Abstract
Background
There is a high incidence of falls in older adults with knee osteoarthritis (OA). Adequate dynamic balance and mobility reduce the risk of falls; however, there are currently no validated, advanced tests of dynamic balance and mobility for individuals with knee OA.
Objective
The purpose of this study was to determine the convergent validity, known-groups validity, and test-retest reliability of a dynamic test of balance and mobility, the Community Balance and Mobility Scale (CB&M), in a knee OA population.
Design
A cross-sectional design was used.
Methods
Twenty-five individuals aged 50 years and older with medial knee OA and an equal number of healthy controls completed the CB&M and other tests of balance and mobility, including the Berg Balance Scale, the Timed “Up & Go” Test, a test of maximal single-leg stance time, and the 10-Meter Walk Test (self-selected and fast walking speed). Convergent validity of balance tests with the CB&M was assessed using Pearson product moment correlation coefficients, and known-groups validity was assessed using independent t tests. Test-retest reliability of the CB&M was assessed using intraclass correlation coefficients (ICCs) and standard error of measurement (SEM).
Results
Scores on the CB&M were significantly correlated with all measures of balance and mobility for those with knee OA. There were significant differences in CB&M scores between groups. Scores on the CB&M were highly reliable in people with knee OA (ICC=.95, 95% confidence interval [95% CI]=0.70 to 0.99; SEM=3, 95% CI=2.68 to 4.67).
Limitations
Few participants had severe knee OA.
Conclusions
The CB&M displayed moderate convergent validity, excellent known-groups validity, and high test-retest reliability. The CB&M can be used as a valid and reliable tool to assess dynamic balance and mobility deficits in people with knee OA.
Falls in elderly people are a significant public health concern. In one sample of more than 5,000 adults aged 65 years and older, more than 25% reported experiencing a fall in the previous year, and two-thirds of those who fell were injured by the fall.1 The risk of mortality increases significantly with an increased frequency of falling.2 Previous studies have highlighted a particularly high prevalence of falls (>50%) in samples of elderly individuals with osteoarthritis (OA).3–5 Compounding this finding is a greater fear of falls in individuals with knee OA compared with healthy controls.3
Balance is a key element of function that allows individuals to maintain posture and respond to perturbations.6 Furthermore, sufficient mobility, often defined as the capacity to ambulate, also is needed to navigate or avoid obstacles and is intrinsically related to independent living.7 Importantly, older adults with mild mobility impairment are at a high risk for falls,7 and exercise interventions that improve mobility can reduce the risk of falling.8,9 These studies are suggestive of the important role of balance and mobility in reducing the prevalence and risk of falls. Both adequate mobility and balance are needed in order to ambulate independently in the community.
Several outcome measures—such as functional reach tests,10 measures of single-leg stance time,11,12 and single-leg11,13 or double-leg14–16 static standing tests that assess variations in center of pressure (COP)—have been used to evaluate static standing balance in people with knee OA. However, dynamic balance (defined as locomotor stability during movement17) is a key component of function that is necessary for activities such as walking and changing direction, and such static outcome measures may not adequately evaluate the dynamic balance and mobility necessary for ambulation and independent living.
Measures of dynamic balance and function, such as the Berg Balance Scale (BBS), the Timed “Up & Go” Test (TUG), and measures of gait speed, have been used previously to assess dynamic balance and mobility. Clinically, the BBS has been widely used to assess balance and mobility in many populations, including elderly people who are healthy and those with knee OA.18–20 However, it has been shown that the BBS has a ceiling effect in individuals who can ambulate independently in the community, including those with mild knee OA.20,21 For example, Kim et al20 found that all healthy older adults who they tested (n=40) had the maximum score of 56 on the BBS, with a similar mean score for those with mild knee OA (54.6/56). The high scores in both healthy and patient populations make identification of individuals in need of further treatment difficult when using the BBS. The TUG has been used frequently as a valid measure of mobility in both healthy individuals and those with knee OA,20,22 and gait speed also is often evaluated as a measure of lower limb physical function and mobility.22–24 Measures of gait speed are valid and reliable22 and can discriminate among different levels of function.24 However, the TUG and measures of gait speed are single measures of mobility that do not assess the balance needed during different tasks to ambulate in the community independently. A dynamic test of both balance and mobility is needed to better assess functioning and balance in people with knee OA.
The Community Balance and Mobility Scale (CB&M) was developed to assess community-level functional deficits in both dynamic balance and mobility.25 This scale was designed to assess advanced balance and mobility activities such as rapid direction changes and dual tasking, originally in young patients after traumatic brain injury (TBI). Importantly, the CB&M has been validated in healthy individuals26 and other patient populations, including TBI25 and stroke,27 to accurately assess dynamic balance and mobility. The CB&M is sensitive to change27 and does not suffer from ceiling effects commonly seen when using other tools such as the BBS and TUG to assess balance and mobility.26,27 The validity and reliability of the CB&M in people with knee OA need to be assessed to determine whether the CB&M can be used to evaluate balance and mobility deficits in the knee OA population to permit focused balance rehabilitation. Therefore, the purpose of this study was to examine the convergent and known-groups validity and test- retest reliability of the CB&M in older adults with knee OA. Reliability values for other tests of balance and mobility are presented for comparison.
Method
Participants
Individuals aged 50 years and older, with and without knee OA, were recruited from the local community using print advertisements and a laboratory database of previous study participants. Presence or absence of knee OA was confirmed with radiographs (see below). Included participants were assigned to 1 of 2 groups: (1) a knee OA group (n=25) or a control (no knee OA) group (n=25) based on radiographic and pain findings. Exclusion criteria for the knee OA group were: articular cartilage degradation in the lateral tibiofemoral compartment greater than in the medial tibiofemoral compartment, an inflammatory arthritic condition, a history of previous lower extremity joint replacement surgery (including hip or knee replacement), or recent (within 6 months) arthroscopic knee surgery. Exclusion criteria for the control group were: any knee pain, any evidence of knee OA on radiographs, and other musculoskeletal abnormality that would affect balance and mobility. Written informed consent was provided by all participants.
Procedure
Interested participants were screened by a study coordinator, and those eligible were referred for radiographic investigation. Evidence of knee OA was determined using the Kellgren and Lawrence (KL)28 rating scale, with knee OA defined as definite osteophytes (minimum KL rating of 2). Participants in the control group had to have a KL rating of 0 or 1 (no OA). Individuals with knee OA were tested on 2 occasions within 2 weeks, whereas controls were assessed in a single testing session only. Participant characteristics that were collected included age, height, and body mass.
Participants in the knee OA group completed the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), the Physical Activity Scale for the Elderly (PASE), and the Survey of Activities and Fear of Falling in the Elderly (SAFFE) for descriptive purposes. The KL grade of knee OA was determined by 2 independent raters (J.T. and M.A.H.) from posteroanterior standing radiographs taken within the previous 6 months. All participants were asked to rate the amount of knee pain felt on average during the previous week on a numeric rating scale from 0 to 10 (0=“no pain,” 10=“worst possible pain”). At each testing session, participants completed the CB&M, BBS, TUG, and tests of single-leg stance time and gait speed. All tests were administered by the same assessor, and participants completed the tests in the same standardized order during all testing sessions.
Outcome Measures
Community Balance and Mobility Scale.
The CB&M comprises 13 tasks, including bending, turning, or looking while walking; single-leg standing; and stair descent. Tasks are rated by a trained assessor on a scale of 0 (“unable to perform”) to 5 (“proficient”), with the exception of stair descent, where participants can earn a maximum of 6 points for completing the task while carrying a load. Lower scores are given if participants are unable to meet time requirements or use discontinuous movements. Tasks such as single-leg stance, walking and looking (over an 8-m distance), running (over an 8-m distance), and step-ups (performance of 5 step-ups onto a stair) are timed, with slower times resulting in the loss of points on the task. Unilateral tasks such as single-leg stance or walking while looking at a target are performed on both sides. The maximum score is 96, with a minimum score of 0. For tasks that required a track on the CB&M, an 8-m track was used in a hallway. During testing on the track, the tester ensured that no other individuals used the hallway. For this study, the CB&M was scored by a trained kinesiologist with 2 years of experience. Assessment of the CB&M takes approximately 15 minutes to complete by a trained assessor and requires minimal equipment, including 2 weighted bags, an 8-m track with a target on the wall, a stopwatch, a set of 3 stair steps, and a beanbag. Further information of the individual tasks has been published by Rocque et al.26
Berg Balance Scale.
The BBS consists of 14 tasks that include static movements such as sitting and standing and movements such as turning and bending. Tasks are scored on a scale of 0 (“unable to perform or needs assistance”) to 4 (“able to perform independently”). Lower scores are given if participants are unable to meet time or distance requirements. The BBS was administered by a trained assessor using published guidelines.29
Timed “Up & Go” Test.
Participants completed the TUG in the same hallway used for completion of the CB&M. When completing the TUG, participants were instructed to rise from their chair without using the hand rests; walk as quickly as they could over 3 m, which was marked by a line of tape; turn around once they crossed the tape; return to the chair; and sit down.23 The chair height used for all tests was 41 cm, and time required to complete the TUG was recorded in seconds. Although permitted, no participants used gait aids during the TUG or during any other tests.
Single-leg stance time.
Participants were asked to stand on one leg for a maximum of 90 seconds. The arthritic knee was used for the knee OA group except in cases of bilateral involvement, in which case the more symptomatic leg was chosen as the stance limb. For the control group, the stance limb was randomly selected. Participants were instructed to bend the knee of the free limb up to 90 degrees and hold the position with arms by their sides. Participants were instructed to maintain their balance on one leg for as long as they could, to a maximum of 90 seconds. The test was completed if the participant touched the free limb to the ground, performed excessive upper body or trunk movements (eg, swinging arms), or completed the 90 seconds. Participants were allowed to try the single-leg stance twice if they were unable to maintain balance for more than 10 seconds during the first attempt, and the maximum time was recorded.
10-Meter Walk Test.
Gait speed was assessed using the 10-Meter Walk Test.23 Participants were asked to walk at their natural pace for 14 m, of which the middle 10 m was timed. The test was completed twice, and the mean of the 2 trials was calculated to determine the normal walking speed of the participant. The same test was repeated with participants asked to walk at a fast walking pace (“walk as quickly as you can, but safely”). Time was recorded in seconds and converted to meters per second.
Data Analysis
Differences on tests of balance and mobility, and in age and BMI, between participants with and without OA were assessed using independent t tests. For all analyses of validity, data from the first test session in the knee OA group were used to compare with the single session of data from the control group. Normal distributions of data were assessed using histograms and the skewness statistic, where skewness scores outside the range −1.0 to 1.0 indicate a non-normally distributed variable.30 Ceiling effects of the CB&M and BBS were calculated as the percentage of participants scoring the maximum possible score on the test.
To assess convergent validity of the CB&M, Pearson product moment correlation coefficients between the CB&M and other tests of balance and mobility were calculated. Significance of correlations was assessed by hypothesis testing, where the null hypothesis was that there is no correlation between outcome measures. The Spearman rank correlation coefficient was used in instances where data were not normally distributed. Correlations less than .5 were considered weak to fair, correlations of .5 to .75 were considered moderate, and correlations greater than .75 were considered strong.31 Known-groups validity of the CB&M was assessed by comparing scores on the CB&M and the other tests of balance between the knee OA and control groups using independent t tests. In instances of non-normality, the Mann-Whitney U test was used. Reliability of the CB&M and other tests of balance in the knee OA group was assessed by calculating intraclass correlation coefficients (ICC [2,1]) and standard error of measurement (SEM). The ICC was calculated using a 2-way random effects model with absolute agreement. Intraclass correlation coefficients greater than .4 were considered moderate, and ICCs greater than .8 were considered highly reliable.32 The SEM was chosen to test absolute reliability and was calculated as follows:
where sX=the standard deviation of the measurement.33 A high SEM indicates a high level of error and implies nonreproducibility of the measurements. Confidence intervals at 95% (95% CI) were calculated around ICC and SEM estimates. A Bland and Altman plot of CB&M scores comparing testing sessions was constructed to visually inspect the data. The minimum detectable change (MDC) at 95% confidence was calculated to provide clinical interpretation, as follows:
Results were considered statistically significant if P<.05. All statistical analyses were conducted using IBM SPSS version 21.0 (IBM Corp, Armonk, New York).
Role of the Funding Source
The authors acknowledge salary support from the Canada Research Chairs Program and the Michael Smith Foundation for Health Research. Support also was provided to Ms Takacs by the Canadian Institutes of Health Research.
Results
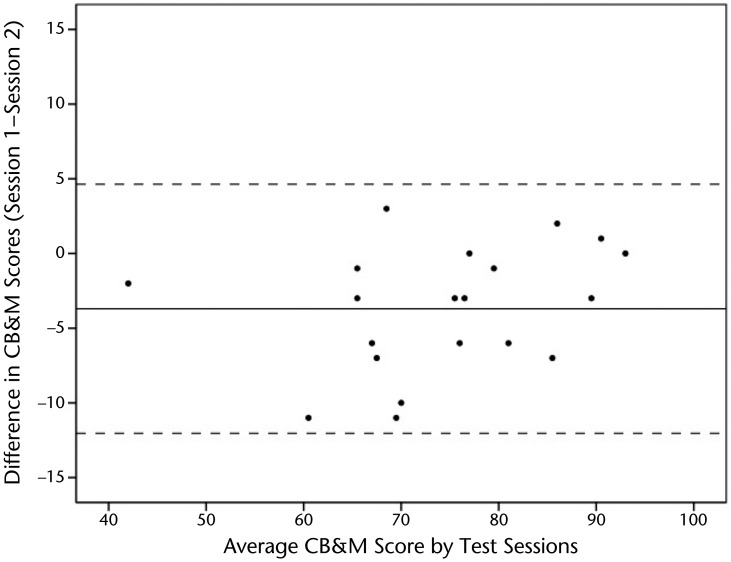
Participant demographics are shown in Table 1. Groups were sex- matched, with no significant differences in age between groups (P=.69). Those with knee OA had a significantly higher body mass index (BMI) than those without (P<.01). Most people had mild (KL rating=2, n=14) or moderate (KL rating=3, n=9) knee OA, with the remaining participants exhibiting severe (KL rating=4, n=2) knee OA. All data were normally distributed with the exception of the BBS data, which were analyzed using the Spearman rank correlation coefficient when examining correlation and with the Mann-Whitney U test when comparing groups. No ceiling effect was experienced on the CB&M in the knee OA group, with the highest score being 93/96, and only 12% of participants in the control group had the maximum score on this test. For the BBS, there was a considerable ceiling effect for both individuals with knee OA (64%) and those without knee OA (92%).
Table 1.
Participant Characteristicsa
Measurements are expressed as mean (SD). BMI=body mass index, WOMAC=Western Ontario and McMaster Universities Osteoarthritis Index, PASE=Physical Activity Scale for the Elderly, SAFFE=Survey of Activities and Fear of Falling in the Elderly, KL=Kellgren and Lawrence rating scale for osteoarthritis, N/A=not applicable. *Significant difference.
Validity
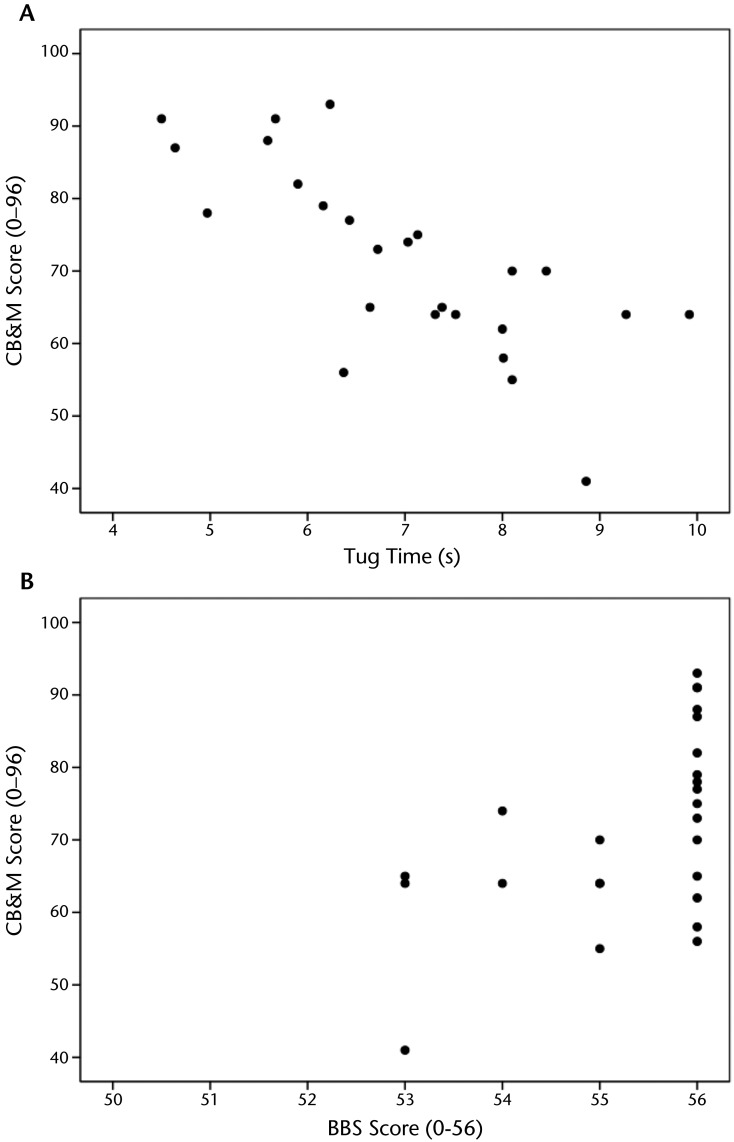
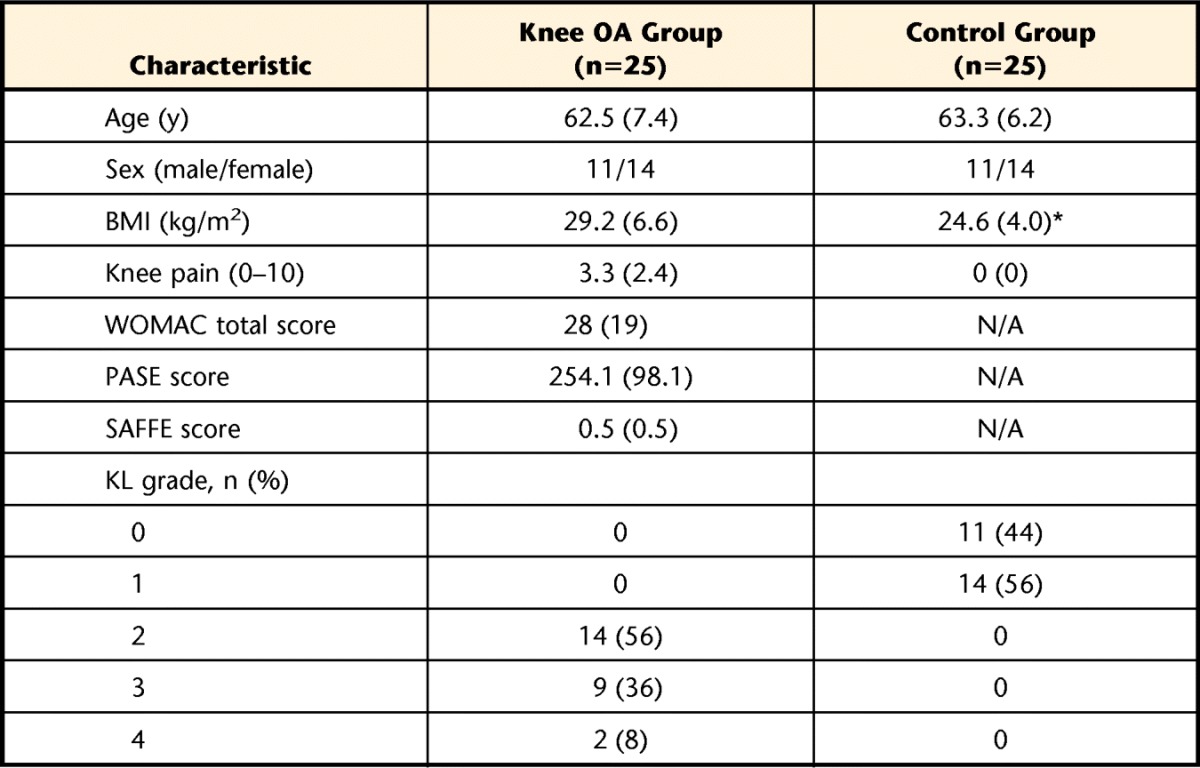
In the knee OA group, scores on all balance and mobility tests were significantly correlated with CB&M scores, with correlations ranging from .52 to .74 (Tab. 2), indicating moderate convergent validity. The CB&M correlated most strongly with the TUG, and least strongly with the BBS (Fig. 1). In the control group, correlations ranged from .21 to .63, with the CB&M correlating most strongly with the measure of single-leg stance time and least strongly with self-selected gait speed. The knee OA group scored significantly lower on all tests of balance and mobility than the control group except on the BBS and the 10-Meter Walk Test for fast walking speed (Tab. 3). Participants with knee OA scored, on average, 71 points (SD=13) on the CB&M, and those in the control group scored 85 points (SD=10). This significant difference in test scores on the CB&M, with individuals with knee OA scoring an average of 14 points lower than those in the control group (P<.001), indicated known-groups validity.
Table 2.
Correlation Matrix for Measures of Balance and Mobilitya
Tests of balance and mobility were correlated with the total score on the Community Balance and Mobility Scale (CB&M) for the group with knee osteoarthritis (OA group) and the control group. *Significant correlation at the .05 level. **Significant correlation at the .01 level.
Figure 1.
(A) Community Balance and Mobility Scale (CB&M) scores are moderately correlated with Timed “Up & Go” Test (TUG) times for participants with knee osteoarthritis (r=−.74; n=25). (B) CB&M scores were weakly correlated with the Berg Balance Scale (BBS) scores for participants with knee osteoarthritis (rho=.52; n=25).
Table 3.
Participant Scores on the Measures of Balance and Mobilitya
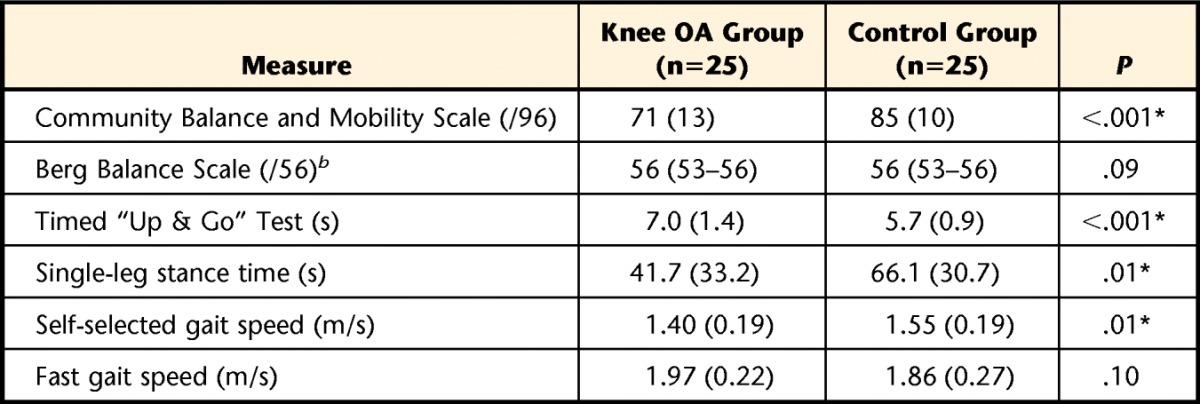
Data are expressed as mean (SD) for normally distributed scores and as median (range) for other scores. OA=osteoarthritis. *Significant difference.
b Non-normally distributed data.
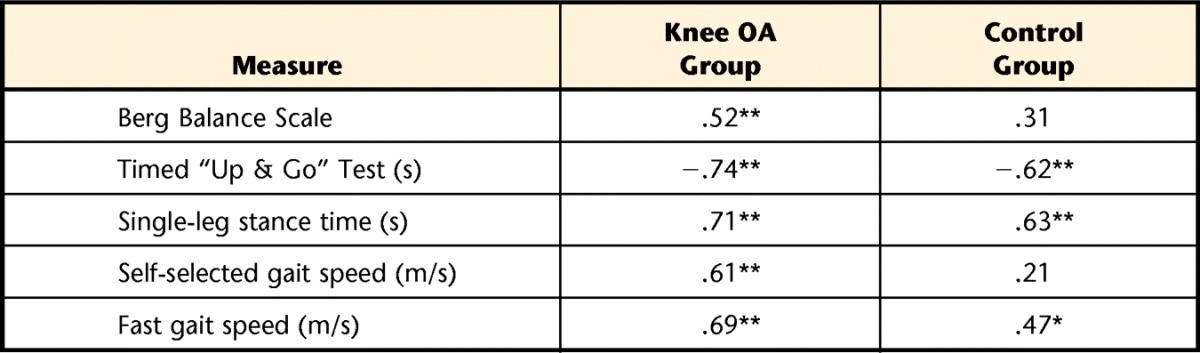
Reliability
Test-retest reliability was conducted on a subsample of 20 individuals with knee OA, as 5 of the participants were unable to return within the test-retest time frame (mean=8.0 days, range=4–14). Scores on each test for these individuals for each session are presented in Table 4. Test-retest reliability of the CB&M was high: ICC=.95 (95% CI=.70 to .99), SEM=3 (95% CI=2.68 to 4.67). A Bland and Altman plot for CB&M scores is presented in Figure 2 and further supports the reliability of this scale. Table 4 displays ICC and SEM values with 95% CI values, relative SEM values (SEM%), and 95% MDC values. The ICC values were greatest for the CB&M and lowest for the BBS (ICC=.59, 95% CI=−.07 to .84). With the exception of the BBS and TUG (which displayed moderate reliability), all other tests of balance and mobility (gait speed, CB&M) exhibited high test-retest reliability (ICC>.8). The 95% MDC value was 10 for the CB&M scores and 3 for the BBS scores. For all other MDC values, see Table 4.
Table 4.
Scores per Session for Participants Included in the Reliability Analysis (n=20)a
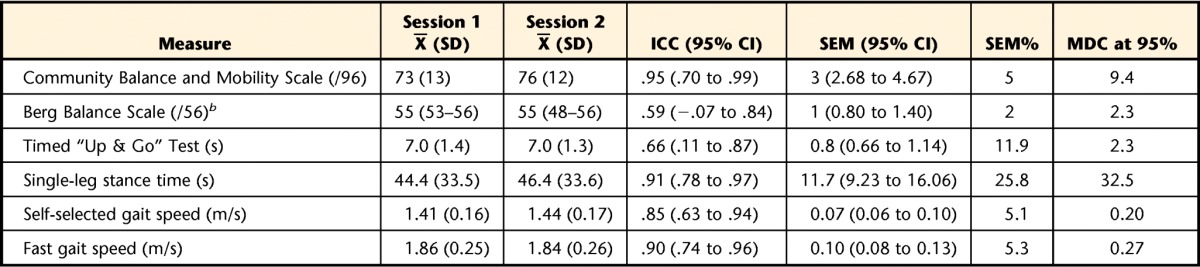
ICC=intraclass correlation coefficient, SEM=standard error of measurement, 95% CI=95% confidence interval, MDC at 95%=minimum detectable change at 95% level of confidence. Single-leg stance time is the maximum time the participant can maintain single-limb stance, up to 90 seconds. Gait speed was measured using the 10-Meter Walk Test.
b Non-normally distributed data.
Figure 2.
Bland and Altman plot representing comparisons between the 2 test sessions for the Community Balance and Mobility Scale (CB&M) score. Solid line indicates the mean difference between sessions, and dashed lines indicate limits of agreement (2 SD).
Discussion
The purpose of this study was to assess the validity and reliability of the CB&M in individuals with knee OA. The CB&M displayed moderate convergent validity with all administered tests of balance and mobility. Scores on the CB&M for the control group were significantly higher than scores for the knee OA group (P<.001), indicating excellent known-groups validity. Test-retest reliability of the CB&M also was high. The observed power for the study was 0.96, indicating the study was adequately powered to answer the research question. These results indicate that the CB&M is a valid and reliable tool for assessing dynamic balance and mobility in individuals with knee OA.
High convergent validity of a measure indicates that people score similarly on tests designed to measure the same construct. The validity of several tests of balance and mobility has been assessed for people with knee OA; however, we are unaware of a universally accepted “gold standard” for balance and mobility in this patient population. Accordingly, we chose to compare the CB&M against multiple valid outcome measures that assess different aspects of balance and mobility. For instance, tests of normal and fast walking speed are valid measures of mobility34 and have been used to measure change in mobility in individuals with knee OA before and after surgery.35 The TUG is similarly valid for assessing mobility in people with knee OA.22,36 Scores on the CB&M were highly correlated with all of these valid measures of mobility, particularly the TUG (r=−.74).
This relationship is similar in other studies that have assessed the validity of the CB&M in other populations. For example, in individuals with stroke, scores on the CB&M were correlated with the TUG (r=−.75), indicating that these 2 tests may measure similar constructs.27 Although the TUG is often used as a measure of mobility, the CB&M measures dynamic balance as well as mobility. Thus, the CB&M can be considered a more comprehensive test of the balance and mobility needed for independent function in the community. The CB&M displayed the lowest correlation with the BBS (r=.52), likely due to the finding that the BBS exhibited a substantial ceiling effect. Previous studies have highlighted possible ceiling effects in the BBS in several populations, including people with knee OA.20,27,37 In the current study, scores on the BBS ranged from 53 to 56, with a median score of 56 (the maximum) both for those with and without knee OA. In another study, individuals with knee OA scored, on average, 55 out of 56 on the BBS,20 similar to our results. These findings may have been be due to the fact that the BBS was originally designed to measure balance in elderly residents at a care facility.29 This lack of appreciable spread on the data may have resulted in the lower correlation between the CB&M and BBS found in the current study.
The knee OA group scored considerably lower on most tests of balance and mobility than the healthy control group, except on the BBS and 10-Meter Walk Test (fast walking speed). Previous literature has indicated that people with knee OA display various deficits in balance,38,39 in line with current results. When assessing balance and mobility, tests that are able to identify deficits in balance and mobility are needed. The CB&M displayed significant differences between groups in dynamic balance and mobility. These differences are similar to the group differences seen in some of the other tests of balance (eg, single-leg stance time) and mobility (eg, TUG) in this and other studies.40,41 Interestingly, the 10-Meter Walk Test (fast walking speed), where participants were asked to walk as quickly as they could, did not show significant differences between the knee OA group and the control group. This finding is contrary to previous literature that has shown small but significant differences in fast walking speeds.42 The self-selected walking speed for both groups was elevated (mean speed of 1.4 m/s for the knee OA group and 1.5 m/s for the control group; P<.01), highlighting the faster than usual speed of individuals with knee OA.43 In the current study, all but 2 individuals with knee OA had mild to moderate levels of disease and were highly functional (as evidenced by their fast walking speed, high BBS scores, and low TUG times). It is possible that the individuals with knee OA, when asked to increase their walking speed to their maximum, simply had the functional capacity to considerably increase their speed to a magnitude similar to the control group.
Test-retest reliability of an instrument is a key property allowing researchers and clinicians to administer a test repeatedly to people to assess change over time. The CB&M displayed very high test-retest reliability (ICC=.95, SEM%=5) in this sample of individuals with knee OA. Other tests of balance or mobility displayed moderate (ICC=.4–.8) and high (ICC>.8) reliability here (Tab. 4) and elsewhere, such as the TUG (r=.75).44 Self-selected walking speed (r=.9)34,45 and the BBS are highly reliable in older adults,23 although reliability of the BBS has not been assessed previously in people with knee OA. Reliability, as calculated by ICC values of the BBS in our population, was moderate but lower than all other tests of balance and mobility (ICC=.58), possibly owing to the low variance of the sample, as most individuals scored the maximum on the test. However, the SEM of the BBS was low, indicating high absolute reliability and further confirming low individual variation. Because both relative and absolute reliability of measures are important when interpreting findings, the high reliability of the CB&M (both ICC and SEM) makes it an attractive tool for assessing changes in dynamic balance and mobility over time.
The MDC values presented in Table 4 suggest, for instance, that for 95% of stable patients with characteristics similar to those of the participants in the current study, the score on the CB&M would change by less than 10 points upon reassessment in our laboratory. Furthermore, if the CB&M score of an individual with knee OA was 71, and after treatment improved to 83, we can be quite confident that the observed change in balance and mobility as measured by the CB&M is a true change because the change exceeds the MDC of 10 points. This MDC is less than 1 standard deviation of the CB&M, indicating that small changes can be true changes in balance and mobility, further supporting the reliability of the CB&M in people with knee OA.
There is growing evidence that some current measures of balance and mobility, such as the BBS, may have ceiling effects, where scores cluster around the maximum possible score with little variance, in some older populations that are more functional, such as people with knee OA. By contrast, no ceiling effect was seen for the CB&M in the current study. Participants in the current study scored between 41 and 93, with no participants with knee OA scoring the maximum 96 on the CB&M. In addition, the lowest score on the CB&M was 41, indicative that no floor effect was present either (minimum score of 0 possible). Furthermore, participants without knee OA were challenged by the tasks on the CB&M, with only 3 individuals scoring the maximum 96 points. A test of balance and mobility that is sufficiently challenging allows researchers and clinicians to evaluate change over time, such as improvement in balance and mobility due to a training intervention.
There were some limitations of the present study. First, all participants performed the CB&M in their own comfortable flat footwear (as per questionnaire guidelines). Because different shoes may have different coefficients of friction, certain tasks of the CB&M may be more difficult to perform (eg, foot scooting) for individuals who wear shoes with more traction. However, allowing participants to wear their own shoes increases the generalizability of the tasks and the scoring of their balance and mobility abilities. In addition, most individuals who participated in the study were mobile and highly functional. Only 2 individuals with KL grade 4 (severe) OA participated, and it is possible that those who have more severe grades of knee OA may have lower levels of function, and thus the relationship of balance and mobility test scores may have been altered.
Our results indicate the CB&M is a valid and reliable test with no indication of floor or ceiling effects. The tool displayed moderate convergent validity when compared with other tests of balance and mobility, and excellent known-groups validity was established by demonstrating significant differences between participants with and without knee OA. Test-retest reliability for the CB&M was very high. These findings indicate that the CB&M can be used as a valid and reliable tool to assess dynamic balance and mobility deficits in people with knee OA. Future research should assess the capacity of the CB&M in predicting falls in individuals with knee OA and other populations.
Footnotes
All authors provided concept/idea/research design and writing. Ms Takacs and Dr Hunt provided data collection and analysis and project management. Dr Hunt provided facilities/equipment.
Ethics approval was obtained from the Clinical Research Ethics Board of the University of British Columbia.
The authors acknowledge salary support from the Canada Research Chairs Program and the Michael Smith Foundation for Health Research. Support also was provided to Ms Takacs by the Canadian Institutes of Health Research.
References
- 1. Milat AJ, Watson WL, Monger C, et al. Prevalence, circumstances and consequences of falls among community-dwelling older people: results of the 2009 NSW Falls Prevention Baseline Survey. N S W Public Health Bull. 2011;22:43–48 [DOI] [PubMed] [Google Scholar]
- 2. Sylliaas H, Idland G, Sandvik L, et al. Does mortality of the aged increase with the number of falls? Results from a nine-year follow-up study. Eur J Epidemiol. 2009;24:351–355 [DOI] [PubMed] [Google Scholar]
- 3. Levinger P, Menz HB, Wee E, et al. Physiological risk factors for falls in people with knee osteoarthritis before and early after knee replacement surgery. Knee Surg Sports Traumatol Arthrosc. 2011;19:1082–1089 [DOI] [PubMed] [Google Scholar]
- 4. Brand C, Juan W, Lowe A, Morton C. Prevalence, outcome and risk for falling in 155 ambulatory patients with rheumatic disease. J Rheumatol. 2005;8:99–105 [Google Scholar]
- 5. Williams SB, Brand CA, Hill KD, et al. Feasibility and outcomes of a home-based exercise program on improving balance and gait stability in women with lower-limb osteoarthritis or rheumatoid arthritis: a pilot study. Arch Phys Med Rehabil. 2010;91:106–114 [DOI] [PubMed] [Google Scholar]
- 6. Pollock AS, Durward BR, Rowe PJ, Paul JP. What is balance? Clin Rehabil. 2000;14:402–406 [DOI] [PubMed] [Google Scholar]
- 7. Barker AL, Nitz JC, Low Choy NL, Haines TP. Mobility has a non-linear association with falls risk among people in residential aged care: an observational study. J Physiother. 2012;58:117–125 [DOI] [PubMed] [Google Scholar]
- 8. Rosendahl E, Gustafson Y, Nordin E, et al. A randomized controlled trial of fall prevention by a high-intensity functional exercise program for older people living in residential care facilities. Aging Clin Exp Res. 2008;20:67–75 [DOI] [PubMed] [Google Scholar]
- 9. Sherrington C, Whitney JC, Lord SR, et al. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc. 2008;56:2234–2243 [DOI] [PubMed] [Google Scholar]
- 10. Adegoke BO, Babatunde FO, Oyeyemi AL. Pain, balance, self-reported function and physical function in individuals with knee osteoarthritis. Physiother Theory Pract. 2012;28:32–40 [DOI] [PubMed] [Google Scholar]
- 11. Hunt MA, McManus FJ, Hinman RS, Bennell KL. Predictors of single-leg standing balance in individuals with medial knee osteoarthritis. Arthritis Care Res. 2010;62:496–500 [DOI] [PubMed] [Google Scholar]
- 12. Piva SR, Gil AB, Almeida GJ, et al. A balance exercise program appears to improve function for patients with total knee arthroplasty: a randomized clinical trial. Phys Ther. 2010;90:880–894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pandya NK, Piotrowski GA, Pottenger L, Draganich LF. Pain relief in knee osteoarthritis reduces the propensity to trip on an obstacle. Gait Posture. 2007;25:106–111 [DOI] [PubMed] [Google Scholar]
- 14. Pua YH, Liang Z, Ong PH, et al. Associations of knee extensor strength and standing balance with physical function in knee osteoarthritis. Arthritis Care Res. 2011;63:1706–1714 [DOI] [PubMed] [Google Scholar]
- 15. Masui T, Hasegawa Y, Yamaguchi J, et al. Increasing postural sway in rural-community-dwelling elderly persons with knee osteoarthritis. J Orthop Sci. 2006;11:353–358 [DOI] [PubMed] [Google Scholar]
- 16. Hall MC, Mockett SP, Doherty M. Relative impact of radiographic osteoarthritis and pain on quadriceps strength, proprioception, static postural sway and lower limb function. Ann Rheum Dis. 2006;65:865–870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kang HG, Dingwell JB. A direct comparison of local dynamic stability during unperturbed standing and walking. Exp Brain Res. 2006;172:35–48 [DOI] [PubMed] [Google Scholar]
- 18. Harada N, Chiu V, Damron-Rodriguez J, et al. Screening for balance and mobility impairment in elderly individuals living in residential care facilities. Phys Ther. 1995;75:462–469 [DOI] [PubMed] [Google Scholar]
- 19. Spagnuolo DL, Jurgensen SP, Iwama AM, Dourado VZ. Walking for the assessment of balance in healthy subjects older than 40 years. Gerontology. 2010;56:467–473 [DOI] [PubMed] [Google Scholar]
- 20. Kim HS, Yun DH, Yoo SD, et al. Balance control and knee osteoarthritis severity. Ann Rehabil Med. 2011;35:701–709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pardasaney PK, Latham NK, Jette AM, et al. Sensitivity to change and responsiveness of four balance measures for community-dwelling older adults. Phys Ther. 2012;92:388–397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dobson F, Hinman RS, Hall M, et al. Measurement properties of performance-based measures to assess physical function in hip and knee osteoarthritis: a systematic review. Osteoarthritis Cartilage. 2012;20:1548–1562 [DOI] [PubMed] [Google Scholar]
- 23. Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther. 2002;82:128–137 [DOI] [PubMed] [Google Scholar]
- 24. Curb JD, Ceria-Ulep CD, Rodriguez BL, et al. Performance-based measures of physical function for high-function populations. J Am Geriatr Soc. 2006;54:737–742 [DOI] [PubMed] [Google Scholar]
- 25. Howe JA, Inness EL, Venturini A, et al. The Community Balance and Mobility Scale: a balance measure for individuals with traumatic brain injury. Clin Rehabil. 2006;20:885–895 [DOI] [PubMed] [Google Scholar]
- 26. Rocque R, Bartlett D, Brown J, Garland SJ. Influence of age and gender of healthy adults on scoring patterns on the Community Balance and Mobility Scale. Physiother Can. 2005;57:2852–2892 [Google Scholar]
- 27. Knorr S, Brouwer B, Garland SJ. Validity of the Community Balance and Mobility Scale in community-dwelling persons after stroke. Arch Phys Med Rehabil. 2010;91:890–896 [DOI] [PubMed] [Google Scholar]
- 28. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Berg KO, Wood-Dauphineé SL, Williams JI, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83(suppl 2):S7–S11 [PubMed] [Google Scholar]
- 30. Gamst G, Meyers LS, Gaurino AJ. Analysis of Variance Designs. New York, NY: Cambridge University Press; 2008 [Google Scholar]
- 31. Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. 3rd ed Upper Saddle River, NJ: Pearson Prentice Hall; 2009 [Google Scholar]
- 32. Shrout P, Fleiss J. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428 [DOI] [PubMed] [Google Scholar]
- 33. Lin D, Seol H, Nussbaum MA, Madigan ML. Reliability of COP-based postural sway measures and age-related differences. Gait Posture. 2008;28:337–342 [DOI] [PubMed] [Google Scholar]
- 34. Marks R. Reliability and validity of self-paced walking time measures for knee osteoarthritis. Arthritis Care Res. 1994;7:50–53 [DOI] [PubMed] [Google Scholar]
- 35. Borjesson M, Weidenhielm L, Elfving B, Olsson E. Tests of walking ability at different speeds in patients with knee osteoarthritis. Physiother Res Int. 2007;12:115–121 [DOI] [PubMed] [Google Scholar]
- 36. Stratford PW, Kennedy DM, Riddle DL. New study design evaluated the validity of measures to assess change after hip or knee arthroplasty. J Clin Epidemiol. 2009;62:347–352 [DOI] [PubMed] [Google Scholar]
- 37. Newstead AH, Hinman MR, Tomberlin JA. Reliability of the Berg Balance Scale and Balance Master Limits of Stability Test for individuals with brain injury. J Neurol Phys Ther. 2005;29:18–23 [DOI] [PubMed] [Google Scholar]
- 38. Hassan B, Mockett S, Doherty M. Static postural sway, proprioception, and maximal voluntary quadriceps contraction in patients with knee osteoarthritis and normal control subjects. Ann Rheum Dis. 2001;60:612–618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hinman R, Bennell K, Metcalf B, Crossley K. Balance impairments in individuals with symptomatic knee osteoarthritis: a comparison with matched controls using clinical tests. Rheumatology. 2002;41:1388–1394 [DOI] [PubMed] [Google Scholar]
- 40. Bade MJ, Kohrt WM, Stevens-Lapsley JE. Outcomes before and after total knee arthroplasty compared to healthy adults. J Orthop Sport Phys. 2010;40:559–567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Zeni JA, Jr, Snyder-Mackler L. Clinical outcomes after simultaneous bilateral total knee arthroplasty: comparison to unilateral total knee arthroplasty and healthy controls. J Arthroplasty. 2010;25:541–546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Landry S, McKean K, Hubley-Kozey C, et al. Knee biomechanics of moderate OA patients measured during gait at a self-selected and fast walking speed. J Biomech. 2007;40:1754–1761 [DOI] [PubMed] [Google Scholar]
- 43. Creaby MW, Bennell KL, Hunt MA. Gait differs between unilateral and bilateral knee osteoarthritis. Arch Phys Med Rehabil. 2012;93:822–827 [DOI] [PubMed] [Google Scholar]
- 44. Kennedy DM, Stratford PW, Wessel J, et al. Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. BMC Musculoskelet Disord. 2005;6:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Davey R, Edwards SM, Cochrane T. Test-retest reliability of lower extremity functional and self-reported measures in elderly with osteoarthritis. Adv Physiother. 2003;5:155–160 [Google Scholar]