Abstract
Purpose
Our goal was to examine the trajectory of bonding impairment across the first 6 months postpartum in the contexts of maternal risk, including maternal history of childhood abuse and neglect and postpartum psychopathology, and to test the association between self-reported bonding impairment and observed positive parenting behaviors.
Method
In a sample of women with childhood abuse and neglect (CA) histories (CA+, n=97) and a healthy control comparison group (CA-, n=53), participants completed questionnaires related to bonding with their infant at 6 weeks, 4 months, and 6 months postpartum and postpartum psychopathology at 6 months postpartum. In addition, during a 6 months postpartum home visit, mothers and infants participated in a dyadic play interaction subsequently coded for positive parenting behaviors by blinded coders.
Results
We found that all women independent of risk status increased in bonding to their infant over the first 6 months postpartum; however, women with postpartum psychopathology (depression and PTSD) showed consistently greater bonding impairment scores at all times points. Moreover, we found that at the 6 months assessment bonding impairment and observed parenting behaviors were significantly associated.
Conclusion
These results highlight the adverse effects of maternal postpartum depression and PTSD on mother-infant bonding in early postpartum in women with child abuse and neglect histories. These findings also shed light on the critical need for early detection and effective treatment of postpartum mental illness in order to prevent problematic parenting and the development of disturbed mother-infant relationships. Results support the use of the Parenting Bonding Questionnaire (PBQ) as a tool to assess parenting quality by its demonstrated association with observed parenting behaviors.
Keywords: Maternal childhood abuse and neglect history, postpartum depression, postpartum PTSD, mother-infant bonding, parenting behaviors
It is well documented that women who have been exposed to childhood maltreatment are more vulnerable to maladaptive psychosocial outcomes, and, in particular, experience more mental health problems across the lifespan (Edwards, Holden, Felitti, & Anda, 2003; Kaplow & Widom, 2007; Widom, 1999). Epidemiological studies confirm that experiencing childhood abuse and neglect is a salient risk specifically for depression and PTSD in adulthood (Edwards et al., 2003; Koenen & Widom, 2009; Widom, 1999). In addition to risk for mental health outcomes, women with childhood abuse and neglect histories are also more likely to experience poor physical health and disturbed attachment relationships (Colman & Widom, 2004; Rodgers et al., 2004).
Given that childhood maltreatment is a salient risk for maladaptive adult functioning, there is similarly strong interest in understanding whether abuse and neglect in childhood also negatively impacts adaptation to parenthood, specifically the ability to be a sensitive and responsive parent to one's child. Most research has focused on exposure to childhood sexual abuse and its ill effects on parenting, and in some studies associations were found to hold true even after controlling for other maltreatment experiences such as physical neglect or abuse (Banyard, 1997; Ruscio, 2001), whereas in others these specific associations became nonsignificant once physical neglect and abuse was added in the model (Zuravin & Fontanella, 1999). Thus, it remains equivocal whether childhood abuse per se or specific exposure to sexual abuse is more detrimental to long-term parenting functioning. During observed mother-child interactions, mothers with childhood sexual abuse histories, are more likely to be emotionally withdrawn (Lyons-Ruth & Block, 1996) or permissive (Ruscio, 2001) in their parenting practices, or demonstrate more frequently hostile caregiving behaviors and physical punishment (Banyard, 1997; Lyons-Ruth & Block, 1996, for a review see DiLillo & Damashek, 2003); subsequently children are more likely to develop disorganized attachment relationships with these mothers (Lyons-Ruth & Block, 1996). Similarly, women who have been exposed to childhood sexual abuse also express more negative views about themselves as parents (Banyard, 1997), have a less balanced perception about parenting (Burkett, 1991), show role reversal in parenting their child (Alexander, Teti, & Anderson, 2000), and have more malevolent, hostile attributions and distorted representations towards parenting (Alexander, 1992). Elucidating such relationship distortions that underlie parenting dysfunction among mothers with childhood abuse and neglect histories may be the first step towards interrupting the intergenerational association between maternal childhood maltreatment histories and poor child outcomes. Furthermore, as women with histories of trauma are at greater risk of psychopathology in adulthood, and psychopathology is known to predict less optimal parenting outcomes (Banyard, Williams, & Siegel, 2003; Lutenbacher & Hall, 1998), such an investigation of maternal parenting deficits in childhood trauma survivors needs to take maternal psychopathology into account. Prior work has explored the role of maternal depression (Roberts, O'Connor, Dunn, & Golding, 2004; Zuravin & Fontanella, 1999), anger (DiLillo, Tremblay, & Peterson, 2000), anxiety (Roberts et al., 2004) or dissociation (Kim, Trickett, & Putnam, 2010) as mediators between maternal trauma exposure and parenting practice, and findings are equivocal (see review Kim et al., 2010). Interestingly, maternal depression was not a significant mediator in a study of low-income, high-risk urban mothers suggesting that in an environment of high socioeconomic risk depression may have limited power to explain mediation (Zuravin & Fontanella, 1999). In this paper we explore the role of maternal psychopathology (depression and posttraumatic stress) and socioeconomic risk among women with childhood abuse and neglect histories and its impact on their attitudes towards parenting and the relationship with their infant.
The Postpartum Bonding Questionnaire (PBQ, Brockington et al., 2001) is a self-report questionnaire designed to assess a mother's emotional connection to her infant as well as her feelings about herself as a parent in the early weeks and months postpartum. It aims to detect maternal relational disturbances characterized by her hostility, aggression, lack of emotion, and rejection directed toward her infant (Brockington et al., 2001; Klier, 2006). The main subscales of the PBQ were found to be both valid and reliable tools for identifying such concerns through self-report (Brockington et al., 2001; Brockington, Fraser, & Wilson, 2006).
Prior studies utilizing the PBQ have linked mothers' ability to feel connected to their infants and efficacious as parents with the presence of psychopathology. The majority of this work has focused on examining the PBQ within the context of postpartum depression and has demonstrated that mothers with symptoms of depression, independent of severity, are more likely to report bonding impairment within the first few months postpartum (Ayers, Wright, & Wells, 2007; Hornstein et al., 2006; Moehler, Brunner, Wiebel, Reck, & Resch, 2006; Noorlander, Bergink, & van den Berg, 2008; Parfitt & Ayers, 2009). In addition, this line of research also indicates that these bonding impairments maintain stability across the first few weeks and months postpartum (Moehler et al., 2006).
Our review found only 2 studies that have examined postpartum bonding in mothers with trauma exposure and subsequent Posttraumatic Stress Disorder (PTSD). Ayers, Wright, and Wells (2007) reported on parent-infant bonding at 9 weeks postpartum in mothers and fathers recruited from maternity ward registers. Participants were mailed self-report questionnaires focusing on several domains of postpartum functioning, including PTSD symptoms and bonding. Bonding was assessed using a modified version of the Bethlehem Mother–Infant Interaction Scale (Pearce & Ayers, 2005). The Bethlehem scale differs from the PBQ in that questions focus on maternal report of interactions with her baby, more so than her feelings of emotional connectedness to her infant. Ayers and colleagues found that bonding was not related to posttraumatic stress symptoms. However, a more recent study conducted by Parfitt and Ayers (2009) reexamined the impact of PTSD on bonding using the PBQ measure. Utilizing on-line survey methodology, the authors oversampled for mothers who had undergone a traumatic birth experience and had infants between the ages of 1-24 months. In this study, postpartum PTSD was indeed a risk factor for bonding impairment, even more so than postpartum depression (Parfitt & Ayers, 2009). The authors suggest the conflicting results may be due to differences in measurement features (instruments and assessment time point varied) and participant risk status as the Parfitt and Ayers (2009) sample was at higher risk for psychopathology than the sample studied by Ayers et al. (2007). Moreover, both studies consider the impact of acute trauma (birth) on the developing mother-infant bond. To date, no study has been published exploring the long-term impact of past trauma, such as exposure to childhood abuse and neglect, on mother-infant bonding using the PBQ. This is particularly important as impaired mother-to-infant bonding may be a crucial early mechanism by which maternal abuse and neglect history may lead to disturbed parenting practice, which in turn, may lay the foundation for adverse child outcomes. Such adverse child outcomes, for example increased vulnerability to negative life events and poor behavioral trajectories from 4-7 years of age (Collishaw, Dunn, O'Connor, & Golding, 2007; Miranda, de la Osa, Granero, & Ezpeleta, 2011), have been reported in offspring of mothers with childhood maltreatment histories; thus, elucidation of early predictors for such adverse outcomes may guide preventive practice.
With the goals of closing these gaps in the extant literature and enhancing our current understanding of the effects of childhood maltreatment on perinatal psychopathology and mother–infant bonding, our group has recently investigated associations between child abuse and neglect histories with peripartum depression and PTSD and possible effects on maternal bonding at 6 weeks postpartum using the PBQ (Seng et al., in press). As potential risk factors we explored pre-pregnancy PTSD and depression status as well as acute, birth-related PTSD. We found the mothers' childhood maltreatment histories were associated with impaired bonding and that this link was mediated by lifetime history of PTSD, alone or comorbid with depression, but not by depression alone. Furthermore, this association of pre-pregnancy psychopathology with maternal 6-week postpartum bonding was in turn mediated by postpartum depression alone or comorbid with pre-existing PTSD. New incident (birth-related) PTSD alone was not a risk factor for impaired bonding.
The present study is a natural sequel to this previous work and aims to shed light on predictors of bonding impairment in the first 6 months postpartum in this sample of mothers overrepresented for histories of child abuse and neglect. In addition, the present paper also extends prior work such that self-rated bonding impairment is validated against the quality of observer-rated mother-infant interaction in the home.
To our knowledge, this is the first study to test unique and concurrent contributions of childhood maltreatment exposure and postpartum psychopathology on mother-infant bonding in the first 6 months postpartum. Our research questions are: 1.) What is the natural course of bonding impairment in the first six months postpartum in the context of postpartum psychopathology and childhood maltreatment history? 2.) Is mothers' perceived bonding impairment associated with observed parenting practice?
Method
The current study focuses on self-report and observed data collected from mothers when their infants were 6 weeks, 4 months, and 6 months old. Women were recruited for the Maternal Anxiety during Childbearing Years (MACY; NIMH K23 MH080147; PI: Muzik) project in one of two ways: as postpartum follow-up to a study (“the STACY project”; NIH NR008767; PI Seng) on the prenatal effects of PTSD on childbearing, when they initiated prenatal care for their first child at 14-28 weeks gestation (previously reported in Seng, Low, Sperlich, Ronis, & Liberzon, 2009), or through community advertisement at 6-8 weeks postpartum. Recruitment in prenatal care accessed potential participants through direct invitation when women presented to their initial antenatal visit at three pregnancy clinics in a large Metropolitan Area. Recruitment in the community was conducted by posting flyers in childcare centers and pediatric offices within the same catchment area. Participants were non-psychiatrically referred English-speaking women, ages 18 and older (N=150). At screening, participants were administered the Childhood Trauma Questionnaire (CTQ, Bernstein et al., 2003) via telephone interview. Those who indicated that they had experienced physical, emotional, or sexual abuse, or physical or emotional neglect before the age of 16 were placed in the childhood abuse and neglect group (CA+, n=97). Those who did not report such experiences were placed in the comparison group (CA-, n=53). Exclusion criteria included the use of illegal or non-prescription drugs during pregnancy, maternal history of bipolar and psychotic illness, child prematurity (<36 weeks term), or child developmental disability and severe illness (e.g., epilepsy). Data were collected in the years 2007-2010. Written, informed consent was obtained from all participants. The study was approved by the Institutional Review Board of the local university.
The MACY project is a longitudinal investigation of the impact of maternal childhood adversity on postpartum psychopathology, entry to motherhood, parenting beliefs and behaviors, and ultimately, on the development of the mother-child relationship and subsequent child developmental trajectories. Participants completed telephone interviews at 6 weeks, 4 months, 12 months, and 18 months postpartum, two home visits at 6 months postpartum, and a playroom visit at 15 months postpartum. Data collected during study interviews and visits include maternal history of childhood abuse and neglect, maternal mental health, mother-infant bonding, parenting assessments including video-taped dyadic observations, and infant and child biological and socio-emotional outcomes. For this manuscript, we narrowed the investigation to maternal abuse and neglect history and postpartum psychopathology, mothers' self-rated bonding, and observed parenting competence, all collected within the first 6 months postpartum.
Sample
One hundred and fifty mother-infant dyads participated in the current study, and maternal age ranged from 18-45 with an average age of 29.00 (SD: 5.66). The majority of the sample was Caucasian (67%) and African-American (19%). On average, participants reported an annual household income of $55,000-59,000 per year. Eighty percent of the participants reported being in a romantic relationship, and 59% completed at least a bachelor's degree. Participant demographic data is presented for each group: CA+ (n=97) and CA+ (n=53). Chi-square and independent sample t-test analyses revealed that there were no significant differences in demographic information for either group. See Table 1.
Table 1. Participant Demographics.
| Characteristics | CA+ | CA- | Sig. Difference |
|---|---|---|---|
| Category | (n=97) | (n=53) | |
| M (SD) or % (n) | M (SD) or % (n) | t-test/χ2 | |
| Mother Age | 29.26 (5.93) | 28.3 (5.15) | ns |
| Education | ns | ||
| ≤ High School Degree | 14.4 (14) | 15.1 (8) | |
| > High School Degree | 85.6 (83) | 84.9 (45) | |
| Race | ns | ||
| Caucasian | 66.0 (64) | 69.8 (37) | |
| African-American | 17.5 (17) | 20.8 (11) | |
| Latina | 5.2 (5) | 0 (0) | |
| Asian/Pacific Islander | 7.2 (7) | 1.9 (1) | |
| Other | 4.2 (4) | 7.6 (4) | |
| Annual Household Income | ns | ||
| < $25,000 | 26.8 (26) | 29.4 (15) | |
| $25,000 - $49,999 | 20.6 (20) | 15.7 (8) | |
| ≥ $50,000 | 52.6 (51) | 54.9 (28) | |
| Partner Status | ns | ||
| Partnered | 80.4 (78) | 79.2 (42) | |
| Not Partnered | 19.6 (19) | 20.8 (11) | |
| Depression Diagnosis | p=.017 | ||
| Depression | 25.8 (25) | 9.4 (5) | |
| No depression | 74.2 (72) | 90.6 (48) | |
| Depression Symptom Count | p=.002 | ||
| 67.11 | 55.45 | ||
| (23.07) | (17.84) | ||
| PTSD Diagnosis | p=.000 | ||
| PTSD | 33.0 (32) | 94.3 (50) | |
| No PTSD | 67.0 (65) | 5.7 (3) | |
| PTSD Symptom Count | p=.000 | ||
| 5.49 (4.35) | 1.78 (3.20) | ||
| Comorbid Depression and PTSD | p=.010 | ||
| Comorbid Diagnosis | 15.5 (15) | 1.9 (1) | |
| No Comorbidity | 84.5 (82) | 98.1 (52) |
Note: “Partnered” refers to participants who are in a relationship with a partner.
Due to the nature of inclusion criteria (oversampling for childhood trauma exposure), rates of postpartum depression and PTSD are higher for participants in the current sample as compared to the general population. Participants in the CA+ group were significantly more likely than the CA- group to have depression, PTSD, and comorbid diagnoses at 6 months postpartum. For a full summary of symptomatology in CA+ and CA- groups, see Table 1.
Measures
Demographics
Maternal demographic information was collected at the baseline phone call (either 6 weeks or 4 months postpartum) and updated at each subsequent data collection time point. The demographic questionnaire yields variables describing yearly household income, maternal race, age, years of education, and marital relationship. A cumulative demographic risk variable was computed based on five variables: income risk (less than $20,000 per year), minority status, age (< 22), education (≤ high school), and partner status (not partnered). These variables were dummy coded into dichotomous variables and summed. Therefore, this variable is an index of the number of risks present (ranging 0-5). This coding scheme is similar to those used in other research on maternal risk and parenting (Sameroff, Seifer, Baldwin, & Baldwin, 1993). Fifty-two percent of the sample had zero risks present, and there were no significant differences on this measure for CA+ compared to CA-.
Mother-Infant Bonding
The Postpartum Bonding Questionnaire (PBQ) is a 25-item scale assessing the mother's feelings or attitudes towards her infant (e.g. “I feel close to my baby”, “my baby irritates me”), and yields a total score and 4 domain scores (impairment, rejection/anger, infant-focused anxiety, and risk of infant abuse). The scale was administered at 4 months postpartum (over the phone) and during a home visit at 6 months postpartum (in person). Participants rate agreement with statements on a 6-point Likert scale ranging from “never” to “always,” and higher scores reflect greater bonding impairment. The original instrument has 25-items with 2 questions tapping into risk of infant abuse; however, based on previously reported poor psychometric properties (Brockington et al., 2006) and the potential to emotionally upset mothers, we chose to omit the 2 questions in this study that pertain to that subscale. Prior work has demonstrated the reliability and validity of the remaining domains of the PBQ (Brockington et al., 2001, 2006). For this study we computed a PBQ total problem score (sum of all 23 items on the measure) as an indicator of problematic cognitions regarding parenting and the infant. Reliability is excellent in the overall MACY study (α=.85 at 6 weeks, α=.88 at 4 months; α=.83 at 6 months).
Maternal Trauma and Psychopathology
Maternal childhood trauma was assessed during a phone interview at study recruitment using the Childhood Trauma Questionnaire (CTQ, Bernstein et al., 2003). The CTQ is a 28-item self-report questionnaire that assesses five types of maltreatment –emotional abuse, physical abuse, sexual abuse, and emotional and physical neglect. Response ratings range from 1=‘never’ to 5=‘very often true’. This measure demonstrates excellent reliability in the current study (α=.92) as well as good construct validity (correlation with PTSD symptom count at 4 months, r=.56, p=.00; correlation with PTSD symptom count at 6 months, r=.53, p=.00). We note that the CTQ has been successfully used in other studies via telephone interview (Pederson et al., 2004; Thombs et al., 2007).
Maternal PTSD was measured using the National Women's Study (NWS, Resnick, Kilpatrick, Dansky, Saunders, & Best, 1993) PTSD Module. In the current study we utilize data from the 6-month timepoint. NWS-PTSD is a structured telephone diagnostic interview designed to be administered by lay interviewers, with a sensitivity of 0.99 and specificity of 0.79 to detect PTSD diagnosis. The measure yields a dichotomous diagnosis based on DSM-IV criteria, and a dimensional symptom count on a scale of 0 to 17. In the current study, we use symptom count for descriptive analyses, and we use diagnosis as the main variable of interest in the models responding to the research questions.
Maternal depression was inventoried using the Postpartum Depression Screening Scale (PPDS; Beck & Gable, 2000). In the current study we utilize data from the 6-month timepoint. The PPDS is a 35 item self-report questionnaire answered on a Likert scale ranging from 1-5. It yields a total symptom count and a diagnosis of major depressive disorder as indicated by a total symptom count > 80 (Beck and Gable 2000). The PPDS has sensitivity of 0.78, specificity of 0.99 and positive predictive value of 0.93 compared with a SCID diagnosis of depression. In the current study, we use symptom count for descriptive analyses, and we use diagnosis as the main variable of interest in the models responding to the research questions.
Observed Maternal Behaviors
Maternal positive parenting behaviors were obtained at 6 months postpartum during a 10-minute in-home, free play segment. Mothers were asked to play with their infants, ‘as you normally would’. The video segments were coded for maternal behaviors by trained and reliable coders utilizing the MACY Infant-Parent Coding System (Earls, Beeghly, & Muzik, 2009; modified from previous published mother-infant coding system, Miller, McDonough, Rosenblum, & Sameroff, 2002). The 10-minute interaction was scored in four 2 1/2 minute intervals on multiple global dimensions tapping into quality of maternal parenting behavior; to obtain one summary score for each dimension the 4 scores across 10 minutes were averaged. A small subset of participants (9.52%) only provided 5 minutes of interactive footage, thus we averaged across two episodes for a summary score. Trained coders masked to maternal trauma history and other study variables independently scored 40 randomly selected videotapes, inter-coder reliability was established with intra-class correlations (ICC). In the present study we derived based on a conceptually driven data reduction analysis (principal-components factor analysis), a maternal positive parenting composite score by averaging scores from five interrelated domains coded from the free play footage: Maternal Behavioral Sensitivity/Supportive Presence, Engagement, Warmth, Affective Sensitivity, and Flexibility. The standardized Cronbach's alpha for the positive parenting composite during free play was .92. The ICC for the scales was as follows: Behavioral Sensitivity/Supportive Presence (ICC = .85); Engagement (ICC = .86); Warmth (ICC = .84); Affective Sensitivity (ICC = .86); and Flexibility (ICC=.77).
Missing Data
Respondents were included in the current study if they had complete data for the Postpartum Bonding Questionnaire at the 6 month timepoint. Among these participants (N=150), participants had complete data on the PBQ at the 4 month timepoint, the observed positive parenting behaviors at 6 months, the PTSD assessment at 6 months, and the demographic risk index. Six percent of respondents were missing data for the depression measure at 6 months, 9% were missing data for the CTQ, and 37% were missing data for the PBQ at 6 weeks. Attrition analyses demonstrated that patterns of missingness were not dependent on maternal MDD or PTSD diagnoses or bonding impairment; data were determined to be missing at random (MAR). We imputed data using the expectation maximization (EM) algorithm, a maximum likelihood approach (Dempster, Laird, & Rubin, 1977).
Results
Descriptive analyses conducted in SPSS 20.0 demonstrate that mothers in the CA+ group reported significantly more bonding problems (t=-2.74, p=.01) and postpartum psychopathology (depression: t=-3.44, p=.00; PTSD: t=-5.97, p=.00) compared to CA- group by 6 months postpartum. We used Repeated Measures Analysis of Variance via SPSS 20.0 and Structural Equation Modeling via LISREL 8.80 to respond to the research questions: 1) What is the natural course of bonding impairment in the first six months postpartum in the context of psychopathology and childhood maltreatment history? 2) Is mothers' perceived bonding impairment associated with observed parenting practice?
What is the natural course of bonding impairment in the first six months postpartum in the context of psychopathology and childhood maltreatment history?
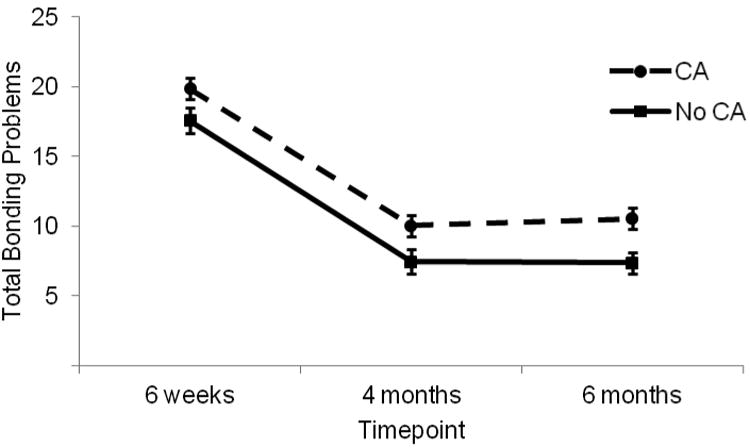
We respond to this question with Repeated Measures Analysis of Variance, examining differential trajectories of bonding impairment across the first 6 months postpartum for the total sample and: 1) women with (n=30) and without (n=120) Major Depressive Disorder (MDD) diagnoses and 2) women with (n=35) and without (n=115) Posttraumatic Stress Disorder (PTSD) diagnoses. In both models we controlled for the presence of childhood maltreatment histories and cumulative risk. Analyses demonstrate significant change in bonding impairment scores over time, modeled first with depression, child abuse and neglect history, and cumulative risk as predictors (F=57.06, p=.00, np2=44; see Figure 1) and subsequently modeled with PTSD, child abuse and neglect history and cumulative risk as predictors (F=65.88, p=.00, np2=48; see Figure 2). Generally, mothers report improved bonding over time. Results show non-significant interaction effects of PBQ scores over time with depression, PTSD, or child maltreatment history. However, there are significant main effects for both depression (F=7.49, p=.01, np2=05) and PTSD (F=4.71, p=.03, np2=03). Child abuse and neglect history demonstrates a significant main effect when modeled with depression (F=4.34, p=.04, np2=.03; see Figure 3) but not when modeled with PTSD. Cumulative risk does not demonstrate significant main or interaction effects in either model. These results indicate that bonding impairment generally improves over time in our sample. In addition, women with psychopathology are more likely across time to experience greater bonding impairment with their infants. Furthermore, mothers with childhood maltreatment histories are more likely to experience impaired bonding over time when controlling for the effects of depression but not when controlling for the effects of PTSD.
Figure 1. Bonding Impairment Across Early Postpartum by Maternal Depression Status.
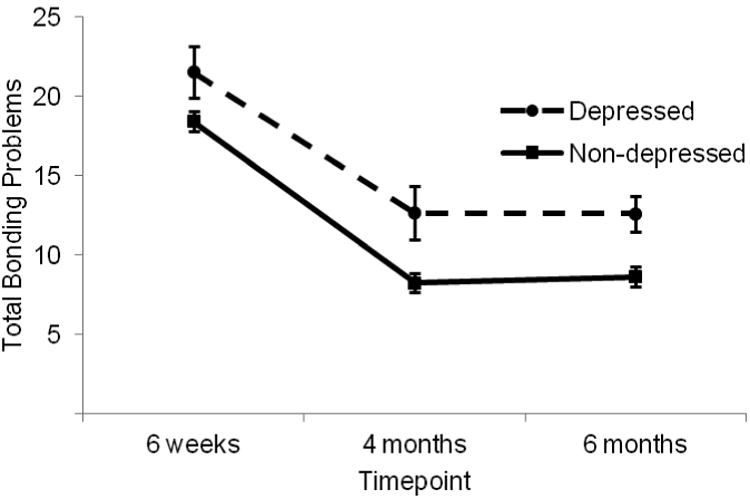
Figure 2. Bonding Impairment Across Early Postpartum by Maternal PTSD Status.
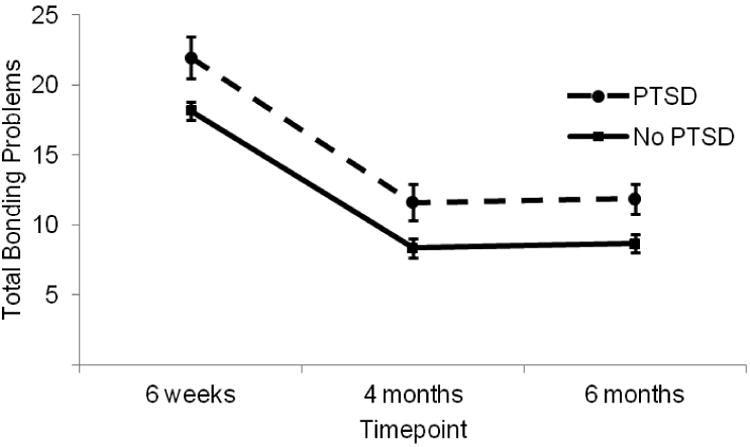
Figure 3. Bonding Impairment Across Early Postpartum by Child Maltreatment History.
Is bonding impairment associated with parenting behavior?
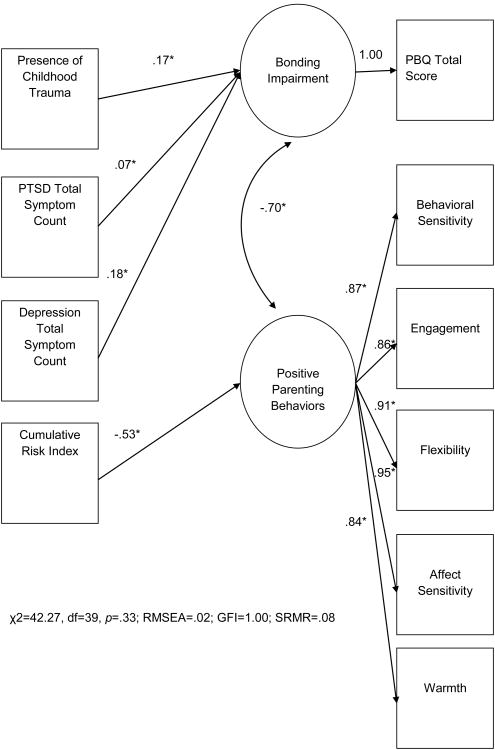
Given the significant change over time in bonding impairment during the first 6 months, we explored the association between self-rated bonding impairment and observed parenting outcomes at the final timepoint (6 months). We employed structural equation modeling (SEM) via LISREL 8.80 to test the covariance between maternal self-reported bonding impairment and the observer-rated positive parenting behaviors (see Figure 4). Control variables (PTSD and depression diagnoses, presence of child maltreatment history, and cumulative risk) were initially freed to predict throughout the model; the final model (Figure 4) presents only the significant paths between control variables and endogenous factors to support the best fitting model. Model fit is excellent (χ2=42.27, df=39, p=33; RMSEA=02; GFI=1.00; SRMR=.08), and there is a significant association between maternal bonding impairment and observed parenting behavior (β=-.70). This final model explains a moderate amount of variance in the latent factor representing observed positive parenting behaviors (R2=.28), and demonstrates a strong association between self-reported bonding impairment and observed positive parenting behaviors, controlling for risk factors related to psychopathology, demographics, and trauma history.
Figure 4.
Association of self-reported bonding impairment and observed positive parenting behaviors at 6 months postpartum.
Discussion
We aimed in the present study to examine the natural course of bonding in a sample of women overselected for histories of child abuse and neglect, and we aimed to explore the role that psychopathology and childhood maltreatment history, as well as socioeconomic risk, play in shaping bonding over time. In addition, analyses tested whether bonding impairment was associated with observed maternal parenting behaviors during dyadic interactions. Taken together, our results confirm that bonding problems normatively improve over time in the first six months postpartum but continue to be predicted by psychopathology and a history of childhood trauma and demonstrate a robust relationship by the end of the first 6 months with parenting behaviors.
Childhood abuse and neglect history was observed to increase the risk for perinatal depression and PTSD, and the presence of this history predicts increased bonding impairment over time when controlling for depression and socioeconomic risk. However, childhood maltreatment history does not continue to be a significant predictor of impaired bonding when modeled with the pathology resulting from trauma, PTSD. Therefore, the present study results suggest that it is psychopathology, and not the maltreatment history per se or current psychosocial risk, that conveys the greatest risk for bonding disturbance. Furthermore, results show that both depression and PTSD put mothers at risk for bonding problems across the first 6 months. However, it is important to note that bonding impairment improved over time for all groups, even the women with psychopathology and maltreatment risk; this may indicate a normative proneness towards a close relational bond between mothers and infants in early postpartum independent of emotional disturbance.
This study joins a strong body of research that identifies depressive symptoms as a potent risk factor for many facets of postpartum functioning, including the parent-infant bond (Hornstein et al., 2006; Klier, 2006; Moehler et al., 2006; Noorlander et al., 2008). From a clinical perspective, it seems likely that the common symptoms of depression, including anhedonia, withdrawal, and amotivation interfere with the maternal propensity to form an affectively strong, engaged stance towards the infant. The co-occurrence of depression and bonding impairment underscores the importance of addressing both in interventions; indeed, recent research suggests that simply targeting depression may not be sufficient to improve parent-child relational outcomes (Forman et al., 2007; Muzik, Marcus, & Flynn, 2009).
Surprisingly, and in contrast to the findings by Zuravin & Fontanella (1999), who found socioeconomic risk to mediate the relation between childhood trauma exposure and later parenting quality, the we did not find any contribution of cumulative demographic risk on bonding impairment. The most parsimonious explanation for this differential finding is that our sample impresses with lower socioeconomic risk compared to the sample of Zuravin & Fontanella (1999).
The role of maternal PTSD for bonding disturbance is less well understood with inconsistent findings in prior studies (Ayers et al., 2007; Parfitt & Ayers, 2009). Parfitt and Ayers (2009) utilized a sample of women overselected for birth trauma, and demonstrated that an acute stressor and PTSD may be more likely to result in immediate impairment in postpartum bonding. The current study indicates that PTSD puts mothers and their infants at risk for impaired bonding across the first six months postpartum. The present research considers the impact of trauma from years past and its long-term impact on postpartum psychopathology, and may in fact highlight the impact of chronic trauma symptoms, rather than the impact of acute trauma. We note that symptoms of PTSD may be more inconsistent in their presence and impact, perhaps thus explaining the less consistent research findings. Clearly, continued work identifying the role of PTSD, and its impact both alone and as a comorbid condition, is warranted.
Our second set of analyses demonstrates the significant relationship at 6 months postpartum between women's self-reports of bonding impairment and observers' ratings of positive parenting behaviors, controlling for psychopathology and demographic risks. This is the first study to test the utility of the PBQ as a possible screening tool to detect parenting behavior problems. Our results support the use of the PBQ, showing that women's perceptions of their relationships are closely tied to demonstrable behaviors during play with their infants. Thus, we show that women who score high on the bonding impairment scale at 6 months postpartum also show deficits in positive parenting behaviors such as low behavioral and affective sensitivity, low warmth, low engagement and flexibility. Furthermore, these results indicate the important interrelationship between mothers' sense of being bonded to their babies and their parenting, an important pathway to outcomes for both mothers and children. In our own previous work using longitudinal data from the MACY sample we have found that mother-infant bonding impairment in early postpartum together with disturbed infant sleep at 4 months postpartum predicted higher rates of child behavioral problems in toddlerhood (Hairston et al., 2011). Clearly, targeting maternal bonding disturbance early on and foster healthy mother-infant relationships has the potential to prevent subsequent poor child outcomes.
Limitations
Limitations related to generalizability of this study include the overrepresentation of adult survivors of childhood abuse and neglect; these results may not be generalizable to samples of women with trauma experiences other than childhood abuse and neglect (e.g., PTSD resultant from current domestic violence or birth trauma). Furthermore, sample participants indicate moderate socioeconomic status and relatively low demographic risk, suggesting these results should be further studied among low SES participants to improve their relevance. In the current study we did not extend analysis of bonding beyond the 6 month postpartum period; future work might explore the natural course of bonding problems across the first year postpartum, with special attention to identifying whether trajectories of psychopathology and bonding disturbance follow a similar course, or whether improvements in one are associated with shifts in the other. Experimental study with interventions targeting psychopathology alone, bonding alone, or both in combination may help elucidate causal pathways, and may also inform the development of targeted treatment protocols.
Conclusion
In concordance with prior literature, the present study confirms that childhood exposure to abuse and neglect is related to several maladaptive outcomes during motherhood, including increased risk for postnatal psychopathology, which in turn is related to a higher likelihood of bonding impairment. Furthermore, bonding problems appear to be related to parenting behaviors during mother-infant interactions, suggesting the PBQ is a valid measure of parenting. Taken together these results suggest that it may be crucial to address maternal psychopathology and bonding impairments early in the postpartum in order to ameliorate the mother-infant relationship risk across time. It is clear that the group of postpartum women with their own histories of childhood maltreatment should be given special consideration and care because of their increased propensity for developing psychopathology in the postpartum, as should the role such psychiatric disturbance may have for the emerging parent-infant bond (Widom, 1999).
Acknowledgments
Support for this research or manuscript preparation was provided by grants from the National Institute of Mental Health and Eunice Kennedy Shriver National Institute of Child Health and Human Development (MH080147; PI: Muzik) and the Michigan Institute for Clinical and Health Research (MICHR) at the University of Michigan (UL1RR024986; PI: Muzik). The authors wish to thank the mothers and children who made this research possible and gratefully acknowledge the valuable research assistance of Ellen Waxler, Amanda Fezzey, Heather Cameron, Rena Menke, Alexi Wisher, Lauren Earls, Lori Stark, Ryan Hill and Kayla Frick.
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- Alexander PC. Application of attachment theory to the study of sexual abuse. Journal of Consulting and Clinical Psychology. 1992;60(2):185–195. doi: 10.1037//0022-006x.60.2.185. [DOI] [PubMed] [Google Scholar]
- Alexander PC, Teti L, Anderson CL. Childhood sexual abuse history and role reversal in parenting. Child Abuse & Neglect. 2000;24(6):829–838. doi: 10.1016/s0145-2134(00)00142-3. [DOI] [PubMed] [Google Scholar]
- Ayers S, Wright DB, Wells N. Symptoms of post-traumatic stress disorder in couples after birth: Association with the couple's relationship and parent-baby bond. Journal of Reproductive and Infant Psychology. 2007;25(1):40–50. doi: 10.1080/02646830601117175. [DOI] [Google Scholar]
- Banyard VL. The impact of childhood sexual abuse and family functioning on four dimensions of women's later parenting. Child Abuse & Neglect. 1997;21(11):1095–1107. doi: 10.1016/S0145-2134(97)00068-9. [DOI] [PubMed] [Google Scholar]
- Banyard VL, Williams LM, Siegel JA. The impact of complex trauma and depression on parenting: an exploration of mediating risk and protective factors. Child Maltreatment. 2003;8(4):334–349. doi: 10.1177/1077559503257106. [DOI] [PubMed] [Google Scholar]
- Beck CT, Gable RK. Postpartum Depression Screening Scale: Development and psychometric testing. Nursing Research. 2000;49(5):272–282. doi: 10.1097/00006199-200009000-00006. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect. 2003;27(2):169–190. doi: 10.1016/S0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Brockington IF, Fraser C, Wilson D. The Postpartum Bonding Questionnaire: a validation. Archives of Women's Mental Health. 2006;9(5):233–242. doi: 10.1007/s00737-006-0132-1. [DOI] [PubMed] [Google Scholar]
- Brockington IF, Oates J, George S, Turner D, Vostanis P, Sullivan M, Loh C, et al. A Screening Questionnaire for mother-infant bonding disorders. Archives of Women's Mental Health. 2001;3(4):133–140. doi: 10.1007/s007370170010. [DOI] [Google Scholar]
- Burkett LP. Parenting behaviors of women who were sexually abused as children in their families of origin. Family Process. 1991;30(4):421–434. doi: 10.1111/j.1545-5300.1991.00421.x. [DOI] [PubMed] [Google Scholar]
- Collishaw S, Dunn J, O'Connor TG, Golding J. Maternal childhood abuse and offspring adjustment over time. Development and Psychopathology. 2007;19(2):367–383. doi: 10.1017/S0954579407070186. [DOI] [PubMed] [Google Scholar]
- Colman RA, Widom CS. Childhood abuse and neglect and adult intimate relationships: A prospective study. Child Abuse & Neglect. 2004;28(11):1133–1151. doi: 10.1016/j.chiabu.2004.02.005. [DOI] [PubMed] [Google Scholar]
- Dempster AP, Laird NM, Rubin DB. Maximum Likelihood from Incomplete Data via the EM Algorithm. Journal of the Royal Statistical Society Series B (Methodological) 1977;39(1):1–38. [Google Scholar]
- DiLillo D, Tremblay GC, Peterson L. Linking childhood sexual abuse and abusive parenting: the mediating role of maternal anger. Child Abuse & Neglect. 2000;24(6):767–779. doi: 10.1016/s0145-2134(00)00138-1. [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the Adverse Childhood Experiences study. The American Journal of Psychiatry. 2003;160(8):1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Forman DR, O'Hara MW, Stuart S, Gorman LL, Larsen KE, Coy KC. Effective treatment for postpartum depression is not sufficient to improve the developing mother-child relationship. Development and Psychopathology. 2007;19(2):585–602. doi: 10.1017/S0954579407070289. [DOI] [PubMed] [Google Scholar]
- Hairston IS, Waxler E, Seng JS, Fezzey AG, Rosenblum KL, Muzik M. The role of infant sleep in intergenerational transmission of trauma. Sleep: Journal of Sleep and Sleep Disorders Research. 2011;34(10):1373–1383. doi: 10.5665/SLEEP.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornstein C, Trautmann-Villalba P, Hohm E, Rave E, Wortmann-Fleischer S, Schwarz M. Maternal bond and mother-child interaction in severe postpartum psychiatric disorders: Is there a link? Archives of Women's Mental Health. 2006;9(5):279–284. doi: 10.1007/s00737-006-0148-6. [DOI] [PubMed] [Google Scholar]
- Kaplow JB, Widom CS. Age of onset of child maltreatment predicts long-term mental health outcomes. Journal of Abnormal Psychology. 2007;116(1):176–187. doi: 10.1037/0021-843X.116.1.176. [DOI] [PubMed] [Google Scholar]
- Kim K, Trickett PK, Putnam FW. Childhood experiences of sexual abuse and later parenting practices among non-offending mothers of sexually abused and comparison girls. Child Abuse & Neglect. 2010;34(8):610–622. doi: 10.1016/j.chiabu.2010.01.007. [DOI] [PubMed] [Google Scholar]
- Klier CM. Mother-infant bonding disorders in patients with postnatal depression: The Postpartum Bonding Questionnaire in clinical practice. Archives of Women's Mental Health. 2006;9(5):289–291. doi: 10.1007/s00737-006-0150-z. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Widom CS. A prospective study of sex differences in the lifetime risk of posttraumatic stress disorder among abused and neglected children grown up. Journal of Traumatic Stress. 2009;22(6):566–574. doi: 10.1002/jts.20478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutenbacher M, Hall LA. The effects of maternal psychosocial factors on parenting attitudes of low-income, single mothers with young children. Nursing research. 1998;47(1):25–34. doi: 10.1097/00006199-199801000-00006. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Block D. The disturbed caregiving system: Relations among childhood trauma, maternal caregiving, and infant affect and attachment. Infant Mental Health Journal. 1996;17(3):257–275. doi: 10.1002/(SICI)1097-0355(199623)17:3<257::AID-IMHJ5>3.0.CO;2-L. [DOI] [Google Scholar]
- Miller AL, McDonough SC, Rosenblum KL, Sameroff AJ. Emotion regulation in context: Situational effects on infant and caregiver behavior. Infancy. 2002;3(4):403–433. doi: 10.1207/S15327078IN0304_01. [DOI] [Google Scholar]
- Miranda JK, de la Osa N, Granero R, Ezpeleta L. Maternal experiences of childhood abuse and intimate partner violence: Psychopathology and functional impairment in clinical children and adolescents. Child Abuse & Neglect. 2011;35(9):700–711. doi: 10.1016/j.chiabu.2011.05.008. [DOI] [PubMed] [Google Scholar]
- Moehler E, Brunner R, Wiebel A, Reck C, Resch F. Maternal depressive symptoms in the postnatal period are associated with long-term impairment of mother-child bonding. Archives of Women's Mental Health. 2006;9(5):273–278. doi: 10.1007/s00737-006-0149-5. [DOI] [PubMed] [Google Scholar]
- Muzik M, Marcus SM, Flynn HA. Psychotherapeutic treatment options for perinatal depression: emphasis on maternal-infant dyadic outcomes. The Journal of Clinical Psychiatry. 2009;70(9):1318–1319. doi: 10.4088/JCP.09com05451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noorlander Y, Bergink V, van den Berg MP. Perceived and observed mother-child interaction at time of hospitalization and release in postpartum depression and psychosis. Archives of Women's Mental Health. 2008;11(1):49–56. doi: 10.1007/s00737-008-0217-0. [DOI] [PubMed] [Google Scholar]
- Parfitt YM, Ayers S. The effect of post-natal symptoms of post-traumatic stress and depression on the couple's relationship and parent-baby bond. Journal of Reproductive and Infant Psychology. 2009;27(2):127–142. doi: 10.1080/02646830802350831. [DOI] [Google Scholar]
- Pearce H, Ayers S. The expected child versus the actual child: implications for the mother-baby bond. Journal of Reproductive and Infant Psychology. 2005;23(1):89–102. doi: 10.1080/0264683042000325528. [DOI] [Google Scholar]
- Pederson CL, Maurer SH, Kaminski PL, Zander KA, Peters CM, Stokes-Crowe LA, Osborn RE. Hippocampal volume and memory performance in a community-based sample of women with posttraumatic stress disorder secondary to child abuse. Journal of Traumatic Stress. 2004;17(1):37–40. doi: 10.1023/B:JOTS.0000014674.84517.46. [DOI] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology. 1993;61(6):984–991. doi: 10.1037/0022-006X.61.6.984. [DOI] [PubMed] [Google Scholar]
- Roberts R, O'Connor T, Dunn J, Golding J. The effects of child sexual abuse in later family life; mental health, parenting and adjustment of offspring. Child Abuse & Neglect. 2004;28(5):525–545. doi: 10.1016/j.chiabu.2003.07.006. [DOI] [PubMed] [Google Scholar]
- Rodgers CS, Lang AJ, Laffaye C, Satz LE, Dresselhaus TR, Stein MB. The impact of individual forms of childhood maltreatment on health behavior. Child Abuse & Neglect. 2004;28(5):575–586. doi: 10.1016/j.chiabu.2004.01.002. [DOI] [PubMed] [Google Scholar]
- Ruscio AM. Predicting the child-rearing practices of mothers sexually abused in childhood. Child Abuse & Neglect. 2001;25(3):369–387. doi: 10.1016/s0145-2134(00)00252-0. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ, Seifer R, Baldwin A, Baldwin C. Stability of intelligence from preschool to adolescence: the influence of social and family risk factors. Child Development. 1993;64(1):80–97. doi: 10.1111/j.1467-8624.1993.tb02896.x. [DOI] [PubMed] [Google Scholar]
- Seng JS, Low LMK, Sperlich M, Ronis DL, Liberzon I. Prevalence, trauma history, and risk for posttraumatic stress disorder among nulliparous women in maternity care. Obstetrics and Gynecology. 2009;114(4):839–847. doi: 10.1097/AOG.0b013e3181b8f8a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng JS, Sperlich M, Low LK, Ronis DL, Muzik M, Liberzon I. Childhood abuse history, posttraumatic stress disorder, postpartum mental health and bonding: A prospective cohort study. Journal of Midwifery & Women's Health. doi: 10.1111/j.1542-2011.2012.00237.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thombs BD, Bennett W, Ziegelstein RC, Bernstein DP, Scher CD, Forde DR. Cultural sensitivity in screening adults for a history of childhood abuse: Evidence from a community sample. Journal of General Internal Medicine. 2007;22(3):368–373. doi: 10.1007/s11606-006-0026-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widom CS. Posttraumatic stress disorder in abused and neglected children grown up. The American Journal of Psychiatry. 1999;156(8):1223–1229. doi: 10.1176/ajp.156.8.1223. [DOI] [PubMed] [Google Scholar]
- Zuravin SJ, Fontanella C. Parenting behaviors and perceived parenting competence of child sexual abuse survivors. Child Abuse & Neglect. 1999;23(7):623–632. doi: 10.1016/s0145-2134(99)00045-9. [DOI] [PubMed] [Google Scholar]