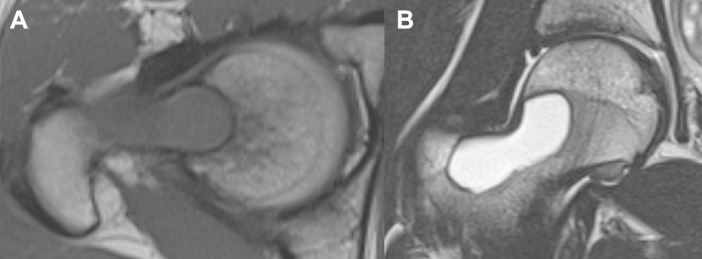
The patient is placed in the supine position on the operating table under general anesthesia (Table 1). The bilateral lower extremity is fixed to a fracture traction table, and the contralateral hip joint is abducted to permit easy intraoperative fluoroscopic assistance. First, on anteroposterior and lateral views under an image intensifier, a guidewire is inserted from a lateral point distal to the greater trochanter into the cavity of the cyst. After confirming an adequate position of the guidewire, the surgeon makes a lateral portal at the insertion point of the guidewire, and blunt dissection of the subcutaneous fatty tissue, fascia, and muscle around the guidewire is performed. Then, a bone tunnel that reaches into the cavity of the cyst is created by means of a cannulated drill with a diameter of 6.5 mm through the guidewire through the lateral portal. Next, a 2.7-mm, 30° angled arthroscope with normal saline solution irrigation delivered by a pressure-controlled pump is inserted through the lateral portal into the cavity, and detailed inspection of the cyst structure is performed. A guidewire is then inserted from an anterior point adjacent to the bone cyst into the cyst cavity under an anteroposterior view with an image intensifier, and an anterior portal is made in a similar fashion. Through the guidewire, the anterior cortical wall is fenestrated by the cannulated drill through the anterior portal from the anterior to the posterior part under endoscopic visualization through the lateral portal (Video 1). Then, through either of the portals under optimal endoscopic visualization, curettage of the fibrous inner surface is performed circumferentially with a small curette and forceps (Figs 3A and 3B, Video 1). After confirmation of sufficient curettage on endoscopy (Fig 3C), the cyst cavity is sufficiently irrigated, and calcium phosphate cement (Biopex; Pentax, Tokyo, Japan) is injected percutaneously under an image intensifier.
Table 1.
Steps and Key Points of Technique
| Step | Key Point |
|---|---|
| Position of patient | The patient is placed in the supine position on a fracture traction table, which permits easy intraoperative fluoroscopic assistance. |
| Creation of portals and approaches to cyst | Use anterior and posterior portals to avoid injury to the neurovascular structures and fluoroscopic imaging to confirm adequate creation of bone tunnels and fenestration of the cortex, which reaches the cyst. |
| Curettage of inner surface of cyst | Perform curettage via one portal under optimal endoscopic visualization via the other portal, and alternate portal for curettage. |
| Injection of calcium phosphate cement | Before the procedure, measure the capacity of the cyst after curettage by injecting saline solution. The volume of injected calcium phosphate cement is 1 mL less than the measured capacity. Obstruct the lateral portal using a metal rod with a diameter of 6 mm. |
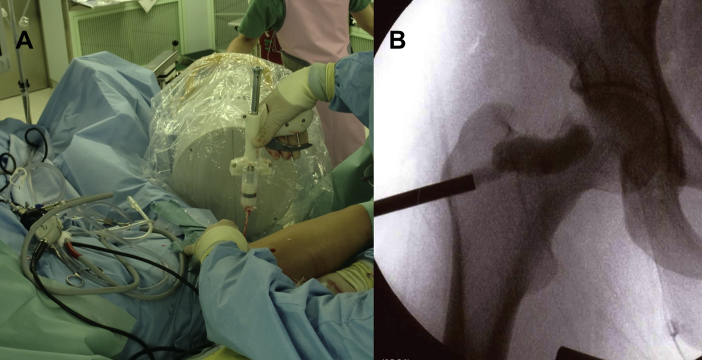
Fig 3.
(A) Clinical imaging of right femur in patient in supine position under fixation with fracture traction table. A 2.7-mm, 30° angled arthroscope and forceps are inserted through the lateral and anterior portals, respectively. (B) Endoscopic imaging shows curettage of the fibrous inner surface by a forceps, which is inserted through the anterior portal under direct endoscopic visualization through the lateral portal. (C) Endoscopic imaging through the lateral portal shows healthy bone marrow, which is exposed after curettage of the inner surface.
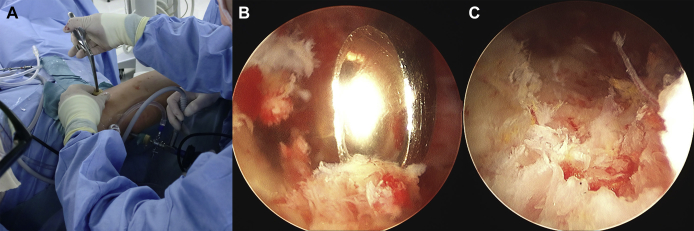
Before the procedure, the lateral portal is obstructed by use of a metal rod with a diameter of 6 mm, and saline solution is injected into the cyst cavity through the anterior portal to measure its capacity. The volume of injected calcium phosphate cement is 1 mL less than the measured capacity to reduce the chance of leakage into the soft tissue, and a gun-type manual cement injector is used to inject calcium phosphate cement (Fig 4). At the end of surgery, each portal is sutured (Fig 5). Partial weight bearing is allowed the day after surgery, and full weight bearing, as well as jogging, is allowed 1 week later. Figure 6 shows radiographs taken 2 years after surgery with the present technique. No radiologic features suggesting recurrence of the cyst are evident.
Fig 4.
(A) Clinical imaging of injection of calcium phosphate cement (Biopex) through anterior portal with gun-type manual cement injector under image intensifier. (B) Fluoroscopic view showing sufficient injection quantity of calcium phosphate cement through anterior portal without leakage. During the injection, the lateral portal is obstructed with a metal rod with a diameter of 6 mm to avoid leakage through this side.
Fig 5.

Clinical imaging of right femur of patient after wound closure. The described technique requires only 2 small incisions.
Fig 6.
(A) Anteroposterior and (B) axial radiographs of right proximal femur 30 months after surgery, showing no signs of recurrence or pathologic fracture.
Discussion
Conventionally, open curettage with autologous bone grafting has been the main procedure for a unicameral bone cyst.2 However, indicating this procedure for young patients engaging in sports activity seems to be problematic because it results in long-term morbidity. Recently, flexible intramedullary nailing, which enables continuous decompression and stability of cystic lesions by a less invasive procedure, has been applied for unicameral bone cysts of the long bones such as the femur and humerus.3,4 Roposch et al.3 studied the result of 12 cases with femoral neck and trochanteric simple bone cysts treated with retrograde insertion of a flexible intramedullary nail. Their results showed that 11 of the 12 simple bone cysts healed within a mean period of 38.3 months after nailing; however, 1 case needed plate fixation because of the loss of a reduced position, and 2 cases needed a nail change. Masquijo et al.4 reported 48 patients treated with intramedullary nailing for unicameral bone cysts. In their series 19 patients had a unicameral bone cyst of the proximal femur, and the healing rate was worse than that of other long bones.
On the other hand, a recent trend in surgical treatment for symptomatic unicameral bone cysts has been toward less invasive curettage and injection of a bone substitute, and several studies have shown the effectiveness of this approach for unicameral bone cysts.8-10 Rougraff and Kling5 applied trephination and percutaneous injection of demineralized bone matrix with autogenous bone marrow. In their study, 5 of 23 patients needed a second procedure because of recurrence. Dormans et al.6 performed percutaneous intramedullary curettage under fluoroscopic imaging and grafting with medical-grade calcium sulfate for unicameral bone cysts, and their method had a recurrence rate of 12.5%. Furthermore, Mik et al.7 reported a recurrence rate of 20% by using a similar technique with medical-grade calcium sulfate. A possible cause for recurrence after such procedures is inaccurate curettage of the fibrous membrane in the cyst wall. In fact, the procedure of Rougraff and Kling was not accompanied by curettage, whereas in another 2 procedures, by Dormans et al. and Mik et al., curettage was performed indirectly under fluoroscopic control.
Endoscopy has been applied for curettage of benign bone lesions on the humerus,11 femur,8,9 and calcaneus.10 For the calcaneus, 1 study showed the effectiveness of endoscopic curettage and injection of calcium phosphate cement in young athletes with symptomatic unicameral bone cysts who desired an early return to sports activity.10 For the proximal femur, only 2 cases have been reported in which endoscopic curettage was applied for benign bone lesions.8,9 Thompson and Woodward8 used an arthroscope as an adjunct in the resection of a chondroblastoma of the femoral head and reported the usefulness of the device, which resulted in minimal capsulotomy and osteotomy and no need to dislocate the hip joint. Similarly, Stricker9 performed endoscopic excision of a femoral head chondroblastoma and mentioned the effectiveness of the procedure with complete curettage possible through good visualization.
The present technique has several advantages (Table 2). First, minimizing muscle damage around the femur is possible by applying a less invasive endoscopic approach. Second, sufficient curettage of the fibrous membrane in the cyst wall and the bony septum can be performed through a 2-portal endoscopic approach, which enables direct detailed visualization. The 2-portal procedure enabled easy and safe access to the lesion without neurovascular injury. Furthermore, sufficient initial strength after curettage can be obtained by injecting calcium phosphate cement as a bone substitute. On the other hand, a possible risk of this technique is iatrogenic fracture during curettage of the inner wall on the thin cortex side by invasion of the cyst. In addition, leakage of calcium phosphate cement leads to damage to the subcutaneous tissue and skin, which may result in delayed wound union, even if each portal is small. Furthermore, for cases with a large bone cyst, the present technique may not be applied because of the limitation of performing circumferential curettage of the large cavity of the cyst through restrictive portals.
Table 2.
Benefits and Risks of Technique
| Benefit | Risk |
|---|---|
| Minimized muscle damage around femur through less invasive endoscopic approach | Iatrogenic fracture during curettage of inner wall on thin cortex side by invasion of cyst |
| Sufficient curettage of inner surface of cyst through 2-portal endoscopic approach | Leakage of calcium phosphate cement during injection |
| Sufficient initial strength after surgery by injecting calcium phosphate cement as bone substitute |
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Endoscopic surgery for symptomatic unicameral bone cyst of proximal femur. First, on anteroposterior and lateral views under an image intensifier, a guidewire is inserted from a lateral point distal to the greater trochanter into the cavity of the cyst, and a lateral portal is made at the insertion point of the guidewire. A bone tunnel that reaches into the cyst cavity is made under an image intensifier with a 6.5-mm cannulated drill. Next, the guidewire is inserted from an anterior point adjacent to the bone cyst into the cyst cavity under an anteroposterior view with an image intensifier, and an anterior portal is made in a similar fashion. Through the anterior portal, the anterior cortical wall is fenestrated with a 6.5-mm cannulated drill through the guidewire through the lateral portal under direct endoscopic visualization with an image intensifier. Then, endoscopic curettage of the fibrous inner surface is performed by inserting a small curette and forceps through the anterior or lateral portal under optimal endoscopic visualization. Finally, calcium phosphate cement (Biopex) is injected through the anterior portal with a gun-type manual cement injector under an image intensifier. During this procedure, the lateral portal is obstructed by use of a metal rod with a diameter of 6 mm.
References
- 1.Wilkins R.M. Unicameral bone cysts. J Am Acad Orthop Surg. 2000;8:217–224. doi: 10.5435/00124635-200007000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Bensahel H., Jepanno P., Desgrippes Y., Pennecot G.F. Solitary bone cyst: Controversies and treatment. J Pediatr Orthop B. 1998;7:257–261. doi: 10.1097/01202412-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Roposch A., Saraph V., Linhart W.E. Treatment of femoral neck and trochanteric simple bone cysts. Arch Orthop Trauma Surg. 2004;124:437–442. doi: 10.1007/s00402-004-0702-5. [DOI] [PubMed] [Google Scholar]
- 4.Masquijo J.J., Baroni E., Miscione H. Continuous decompression with intramedullary nailing for the treatment of unicameral bone cysts. J Child Orthop. 2008;2:279–283. doi: 10.1007/s11832-008-0114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rougraff B.T., Kling T.J. Treatment of active unicameral bone cysts with percutaneous injection of demineralized bone matrix and autogenous bone marrow. J Bone Joint Surg Am. 2002;84:921–929. doi: 10.2106/00004623-200206000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Dormans J.P., Sankar W.N., Moroz L., Erol B. Percutaneous intramedullary decompression, curettage, and grafting with medical-grade calcium sulfate pellets for unicameral bone cysts in children: A new minimally invasive technique. J Pediatr Orthop. 2005;25:804–811. doi: 10.1097/01.bpo.0000184647.03981.a5. [DOI] [PubMed] [Google Scholar]
- 7.Mik G., Arkader A., Manteghi A., Dormans J.P. Results of a minimally invasive technique for treatment of unicameral bone cysts. Clin Orthop Relat Res. 2009;467:2949–2954. doi: 10.1007/s11999-009-1008-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thompson M.S., Woodward J.S., Jr. The use of the arthroscope as an adjunct in the resection of a chondroblastoma of the femoral head. Arthroscopy. 1995;11:106–111. doi: 10.1016/0749-8063(95)90097-7. [DOI] [PubMed] [Google Scholar]
- 9.Stricker S.J. Extraarticular endoscopic excision of femoral head chondroblastoma. J Pediatr Orthop. 1995;15:578–581. [PubMed] [Google Scholar]
- 10.Innami K., Takao M., Miyamoto W., Abe S., Nishi H., Matsushita T. Endoscopic surgery for young athletes with symptomatic unicameral bone cyst of the calcaneus. Am J Sports Med. 2011;39:575–581. doi: 10.1177/0363546510388932. [DOI] [PubMed] [Google Scholar]
- 11.Randelli P., Arrigoni P., Cabitza P., Denti M. Unicameral bone cyst of the humeral head: Arthroscopic curettage and bone grafting. Orthopedics. 2009;32:54. doi: 10.3928/01477447-20090101-18. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic surgery for symptomatic unicameral bone cyst of proximal femur. First, on anteroposterior and lateral views under an image intensifier, a guidewire is inserted from a lateral point distal to the greater trochanter into the cavity of the cyst, and a lateral portal is made at the insertion point of the guidewire. A bone tunnel that reaches into the cyst cavity is made under an image intensifier with a 6.5-mm cannulated drill. Next, the guidewire is inserted from an anterior point adjacent to the bone cyst into the cyst cavity under an anteroposterior view with an image intensifier, and an anterior portal is made in a similar fashion. Through the anterior portal, the anterior cortical wall is fenestrated with a 6.5-mm cannulated drill through the guidewire through the lateral portal under direct endoscopic visualization with an image intensifier. Then, endoscopic curettage of the fibrous inner surface is performed by inserting a small curette and forceps through the anterior or lateral portal under optimal endoscopic visualization. Finally, calcium phosphate cement (Biopex) is injected through the anterior portal with a gun-type manual cement injector under an image intensifier. During this procedure, the lateral portal is obstructed by use of a metal rod with a diameter of 6 mm.