Abstract
The crowned dens syndrome (CDS), also known as periodontoid calcium pyrophosphate dehydrate crystal deposition disease, is typified clinically by severe cervical pain, neck stiffness and atlantoaxial synovial calcification which could be misdiagnosed as meningitis, epidural abscess, polymyalgia rheumatica, giant cell arthritis, rheumatoid arthritis, cervical spondylitis or metastatic spinal tumor. Crystalline deposition on cervical vertebrae is less well known disease entity and only a limited number of cases have been reported to date. Authors report a case of CDS and describe the clinical feature.
Keywords: Neck pain, Calcium pyrophosphate, Axis, Computed tomography
INTRODUCTION
Firstly, the crowned dens syndrome (CDS) was named by Bouvet et al. in 1985 as it was presented by cervical pain due to deposition of calcium pyrophosphate dehydrate (CPPD) crystals or hydroxylapatite at cervical spine and shown radiologically as crown or halo-like distribution when radio-opaque density appeared at the top and side of the odontoid process4). CPPD crystal or basic calcium phosphate crystal is originated from hyaline cartilage which contains hypertropic chondrocyte, and it can arise from any joint that is composed of cartilage but rarely from tendon or bursa. If it occurs at cervicoaxial joint surrounded by several ligaments and if it causes severe pain and limitation of neck rotation at the same time, so it can be named as CDS3,13). Authors report a case of CDS and review of the literature of this underrecognized condition.
CASE REPORT
A 49-year-old female visited the outpatient clinic with a 7-day history of acute onset severe posterior neck pain. On the day of symptom onset, she took an acupuncture and chiropractic manipulation of cervical spine which did not turn out to be helpful, and she experienced gradual worsening of pain and marked restriction of neck motion. There was no history of trauma and medical illness. On physical examination, passive cervical spine movements were significantly reduced without any focal neurologic deficit. Range of neck motion was limited to 20 degrees on rotation whereas extension and flexion were slightly diminished. At the end of the range of neck motion, pain was markedly provoked. Patient's vital signs were stable.
Plain radiographs of the cervical spine with open mouth view revealed abnormal radio-opaque lesion on the right side of the odontoid process (Fig. 1A). There was not any evidence of spinal instability on dynamic images. Computed tomography (CT) images showed atlantoaxial synovial calcifications in a crown or halo-like distribution around the odontoid process (Fig. 2A). Magnetic resonance image (MRI) showed low signal intensity around the odontoid process lesion on T1 weighted image but not involving itself (Fig. 3). Bone scan demonstrated increased radionuclide uptake around the odontoid process. We could not find any other lesion causative of pain within the spinal cord, nerve roots, intervertebral discs, cerebrospinal fluid and muscles. Laboratory tests revealed elevated high sensitive C-reactive protein (hsCRP) of 1.97mg/dL (normal range: 0.01-0.29mg/dL) while others were unremarkable. By integrating the result of tests listed above, we presumed a diagnosis as crowned dens syndrome.
Fig. 1.
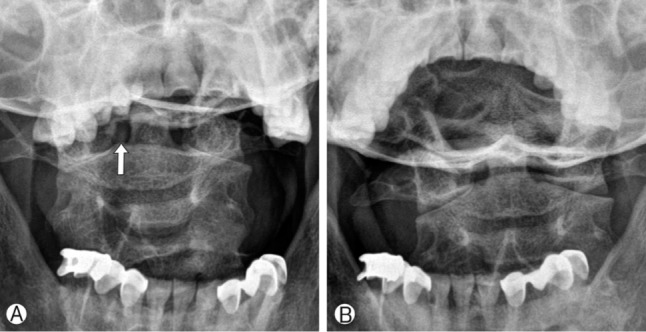
Open mouth view demonstrates radio-opaque lesion beside the odontoid process (arrow) (A). Open mouth view checked in one month reveals pre-existing radio-opaque lesion disappeared (B).
Fig. 2.
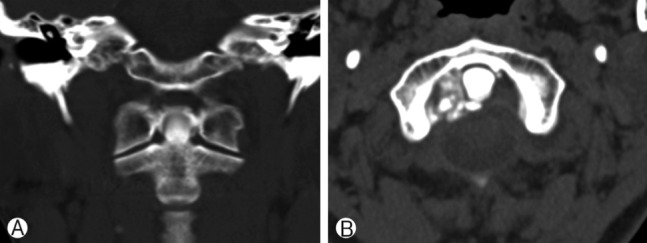
Coronal CT scan at C1/2 level demonstrates atlantoaxial synovial calcifications in a crown- or halo-like distribution around the odontoid process (A). Axial CT scan shows calcified lesion on the right side of periodontoid space and subchondral erosion (B).
Fig. 3.
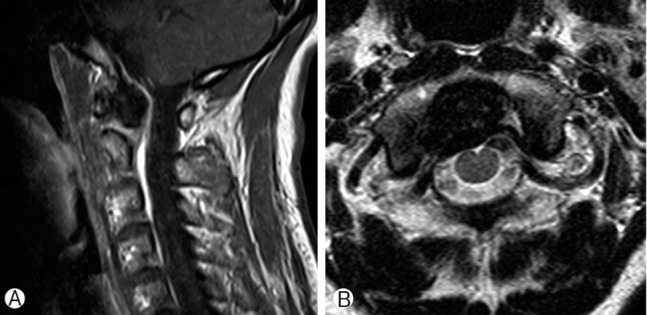
Sagittal (A) and axial (B) T1 enhanced magnetic resonance image reveal non-enhancing, non-invasive mass like lesion around the odontoid process.
Combination of prednisolone and nonsteroidal anti-inflammatory drug (NSAID) was taken and tapered off within three weeks, which led to resolve symptoms and normalize hsCRP. Neckbrace was put on to relieve motion-provoked pain during hospitalization. The lesion disappeared on plain radiographs followed in one month, which gave us a diagnostic clue to exclude such a condition from degenerative arthritis of the region (Fig. 1B).
DISCUSSION
The crowned dens syndrome is a rare disease entity which radiologically shows calcification at cruciform ligament around odontoid process and clinically presents acute cervico-occipital pain, fever, and neck stiffness accompanied by biological inflammatory reaction as mentioned earlier. In our case, clinical manifestations include severe posterior neck pain of acute onset, significant restriction of neck rotation and elevation of serum CRP. So that clinicians could make a confusion with spondyloarthritis around atlantoaxial joint area.
The duration of pain varies from few days to several weeks, the location can be from suboccipital area to inferior posterior neck, and the characteristics of pain are also diverse from mild neck discomfort to sleep-breaking severe pain5). Most of the crystalline deposits are calcium pyrophosphate dehydrate (CPPD) crystals or hydroxyapatite crystal. There is no specific symptom when the crystal's size is small, but as it grows, it causes chronic cervical pain or spinal cord compression. Calcification can occur at not only cruciform ligament but also transverse, alar and apical ligament. Especially when CPPD crystal deposition occurs at ligamentum flavum, compressive cervical myelopathy can be presented8,16). Dirheimer et al. performed plain radiographs to 27 patients who had articular chondrocalcinosis but neurologically asymptomatic, and demonstrated that syndesmo-odontoid joint calcification was found in 12 patients (44%)6). Constantin et al. performed CT scan to 21 patients with articular chodrocalcinosis, and found that 14 patients had calcifications at transverse ligament and 5 patients among the 14 presented neck pain5).
CDS can be misdiagnosed as meningitis, epidural abscess, rheumatoid arthritis, polymyalgia rheumatica (PMR), giant cell arthritis (GCA), cervical spondylitis or metastatic spinal tumor1,15,18). Especially, A. Aouba et al. emphasized that association with cervical stiffness and shoulder girdle pain or jaw claudication can be mislead to PMR or GCA1), and Laborie Y et al. reported that chondrocalcinosis such as CDS can be included in the category of rheumatic disease from a wide-spectrum perspective. However, it should be noted that the pathophysiologic process has not been completely proven9), and therefore, caution should be used in relying on such statements or findings. There are several pathophysiologic theories about CPPD deposition at atlantoaxial joint. First, Constantin et al. set forth that chondroid cell in fibrous cartilage structures like meniscus of knee can be found in transverse ligament around odontoid process, and the presentation of these cell causes the disease5). Another theory is that fibroblast in cervical spine ligament transforms into chondrocyte and the transformation may cause calcification7).
For diagnosis, CT scan focused on C1-2 region is gold standard to detect calcification in transverse, apical and alar ligament. CT is even more helpful for small sized lesion when three-dimensional reconstruction is possible1,15,17,18). CT scan seems to be superior to other diagnostic modality for ruling out CDS-like odontoid process fracture or Os odontoideum, and so forth. However, when CT scan is performed long time after the onset of symptom, calcification around odontoid process cannot be detected as it has been absorbed. So, CT scan should be done as soon as the symptom occurs10,20). The presence of calcification can be assumed through plain radiograph by radio-opacity difference around odontoid process, but there is limitation as anatomical structures around odontoid process cannot be clearly distinguished. MRI is also helpful in identifying compressed spinal cord or soft tissues like nerve root, tendon, etc. What is interesting is that performing plain radiograph systemically over other joints like knee or wrist even though there is no specific symptom might be helpful because there were many cases which involve joints other than atlantoaxial joint in the CDS patients group19). We couldn't find any abnormal joint except for periodontoid region. Elevation of ESR and CRP due to inflammatory reaction is common, and our case also showed slight elevation of CRP as 1.97mg/dL which could be explained by time interval between symptom onset and blood sampling11).
Surgical procedure is performed rarely to patients who are diagnosed with CDS, but Baysal et al. demonstrates that 1 among 17 cases of CDS patients who progressively presented neurologic symptom and was treated by decompression surgery. And under microscopic examination, CPPD crystal in fibrous tissue was found and chronic inflammatory change was presented2). In our case, when treated by combination therapy of prednisolone and NSAID, clinical symptoms showed dramatic improvement within 7 days. Although it was not clearly found that the period between the administration of NSAID and complete clinical recovery as many articles did not precisely describe, Ziza JM et al. and Resnick et al. reported that symptom had resolved on the 4th day of administration and complete recovery had been made in 3 weeks14,20). Reginato et al. reported that after the dramatic initial improvement within a week, there is a slow but persistent improvement in 3 to 5 weeks as the second phase, and it is the same at other lesions with microcrystalline joint. They also reported that colchicine seems to be effective, though not much as the effect of NSAID. There were debates about use of steroid, and low dose administration of steroid could be helpful to patients who have no effect from NSAID12).
CONCLUSION
Authors present a case of CDS as a rare cause of posterior neck pain with limitation of neck rotation. We suggest that clinicians should be aware of clinical feature of CDS for avoiding unnecessary lumbar puncture or biopsy, and cutting down hospitalization period.
Footnotes
This work was supported by the Soonchunhyang University Research Fund.
References
- 1.Aouba A, Vuillemin-Bodaghi V, Mutschler C, De Bandt M. Crowned dens syndrome misdiagnosed as polymyalgia rheumatica, giant cell arteritis, meningitis or spondylitis: an analysis of eight cases. Rheumatology (Oxford) 2004;43:1508–1512. doi: 10.1093/rheumatology/keh370. [DOI] [PubMed] [Google Scholar]
- 2.Baysal T, Baysal O, Kutlu R, Karaman I, Mizrak B. The crowned dens syndrome: a rare form of calcium pyrophosphate deposition disease. Eur Radiol. 2000;10:1003–1005. doi: 10.1007/s003300051052. [DOI] [PubMed] [Google Scholar]
- 3.Beutler A, Rothfuss S, Clayburne G, Sieck M, Schumacher HR., Jr Calcium pyrophosphate dihydrate crystal deposition in synovium. Relationship to collagen fibers and chondrometaplasia. Arthritis Rheum. 1993;36:704–715. doi: 10.1002/art.1780360520. [DOI] [PubMed] [Google Scholar]
- 4.Bouvet JP, le Parc JM, Michalski B, Benlahrache C, Auquier L. Acute neck pain due to calcifications surrounding the odontoid process: the crowned dens syndrome. Arthritis Rheum. 1985;28:1417–1420. doi: 10.1002/art.1780281215. [DOI] [PubMed] [Google Scholar]
- 5.Constantin A, Bouteiller G. Acute neck pain and fever as the first manifestation of chondrocalcinosis with calcification of the transverse ligament of the atlas. Five case-reports with a literature review. Rev Rhum Engl Ed. 1998;65:583–585. [PubMed] [Google Scholar]
- 6.Dirheimer Y, Bensimon C, Christmann D, Wackenheim C. Syndesmo-odontoid joint and calcium pyrophosphate dihydrate deposition disease (CPPD) Neuroradiology. 1983;25:319–321. doi: 10.1007/BF00439211. [DOI] [PubMed] [Google Scholar]
- 7.Doherty M, Dieppe P. Crystal deposition disease in the elderly. Clin Rheum Dis. 1986;12:97–116. [PubMed] [Google Scholar]
- 8.Fye KH, Weinstein PR, Donald F. Compressive cervical myelopathy due to calcium pyrophosphate dihydrate deposition disease: report of a case and review of the literature. Arch Intern Med. 1999;159:189–193. doi: 10.1001/archinte.159.2.189. [DOI] [PubMed] [Google Scholar]
- 9.Laborie Y, Berthelot JM. Rhizomelic pseudopolyarthritis: update. Rev Med Interne. 2002;23:518–532. doi: 10.1016/s0248-8663(02)00607-0. [DOI] [PubMed] [Google Scholar]
- 10.Malca SA, Roche PH, Pellet W, Combalbert A. Crowned dens syndrome: a manifestation of hydroxy-apatite rheumatism. Acta Neurochir (Wien) 1995;135:126–130. doi: 10.1007/BF02187755. [DOI] [PubMed] [Google Scholar]
- 11.Ogata M, Ishikawa K, Ohira T. Cervical myelopathy in pseudogout. Case report. J Bone Joint Surg Am. 1984;66:1301–1303. [PubMed] [Google Scholar]
- 12.Reginato AJ, Reginato AM. Disease associated with depositon of calcium pyrophosphate or hydroxyapatie. In: Rubby S, Harris EDJ, Sledge CB, editors. Kelly's Textbook of Rheumatology. ed 6. Vol 1. Philadelphia: W.B.Saunders; 2001. pp. 1377–1390. [Google Scholar]
- 13.Reginato AJ, Schumacher HR, Martinez VA. The articular cartilage in familial chondrocalcinosis. Light and electron microscopic study. Arthritis Rheum. 1974;17:977–992. doi: 10.1002/art.1780170611. [DOI] [PubMed] [Google Scholar]
- 14.Resnick D, Pineda C. Vertebral involvement in calcium pyrophosphate dihydrate crystal deposition disease. Radiographic-pathological correlation. Radiology. 1984;153:55–60. doi: 10.1148/radiology.153.1.6089266. [DOI] [PubMed] [Google Scholar]
- 15.Salaffi F, Carotti M, Guglielmi G, Passarini G, Grassi W. The crowned dens syndrome as a cause of neck pain: clinical and computed tomography study in patients with calcium pyrophosphate dihydrate deposition disease. Clin Exp Rheumatol. 2008;26:1040–1046. [PubMed] [Google Scholar]
- 16.Sato R, Takahashi M, Yamashita Y, Izunaga H, Sakamoto Y, Yamamoto M, et al. Calcium crystal deposition in cervical ligamentum flavum: CT and MR findings. J Comput Assist Tomogr. 1992;16:352–355. doi: 10.1097/00004728-199205000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Scutellari PN, Galeotti R, Leprotti S, Ridolfi M, Franciosi R, Antinolfi G. The crowned dens syndrome. Evaluation with CT imaging. Radiol Med. 2007;112:195–207. doi: 10.1007/s11547-007-0135-7. [DOI] [PubMed] [Google Scholar]
- 18.Wu DW, Reginato AJ, Torriani M, Robinson DR, Reginato AM. The crowned dens syndrome as a cause of neck pain: report of two new cases and review of the literature. Arthritis Rheum. 2005;53:133–137. doi: 10.1002/art.20915. [DOI] [PubMed] [Google Scholar]
- 19.Zapletal J, Hekster RE, Straver JS, Wilmink JT, Hermans J. Association of transverse ligament calcification with anterior atlanto-odontoid osteoarthritis: CT findings. Neuroradiology. 1995;37:667–669. doi: 10.1007/BF00593391. [DOI] [PubMed] [Google Scholar]
- 20.Ziza JM, Bouvet JP, Auquier L. Acute suboccipital neck pain of calcifying origin. Rev Rhum Mal Osteoartic. 1982;49:549–551. [PubMed] [Google Scholar]


